Abstract
As a class, tumor necrosis factor (TNF)-α inhibitors have provided clinicians significant control over chronic inflammatory diseases. With their widespread use has come the emergence of new side effects such as the reactivation of latent infections. One such infection that may reactivate is the hepatitis B virus (HBV). It is currently unknown if HBV reactivation is a class effect or attributable to a particular TNF-α inhibitor. To answer this question, a comprehensive literature review to identify trends in related cases was performed. A systemic literature review was performed using the PubMed and Medline databases (1996 to January 2010) searching for the index term “Hepatitis B” combined with the terms “tumor necrosis factor,” “TNF-α inhibitors,” “etanercept,” “adalimumab,” “certolizumab,” and “golimumab.” All relevant articles in English were reviewed, and secondary references of interest were also retrieved. Thirty-five cases with hepatitis B surface antigen (HBsAg) positivity known prior to initiation of TNF-α inhibitors were identified. Infliximab was used in 17 cases, etanercept in 12 cases, and adalimumab in 6 cases. All six cases of clinically symptomatic hepatitis were associated with infliximab therapy. Infliximab was associated with the most cases of greater than 2-fold increase in alanine aminotransferase (six of nine cases) and greater than 1,000-fold increase in HBV DNA load (three of four). The two deaths reported occurred with infliximab therapy. Potential mechanisms of action for the reported observations include differences in molecular design, route of administration, and potency in clearing TNF-α. In patients with a positive HBsAg prior to starting a TNF-α inhibitor, infliximab has the most reported cases associated with HBV reactivation. While such reactivation may be due to a variety of reasons, clinicians prescribing TNF-α inhibitors to HBsAg-positive patients should consider prophylactic antiviral therapy and close monitoring for any clinical or serological evidence of hepatitis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tumor necrosis factor α (TNF-α) inhibitors are an evolving class of medication that since their introduction over a decade ago have revolutionized the treatment of chronic inflammatory conditions. Whether used as monotherapy or in conjunction with disease-modifying agents such as methotrexate or azathioprine, TNF-α inhibitors give clinicians a level of control over rheumatologic, dermatologic, and gastrointestinal illnesses once previously unattainable [1]. Though each TNF-α inhibitor has a unique molecular construct, they all have as their specific target the critical proinflammatory cytokine TNF-α [1, 2]. To date, five TNF-α inhibitors have been approved by the United States Food and Drug Administration (FDA) for treatment of rheumatoid arthritis: infliximab (Remicade), etanercept (Enbrel), adalimumab (Humira), certolizumab (Cimzia), and golimumab (Simponi). Several of these agents are also FDA approved for treatment of ankylosing spondylitis as well as nonrheumatologic diseases such as Crohn's disease and psoriasis. In all of these diseases, the aberrant production of TNF-α is often an initiator as well as the perpetuator of these conditions [1].
A serious side effect associated with the use of TNF-α inhibitors has been the reactivation of latent infections. As TNF-α often plays a key role in both the initial clearance and then containment of such infections, neutralization of TNF-α has both direct and indirect consequences. A direct consequence of TNF-α inhibition is impaired granuloma formation due to suppressed cell-mediated immunity. This impairment has been associated with reactivation of latent infections with both Mycobacterium tuberculosis (TB) and histoplasmosis [1, 2]. An indirect consequence of TNF-α inhibition is the creation of a cytokine imbalance with interferon (IFN). While TNF-α is not a dominant cytokine in the initial host response, it acts synergistically with IFN-gamma (IFN-γ) to eradicate or contain infection by TB and histoplasmosis [1]. IFN-γ without TNF-α lacks the potency to successfully contain the initial infection by such organisms.
As with TB and histoplasma, hepatitis B virus (HBV) can avoid initial eradication and enter a latent state, reactivating when the immune system is depressed. Affecting up to 400 million people worldwide [3], both the acute eradication and the chronic containment of the virus are dependent on the production of TNF-α by various cells of the immune system. Emerging evidence suggests that neutralization of TNF-α may foster an environment favorable for HBV reactivation [4]. While all TNF-α inhibitors carry warnings about the risk of HBV reactivation [5–9], the available literature suggests that this risk may not be the same for each medication. The purpose of this article was to review the published literature for cases where chronic HBV infection was known prior to initiation of a TNF-α inhibitor, regardless of the chronic inflammatory condition for which it was used to treat and identify whether HBV reactivation was attributable to a class effect or a specific medication in the class.
Methods
A review of the published English literature between 1996 up to January 2010 was performed using PubMed (http://www.ncbi.nlm.nih.gov/PubMed) and the Medline database through Ovid (http://gateway.ovid.com). The search screened articles for the keywords “tumor necrosis factor” and “hepatitis B” as well as the currently approved FDA TNF-α inhibitors “infliximab,” “etanercept,” “adalimumab,” certolizumab,” and “golimumab.” Articles were selected if a review of the title and/or abstract suggested it discussed the interaction of a TNF-α inhibitor in patients with hepatitis B infection. Additional articles of interest were selected from the bibliographies of articles retrieved using this search.
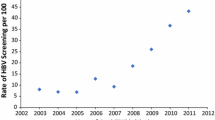
All cases included in this review were reported as having a positive hepatitis B surface antigen (HBsAg) prior to initiation of a TNF-α inhibitor. All cases also provided either reasonable descriptions of their chronic inflammatory condition or the authors stated they satisfied currently accepted classification criteria. In three instances, two articles described the same case(s) [10–15]. Such cases were counted only once. In the case series by Wendling et al. in 2009, the cases were described as having “latent HBV infection” [10], but the HBsAg status was not reported. Since one of the cases in this series had been published in 2005 and provided the HBV antigen/antibody profile [11], all the cases in the 2009 series were treated as HBsAg positive. A case described by Roux et al. [16] in 2006 with a diagnosis of “spondyloarthropathy” was considered in the group with ankylosing spondylitis in this review. One case described in the series by Cansu et al. [17] in 2008 was not included as they were coinfected with HCV. Based on these criteria, 23 articles describing 35 cases were identified between 2003 and 2009 [10–32].
Results
The demographic information of the 35 cases with known HBsAg positivity prior to treatment with TNF-α inhibitors is summarized in Table 1. The mean reported disease duration before a TNF-α inhibitor was used was 9 years for cases with rheumatoid arthritis, 7 years for ankylosing spondylitis, and 17 years for Crohn's disease. Prior to starting a TNF-α inhibitor, 12 (75%) of the 16 cases with rheumatoid arthritis had active articular disease. The six cases of Crohn's disease all described active intestinal symptoms with four of these (66.7%) reporting fistulizing disease. Three (25%) of the 12 cases with ankylosing spondylitis reported active axial and/or peripheral disease. Twenty-one (60%) of the cases in this review were concomitantly prescribed disease-modifying medications such as methotrexate (10 cases), sulfasalazine (8 cases), glucocorticoids (7 cases), or azathioprine (4 cases). Ten (47.6%) of the 21 cases were on at least two disease-modifying medications when therapy with a TNF-α inhibitor was started. Antecedant knowledge about HBV infection was known for an average of 7.3 years (±8.4 years) prior to initiation of a TNF-α inhibitor. Five (14.3%) of 35 cases were hepatitis B envelope antigen (HBeAg) positive, Twenty-six (74.3%) were hepatitis B envelope antibody (HBeAb) positive, and 17 (48.6%) were hepatitis B core antibody (HBcAb) positive.
Seventeen of the cases (48.6%) were receiving infliximab, 12 (34.3%) etanercept,6 (17.1%) adalimumab, none certolizumab, and none golimumab, at the time of HBV reactivation. In seven cases, the first TNF-α inhibitor was later changed to a second TNF-α inhibitor. This change occurred on average around 17 months into therapy with the first TNF-α inhibitor. Infliximab was not used as a second TNF-α inhibitor in any case. Five (83.3%) of 6 cases treated with adalimumab as the first TNF-α inhibitor were prescribed concomitant disease-modifying medications. When etanercept was the initial TNF-α inhibitor prescribed, 8 (66.7%) of 12 cases were prescribed concomitant disease-modifying medications. For infliximab, 8 (47.1%) of 17 cases were prescribed concomitant disease-modifying medications.
Clinical outcomes, changes in alanine aminotransferase (ALT), and HBV DNA viral load changes associated with exposure of HBsAg-positive cases to TNF-α inhibitors is summarized in Table 2. Infliximab was the only TNF-α inhibitor associated with the 6 (of 35) cases that reported symptoms associated with HBV reactivation, such as jaundice, malaise, nausea, or weight loss. Hospitalization for symptomatic HBV reactivation after treatment with infliximab occurred in three of the four cases that reported this outcome. No cases of clinically symptomatic HBV reactivation or hospitalization were reported when etanercept or adalimumab was used. Nine cases reported sufficient data to calculate a twofold rise in ALT. While information about changes in HBV DNA load was limited, four cases reported sufficient data that showed a greater than 1,000-fold increase.
Clinical or biochemical evidence of HBV reactivation after initiation of infliximab occurred on average after the fourth dose (±4 doses), with a median onset after the third dose. The average infliximab dose associated with clinical or biochemical evidence of HBV reactivation was 4 mg/kg (±1 mg/kg). Time to reactivation after the last dose of infliximab was 38 days (±33 days), with a median of 33 days. The time to a greater than twofold increase in ALT with use of etanercept was 4–6 months [19] and with adalimumab was 13–18 months [19]. Lamivudine was the most commonly used antiviral medication either as prophylaxis or when clinical or biochemical evidence of HBV reactivation occurred. The majority of cases (11 of 18) were treated with lamivudine after initiation of a TNF-α inhibitor; however, 4 cases were treated at the start of a TNF-α inhibitor and 3 cases lamivudine was started as prophylaxis.
Liver biopsy results were reported in eight (22.9%) cases in this review. Five of these cases had the initial liver biopsy performed after treatment with a TNF-α inhibitor had been started [18, 20, 22, 31, 32]. Two of these five cases were on HBV antiviral medication at the time of initial biopsy [18, 32]. Variable degrees of portal fibrosis were reported. Two cases provided information about repeat liver biopsy [13, 18]. Repeat biopsy reported by Esteve et al. [13] was performed after 1 year after 24 months of treatment with infliximab while on adefovir therapy and showed septal fibrosis and two incomplete nodules. Repeat biopsy reported by Carroll and Bond [18] was performed after 67 months of treatment with etanercept but treated with varying courses with lamuvidine and adefovir and showed mild improvement in the grade of fibrosis.
The average length of follow-up after initiation of a TNF-α inhibitor was 17 months, with the longest reported follow-up being 96 months. Of the 35 cases in this review, 2 deaths were reported (as noted in Table 2), both of which were associated with infliximab use [13, 31]. Death from variceal bleeding was reported in one case as liver decompensation occurred despite initial improvement when infliximab was stopped [13]. The other death reported was attributed to fulminant hepatic failure [31]. Of the five cases that reported HBeAg positivity, four were exposed to infliximab and one to etanercept [10, 12, 18, 25, 31]. Two of the four HBeAg-positive cases treated with infliximab developed symptomatic reactivation of HBV [12, 31], with one case requiring hospitalization [31].
Discussion
Upon initial infection of the hepatocyte by HBV, viral replication leads to the production of surface, core, polymerase, and X proteins [33]. These foreign proteins undergo intracellular processing and are presented by the human leukocyte antigen (HLA) class I complex. Cytotoxic (CD8+) T cells bind to the HLA class I complex and, with costimulation, initiate a robust immune response [34]. A consequence of this is the production and secretion of cytokines such as IFN-γ, TNF-α, and interleukin (IL)-10 [35, 36]. While these cytokines work in concert to help control acute infection by HBV, studies over the past few years have demonstrated that genetic polymorphisms involving any of these can influence whether the immune system is able to successfully clear the virus. Of importance are genetic polymorphisms that lead to lower constitutive and inducible TNF-α secretion as these have been related to an increased risk of progression to chronic HBV infection [36, 37]. The −238GA polymorphism of the TNFA gene has been shown in multivariate analyses in white German [37], Chinese [38, 39], and Korean [40] populations to be associated with a higher risk of progressing to chronic infection with HBV. Other polymorphisms such as the −308GG haplotype [35], the −857CC haplotype [38, 39, 41], and combination −308G/−238G homozygotes [35] also have been associated with an impaired ability to clear HBV infection acutely. Lower constitutive and inducible levels of TNF-α have several important effects on the acute response of the host immune system to HBV. First, the cytokine cascade initiated and propagated by TNF-α is not as robust [42]. Second, hepatocyte clearance via Fas/Fas ligand-mediated apoptosis may not be as vigorous [43]. Last, the relative imbalance between lower levels of TNF-α and higher levels of IFN-γ impairs clearance of HBV through dampening of CD8+ T-cell responses [36, 44]. As demonstrated in an animal model, the response of CD8+ T-cells to HBV infection is more important in acute virus eradication compared with the other cells of the host immune system [45]. Selective suppression of the CD8+ T-cell response to acute HBV infection leads to persistent viral infection with a delay in HBV DNA clearance and prolonged hepatocyte destruction [45].
When HBV is not eradicated during the acute infection, it is able to establish a chronic infectious state through the establishment of a pool of viral chromosomal material, covalently closed circular DNA (cccDNA), that acts as a template for viral proteins and ultimately infectious particles [46]. The relaxed open circular, double-stranded of HBV DNA is converted in the hepatocyte nucleus into cccDNA [47]. The resulting minichromosome, colocated with host chromatin, persists at the level of several copies per hepatocyte [48, 49]. This cccDNA reservoir may persist indefinitely or become encapsulated and enveloped to spread to uninfected hepatocytes [50]. During the lifetime of the host, the immune system maintains a delicate balance between virus-specific CD8+ T cells and replicating virus. Part of this balance is dependent on the amount of TNF-α present in the liver [51]. Higher intrahepatic levels of TNF-α have been associated with increased expression of HLA class I molecules and an enhanced CD8+ T-cell response to the virus [52]. This can shift the host immune response toward destroying hepatocytes infected by the virus [52, 53]. Hepatocyte damage from replicating HBV during chronic infection triggers the release of TNF-α from Küpffer cells [54]. Under these circumstances, TNF-α can promote hepatic fibrosis (and ultimately hepatocellular carcinoma) through several mechanisms. First, TNF-α with inflammatory byproducts from chronic HBV infection can generate reactive oxygen species and toxic free radicals [53, 54]. Second, TNF-α itself can promote hepatic fibrogenesis [54]. Last, TNF-α can facilitate production and secretion of transforming growth factor-β, IL-1, and IL-6 [54]. These latter cytokines further drive hepatic inflammation and fibrogenesis.
While as a class TNF-α inhibitors have a high affinity for TNF-α, they are distinct molecules that exploit different facets of the cytokine and how it interacts with its cognate receptor to modulate its aberrant effects. Our review of the published literature suggests that infliximab, used in the treatment of more than one million people worldwide to date, is the TNF-α inhibitor associated with a higher relative risk of reactivation of HBV in HBsAg-positive patients [55]. This association can potentially be explained by the route of administration and the molecular design of infliximab. As the sole TNF-α inhibitor administered intravenously, infliximab rapidly achieves higher serum peak concentrations as compared with TNF-α inhibitors administered subcutaneously [56, 57]. Some of the efficacy of infliximab has been linked to its intravenous administration as the maximal bioavailability afforded by this route results in a “cytokine washout” through the clearance of a large amount of soluble and transmembrane TNF-α [58]. As the only chimeric protein, infliximab has consistently been shown to be the most immunogenic, with the most reported autoantibody and human antidrug antibodies formed after treatment with the medication [56, 59, 60]. While most of the TNF-α inhibitors have Fc portions incorporated in their structure, as a chimeric monoclonal antibody, infliximab can be a more potent activator of complement-dependent cytotoxicity [56, 58, 59, 61, 62]. Etanercept, a p75 TNF-α receptor fusion protein, is less able to activate complement-dependent cytotoxicity when compared with infliximab [56, 58, 59, 61, 62]. In contrast, certolizumab, an anti-TNF-α Fab' fragment conjugated to polyethylene glycol, will not trigger complement-dependent cytotoxicity [56, 61, 63, 64]. As a chimeric monoclonal antibody, infliximab can also be a more potent inducer of transmembrane TNF-α dependent apoptosis. Again, reflecting differences in structure etanercept is less potent an inducer of transmembrane TNF-α apoptosis, whereas certolizumab is unable to trigger this process [61, 62, 65]. Since transmembrane TNF-α is important in granuloma formation, it plays a role not only in the latent host defense against M. tuberculosis but also the histopathologic changes noted in Crohn's disease. The eradication of cells bearing transmembrane TNF-α by infliximab may in part explain the higher rates of TB reactivation reported as well as explain the efficacy this molecule has in reversing the histopathologic changes seen in Crohn's disease [56, 62, 66].
Despite the plausible link of HBV reactivation to treatment with infliximab, this association has limitations. First, with conclusions drawn exclusively from case reports and case series, any associations made will be influenced by publication bias. Second, the current literature does not make as clear-cut an association between HBV reactivation and treatment with infliximab. A retrospective study of 100 Thai patients treated with TNF-α inhibitors reported two cases of HBV reactivation in those who received etanercept, while no cases were documented in those who received infliximab [67]. Two recent Japanese postmarketing surveillance safety studies of infliximab and etanercept in rheumatoid arthritis patients did not report any cases of HBV reactivation [68, 69]. Both of these studies were of large cohorts (5,000 patients or more) in an area of the world where HBV is endemic [68, 69]. Third, in the United States, infliximab was the first TNF-α inhibitor approved by the FDA. The initial approval in 1998 for the treatment of fistulizing Crohn's disease was closely followed in 1999 with the approval to treat rheumatoid arthritis [70]. While etanercept was approved by the FDA in late 1998 for the treatment of rheumatoid arthritis, it did not gain a second FDA approval for adults until 2002 [71]. Adalimumab received initial FDA approval in late 2002, certolizumab in 2008, and golimumab in 2009. Receiving FDA approval the earliest would have increased the likelihood that a greater number of more seriously ill patients would have been treated with infliximab as compared with TNF-α inhibitors approved later. Fourth, a 4- to 6-year lag time appears from the FDA approval of the TNF-α inhibitor to when case reports of HBV reactivation are reported. The first case reports published in 2003 were exclusively of patients treated with infliximab [22, 23]. The first case reports of HBV reactivation with etanercept were reported in 2006 with those for adalimumab first reported in 2008 [20]. This delay creates the false impression that infliximab has been responsible for more cases of HBV reactivation when it may be solely due to it receiving approval the earliest. Fifth, in clinical practice, infliximab tends to be used more frequently with other disease-modifying medications not only to improve clinical efficacy but also to mitigate autoimmune reactions and autoantibody formation. In this review, the opposite was noted as only about half of the infliximab cases received concomitant disease-modifying agents as compared with the higher percentages seen with etanercept and adalimumab use. It is possible that in the absence of concomitant disease-modifying agents, infliximab withdrawal led to an immune reconstitution response as TNF-α bearing cells regenerated a month after the last dose [72]. Sixth, without full knowledge of the baseline HBV antigen/antibody profile and HBV DNA load prior to the initiation of a TNF-α inhibitor, it is possible that cases experiencing HBV reactivation after starting infliximab had higher viral activity. Not all case reports published information about chronic HBV serologic markers and viral loads; thus, distinguishing patients in the “immune tolerance phase” with high levels of HBe Ag and HBV DNA who would be at increased risk for reactivation from those in the “inactive carrier state” (loss of HBeAg and low to undetectable HBV DNA) was not possible [73].
Currently, the American College of Rheumatology and British Society of Rheumatology (BSR) have published guidelines regarding the use of TNF-α inhibitors in patients chronically infected with HBV [74, 75]. The American College of Rheumatology guidelines for the use of TNF-α inhibitors in rheumatologic conditions were published in 2008 and, to date, are the most comprehensive. For patients acutely infected with HBV, “biologic agents” were contraindicated per the task force [74]. For patients chronically infected with HBV, regardless of whether they were receiving antiviral therapy, “biologic agents” were contraindicated in Childs-Pugh Class B or C [74]. While no affirmative recommendation was made, use of TNF-α inhibitors in patients with chronic HBV infection and Childs-Pugh Class A was not listed as a contraindication [74]. In the July 2004 BSR guidelines for the use of TNF-α inhibitors in patients with rheumatoid arthritis, Ledingham and Deighton [75] stated that “the effects of anti-TNF therapy on patients with hepatitis B patients are contradictory” and “until more data are available, anti-TNF therapy should be avoided in patients with hepatitis B infection.” BSR guidelines for the treatment of other rheumatologic conditions such as ankylosing spondylitis and psoriatic arthritis do not offer a position regarding the use of TNF-α inhibitors in patients infected with HBV, but presumably, the same position for rheumatoid arthritis would apply [76]. For Crohn's disease, a review of published treatment guidelines from both the American Gastroenterological Association and the British Society of Gastroenterology did not provide a position on how to approach chronically infected HBV patients [77, 78].
While professional societies have provided some insight on how to address the issue of patients chronically infected with HBV who may need therapy with a TNF-α inhibitor, gaps in our knowledge remain. In the absence of clinical trials, most authors proposed the cautious administration of TNF-α inhibitors in patients with chronic HBV infection with close monitoring of HBV DNA and aspartate aminotransferase/ALT levels [16, 19, 22–25, 79]. With the current arsenal of effective medications for HBV prophylaxis as well as based on the experience from oncology patients [80], a call for screening for HBV infection prior to starting TNF-α inhibitors has been made [10, 21, 23, 69, 79–83]. Calabrese et al. [83] recommended antiviral prophylaxis for all patients who are HBsAg positive and need a disease-modifying drug (to include TNF-α inhibitors) to control their rheumatologic illness. Nathan et al. [72] made similar recommendations for prophylaxis of all HBsAg-positive patients but proposed that antiviral agents could be started 1–2 weeks prior to TNF-α inhibitor use (“option 1”) or once the ALT rose above the upper limit of normal and HBV DNA load increased (“option 2”). Nathan et al. [72] further recommended monitoring ALT monthly in those patients who received antiviral prophylaxis (continuing 3 months after cessation of therapy) with more frequent ALT testing and HBV DNA measurements in those who did not receive prophylaxis. Intensive monitoring 4–8 weeks after an infliximab infusion could allow earlier detection of HBV reactivation [72]. The clinical impact and cost effectiveness of these strategies have not been ascertained.
Based on our clinical experience, the data presented in this review, and the expert opinion of other authors, we favor a conservative strategy of starting antiviral therapy 1–2 weeks prior to treatment with a TNF-α inhibitor. We would initiate treatment with any TNF-α inhibitor except infliximab, reserving infliximab as a second (or lower) agent should the patient not demonstrate a clinical response. This decision is based on the information that we have presented here, even with the limitations discussed. Baseline liver function tests (at a minimum a serum Albumin and ALT) along with HBV DNA viral load should be obtained at the start of antiviral therapy, at the start of TNF-α inhibitor therapy, and then every 1–2 months thereafter while on TNF-α inhibitor therapy. More intensive monitoring with prompt cessation of TNF-α inhibitor therapy would be warranted if the patient had clinical or serologic evidence of HBV reactivation. Upon cessation of the TNF-α inhibitor, antiviral therapy along with liver function testing and HBV DNA viral load monitoring should be continued at least 1 to 3 months afterward. If a patient whose HBV status is unknown prior to starting a TNF-α inhibitor develops evidence of HBV infection or reactivation while on a TNF-α inhibitor, antiviral therapy should be started and close (weekly to every other week) clinical and serologic monitoring undertaken until stability has been documented. The role for other biologic response modifiers such as anakinra, an IL-1 receptor antagonist, and newer agents such as abatacept and tocilizumab is unclear at this time. Though these therapies may serve as alternatives to TNF-α inhibitors in patients at risk for HBV reactivation, data supporting such use are very limited and the antiviral and monitoring measures described in this paragraph should still apply.
A long-term consideration yet to be addressed is the impact that extended continuous exposure (more than several years) to TNF-α inhibitors has on patients chronically infected with HBV. For conditions that require TNF-α inhibitors for control, once such therapy is started, it is continued so long as the clinical response is sustained or a side effect is experienced. Very little is known about sustained TNF-α inhibitor use, with or without concomitant HBV antiviral medications, on complications of HBV such as hepatic fibrosis, cirrhosis, or hepatocellular carcinoma. In chronic HBV infection, TNF-α has a dual role that protects the hepatocyte by decreasing transcriptional activity of the HBV core promoter gene but yet can through different mechanisms lead to hepatocyte injury and apoptosis [84, 85]. With the combined positivity of HBsAg and HBeAg being related to a higher cumulative risk of developing hepatocellular carcinoma [86], do changes noted in HBV DNA with use of TNF-α inhibitors impact this risk? Can the long-term suppression of TNF-α actually have a protective effect on the hepatocyte, sparing it from injury and the liver from progressive fibrosis? As noted earlier, eight cases in this review had a liver biopsy performed [13, 18, 20, 22, 24, 27, 31, 32], two of which reported the results of repeat liver biopsies. In one case treated with infliximab, repeat biopsy demonstrated new septal fibrosis and incomplete nodules [13], whereas the other treated with etanercept on repeat biopsy reported no significant progression [18], although both cases received varying treatment courses with HBV antiviral medications. While it is unlikely that long-term clinical trials will be designed to prospectively answer these questions, postmarketing surveillance and long-term safety monitoring programs will be paramount in studying these clinically relevant issues.
In conclusion, while the class of TNF-α inhibitors have brought a great deal of promise in achieving control of chronic inflammatory conditions such as rheumatoid arthritis, Crohn's disease, and psoriasis, they have also been associated with the reactivation of latent infections. One such infection is HBV. This review sought to identify trends in the current medical literature of the reactivation of HBV among patients reported as having a positive HBsAg prior to initiation of a TNF-α inhibitor. Though a plausible relationship between the reactivation of HBV and the use of infliximab can be made based on the mechanism of action, route of administration, and potency in clearing TNF-α, such an association has methodological limitations and is not supported by some postmarketing data. It is the recommendation of the authors that when a patient is identified as positive for HBsAg prior to starting a TNF-α inhibitor, an antiviral agent is started first. After at least a week of antiviral therapy, with clinical and biochemical stability demonstrated, therapy with a TNF-α inhibitor may then commence. Close clinical and hepatic/viral biochemical monitoring is warranted with prompt cessation of TNF-α inhibitor therapy at the initial signs of worsening HBV infection.
References
Giles JT, Bathon JM (2004) Serious infections associated with anticytokine therapies in the rheumatic diseases. J Intensive Care Med 19:320–334
Keane J, Gershon S, Wise RP et al (2001) Tuberculosis associated with infliximab, a tumor necrosis factor α-neutralizing agent. N Engl J Med 345:1098–1103
Dienstag JL (2008) Hepatitis B virus infection. N Engl J Med 359(14):1486–1500
Shale MJ, Seow CH, Coffin CS et al (2009) Review article: chronic viral infection in the anti-tumour necrosis factor therapy era in inflammatory bowel disease. Aliment Pharmacol Ther 31:20–34
U.S. Food and Drug Administration Center for Drug Evaluation and Research (2008) Drugs@FDA: Adalimumab Label Information. http://www.accessdata.fda.gov/drugsatfda_docs/label/2008/125057s114lbl.pdf. Accessed 8 August 2009
U.S. Food and Drug Administration Center for Drug Evaluation and Research (2008) Drugs@FDA: Certolizumab Label Information. http://www.accessdata.fda.gov/drugsatfda_docs/label/2008/125160s000lbl.pdf. Accessed 8 August 2009
U.S. Food and Drug Administration Center for Drug Evaluation and Research (2008) Drugs@FDA: Etanercept Label Information. http://www.accessdata.fda.gov/drugsatfda_docs/label/2008/103795s5359lbl.pdf. Accessed 8 August 2009
U.S. Food and Drug Administration Center for Drug Evaluation and Research (2009) Drugs@FDA: Golimumab Label Information. http://www.accessdata.fda.gov/drugsatfda_docs/label/2009/125289s000lbl.pdf. Accessed 8 August 2009
U.S. Food and Drug Administration Center for Drug Evaluation and Research (2009) Drugs@FDA: Infliximab Label Information. http://www.accessdata.fda.gov/drugsatfda_docs/label/2009/103772s5234lbl.pdf. Accessed 8 August 2009
Wendling D, Di Martino V, Prati C et al (2009) Spondyloarthropathy and chronic B hepatitis. Effect of anti-TNF therapy. Jt Bone Spine 76:308–311
Wendling D, Auge B, Bettinger D et al (2005) Reactivation of a latent precore mutant hepatitis B virus related chronic hepatitis during infliximab treatment for severe spondyloarthropathy. Ann Rheum Dis 64:788–789
Esteve M, Loras C, González-Huix F (2007) Lamivudine resistance and exacerbation of hepatitis B in infliximab-treated Crohn's disease patient. Inflamm Bowel Dis 13(11):1450–1451
Esteve M, Saro C, González-Huix F et al (2004) Chronic hepatitis B reactivation following infliximab therapy in Crohn's disease patients: need for primary prophylaxis. Gut 53:1363–1365
Zingarelli S, Frassi M, Bazzani C et al (2009) Use of tumor necrosis factor-α-blocking agents in hepatitis B virus-positive patients: reports of 3 cases and review of the literature. J Rheumatol 36(6):1188–1194
Zingarelli S, Airò P, Frassi M et al (2008) Prophylaxis and therapy of HBV infection in 20 patients treated with disease modifying antirheumatic drugs or with biological agents for rheumatic diseases. Reumatismo 60(1):22–27
Roux CH, Brocq O, Breuil V et al (2006) Safety of anti-TNF-α therapy in rheumatoid arthritis and spondyloarthropathies with concurrent B or C chronic hepatitis. Rheumatology 45:1294–1297
Cansu DU, Kalifoglu T, Korkmaz C (2008) Short-term course of chronic hepatitis B and C under treatment with etanercept associated with different disease modifying antirheumatic drugs without antiviral prophylaxis. J Rheumatol 35:421–424
Carroll MB, Bond MI (2008) Use of tumor necrosis factor-α inhibitors in patients with chronic hepatitis B infection. Semin Arthritis Rheum 38(3):208–217
Li S, Kaur PP, Chan V (2009) Use of tumor necrosis factor-α (TNF-α) antagonists infliximab, etanercept, and adalimumab in patients with concurrent rheumatoid arthritis and hepatitis B or hepatitis C: a retrospective record review of 11 patients. Clin Rheumatol 28:787–791
Kaur PP, Chan VC, Berney SN (2008) Histological evaluation of liver in two rheumatoid arthritis patients with chronic hepatitis B and C treated with TNF-alpha blockade: case reports. Clin Rheumatol 27:1069–1071
Millonig G, Kern M, Ludwiczek O et al (2006) Subfulminant hepatitis B after infliximab in Crohn's disease: need for HBV-screening? World J Gastroenterol 12:974–976
Michel M, Duvoux C, Hezode C et al (2003) Fulminant hepatitis after infliximab in a patient with hepatitis B virus treated for an adult onset Still's disease. J Rheumatol 30:1624–1625
Ostuni P, Botsios C, Punzi L et al (2003) Hepatitis B reactivation in a chronic hepatitis B surface antigen carrier with rheumatoid arthritis treated with infliximab and low dose methotrexate. Ann Rheum Dis 62:686–687
Oniankitan O, Duvous C, Challine D et al (2004) Infliximab therapy for rheumatic diseases in patients with chronic hepatitis B or C. J Rheumatol 31:107–109
Ueno Y, Tanaka S, Shimamoto M et al (2005) Infliximab Therapy for Crohn's disease in patient with chronic hepatitis B. Dig Dis Sci 50:163–166
Anelli MG, Torres DD, Manno C et al (2005) Improvement of renal function and disappearance of hepatitis B virus DNA in a patient with rheumatoid arthritis and renal amyloidosis following treatment with infliximab. Arthritis Rheum 52:2519–2520
MdV G-S, Gomez-Camacho F, Poyato-Gonzalez A et al (2004) Infliximab therapy in a patient with Crohn's disease and chronic hepatitis B virus infection. Inflamm Bowel Dis 10(5):701–702
Madonia S, Orlando A, Scimeca D et al (2007) Occult hepatitis B and infliximab-induced HBV reactivation. Inflamm Bowel Dis 13(4):508
Robinson H, Walker-Bone K (2009) Anti-TNF-α therapy for rheumatoid arthritis among patients with chronic hepatitis B infection. Rheumatology 48:450–451
Sakellariou GT, Chatzigiannis I (2007) Long-term anti-TNFα therapy for ankylosing spondylitis in two patients with chronic HBV infection. Clin Rheumatol 26:950–952
Colbert C, Chavarria A, Berkelhammer C (2007) Fulminant hepatic failure in chronic hepatitis B on withdrawal of corticosteroids, azathioprine and infliximab for Crohn's disease. Inflamm Bowel Dis 13:1453–1454
Ojiro K, Naganuma M, Ebinuma H et al (2008) Reactivation of hepatitis B in a patient with Crohn's disease treated using infliximab. J Gastroenterol 43:397–401
Calabrese LH, Zein NN, Vassilopoulos D (2006) Hepatitis B virus (HBV) reactivation with immunosuppressive therapy in rheumatic diseases: assessment and preventive strategies. Ann Rheum Dis 65:983–989
Rehermann B (2000) Intrahepatic T cells in hepatitis B: viral control versus liver cell injury. J Exp Med 191:1263–1268
Cheong JY, Cho SW, Hwang IL et al (2006) Association between chronic hepatitis B virus infection and interleukin-10, tumor necrosis factor-α gene promoter polymorphisms. J Gastro Hepatology 21:1163–1169
Ben-Ari Z, Mor E, Papo O et al (2003) Cytokine gene polymorphisms in patients infected with hepatitis B virus. Am J Gastroenterol 98:144–150
Höhler T, Kruger A, Gerken G et al (1998) A tumour necrosis factor-alpha (TNF-α) promoter polymorphism is associated with chronic hepatitis B infection. Clin Exp Immunol 111:579–582
Li HQ, Li Z, Liu Y et al (2006) Association of-238G/A and -857C/T polymorphisms of tumor necrosis factor-alpha gene promoter region with outcomes of hepatitis B virus infection. Biomed Environ Sci 19(2):133–136
Li HQ, Li Z, Liu Y (2005) Association of polymorphism of tumor necrosis factor-alpha gene promoter region with outcome of hepatitis B virus infection. World J Gastroenterol 11(33):5213–5217
Kim YJ, Lee HS, Yoon JH et al (2003) Association of TNF-alpha promoter polymorphisms with the clearance of hepatitis B virus infection. Hum Mol Genet 12(19):2541–2546
Du T, Guo XH, Zhu XL et al (2006) Association of TNF-alpha promoter polymorphisms with the outcomes of hepatitis B virus infection in Chinese Han population. J Viral Hepat 13(9):618–624
Fang JWS, Shen WW, Meager A et al (1996) Activations of the tumor necrosis factor-α system in the liver in chronic hepatitis B virus infection. Am J Gastroenterol 91:748–753
Rehermann B (2000) Intrahepatic T cells in hepatitis B: viral control versus liver cell injury. J Exp Med 191:1263–1268
Su F, Schneider RJ (1997) Hepatitis B virus HBx protein sensitizes cells to apoptotic killing by tumor necrosis factor α. Proc Natl Acad Sci USA 94:8744–8749
Thimme R, Wieland S, Steiger C et al (2003) CD8+ T cells mediate viral clearance and disease pathogenesis during aucte hepatitis B virus infection. J Virol 77:68–76
Block TM, Guo H, Guo JT (2007) Molecular virology of hepatitis B virus for clinicians. Clin Liver Dis 11:685–706
Petersen J, Lutgehetmann M, Volz T et al (2007) What is the role of cccDNA in chronic HBV infection? Impact on HBV therapy. Hepatol Rev 4:9–13
Gao W, Hu J (2007) Formation of hepatitis B virus covalently closed circular DNA: removal of genome-linked protein. J Virol 81:6164–6174
Sung JJ, Wong ML, Bowden S (2005) Intrahepatic hepatitis B virus covalently closed circular DNA can be a predictor of sustained response to therapy. Gastroenterol 128:1890–1897
Zoulim F (2005) New insight on HBV persistence from the study of intrahepatic viral cccDNA. J Hepatol 42:302–308
Maini MK, Boni C, Lee CK et al (2000) The role of virus-specific CD8+ cells in liver damage and viral control during persistent hepatitis B virus infection. J Exp Med 191:1269–1281
Hussain MJ, Lau JY, Williams R et al (1994) Hepatic expression of tumour necrosis factor-alpha in chronic hepatitis B virus infection. J Clin Pathol 47(12):1112–1115
Ganem D, Prince AM (2004) Hepatitis B virus infection—natural history and clinical consequences. N Engl J Med 350:1118–1129
Jeng JE, Tsai JF, Chuang LY et al (2007) Tumor necrosis factor-alpha 308.2 polymorphism is associated with advanced hepatic fibrosis and higher risk for hepatocellular carcinoma. Neoplasia 9(11):987–992
Remicade website (2010) Centocor. http://www.remicade.com/remicade/global/index.html. Accessed 7 April 2010
Tracey D, Klareskog L, Sasso EH et al (2008) Tumor necrosis factor antagonist mechanisms of action: a comprehensive review. Pharmacol Ther 117:244–279
Furst DE, Beenhouwer O (2006) Tumor necrosis factor antagonists: different kinetics and/or mechanisms of action may explain differences in the risk for developing granulomatous infection. Semin Arthritis Rheum 36(3):159–167
Weaver AL (2003) Differentiating the new rheumatoid arthritis biologic therapies. J Clin Rheumatol 9(2):99–114
Olsen NJ, Stein CM (2004) New drugs for rheumatoid arthritis. N Engl J Med 350(21):2167–2179
U.S. Food and Drug Administration Center for Drug Evaluation and Research (2004) Drugs@FDA: Infliximab Label Information. http://www.accessdata.fda.gov/drugsatfda_docs/label/2004/103772_5077_lbl.pdf. Accessed 8 August 2009
Bourne T, Fossati G, Nesbitt A (2008) A PEGylated Fab' fragment against tumor necrosis factor for the treatment of Crohn's disease. Biodrugs 22(5):331–337
Mitoma H, Horiuchi T, Tsukamoto H et al (2008) Mechanisms for cytotoxic effects of anti-tumor necrosis factor agents on transmembrane tumor necrosis factor α-expressing cells: comparison among infliximab, etanercept, and adalimumab. Arthritis Rheum 58(5):1248–1257
Scott DL, Cope A (2009) New tumor necrosis factor inhibitors for rheumatoid arthritis: are there benefits from extending choice? Ann Rheum Dis 68(6):767–769
Fossati G, Nesbitt A (2005) In vitro complement-dependent cytotoxicity and antibody-dependent cellular cytotoxicity by the anti-TNF agents adalimumab, etanercept, infliximab, and certolizumab pegol (CDP870): 807. Am J Gastro 100(supp 1):S299
Saliu OY, Sofer C, Stein D et al (2006) Tumor-necrosis-factor blockers: differential effects on mycobacterial immunity. J Infect Dis 194:486–492
Tubach F, Salmon D, Ravaud P et al (2009) Risk of tuberculosis is higher with anti-tumor necrosis factor monoclonal antibody therapy than with soluble tumor necrosis factor receptor therapy. Arthritis Rheum 60(7):1884–1894
Suwannalai P, Auethavekiat P, Udomsubpayakul U et al (2009) The infectious profiles of anti-tumor necrosis factor agents in a Thai population: a retrospective study a the university-based hospital. Int J Rheum Dis 12(2):118–124
Takeuchi T, Tatsuki Y, Nogami Y et al (2008) Postmarketing surveillance of the safety profile of infliximab in 5000 Japanese patients with rheumatoid arthritis. Ann Rheum Dis 67(2):189–194
Koike T, Harigai M, Inokuma S et al (2009) Postmarketing surveillance of the safety and effectiveness of etanercept in Japan. J Rheum 36(5):898–906
U.S. Food and Drug Administration Center for Drug Evaluation and Research (1999) Drugs@FDA: Infliximab Product Approval Information. <http://www.accessdata.fda.gov/drugsatfda_docs/appletter/1999/inflcen111099L.htm. Accessed 17 March 2010
U.S. Food and Drug Administration Center for Drug Evaluation and Research (2002) Drugs@FDA: Etanercept Product Approval Information-Licensing Action. http://www.accessdata.fda.gov/drugsatfda_docs/appletter/2002/etanimm011502L.htm. Accessed 17 March 2010
Nathan DM, Angus PW, Gibson PR (2006) Hepatitis B and C virus infections and anti-tumor necrosis factor-α therapy: guidelines for clinical approach. J Gastroenterol Hepatol 21:1366–1371
Liang TJ (2009) Hepatitis B: the virus and disease. Hepatology 49(5 Suppl):S13–S21
Saag KG, Teng GG, Patkar NM et al (2008) American College of Rheumatology 2008 recommendations for the use of nonbiologic and biologic disease-modifying antirheumatic drugs in rheumatoid arthritis. Arthritis Rheum 59(6):762–784
Ledingham J, Deighton C (2005) Update on the British Society for Rheumatology guidelines for prescribing TNFalpha blockers in adults with rheumatoid arthritis (update of previous guidelines of April 2001). Rheumatology 44(2):157–163
British Society of Rheumatology. “BSR Guidelines.” http://www.rheumatology.org.uk/guidelines/. Accessed 15 August 2009
Lichtenstein GR, Abreu MT, Cohen R et al (2006) American Gastroenterologic Association Institute medical position statement on corticosteroids, immunomodulators, and infliximab in inflammatory bowel disease. Gastroenterology 130:935–939
Carter MJ, Lobo AJ, Travis SPL (2004) Guidelines for the management of inflammatory bowel disease in adults. Gut 53(Supp V):v1–v16
Desai SB, Furst DE (2006) Problems encountered during anti-tumor necrosis factor therapy. Best Prac & Res Clin Rheum 20(4):757–790
Vassilopoulos D, Calabrese LH (2007) Risks of immunosuppressive therapies including biologic agents in patients with rheumatic diseases and co-existing chronic viral infections. Curr Opin Rheumatol 19:619–625
Marignani M, Cox MC, Delle Fave G (2009) Hepatitis B virus infection. N Engl J Med 360(3):304–306
Tilg H, Kaser A, Moschen AR (2006) How to modulate inflammatory cytokines in liver disease. Liver Int 26:1029–1039
Calabrese LH, Zein NN, Vassilopoulos D (2006) Hepatitis B virus (HBV) reactivation with immunosuppressive therapy in rheumatic diseases: assessment and preventive strategies. Ann Rheum Dis 65:983–989
Cheong JY, Cho SW, Hwang IL et al (2006) Association between chronic hepatitis B virus infection and interleukin-10, tumor necrosis factor-α gene promoter polymorphisms. J Gastro Hepatology 21:1163–1169
Thio CL, Thomas DL, Carrington M (2000) Chronic viral hepatitis and the human genome. Hepatology 31:819–827
Yang HI, Lu SN, Liaw YF et al (2002) Hepatitis B e antigen and the risk of hepatocellular carcinoma. N Engl J Med 347(3):168–174
Disclosures
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors confirm that this manuscript has neither been submitted nor is simultaneously being submitted elsewhere. No portion of the data has been or will be published in proceedings or transactions of meetings or symposium volumes.
The authors have no financial support or other benefits from commercial sources to disclose. They received no pharmaceutical or industry support in writing this manuscript.
The views expressed in this article are those of the authors and do not reflect the official policy or position of the United States Air Force, Department of Defense, or the US Government.
Rights and permissions
About this article
Cite this article
Carroll, M.B., Forgione, M.A. Use of tumor necrosis factor α inhibitors in hepatitis B surface antigen-positive patients: a literature review and potential mechanisms of action. Clin Rheumatol 29, 1021–1029 (2010). https://doi.org/10.1007/s10067-010-1523-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-010-1523-2