Abstract
The primary objective of this study is to describe the demographics and clinical characteristics of patients with Poncet’s disease (PD) in the Makkah region in Saudi Arabia, where tuberculosis is on the rise. The secondary objective is conducting a PD systematic literature review to compare our findings. We studied seven patients who presented with arthritis within the first 3 years from diagnosis of active tuberculosis in two centers in the Makkah region: King Faisal Specialist Hospital and King Fahad Hospital in Jeddah from January 2005 to December 2011. We conducted a literature review on PD in multiple biomedical/pharmaceutical databases up to December 2011. We detected a new pattern of reactive arthritis associated with tuberculosis (TB). We identified this as PD or tuberculous rheumatism, which is a sterile reactive arthritis that can emerge during any stage of acute TB infection. Seven cases of Poncet’s disease were identified in our study. The most common presentation was extrapulmonary with involvement of multiple sites. Six out of seven patients developed arthritis after initiation of anti-TB drugs; one patient developed polyarthritis after completion of anti-TB medication. Asymmetrical polyarthritis was the most common presentation and the resolution of the arthritis was with symptomatic treatment and continuation of anti-TB drugs except in one case. PD may manifest in a variable pattern during the course of active tuberculous infection. Physicians should be aware of this rare complication associated with a common disease to prevent delay in diagnosis and initiation of appropriate treatment.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Poncet’s disease (PD) or tuberculous rheumatism is a sterile reactive arthritis that is not well known and therefore often missed [1]. PD is characterized by a polyarthritis that occurs during acute tuberculosis (TB) infection in which no evidence of direct mycobacterial involvement of the joints or other known cause of polyarthritis is detected. Therefore, it is a different entity from tuberculous arthritis because unlike tuberculous arthritis, which is usually monoarticular and in which the organism can be isolated from the joint, PD is detected through a diagnosis of exclusion [2, 3]. The pathogenic mechanism hypothesized is: after infection as a result of systemic immunization sensitized CD4+ cells and the bacterial antigens migrate to the joints and cause arthritis [4].
There are two objectives to this study. The first is to describe the demographics, clinical characteristics, and outcome of patients with PD in the Makkah region where tuberculosis is on the rise. The study was conducted in two rheumatology centers in the Makkah region: King Faisal Specialist Hospital (KFSH) and King Fahd Hospital (KFH) in Jeddah from January 2005 to December 2011. The second objective is to conduct a systematic literature review about PD and compare our findings.
It is a concern reported in many studies by Khoury [5], Summers [6], and Keat [7] that not all clinicians are aware of PD. The majority of the cases reported in the literature were at time of initial diagnosis of TB, in contrast to our cohort which developed the arthritis during all stages of tuberculous infection. We describe a new pattern of reactive arthritis associated with TB that developed during and/or after completion of all anti-tuberculous (anti-TB) therapy where all other causes of arthritis were excluded. We conducted a systematic literature review about PD to compare our findings.
Materials and methods
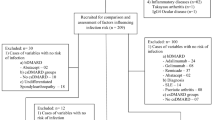
We retrospectively reviewed the medical records of all patients with PD presenting to the rheumatology unit at two centers (KFSH and KFH in Jeddah) from January 2005 to December 2011. Institutional review board approved the research protocol in both centers. The inclusion criteria included all patients above the age of 13 with the following features: confirmed diagnosis of tuberculosis with definite isolation of the organism either by direct culture of a body fluid (using acid fast bacilli smear and/or culture with PCR technique to confirm it) or by a histopathological confirmation by the presence of caseating granuloma with preferred detection of acid fast bacilli and/or isolation of the organism by direct culture of the body tissue, and a confirmed clinical diagnosis of arthritis by a qualified rheumatologist. The clinical diagnosis of arthritis could be made either before the diagnosis of TB, with the initial presentation of TB, in a patient on anti-TB drugs, or in a patient who had received full course of treatment with anti-TB drugs in the last 3 years. Synovial fluid culture and/or histopathological examination of the synovial membrane should be negative to isolate the organism in the joint(s) involved in PD.
Exclusion criteria included age less than 13 years, positive synovial fluid culture for TB in the joints involved in PD, synovial biopsy demonstrating findings consistent with TB, clinical findings, and serology highly suggestive of other rheumatological diseases.
Data was collected from each chart in a case sheet and included: demographic of the patients, full details about their TB status including site, confirmation tests, imaging, and anti-TB medications. Other data included: time of presentation with arthritis, site and number of joints involved, joint aspiration results, acid fast bacilli cultures, and PCR technique. Serological tests were included if they were done including rheumatoid factor (RF), anticitrullinated protein antibodies (ACPA), and C-reactive protein (CRP). Results of all radiological images and all medications that the patients received were included as well.
A literature search was conducted in several biomedical/pharmaceutical databases for information regarding PD. The list of databases and resources searched are shown in Table 1. The search key words used were Poncet’s (disease or disorder or illness or arthritis), reactive arthritis, and tuberculosis found in the title (ti), abstract (ab), or subject term (de) fields. The references were limited to English language and human subjects, but not the publication date.
Results
Seven cases of PD were identified in our retrospective review from January 2005 to December 2011, which are presented below. A total of 57 cases were detected in the systemic literature review; 52 cases were summarized in an early previous literature review by Kroot et al. in 2007 [8]. Our literature review revealed additional five cases since then. All additional cases with our cases are described in this report are summarized in Table 2.
Case 1
A 23-year-old female patient born in1987 was evaluated in KFSH with 1-year history of chronic abdominal pain and significant weight loss. Upper and lower gastrointestinal endoscopy were unremarkable. CT abdomen with contrast showed extensive omental nodules in upper abdomen. Peritoneal biopsy and cytology showed chronic granulomatous inflammation and giant cells with no malignant cells. Culture was not available. TB peritonitis was diagnosed and she was started on anti-TB treatment (ethambutol, pyrazinamide for 2 months, isonazide and rifampicine to complete a course for 1 year). On 9 June 2010, 4 months after starting treatment with anti-TB drugs she complained of knees, shoulders, and hands pain and swelling. Examination revealed temp of 36.8 °C and tenderness on both knees, shoulders, and second and third metacarpophalangeal (MCP) joints of the hands with no effusion. Laboratory testing showed leukocyte count of 4.3 × 109/l, CRP of 101 mg/dl and erythrocyte sedimentation rate (ESR) of 32 mm/h; RF and ACPA were negative. Synovial fluid gram stain and acid fast bacilli were negative as well as the cultures. X-ray of chest showed no infiltration. PD was diagnosed and the patient was started on naproxen 500 mg every 12 h, omeprazole 20 mg once daily, and prednisone 10 mg daily. During the follow-up in out-patient clinics, her arthritis improved over a 6-month duration with normalization of her ESR and CRP.
Case 2
A 50-year-old female patient born in 1960 was admitted in KFSH with history of productive cough, fever, and night sweats for 1-year duration. Upon admission, she was investigated for pulmonary TB. Frequents sputum culture and stain for TB were negative. Chest X-ray showed right pleural effusion, CT scan of the chest showed small nodule on anterior chest wall with right pleural effusion. Bronchoalveolar lavage was done and showed negative culture for TB. Video-assisted thoracic surgical biopsy of the pleura was done by thoracic surgeon and showed multiple caseating granulomas consistent with TB. The patient was started on anti-TB drugs (ethambutol and pyrazinamide for 2 months, isonazide and rifampicine for 9 months). On 4 July 2010, she developed pain and swelling over the knees 2 months after starting her anti-TB drugs. On physical examination, with temperature of 36.5 C, there was acute arthritis of both knees. Laboratory findings showed a leukocyte count of 5.5 × 109/l with a CRP of 82.5 mg/dl. ESR was not done. RF and ACPA were negative. Analysis of synovial fluid was traumatic, bloody fluid with neutrophil count 54 % and lymphocyte count 29 %, cultures were negative and no crystal were detected. X-ray of knees showed osteoarthritic degenerative changes. PD based on these findings was diagnosed. The patient was started on prednisone 10 mg and acetaminophen and the anti-TB drugs were continued. She tolerated the medication well. During her regular visits in the clinic, the arthritis improved over 5 months and CRP returned to normal levels.
Case 3
A 48-year-old female born in 1963 was admitted in KFSH with cervical and axillary lymphadenopathy for 6 months. Fine needle biopsy of the cervical node showed necrotizing granulomatous disease consistent with TB. She was started on pyrizinamide and ethambutol for 2 months and isonazide, rifampicine to complete 6 months of therapy. On 13 March 2009, she developed arthritis in left second and fourth MCP joints, left wrist, and in both knees 1 month after completing her course of anti-TB therapy. There was no evidence of recurrence with radiological regression of lymphadenopathy. Laboratory testing showed leucocytes of 5 × 109/l and ESR 40 mm/h; RF and ACPA were negative and with CRP of 33 mg/dl. Chest X-ray was unremarkable. MRI of the left hand showed no degenerative changes and MRI of the left knee showed minimal effusion and minimal degenerative changes. She was started on plaqunil 200 mg twice daily, methotrexate 15 mg/week, and folic acid and prednisone 10 mg daily. Two months later, the patient developed right thumb tenosynovitis and arthritis in right second and third MCP and right knee. The patient was not adherent to her medications as she poorly tolerated them. ESR and CRP remained elevated and no improvement in patient condition. She was offered anti-TNF-alpha therapy but was reluctant to accept the risk of TB reactivation.
Case 4
A 30-year-old Yemeni male patient born in 1980 was admitted to KFH with confusion and seizures. CT brain showed multiple enhanced cerebral lesions. Chest X-ray showed a cavitatory lesion. MRI of spine showed paraspinal abscess involving from fifth to seventh thoracic vertebrae. Paraspinal biopsy showed granulomatous disease consistent with TB. Tuberculin test was positive. Standard cultures of blood and sputum for TB were negative. Anti-TB drugs were started with ethambutol and pyrazinamide for 2 months, rifampicine and isoniazide for 9 months. Topamax was added for seizures. On 10 May 2010, 2 months after starting the treatment, he developed arthritis of both ankles and right knee. Laboratory tests showed leucocytes of 3.3 × 109/l and ESR of 110 mm/h; RF and ACPA were not done, CRP of 19.5 mg/dl and uric acid of 5.4 mg/dl. X-rays of knees and ankles showed soft tissue swelling bilaterally. Analysis of synovial fluid was negative for crystals. PD was diagnosed. He was started on nonsteroidal anti-inflammatory drugs (NSAID) and the anti-TB drugs continued. The arthritis was resolved in 3 months time.
Case 5
A 30-year-old Indonesian female patient born in 1980 was admitted to KFH complaining of shortness of breath and productive cough for 2 months. At presentation, her chest examination showed right pleural effusion with supraclavicular lymph node enlargement. Tuberculin test was positive. CT scan of the chest showed necrotizing left supraclavicular lymph nodes, left and right paratracheal lymph node enlargement, and right lung consolidation with mild pleural and pericardial effusion. Pleural fluid was exudative and biopsy showed vague epitheloid granuloma with negative culture for TB. She was diagnosed to have TB of pulmonary, pleural, pericardial, and lymph nodes. She was started on ethambutol and pyrazinamide for 2 months, isoniazide and rifampicine for 9 months. On 4 August 2010, 4 months after starting anti-TB medications, she developed arthritis of the left wrist, all MCP joints, dactylitis of second, third and fourth digits of the right hand, and arthritis of the left ankle, with ulcerative skin lesions on the right shoulder and the right foot. Chest examination showed resolution of the pleural effusion. Laboratory testing showed leucocytes of 5.5 × 109/l, ESR 110 mm/h, RF, ANA (anti-nuclear antibodies), anti-double-stranded DNA antibodies, and anti-neutrophil cytoplasmic antibodies were all negative. ACPA was not done. X-rays of ankles, hands, and feet showed soft tissue swelling with destructive bone lesion in the third right proximal interphalangeal (PIP) joint. Skin biopsy showed granulation tissue with giant cells consistent with TB. Analysis of synovial fluid was not done due to scanty fluid. Standard cultures and cultures for TB revealed no pathogen. Culture of the skin biopsy was negative. Based on these findings, PD was diagnosed with tuberculosis of the skin and osteomyelitis of the right third PIP joint. Therapy with ibuprofen 400 mg Q 12 h was started, after which the arthritis resolved in 8 months, with continuation of the anti-TB drugs. Ciprofloxacillin was added to the conventional anti-TB drugs.
Case 6
A 20-year-old Saudi female patient born in 1985 was referred to the rheumatology clinic in KFH with polyarthritis in November 2005. She was recently diagnosed to have pulmonary TB in the chest hospital. Chest X-ray showed consolidation of the left lower lobe with strong positive history of exposure to TB (brother had pulmonary TB). Sputum was positive for acid fast bacilli (AFB). She was started on first-line conventional anti-TB medications. On 21 November 2005, 1 month after starting the anti-TB therapy, she started to complain of pain and swelling in knees, ankles, and the small joints of the hands. Physical examination revealed a temperature of 38 °C with acute arthritis of both knees, both ankles, and all MCPS and PIP joints Laboratory testing showed leucocytes of 10 × 109/l, ESR of 118 mm/h, and uric acid of 7.6 mg/dl; RF and ACPA were not done. X-rays of ankles, hands, and feet revealed soft tissue swelling. Analysis of synovial fluid of the right knee joint revealed white cell count of 60 cells/mm3 with 100 % polymorph. The synovial fluid was positive for uric acid crystals. Standard cultures of body fluids and cultures for TB of all obtained synovial fluid samples were negative. Based on these results, pyrazinamide induce crystal gouty arthritis was diagnosed and it was stopped and replaced by ciprofloxacillin. The patient was started on colchicine and NSAIDs. As gouty arthritis is mainly a monoarthritis, it was presumed retrospectively that the patient had Poncet’s disease superadded with the drug-induced gouty arthritis. Polyarticular gouty arthritis usually occurs in patients with a past history of intermittent acute gout, prior attacks of polyarticular arthritis, previous hyperuricaemia, and/or obvious tophi. During her regular follow up in the rheumatology clinic, the arthritis of the affected joints improved over 30 days with normalization of the ESR and uric acid levels.
Case 7
A 23-year-old Saudi female teacher born in 1986 was admitted to KFH with fever, weight loss, night sweats, productive cough, and headache for 1 month. On examination, her temperature was 39 °C with neck stiffness. CT scan brain and spine showed basal meningeal enhancement with myelitis and epidural abscess. CT chest and abdomen revealed pinpoint multiple tiny nodules in the lungs, liver, and spleen. Sputum AFB was positive. Cultures were not available. She was diagnosed as military tuberculosis and started on conventional anti-TB drugs with dexamethasone. Surgical drainage of the paraspinal abscess with decompression of the dorsal spine was done. Biopsy showed necrotic and hemorrhagic tissue. On 23 June 2009, the patient suffered from pain and swelling of both knees that started 8 weeks after initiation of anti-TB drugs. Physical examination revealed arthritis of both knees. Aspiration of the joints was not done. PD was the likely diagnosis with this presentation. Laboratory testing showed leucocytes of 4.7 × 109/l and ESR of 10 mm/h; RF and ACPA were not done. X-rays of knees showed soft tissue swelling. Bone scan showed homogeneous uptake in both knees. Sputum analysis was still positive for AFB after 8 weeks of treatment, so streptomycin was added. Treatment with NSAIDS was started for the arthritis. The patient’s general condition improved and the arthritis resolved in 2 months.
Discussion
Saudi Arabia is at an increased risk for TB transmission because of mass gatherings due the presence of holy places and the large number of immigrant workers [9]. Makkah region, were this study was conducted, reported the greatest number of TB cases (1,648) and the highest TB incidence rate (26 per 100,000) [9].
There is a concern that Saudi Arabia is not meeting the WHO target of 85 % of successful treatment [10]. One of the solutions is to improve and unify diagnostic services [10]. The same concept should be applied on improving awareness of clinicians about musculoskeletal TB. Approximately 10–11 % of extrapulmonary TB involves joints and bones, which is approximately 1–3 % of all TB cases [4]. The study of Kroot et al. focused on a sterile reactive arthritis that may complicate TB rather than TB septic arthritis. This condition is less known as the literature is scarce and restricted to case reports and therefore often missed and underdiagnosed [8, 11].
One of the old definitions of PD stated that it is a polyarthritis associated with extrapulmonary TB with no evidence of direct bacteriological involvement of the joints [12]. In one review about PD that included 52 cases of PD, an extrapulmonary site was only present in 48 % of the patients [8]. Our extended review from 2007 to April 2012 showed that three cases out of five had extrapulmonary TB. However, in our cohort, five out of seven patients had extrapulmonary TB. It was observed by Simcock et al. that the extrapulmonary site associated with PD is usually the lymph node [12]. In a study conducted in Saudi Arabia by Al-Otaibi and El Hazmi, the prevalence of extrapulmonary TB was 57.5 % in comparison to pulmonary TB (42.5 %), and the most common site was lymph node TB (42 %) [13]. TB lymphadenitis was not a common site in our cohort associated with PD but with severe disease with multiple site involvement. It is concluded that this immunologic phenomenon has its association with the organism itself rather than its primary location.
The classic clinical presentation of PD in most reported cases is arthritis as part of systemic and acute presentation of TB. This was stated even as a definition for PD in several case series [2, 3, 8].
In four out of five additional PD cases in Table 2 identified in the literature, arthritis was reported as an initial presentation for acute TB infection [1, 14, 15]. Only one case reported additive polyarthritis involving knees, ankles, and wrist joints in a patient who had chronic polyarthritis following nephrectomy 5 years prior to presentation due to confirmed renal tuberculosis [19]. In our cohort of patients reported in this study, six out of seven patients developed arthritis after initiation of anti-TB drugs by a range from 1 to 4 months. Only one patient, after receiving full treatment for TB lymphadenitis, developed polyarthritis with tenosynovitis. All serological work up for arthritis was negative in this patient. This may broaden our understanding of PD in association with the clinical course of TB presentation and treatment. The onset of arthritis may present acutely and concomitantly with symptoms and signs of TB from its primary site weather pulmonary or extrapulmonary in origin. The extrapulmonary site might be even septic tuberculous arthritis with nonspecific arthritis of the other joints at the same acute presentation [8]. This acute presentation of arthritis with the acute onset of TB is the most commonly described presentation in the literature. Another presentation observed in this study is the development of arthritis after initiation of anti-TB drugs. However, TB septic arthritis of the joints and crystal-induced arthritis by anti-TB drugs should be excluded as we had demonstrated. It has to be noted that in one review of PD [8], one case was excluded due to development of arthritis 6 months after initiation anti-TB drugs [17]. This case would have been consistent with our observation for expanding the definition of PD. Even after completion of anti-TB course of therapy, PD may develop as in one case reported in this study where the patient developed a new onset of polyarthritis and tenosynovitis after completion of full and adequate course of therapy for TB lymphadenitis. The clinical presentations of PD should include not only acute arthritis at the time of clinical onset of TB, but it should include as well arthritis developing during the course of anti-TB therapy and arthritis developing after completion of full course of therapy.
Polyarthritis is the most common presenting feature in our cohort consistent with the literature [8]. Knees followed by small joints of the hands particularly MCP joints were the most commonly involved joints in our cohort of patients. In a review by Kroot et al., knees and ankles were the most commonly involved joints followed by the wrists [8]. In a recent study by Garg et al. where they included 18 patients with acute inflammatory ankle arthritis, eight of them were classified as having PD based on positive Mantoux test with only mediastinal and/or paratracheal and/or unilateral hilar lymphadenopathy with central necrosis [18]. In this study from India, Lofgren’s syndrome was diagnosed if Mantoux test was negative and bilateral hilar lymphadenopathy was present without central necrosis [18]. This study suggested a diagnostic approach to acute ankle arthritis in an endemic area for TB. It was based on Mantoux test and computed tomography scan of the chest. The lack of microbiological and histopathological diagnostic confirmation questions the accuracy of this diagnostic approach. It is a common observation across all reports that the arthritis of PD resolves upon starting or receiving adequate anti-TB therapy [1, 8, 14, 15, 19, 20] but one of the patients in our cohort did not respond to multiple interventions due to significant drug allergies.
Diagnosing PD represents a real challenge to clinicians. The clinical presentation of PD should be expanded based on our observation since PD is an underdiagnosed clinical entity. The differential diagnoses of polyarthritis in a young patient in an endemic area should include TB with a thorough search for primary site of infection with adequate history, physical examination, and imaging studies particularly simple chest X-rays. Synovial fluid analysis, culture, and possibly biopsy should always be obtained to rule out septic tuberculous arthritis and assure sterility of the joints to confidently establish the diagnosis of PD. This condition was not always available for several cases of PD in the literature. Synovial fluid culture and histology was conducted for 30 % only in one literature review of PD [8]. Only in one case in our literature review, septic tuberculous arthritis was ruled out by negative TB culture but the synovial fluid was positive for DNA of the Mycobacterium tuberculosis [14]. Most clinicians would rely primarily on the classic clinical presentation where there is polyarthritis acutely in a patient with a clear primary site for TB. This is in addition to the rapid resolution of arthritis once anti-TB drugs are commenced. It was reported to resolve in as short as 3 days after the initiation of anti-TB drugs [1]. This feature may be used as a confirmatory observation for PD. This rapid resolution of arthritis was not observed in our cohort of patients. However, synovial fluid analysis should always be considered and ruling out septic tuberculous arthritis by culture and/or histopathology should always be considered particularly if big joints are involved. Isolating M. tuberculosis DNA from synovial fluid may not be an essential step to diagnose PD as this technique needs validation in addition to its high cost particularly in developing countries. In a recent case report of PD, the diagnosis was established based on demonstration of two- to sixfold increase in M. tuberculosis-specific T cells in synovial fluid than in blood using M. tuberculosis-specific interferon γ enzyme-linked immunospot assay [14]. In another case of PD, the test was conducted in the blood and gave positive results [19].
Reactive arthritis could be considered to occur in two forms, one HLA-B27 associated and another HLA-B27 non-associated [16]. Mycobacterium has been considered as non-associated with HLA-B27 [16]. A majority of previously reported cases in the literature did not test for the presence of HLA-B27 [8] but it was reported positive in a few case reports of PD [14, 21]. Moreover, a recent case has been reported of HLA-B27-positive reactive arthritis developed in a patient following intravesical instillation of BCG [22]. In a systematic review, all reactive arthritis cases developing after BCG immunotherapy for bladder cancer 60 % of patients were HLA-B27 positive [23]. It has to be noted that the epidemiology of HLA-B27 varies based on ethnic background for patients in the same country [24], so the interpretation of these results should consider the ethnic background of the patients. Furthermore, the relationship of HLA-B27 to PD needs further research. Genotyping for HLA-B27 was not included in the initial investigations for our patients reported here. The prevalence of HLA-B27 is not expected to be high in Saudi Arabia as in other western countries. Therefore, we did not recommend using HLA-B27 as a diagnostic tool for patients with possible PD. It was suggested even not to be used as a diagnostic tool for patients with acute reactive arthritis [25]. The presence of HLA-B27 however, represents a risk factor for severity for patients with reactive arthritis [26–28].
Ruling out other rheumatological diseases is an essential step for proper diagnosis of PD, particularly crystal-induced arthritis and drug-induced systemic lupus erythematosus from anti-TB drugs. RF and ACPA were negative in four out of seven patients tested in our cohort as well as in other case reports [1, 8, 14, 15, 19].
TB is a common disease in Saudi Arabia and several other places in the world. PD is a MSK manifestation related to TB and it is an entity that is usually underdiagnosed. It is presumed, based on the observation that was outlined in this study, that PD is more common than expected. Our cohort of patients was obtained from rheumatology clinics with significant and serious joint symptoms for patients who have had access to such tertiary care rheumatology services. More accurate estimation of this disease requires a data registry for all MSK manifestations of TB particularly in TB treatment centers. Several clinical presentations of PD were described in this study either prior to initiation of anti-TB, during treatment or after completion of anti-TB course of therapy. PD may affect small joints of the hands, particularly MCPs. Resolution of arthritis with adequate anti-TB therapy is the expected outcome. It is hoped that clinicians dealing with patients with TB be aware of various MSK manifestations of TB particularly PD. This would help greatly the quality of care delivered to patients suffering from such a common disease in several societies.
References
Ideguchi H, Ohno S, Takase K, Tsukahara T, Kaneko T, Ishigatsubo Y (2009) A case of Poncet’s disease (tuberculous rheumatism). Rheumatol Int 29(9):1097–1099, Epub 2008/12/04
Dall L, Long L, Stanford J (1989) Poncet’s disease: tuberculous rheumatism. Rev Infect Dis 11(1):105–107, Epub 1989/01/01
Hameed K, Karim M, Islam N, Gibson T (1993) The diagnosis of Poncet’s disease. Br J Rheumatol 32(9):824–826, Epub 1993/09/01
Malaviya AN, Kotwal PP (2003) Arthritis associated with tuberculosis. Best Pract Res Clin Rheumatol 17(2):319–343, Epub 2003/06/06
Khoury MI (1989) Does reactive arthritis to tuberculosis (Poncet’s disease) exist? J Rheumatol 16:1162–1164
Summers SD (1980) Does Poncets disease exist. Rheum Rehab 19:49–50
Keat A (1993) TB or not TB?: that is the question. Br J Rheumatol 32:769–771
Kroot EJ, Hazes JM, Colin EM, Dolhain RJ (2007) Poncet’s disease: reactive arthritis accompanying tuberculosis. Two case reports and a review of the literature. Rheumatol (Oxford) 46(3):484–489, Epub 2006/08/29
Gleason JA, McNabb SJ, Abduljadayel N, Abouzeid MS, Memish ZA (2012) Tuberculosis trends in the Kingdom of Saudi Arabia, 2005 to 2009. Ann Epidemiol 22(4):264–269, Epub 2012/03/01
Al-Hajoj SA (2010) Tuberculosis in Saudi Arabia: can we change the way we deal with the disease? J Infect Public Health 3(1):17–24, Epub 2010/08/13
Isaacs AJ, Sturrock RD (1974) Poncet’s disease—fact or fiction? A re-appraisal of tuberculous rheumatism. Tubercle 55(2):135–142, Epub 1974/06/01
Simcock DE, Mukherjee D, Gendi NS (2004) Poncet’s disease—a novel cause of non-compliance with anti-tuberculous drugs. Respir Med 98(8):795–797, Epub 2004/08/12
Al-Otaibi F, El Hazmi MM (2010) Extra-pulmonary tuberculosis in Saudi Arabia. Indian J Pathol Microbiol 53(2):227–231, Epub 2010/06/17
Valleala H, Tuuminen T, Repo H, Eklund KK, Leirisalo-Repo M (2009) A case of Poncet disease diagnosed with interferon-gamma-release assays. Nat Rev Rheumatol 5(11):643–647, Epub 2009/10/30
Singhania P, Banerjee A, Singhania B, Banerjee I, Kumar V, Maitra S (2011) Poncet’s disease or tuberculous rheumatism. Ceylon Med J 56(1):43–44, Epub 2011/05/06
Toivanen P, Toivanen A (1999) Two forms of reactive arthritis? Ann Rheum Dis 58(12):737–741, Epub 1999/12/01
Kowalski M, Seitz M (1999) Tuberculosis manifestations in the musculoskeletal system exemplified by Poncet’s disease. Schweiz Med Wochenschr 129(47):1839–1842, Tuberkulose Manifestationen am Bewegungsapparat, diskutiert am Beispiel der “Poncet-Krankheit”
Garg S, Malaviya AN, Kapoor S, Rawat R, Agarwal D, Sharma A (2011) Acute inflammatory ankle arthritis in northern India–Lofgren’s syndrome or Poncet’s disease? J Assoc Physicians India 59:87–90, Epub 2011/07/15
Tian J, Chen JW, Gao JS, Li F, Xie X (1952) A case of Poncet’s disease: retroperitoneal tuberculous lymphadenitis and polyarthritis. Chin Med J (Engl) 123(14), Epub 2010/09/08
Schweitzer LC, Lipnharski F, Prezzi SH (2011) Poncet’s arthritis: case report. Rev Bras Reumatol 51(4):388–390, Epub 2011/07/23
Ozgul A, Baylan O, Taskaynatan MA, Kalyon TA (2005) Poncet’s disease (tuberculous rheumatism): two case reports and review of the literature. Int J Tuberc Lung Dis 9(7):822–824, Epub 2005/07/15
Macia Villa C, Sifuentes Giraldo W, Boteanu A, Gonzalez Lanza M, Bachiller Corral J (2012) Reactive arthritis after the intravesical instillation of BCG. Reumatologia clinica (in press). Artritis reactiva secundaria a la instilacion intravesical de bacilo de Calmette-Guerin
Tinazzi E, Ficarra V, Simeoni S, Artibani W, Lunardi C (2006) Reactive arthritis following BCG immunotherapy for urinary bladder carcinoma: a systematic review. Rheumatol Int 26(6):481–488, Epub 2005/10/13
Skare TL, Bortoluzzo AB, Goncalves CR, da Silva JA B, Ximenes AC, Bertolo MB et al (2012) Ethnic influence in clinical and functional measures of Brazilian patients with spondyloarthritis. J Rheumatol 39(1):141–147, Epub 2011/11/03
Hannu T (2011) Reactive arthritis. Best Pract Res Clin Rheumatol 25(3):347–357, Epub 2011/11/22
Leirisalo M, Skylv G, Kousa M, Voipio-Pulkki LM, Suoranta H, Nissila M et al (1982) Followup study on patients with Reiter’s disease and reactive arthritis, with special reference to HLA-B27. Arthritis Rheum 25(3):249–259, Epub 1982/03/01
Leirisalo-Repo M, Suoranta H (1988) Ten-year follow-up study of patients with Yersinia arthritis. Arthritis Rheum 31(4):533–537, Epub 1988/04/01
Leirisalo-Repo M, Helenius P, Hannu T, Lehtinen A, Kreula J, Taavitsainen M et al (1997) Long-term prognosis of reactive salmonella arthritis. Ann Rheum Dis 56(9):516–520, Epub 1997/11/26
Acknowledgments
The study was supported and funded by Alzaidi’s Chair of Research in Rheumatic Diseases, Umm Alqura University. The authors would like to acknowledge Dr Khatijah Bawazeer for her help provided during the manuscript preparation and Dr Alyaa Khodarwardi for her help provided in the data collection.
Disclosures
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Abdulaziz, S., Almoallim, H., Ibrahim, A. et al. Poncet’s disease (reactive arthritis associated with tuberculosis): retrospective case series and review of literature. Clin Rheumatol 31, 1521–1528 (2012). https://doi.org/10.1007/s10067-012-2042-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-012-2042-0