Abstract
We retrospectively examined the effect of combination therapy with prednisolone and cyclosporin-A (CSA) on the findings of pulmonary function tests (PFTs) and chest high-resolution computed tomography (HRCTs) scans in patients with dermatomyositis (DM) and acute/subacute interstitial pneumonia (A/SIP). We also examined whether CSA therapy improved PFT and chest HRCT findings. DM patients (n = 14) with A/SIP were treated with 1 mg/kg/day prednisolone and 4 mg/kg/day CSA within 4.4 days (range, 1–12 days) from diagnosis. The trough level (C0) and 2-h post-dose blood concentration (C2) of CSA were measured. PFTs and HRCT scans were performed before and 1 year after treatment. The total ground-glass opacity area was calculated with the HRCT findings and used as the CT score. Combination prednisolone and CSA therapy improved the TLC%, VC%, FVC%, EFV1.0%, and CT score (P = 0.027, 0.003, 0.002, 0.001, and 0.001, respectively). The C0 level was 178.8 ng/ml (range, 71–456 ng/ml), and the C2 level was 1,336.6 ng/ml (range, 814–2,873 ng/ml). Therapeutic changes in FVC%, FEV1.0%, and DLCO% were correlated with the C2 CSA level (P = 0.047, 0.025, and 0.035, respectively). However, the PFT results and CT scan scores did not correlate with the daily dose or C0 level of CSA. Improvements in the CT score were correlated with time from IP diagnosis to CSA initiation (P = 0.014). Early intervention with prednisolone and CSA combination therapy and tight control of the daily CSA dose by monitoring the C2 level improved PFT and chest HRCT findings in DM–A/SIP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dermatomyositis (DM) is a chronic inflammatory disorder that mainly involves muscle and skin lesions, such as the Gottron's sign and heliotrope rash [1–3]. Interstitial pneumonia (IP) is a common complication of dermatomyositis (DM), causing increased morbidity and mortality [4, 5]. On the basis of the clinical course, DM patients with IP are classified into one of two groups: DM with acute/subacute IP (A/SIP) and DM with chronic IP (CIP). DM–CIP responds well to treatment with corticosteroids and has a good prognosis, whereas DM–A/SIP progresses rapidly, and the prognosis is poor. An aggressive combination therapy with corticosteroids and immunosuppressive drugs such as cyclosporin-A (CSA) and intravenous pulse cyclophosphamide (IVCY) needs to be performed in corticosteroid-resistant DM–A/SIP.
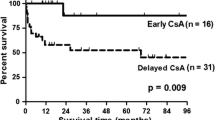
Recent studies have reported the efficacy of combination therapy with corticosteroids and CSA for DM–A/SIP. The survival rate in response to combination therapy ranges from 42% to 69%, and the prognosis remains poor [6–11]. We previously reported that an early intervention with corticosteroids and 4 mg/kg/day of CSA (within 11 days, 1–22) and 2-h post-dose blood concentration (C2) monitoring improved the prognosis of DM–A/SIP (survival rate, 89%) [12]. However, it remains unclear whether the combination therapy with steroids and CSA improves the findings of pulmonary function tests (PFTs) and chest high-resolution computed tomography (HRCT) scans.
In this study, we evaluate the therapeutic changes of PFTs and chest HRCT scan findings before and 1 year after the combination therapy with corticosteroids and CSA and examine whether the therapeutic strategy involving CSA relates to the improvement of PFTs and chest HRCT scan findings.
Materials and methods
Patients
The subjects were 14 DM–A/SIP patients who were admitted to Osaka Medical College Hospital between January 2002 and January 2009. DM was diagnosed according to the criteria of Bohan and Peter [13, 14]. Clinically amyopathic DM (C-ADM) was diagnosed according to the criteria proposed by Sontheimer [15] and Gerami et al [16]. Patients with typical dermatomyositis-related exanthema who met three or more of the following four items were regarded as having definite DM, and those meeting two or more, as having probable DM: weakness of the proximal limb muscles, myositis verified on muscle biopsy, an increase in the serum myogenic enzyme level, and myogenic changes on electromyograms. IP was diagnosed by HRCT of the chest. Typical images of IP in DM show ground-glass opacity (GGO), consolidation, traction bronchiectasis, linear opacity, and less marked honeycomb lungs. DM patients with A/SIP experience an acute onset of respiratory symptoms and a rapid progressive course of within 3 months with respect to respiratory symptoms and laboratory findings such as those on chest X-rays, chest HRCT scans, PFTs, and arterial blood gas analyses. Four patients underwent bronchoalveolar lavage (BAL) and lung biopsy. After the exclusion of infections based on clinical and laboratory findings, all patients were treated with a combination therapy of corticosteroids and CSA and with C2 monitoring in the early stage of A/SIP. One patient died due to the rapid exacerbation of A/SIP on the 53rd day after admission. Of 13 patients who survived for 1 year after the diagnosis of DM–A/SIP, respiratory function tests and chest HRCT were performed before and 1 year after therapy in all patients (10 women, 3 men).
Pulmonary function test
Static and dynamic lung volumes were measured by spirometry (SYSTEM21; Minato Medical Science, Osaka, Japan). The total lung capacity (TLC) and vital capacity (VC) were determined by the N2 washout method. The diffusion capacity of the lung for carbon monoxide (DLCO) was determined by the single-breath method. The results of PFT were expressed as a percentage of the predicted.
HRCT scoring
HRCT was performed using a 64-detector row CT Aquilion multiscanner (Toshiba Corporation Medical System, Tokyo, Japan). Slice thickness was 1.0–1.5 mm at every 10 mm, which included the entire lung. Typical images of IP in DM show GGO, consolidation, traction bronchiectasis, linear opacity, and less marked honeycomb lungs [17]. GGO showed more significant improvement than other findings in DM–IP, and the improvement of GGO correlated with the improvement of clinical manifestations and PFTs [18]. Therefore, GGO was scored to assess HRCT findings, as previously described [19]. Briefly, limited 3-CT levels were pre-selected: mid-arch of the aorta, tracheal carina, and 1 cm above the top of the right diaphragm. Each lobe (right upper, middle, and lower and left upper and lower lobes) of the lung was scored at the three sites on a scale of 0–5, and they were summed as the total CT score.
Treatment
All patients were treated initially with 1 mg/kg/day of prednisolone plus 4 mg/kg/day of CSA. All patients in this study started treatment with oral CSA. When it was difficult to administer CSA orally because of ventilation, liquid CSA was administered by a tube. CSA was administered within 14 days from the diagnosis of A/SIP. The area under the blood concentration–time curve (AUC) of CSA was found to be closely correlated with clinical effects. Nagai et al. reported that AUC is correlated with C2 in DM–A/SIP patients [20]. The dose of CSA was controlled with C2 monitoring to maintain the serum level at above 1,000 ng/ml in all patients, as previously described [12]. When IP progressed despite the combination of corticosteroids and CSA, methylprednisolone (MPDN) (1,000 mg × 3 days) and/or IVCY (200–500 mg/day) therapy was added. Trimethoprim–sulfamethoxazole was routinely given to all patients to prevent Pneumocystis jirovecii pneumonia. The response to treatment and clinical course of IP were assessed using ATS guidelines [21].
Infection surveillance
For the surveillance of infection, complete blood cell counts, the serum C-reactive protein level, and serum levels of β-d-glucan and C7-HRP were measured, as previously described [12].
Statistical analysis
The difference in baseline clinical and laboratory findings between patients undergoing and not undergoing the additional treatment by MPDN and/or IVCY was evaluated using Fisher's exact test or the Mann–Whitney U test. Wilcoxon's rank sum test was used to assess both the CT score and PFT results before and after CSA treatment. Spearman's rank correlation was used to assess the association between the changes in respiratory functions, CT score, or serum creatinine (Cr) level vs the time from the diagnosis of IP to the initiation of the CSA treatment, CSA dose, CSA C2 level, or CSA trough (C0) level.
Results
Patient profiles and outcomes
The clinical characteristics are summarized in Table 1. Fourteen patients (11 women, 3 men) with a mean age of 53.6 years (43–68 years) were included. Six had definite DM, and 8 had probable DM. The dyspnea scores based on the Hugh-Jones classification were level II in 3 patients, level III in 6 patients, and level IV in 5 patients. Nine of the 14 (64%) patients had C-ADM with a CK/LDH ratio of less than 2. Five of the 14 (36%) were positive for anti-Jo-1 antibodies. In all 4 patients who underwent BAL, the percentage of lymphocytes was high, and the CD8/CD4 ratio was increased. Lung biopsy was performed in 4 patients, and it was open lung biopsy in 3, all of whom presented findings of cellular non-specific interstitial pneumonia. Transbronchial lung biopsy was performed in the remaining 1 patient, yielding only very non-specific findings. Regarding the timing of complications of DM and IP, 3 cases had preceding IP, and the others were simultaneous. Pneumomediastinum was present in 3 (21%) patients. The therapies, response to therapies, and outcomes are summarized in Table 2. The average time from the diagnosis of IP to the initiation of CSA treatment was 4.4 days (1–12). The dose, the C0 level, and the C2 level were 208.9 mg/day (175–275), 178.8 ng/ml (71–456), and 1,336.6 ng/ml (814–2,873), respectively. Seven patients were treated with MPDN and/or IVCY in addition to the combination therapy of prednisolone and CSA. In the ADM group, the proportion of patients who underwent additional treatment was higher than in the non-ADM group (64.3% vs. 35.7%, respectively). There was no other significant difference in the clinical characteristics and respiratory function at the start of treatment between patients undergoing and not undergoing the additional treatment (data not shown). One patient (case 3) died due to the rapid exacerbation of A/SIP on the 53rd day after admission. Two patients (cases 3 and 8) required admission to the intensive care unit/ventilation. In the response to therapy, 10 showed an improved response; 3, a stable response, and 1 failed to respond to therapy. There were no differences in the response to therapy between the patients receiving and not receiving additional treatment such as MPDN and/or IVCY.
The improvement of PFT and chest CT score
The PFT and chest CT score before and 1 year after the combination therapy with prednisolone and CSA are shown in Fig. 1. TLC%, VC%, FVC%, and FEV1.0% before the therapy were 74.3% (range, 48.4–105.3), 74.0% (range, 51.3–100.5), 72.8% (range, 50.5–98.1), and 72.3% (range, 50.9–97.6), respectively. The DLCO% was markedly decreased at 44.9% (range, 30.2–67.5), and the CT score was 10.0 (range, 6–18). The PFT and CT scores improved 1 year after the therapy. The TLC%, VC%, FVC%, FEV1.0%, and CT score were significantly increased after the combination therapy (P = 0.027, 0.003, 0.002, 0.001, and 0.001, respectively), but DLCO% was not.
Change in pulmonary function tests and CT scan scores before and 1 year after combination therapy in each patient. The difference was significant (P < 0.05) by the Wilcoxon signed rank test. TLC total lung capacity, VC vital capacity, FVC forced vital capacity, FEV1.0 forced expiratory volume in 1.0 s, DLCO carbon monoxide diffusing capacity
The changes of PFT and CT score correlate with C2 level of CSA
We examined whether the improvement in the PFT and CT score were affected by the following factors: daily dose, C0 and C2 levels of CSA, and time from the diagnosis of IP to the initiation of CSA. The C2 level of CSA correlated with the therapeutic changes in FVC%, FEV1.0%, and DLCO% significantly (P = 0.047, 0.025, and 0.035, respectively), but not the changes in TLC%, VC%, and CT score (Fig. 2). The changes in the PFT and CT score revealed no correlation with the C0 level (Fig. 3) or the daily dose of CSA (data not shown). The time from the diagnosis of IP to the initiation of CSA correlated with the therapeutic changes in the CT score (P = 0.014) (Fig. 4).
Adverse events
The mean serum Cr level increased by 0.35 mg/dl (range, −0.09 to 0.72) 1 year after the therapy, but the change in serum Cr level was not correlated with the C0 and C2 levels of CSA (data not shown). The incidence of other side effects was not increased in 3 patients with C0 levels above 200 ng/ml. Diabetes mellitus was shown in 2 patients (cases 11 and 12), 1 patient treated with regular insulin at 27 U/day and the other patient treated with miglitol at 150 mg/day. Infections were identified in 5 out of the 13 patients, were caused by herpes virus (cases 2 and 7), bacteria (cases 6 and 8), or trichophytosis unguium (case 1) infection, and were successfully treated with acyclovir, antimicrobial agents, or fluconazole. Nine out of 14 patients had positive C7-HRP tests without clinical symptoms and were successfully treated with ganciclovir.
Discussion
Studies on the efficacy of combination therapy with corticosteroids and CSA for DM–A/SIP have been reported [6–11]. However, there are no established guidelines for this combination therapy. Recently, we reported the efficacy of early intervention with combination therapy and C2 monitoring of CSA for DM–A/SIP and suggested that the dose of CSA and the CSA administration time from diagnosis of IP were involved in the prognosis of DM–A/SIP [12]. In this study, we demonstrate that early intervention with prednisolone and CSA improved the findings of PFTs and chest HRCT scans and that the C2 level of CSA is significantly correlated with the improvement of PFT findings in DM–A/SIP. This suggests that tight control of the CSA dosage by C2 monitoring is needed to treat DM–A/SIP patients.
The results of PFTs and chest HRCT scans were improved by immunosuppressive drugs in IP patients with myositis. Yamasaki et al. reported that VC% and chest HRCT scan findings were improved by the combination therapy with corticosteroids and IVCY in 17 PM/DM–IP patients (3 with PM, 9 with DM, and 5 with ADM) during a mean follow-up of 32 months [22]. Arakawa et al. reported that chest HRCT scans were improved by the treatment in 14 nonspecific IP patients with associated PM/DM (3 with PM and 11 with DM) during a mean follow-up of 27.6 months [18]. The improvement in FVC% was positively correlated with the improvement of chest HRCT scan scores. These reports included PM–IP patients and chronic DM–IP patients with good prognoses, and it remains unclear whether immunosuppressive therapy improves the findings of PFTs and chest HRCT scans in DM–A/SIP patients who have a poor prognosis. The present study demonstrates that the combination therapy of corticosteroids and CSA improves the findings of PFT and chest HRCT as well as the prognosis in DM–A/SIP.
The daily CSA dose for the treatment of DM–A/SIP ranges from 100 to 300 mg/day [8, 10, 11, 23]. The absorption of CSA differs between individuals, and the C0 and C2 levels of CSA are monitored to determine the daily CSA dose. However, little attention has been given in this regard to the therapeutic dose of CSA in DM–A/SIP. In our study, the C2 level, but not the C0 level, was correlated with the improvement of PFT (Fig. 2). In organ transplantation, recent studies have indicated that the C2 level must reach approximately 1,000 ng/ml or more to achieve maximal immunosuppressive effect [24, 25]. The necessary C2 level of CSA for the treatment of DM–A/SIP remains unclear, and further studies are needed to determine this.
The time from diagnosis of A/SIP to initiation of CSA treatment was also crucial for the treatment of DM–A/SIP. CSA was effective and improved the prognosis in the treatment of DM–IP when given early during the course of IP [8, 12]. Yamasaki et al. reported that earlier intervention of corticosteroids and IVCY after diagnosis more markedly improved VC% in PM/DM–IP patients [22]. In this study, there was a positive correlation between the time from diagnosis of A/SIP to initiation of the combination therapy and the improvement in the CT score. However, no significant correlation was observed between the time interval from A/SIP diagnosis to the therapy initiation and the improvement of respiratory function. This is presumably because all patients were started on treatment as early as within 2 weeks after the diagnosis of A/SIP.
The major adverse effects of CSA were renal damage, hypertension, diabetes mellitus, and liver damage. The incidence of side effects was significantly increased when the C0 level exceeded 200 ng/ml [26]. In this study the mean C0 level was 178.8 ng/ml (range, 71–456 ng/ml), when the mean C2 level was 1,336.6 ng/ml (range, 814–2,873 ng/ml). There was no significant relation between the change in Cr level and C0 or C2 level of CSA. Diabetes mellitus was observed in 2 patients; it is unclear whether this was due to Cy-A or corticosteroids. Viral infections, including herpes virus and cytomegalovirus, and bacterial infections were observed, but were treatable with acyclovir, ganciclovir, and antimicrobial agents. Thus, CSA could be safely used up to the above level of C0 and C2 for DM–A/SIP in this study, but repeated infection surveillance is needed.
We demonstrate that the combination of corticosteroids and CSA improved the findings of PFTs and chest HRCT scans in DM–A/SIP. Moreover, it was important to control the daily dose of CSA tightly by C2 monitoring alongside the early therapeutic intervention.
References
Hirakata M, Nagai S (2000) Interstitial lung disease in polymyositis and dermatomyositis. Curr Opin Rheumatol 12:501–508
Marie I, Hachulla E, Cherin P et al (2002) Interstitial lung disease in polymyositis and dermatomyositis. Arthritis Rheum 47:614–622
American Thoracic Society; European Respiratory Society (2002) American Thoracic Society/European Respiratory Society International Multidisciplinary Consensus Classification of the Idiopathic Interstitial Pneumonias. This joint statement of the American Thoracic Society (ATS), and the European Respiratory Society (ERS) was adopted by the ATS board of directors, June 2001 and by the ERS Executive Committee, June 2001. Am J Respir Crit Care Med 165:277–304
Maugars YM, Berthelot JM, Abbas AA, Mussini JM, Nguyen JM, Prost AM (1996) Long-term prognosis of 69 patients with dermatomyositis or polymyositis. Clin Exp Rheumatol 14:263–274
Benbassat J, Gefel D, Larholt K, Sukenik S, Morgenstern V, Zlotnick A (1985) Prognostic factors in polymyositis/dermatomyositis. A computer-assisted analysis of ninety-two cases. Arthritis Rheum 28:249–255
Kuroda H, Morinaga H, Satoh C, Miyake A, Sunami K (2003) Clinical study of 10 cases of acute or subacute interstitial pneumonia associated with dermatomyositis. Mod Rheumatol 13:313–318
Euwer RL, Sontheimer RD (1993) Amyopathic dermatomyositis: a review. J Invest Dermatol 100:124S–127S
Nagasaka K, Harigai M, Tateishi M et al (2003) Efficacy of combination treatment with cyclosporin A and corticosteroids for acute interstitial pneumonitis associated with dermatomyositis. Mod Rheumatol 13:231–238
Kameda H, Nagasawa H, Ogawa H et al (2005) Combination therapy with corticosteroids, cyclosporin A, and intravenous pulse cyclophosphamide for acute/subacute interstitial pneumonia in patients with dermatomyositis. J Rheumatol 32:1719–1726
Maeda K, Kimura R, Komuta K, Igarashi T (1997) Cyclosporine treatment for polymyositis/dermatomyositis: is it possible to rescue the deteriorating cases with interstitial pneumonitis? Scand J Rheumatol 26:24–29
Ozawa Y, Kurosaka D, Yokoyama T, Tajima N (2000) Therapeutic efficacy of cyclosporin A in four cases of amyopathic dermatomyositis with rapidly progressive interstitial pneumonia. Ryumachi 40:798–809 (in Japanease)
Kotani T, Makino S, Takeuchi T et al (2008) Early intervention with corticosteroids and cyclosporin A and 2-hour postdose blood concentration monitoring improves the prognosis of acute/subacute interstitial pneumonia in dermatomyositis. J Rheumatol 35:254–259
Bohan A, Peter JB (1975) Polymyositis and dermatomyositis (first of two parts). N Engl J Med 292:344–347
Bohan A, Peter JB (1975) Polymyositis and dermatomyositis (second of two parts). N Engl J Med 292:403–407
Sontheimer RD (2002) Dermatomyositis: an overview of recent progress with emphasis on dermatologic aspects. Dermatol Clin 20:387–408
Gerami P, Schope JM, McDonald L, Walling HW, Sontheimer RD (2006) A systematic review of adult-onset clinically amyopathic dermatomyositis (dermatomyositis sine myositis): a missing link within the spectrum of the idiopathic inflammatory myopathies. J Am Acad Dermatol 54:597–613
Hayashi S, Tanaka M, Kobayashi H et al (2008) High-resolution computed tomography characterization of interstitial lung diseases in polymyositis/dermatomyositis. J Rheumatol 35:260–269
Arakawa H, Yamada H, Kurihara Y et al (2003) Nonspecific interstitial pneumonia associated with polymyositis and dermatomyositis. Chest 123:1096–1103
Kazerooni EA, Martinez FJ, Flint A et al (1997) Thin-section CT obtained at 10-mm increments versus limited three-level thin-section CT for idiopathic pulmonary fibrosis: correlation with pathologic scoring. Am J Roentgenol 169:977–983
Nagai K, Takeuchi T, Kotani T et al (2011) Therapeutic drug monitoring of cyclosporine microemulsion in interstitial pneumonia with dermatomyositis. Mod Rheumatol 21:32–36
Society AT (2000) Idiopathic pulmonary fibrosis: diagnosis and treatment. International consensus statement. American Thoracic Society (ATS), and the European Respiratory Society (ERS). Am J Respir Crit Care Med 161:646–664
Yamasaki Y, Yamada H, Yamasaki M et al (2007) Intravenous cyclophosphamide therapy for progressive interstitial pneumonia in patients with polymyositis/dermatomyositis. Rheumatology 46:124–130
Nawata Y, Kurasawa K, Takabayashi K et al (1999) Corticosteroid resistant interstitial pneumonitis in dermatomyositis/polymyositis: prediction and treatment with cyclosporine. J Rheumatol 26:1527–1533
Levy G, Thervet E, Lake J, Uchida K, Consensus on Neoral C(2): Expert Review in Transplantation (CONCERT) Group (2002) Patient management by Neoral C(2) monitoring: an international consensus statement. Transplantation 73:S12–S18
Levy GA (2001) Neoral C(2) in liver transplant recipients. Transplant Proc 33:3089–3091
Min DI, Perry PJ, Chen HY, Hunsicker LG (1998) Cyclosporine trough concentrations in predicting allograft rejection and renal toxicity up to 12 months after renal transplantation. Pharmacotherapy 18:282–287
Funding
This study was supported in part by Grant-in-Aid for Scientific Research (20590588).
Disclosures
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kotani, T., Takeuchi, T., Makino, S. et al. Combination with corticosteroids and cyclosporin-A improves pulmonary function test results and chest HRCT findings in dermatomyositis patients with acute/subacute interstitial pneumonia. Clin Rheumatol 30, 1021–1028 (2011). https://doi.org/10.1007/s10067-011-1713-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-011-1713-6