Abstract
We present a 45-year-old male patient who presented to Accident and Emergency department with a 6-week history of pain and stiffness involving his bilateral legs. Both calves were markedly tender, and he was not able to bear weight. He also complained of numbness involving his left big toe for a few days, which later spread to involve his arms, and tinnitus and hearing loss in his left ear. There were no respiratory, gastrointestinal or urinary symptoms. He had a background history of hypercholesterolemia and was treated with atorvastatin 10 mg for 6 months. His initial investigations showed markedly increased inflammatory markers, and serum antineutrophil cytoplasmic antibody (ANCA) was markedly positive at a titre of 1:160 (P-ANCA). Electromyography and muscle biopsy showed myopathic features. A diagnosis of drug-induced ANCA-associated vasculitis (on the basis of mononeuritis multiplex, sensorineural hearing loss and markedly increased anti-myeloperoxidase (MPO) ANCA) and statin-induced distal myopathy was made. He was treated with three 500 mg doses of methylprednisolone, followed by slowly tapering dose of oral corticosteroids from 30 mg once daily (OD). He was also started on azathioprin (2.5 mg/kg). He had a dramatic improvement of his myalgia, hearing loss and sensory symptoms and went into complete clinical remission. His inflammatory markers rapidly returned to normal, and MPO-ANCA normalised within 3 months of starting immunosuppressive therapy and remained negative on further testing. He is currently on a tapering regimen of corticosteroids (7 mg OD), and after weaning him off corticosteroids, we plan to slowly taper his azathioprin.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Case report
Statins (3-hydoxy-3-methyl-glutaryl coenzyme A (HMG-CoA) reductase inhibitors) are the principal treatment for hypercholesterolemia and are also used extensively in the secondary prevention of cardiovascular events. HMG-CoA reductase inhibition has beneficial pleitropic effects that extend well beyond its role in lipid metabolism, for example, reduction of low-density lipoprotein and triglyceride levels, anti-atherosclerotic effects and reduction of platelet aggregation, and it has also been described to have anti-inflammatory effects. Hence, statin has contributed significantly in the reduction of cardiovascular morbidity and mortality, and the number of statin users is increasing. Hepatic dysfunction and muscle injury are the main concerns. However, few case reports of autoimmune reactions such as myositis [1, 2], lupus [3, 4] and interstitial lung disease [5, 6], suspected to be associated with statin, have been described. To our knowledge, this is the first reported case of an antineutrophil cytoplasmic antibody (ANCA)-associated systemic vasculitis induced by a statin (atorvastatin). Moreover, our patient had simultaneous development of lower leg myopathy, and this combination of drug-induced ANCA-associated vasculitis and myopathy is unique on its own.
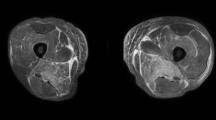
A 45-year-old male patient presented in September 2007 with a 6-week history of pain and stiffness involving both his legs. Later on, this extended to involve his forearms. Both calves were markedly tender, and he was not able to bear weight. He also complained of numbness involving his left big toe for a few days, which later spread to involve his arms, and tinnitus and hearing loss in his left ear. There were no respiratory, gastrointestinal or urinary symptoms. He had a background history of hypercholesterolemia and was treated with atorvastatin 10 mg for 6 months. However, he had stopped atorvastatin 2 months earlier. On laboratory tests, he showed normal complete blood count, normal kidney disease profile (including urea, creatinine, calcium, phosphate, albumin) and normal muscle enzymes (creatine phosphokinase , lactate dehydrogenase, aspartate aminotransferase). He was found to have markedly elevated inflammatory markers, with a C-reactive protein of 198 mg/ml (normal 1–10 mg/l).Viral serology was negative (including serology for parvovirus, mycoplasma, brucella, enterovirus), and there were no cryoglubins detected. The patient had negative results on antinuclear antibody and rheumatoid factor testing. Electromyography showed myopathic features in anterior and posterior compartments of both legs, and there were no myopathic features in upper limbs. Biopsy of his symptomatic left gastrocnemius showed type-1 fibre atrophy along with cytochrome-oxidase depleted fibres, and there was no evidence of myositis or neuropathy. These changes were reported to suggest myopathic features. A diagnosis of drug-induced ANCA-associated vasculitis (on the basis of mononeuritis multiplex, sensorineural hearing loss and markedly increased anti-myeloperoxidase (MPO) ANCA levels) and statin-induced distal myopathy was made. It is possible that his leg symptoms were contributed to by myositis, vasculitis or both, but muscle biopsy showed only myopathy features. He was treated initially with three 500 mg doses of methylprednisolone, followed by slowly tapering dose of oral corticosteroids from 30 mg once daily (OD). He was also started on azathioprin at a dose of 2.5 mg/kg. He had a dramatic response with improvement of myalgia, hearing loss, sensory symptoms and inflammatory markers, and later, he went into complete clinical remission. His inflammatory markers returned to normal within 6 weeks, and MPO-ANCA normalised rapidly within 3 months of starting immunosuppressive therapy and remained negative on further testing. He is currently on a tapering regimen of corticosteroids (7 mg OD at present), and after weaning him off corticosteroids, we plan to slowly taper his azathioprin.
Discussion
Statins are generally well tolerated and have an excellent safety profile. Research has revealed that statins have profound multi-system effects, and these extend beyond the lipid metabolism. Statins occasionally cause muscle and liver toxicity. Muscle toxicity presents with a variety of complaints ranging from simple myalgia and myositis to life-threatening rhabdomyolysis. As we observed in our patient, it should be emphasised that creatine kinase levels can be normal in muscle injury. This reveals that muscle toxicity may occur below the threshold required to increase enzyme levels. Statin-induced myopathy is generally self-limiting and runs a benign clinical course. In one of the largest case series, Hansen et al. [7] report that, in their clinical practice, myopathy associated with statin use is reversible after discontinuation of the offending drug, and it carries a good outcome.
Drug use may also result in development of an immunologic reaction, and the association between drugs and ANCA-associated vasculitis is well described. This syndrome spans a spectrum of complaints ranging from constitutional symptoms to target-organ damage. Anti-thyroidism drugs are a well-documented cause of ANCA-associated vasculitis. Moreover, hydralazine, allopurinol, sulphasalazine, minocycline, ciprofloxacin, isoniazid, rifampicin, phenytoin and clozapaine have also been implicated as culprit drugs. This form of vasculitis is frequently associated with very high titres of anti-myeloperoxidase ANCA [8] and has also been described as characteristic of drug-induced ANCA-associated vasculitis. A very small number of patients have been reported to have PR3-ANCA. Pathogenesis of this form of vasculitis remains undefined. Drug-induced ANCA-associated vasculitis may be difficult to distinguish from idiopathic ANCA vasculitides, and reported prognosis is better compared to idiopathic ANCA-associated vasculitis. It is frequently slow to resolve after cessation of the offending drug and, in severe cases, may require short course of immunosuppresives. As ANCA-associated vasculitis is associated with significant morbidity, rechallenge with the offending agent is best avoided.
There has been an increase in reported adverse events paralleling increased usage of statin. Although, drug-induced ANCA-associated vasculitis is very rare, awareness of this potential association with statin therapy is important. In summary, we report herein the first case of statin-induced ANCA-associated vasculitis. Patient’s symptoms and laboratory abnormalities resolved rapidly after cessation of the offending drug (statin) and the institution of immunosuppressive therapy, which is slowly being withdrawn.
References
Vasconelos OM, Campbell WW (2004) Dermatomyositis-like syndrome and HMG-CoA reductase inhibitor (statin) intake. Muscle Nerve 30(6):803–807, (Dec)
Zuech P, Pauwels C, Duthoit C, Mery L, Somogyi A, Louboutin A, Veyssier-Belot C (2005) Pravastatin-induced dermatomyositis. Rev Med Interne 26(11):897–902, (Nov)
Noël B, Panizzon RG (2004) Lupus-like syndrome associated with statin therapy. Dermatology 208(3):276–277
Suchak R, Benson K, Swale V (2007) Statin-induced Ro/SSa-positive subacute cutaneous lupus erythematosus. Clin Exp Dermatol 32(5):589–591, (Sep)
Walker T, McCaffery J, Steinfort C (2007) Potential link between HMG-CoA reductase inhibitor (statin) use and interstitial lung disease. Med J Aust 186(2):91–94, (Jan 15)
Veyrac G, Cellerin L, Jolliet P (2006) A case of interstitial lung disease with atorvastatin (Tahor) and a review of the literature about these effects observed under statins. Therapie 61(1):57–67, (Jan–Feb)
Hansen KE, Hildebrand JP, Ferguson EE et al (2005) Outcomes in 45 patients with statin-associated myopathy. Arch Intern Med 165:2671–2676
Choi KH, Merkel AP, Walker MA, Niles LJ (2000) Drug-associated antineutrophil cytoplasmic antibody-positive vasculitis: prevalence among patients with high titres of antimyeloperoxidase antibodies. Arthritis Rheum 43:405–413
Disclosures
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Haroon, M., Devlin, J. A case of ANCA-associated systemic vasculitis induced by atorvastatin. Clin Rheumatol 27 (Suppl 2), 75–77 (2008). https://doi.org/10.1007/s10067-008-1020-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-008-1020-z