Abstract
Statin-induced immune-mediated necrotizing myopathy (IMNM) is a rare systemic neuromuscular condition. We present a case of a patient with a severe phenotype of the disease that was found to have an increase in anti-HMGCR and anti-ACHR antibodies. A potential association between these antibodies have not been previously described. A 67-year-old male with hyperlipidemia, who was recently initiated on atorvastatin therapy, presented to the ED with progressive muscle weakness. Within a few days of admission, the patient developed complete flaccid paralysis and respiratory distress requiring intubation. The patient’s CK was elevated to 24,000 and there was an increase of anti-HMGCR and anti-ACHR antibodies. Impressions from MRI and thigh biopsy solidified a diagnosis of statin-induced IMNM. The patient was treated with methylprednisolone, IVIG, and rituximab, which provided resolution of symptoms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Idiopathic inflammatory myopathies (IIM) are a group of systemic muscular diseases characterized by proximal muscle weakness, elevated levels of creatinine kinase (CK), and inflammatory findings on muscle biopsy [1]. Immune-mediated necrotizing myopathy (IMNM) is a subset of IIM which is classified based on findings of anti-signal recognition particle (SRP) and anti-hydroxy-3-methylglutaryl-CoA reductase (HMGCR) [2]. Furthermore, anti-HMGCR myopathy has been demonstrated to be associated with statin exposure [3].
Myasthenia gravis (MG) is an autoimmune disorder of the neuromuscular junction that presents with fluctuating muscle weakness and potential respiratory distress that is exacerbated by exertion [4]. MG is classically associated with anti-acetylcholine receptor (ACHR) antibodies which contributes to its pathogenesis by inhibiting its associated nicotinic receptors on the post-synaptic membrane of the neuromuscular junction and preventing depolarization and consequent muscle contraction [5]. Identification of anti-ACHR antibodies in a patient presenting with the associated clinical features such as extraocular, bulbar, or limb weakness is virtually diagnostic of MG [6].
In this case study, we present a patient found to have statin-induced IMNM with anti-HMGCR and anti-ACHR antibodies, as well as profound elevations of CK. By literature review, the concomitant increase in anti-HMGCR and anti-ACHR antibodies have only once been reported previously and may provide implications for our understanding of disease pathophysiology and management.
Case description
A 67-year-old male, with a past medical history of hyperlipidemia, presented to the emergency department with progressive muscle weakness for 1 month. There was also an associated back rash, difficulty swallowing, and shortness of breath during the same period. He reported difficulty with moving all extremities and his neck, which hindered his ability to maintain an upright head position. On physical examination, there was pain with motion of the head, a scattered erythematous rash on the posterior neck and upper back, slurred speech, and bilateral weakness in all extremities with a greater prominence in the proximal muscles.
The patient’s only medication was 20 mg of atorvastatin daily for 21 months. On initial presentation, his laboratory tests were notable for an elevated CK of 24,000 U/L, along with leukocytosis and elevated erythrocyte sedimentation rate, C-reactive protein, aldolase, alanine transaminase, aspartate aminotransferase, and thyroid stimulating hormone (Table 1). This prompted inpatient admission. The following day, he was transferred to the ICU and intubated due to respiratory distress, dysphagia, and flaccid paralysis of all extremities.
An inflammatory myopathy was suspected, which warranted a comprehensive diagnostic work-up. MRI of the lower extremities demonstrated edema and patchy hyperenhancement within posterior compartments bilaterally (Fig. 1). Investigation for paraneoplastic syndrome due to malignancy was negative by esophagogastroduodenoscopy, colonoscopy, and CT of the chest, abdomen, and pelvis. Furthermore, CT of the chest did not demonstrate any thymic pathology that might have contributed to the presentation. Viral and bacterial screening for infectious etiologies were negative. A comprehensive autoimmune and myositis panel was positive for HMGCR and ACHR antibodies. Pertinent negative laboratory tests included ANA, RF, anti-Jo, anti-Mi, anti-SRP, anti-SSA, anti-SSB. Total serum immunoglobulin levels were in reference range (IgG = 1290, IgA = 272).
Punch biopsies of skin from the left and right upper back demonstrated patchy basal vacuolar changes and superficial perivascular dermatitis with scattered neutrophils bilaterally. A muscle biopsy of the right rectus femoris demonstrated scattered necrotic and regenerating fibers, variation in fiber size and a mild neurogenic process with denervation and reinnervation. Immunohistochemical staining highlighted CD56 positive scattered fibers and CD163 positive scattered macrophages with fibers undergoing myophagocytosis. Lymphocytic inflammation was not observed. Further immunohistochemical analysis for major histocompatibility complex showed occasional fibers with positive staining and rare membrane attack complex positive fibers.
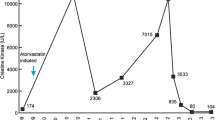
Statins were immediately discontinued on admission. He was started on 1 g methylprednisolone IV for 3 days and 60 g IVIG for 2 days, which temporarily provided mild symptomatic improvement and a decrease in CK to 8400. Following the course of the initial treatment, his extremity weakness and increased work of breathing persisted, along with an increase in CK to 13,000. This prompted administration of two 1 g rituximab IV treatments given 2 weeks apart, monthly IVIG, and weekly 1 g methylprednisolone IV treatment. The symptoms progressively improved and the patient was discharged to a long-term acute care hospital. Within the following 2 months, his CK stabilized to reference range, he was weaned from ventilation, and he had his PEG tube removed. The patient made a near complete recovery, without any persistence of dyspnea, dysphagia, paresthesia, weakness, or paralysis.
CK levels were assessed daily through the patient’s hospitalization (Fig. 2). His initial CK level on admission was 24,364 and had decreased to 2242 by the time of discharge. On day 1 of admission, the patient received a 2-day course of 60 g IVIG and 3-day course of 1 g methylprednisolone. He received his first infusion of 1 g rituximab on day 5 and second infusion on day 20. Following discharge to the long-term acute care hospital, he received biweekly 1 g methylprednisolone treatments and monthly 2-day infusions of 60 g IVIG. At his outpatient follow-up, 2 months after discharge from the hospital, his laboratory test levels were within reference range (Table 1).
Search strategy
A literature review was conducted by searching databases of Pubmed/Medline, Embase, and Web of Science. Search keywords included a combination of the terms “statin induced”, “immune mediated necrotizing myopathy”, “necrotizing autoimmune myopathy”, “anti-hmgcr”, “myasthenia gravis”, “anti-achr”, and “acetylcholine receptor antibody”. A narrow inclusion criterion was utilized to identify all cases of interest. Cases were included if they discussed a clinical presentation of a patient diagnosed with statin-induced IMNM that was found to have both anti-HMGCR and anti-ACHR antibodies. Cases were excluded if there were no report of the concomitant increases of the antibodies of interest.
Results
The literature review revealed only one previously published case study that reported the concomitant increase of both anti-HMGCR and anti-ACHR antibodies in a patient with statin induced IMNM [7]. Many similarities are present between the cases such as the induction by atorvastatin, significantly elevated CK, LDH, AST, ALT, and presentation with progressive muscle weakness and dyspnea. However, the respiratory distress in their reported patient did not lead to intubation and the muscle weakness was less profound. Fortunately, persistent improvement of symptoms were achieved by IVIG, methotrexate, prednisone, and pyridostigmine.
Discussion
Statins are among the most widely used medications for management of cardiovascular disease. The mechanism of action of statins involves inhibition of the HMG-CoA reductase enzyme, which consequently limits cholesterol synthesis within hepatocytes [8]. Although relatively safe, neuromuscular disorders comprise a majority of the adverse effects associated with use of statins [9]. A rare side-effect of statins is the induction of autoimmune illnesses, such as IMNM, myasthenia gravis, dermatomyositis, and polymyositis [9].
The incidence of IMNM has been reported to be 2–3 per 100,000 patients using statins [10]. Patients with IMNM have an associated increase in specific antibodies, such as anti-SRP or anti-HMGCR [11].
Physical manifestations of IMNM with anti-HMGCR include proximal muscle weakness, myalgia, fatigue, dysphagia, and uncommon non-specific findings such as rash, arthritis, or Raynaud’s phenomenon [12]. Diagnostic studies usually demonstrate an elevated CK (2000–20,000 U/L) and a muscle biopsy demonstrating muscle fiber necrosis and inflammation with a macrophage predominance [13].
The novelty of our presented case is attributed to the simultaneous elevation of anti-HMGCR and anti-ACHR antibodies, in a previously healthy individual who had recently started statin therapy. The presence of anti-HMGCR is strongly suggestive of statin-induced IMNM, with a 94.4% sensitivity and 99.3% specificity [14]. ACHR antibodies are more suggestive of MG which statin use has also previously been observed to promote presentation of [15]. However, a potential association between anti-ACHR and anti-HMGCR has not been previously reported. The concomitant elevation of these antibodies likely contributed to the increased severity of presentation within the current case.
Multiple findings had led to the diagnosis of IMNM within this patient. Initial suspicions occurred when discovering the dramatically increased CK levels, proximal muscle weakness, and recent initiation of statin therapy. Identification of the associated antibody after a broad autoimmune antibody panel warranted a comprehensive diagnostic assessment. Imaging of the extremities then demonstrated a potential necrotic pattern. The diagnosis of IMNM was finalized following histologic examination of the muscle biopsy, which confirmed the necrotic features associated with IMNM. Thus, the findings of HMGCR antibodies, proximal muscle weakness, elevated CK, muscle hyperintensity on MRI, and necrotic features on muscle biopsy fulfil all the criteria suggested for the diagnosis of IMNM [2]. Full body imaging and endoscopic examinations did not reveal other remarkable findings that may explain another disease process.
Although ACHR antibodies are usually indicative of MG, this patient did not initially present with classical features associated with the disease. For instance, he did not have diplopia, ptosis, blurry vision, or ocular fatigue followed by sustained upgaze. Since multiple neurologic examinations were not consistent with MG, there were no pertinent diagnostic tests that followed. However, upon admission, the patient developed respiratory distress and dysphagia which shared dangerous characteristics of MG [16]. The presence of anti-ACHR found during hospitalization may suggest a potentially additive effect of MG with IMNM or a severe phenotype of IMNM associated with an increase in both ACHR and HMGCR antibodies.
Initially, this patient demonstrated a large area of scattered non-pruritic erythematous rash on the posterior neck and upper back, which had subsided 1 week into admission. This finding resulted in the consideration of dermatomyositis in the differential diagnosis due to the similar appearance of the shawl sign associated with the disease [17]. However, the presence of an erythematous rash is not uncommon in statin-induced IMNM. Several previous case reports have reported a dermatomyositis resembling skin rash in patients with statin-induced IMNM [18,19,20]. Thus, the presence of a rash should not discount the possibility for IMNM.
The severity of symptoms of this patient is important to emphasize. Within the first several days of hospitalization, this patient exhibited respiratory failure requiring intubation, dysphagia, and near complete flaccid paralysis of all extremities. In a retrospective review of 63 patients with necrotizing autoimmune myopathy, 5 patients ultimately required intubation [21]. This suggests that a subset of patients with the disease develop a more severe phenotype.
Due to the rarity of the disease, there are currently no clinical trials that may be referenced to guide therapeutic management of patients with statin-induced IMNM. However, based on the availability of reported cases, induction of immunosuppression appears to be the best course to pursue [22]. Success has been demonstrated with oral prednisone, methotrexate, azathioprine, mycophenolate mofetil, IVIG, and rituximab [22]. In a retrospective study of 55 patients with statin-induced IMNM, a triple therapy of steroid, IVIG, and steroid-sparing immunosuppressant demonstrated efficacious results [23]. Therefore, when statin-induced IMNM is expected, rapid immunosuppression should be initiated to ensure optimal prognosis for the patient.
References
Malik A, Hayat G, Kalia JS, Guzman MA (2016) Idiopathic inflammatory myopathies: clinical approach and management. Front Neurol 20(7):64. https://doi.org/10.3389/fneur.2016.00064
Pinal-Fernandez I, Casal-Dominguez M, Mammen AL (2018) Immune-mediated necrotizing myopathy. Curr Rheumatol Rep 20(4):21. https://doi.org/10.1007/s11926-018-0732-6
Troyanov Y, Landon-Cardinal O, Fritzler MJ, Ferreira J, Targoff IN, Rich E, Goulet M, Goulet JR, Bourré-Tessier J, Robitaille Y, Drouin J, Albert A, Senécal JL (2017) Atorvastatin-induced necrotizing autoimmune myositis: an emerging dominant entity in patients with autoimmune myositis presenting with a pure polymyositis phenotype. Medicine (Baltimore) 96(3):e5694. https://doi.org/10.1097/MD.0000000000005694
JayamTrouth A, Dabi A, Solieman N, Kurukumbi M, Kalyanam J (2012) Myasthenia gravis: a review. Autoimmune Dis 2012:874680. https://doi.org/10.1155/2012/874680
Meriggioli MN, Sanders DB (2012) Muscle autoantibodies in myasthenia gravis: beyond diagnosis? Expert Rev Clin Immunol 8(5):427–438. https://doi.org/10.1586/eci.12.34
Rousseff RT (2021) Diagnosis of myasthenia gravis. J Clin Med 10(8):1736. https://doi.org/10.3390/jcm10081736
Frasson E, Simonetto M, Bertolasi L, Caneve G, Vilotti C, Ruzza G, Perelli A, Piccinno MG, Monaco S (2021) Statin-associated necrotizing autoimmune myopathy with concurrent myasthenia gravis. Clin Case Rep 9(5):e03925. https://doi.org/10.1002/ccr3.3925
Stancu C, Sima A (2001) Statins: mechanism of action and effects. J Cell Mol Med 5(4):378–387. https://doi.org/10.1111/j.1582-4934.2001.tb00172.x
Attardo S, Musumeci O, Velardo D, Toscano A (2022) Statins neuromuscular adverse effects. Int J Mol Sci 23(15):8364. https://doi.org/10.3390/ijms23158364
Villa L, Lerario A, Calloni S, Peverelli L, Matinato C, De Liso F, Ceriotti F, Tironi R, Sciacco M, Moggio M, Triulzi F, Cinnante C (2018) Immune-mediated necrotizing myopathy due to statins exposure. Acta Myol 37(4):257–262
Mammen AL (2011) Autoimmune myopathies: autoantibodies, phenotypes and pathogenesis. Nat Rev Neurol 7(6):343–354. https://doi.org/10.1038/nrneurol.2011.63
Mohassel P, Mammen AL (2018) Anti-HMGCR myopathy. J Neuromuscul Dis 5(1):11–20. https://doi.org/10.3233/JND-170282
Selva-O’Callaghan A, Alvarado-Cardenas M, Pinal-Fernández I, Trallero-Araguás E, Milisenda JC, Martínez MÁ, Marín A, Labrador-Horrillo M, Juárez C, Grau-Junyent JM (2018) Statin-induced myalgia and myositis: an update on pathogenesis and clinical recommendations. Expert Rev Clin Immunol 14(3):215–224. https://doi.org/10.1080/1744666X.2018.1440206. (Epub 2018 Feb 23)
Joudeh AI, Albuni MK, Hassen SS, Iqbal P, Aziz Bedair EM, Mahdi S (2022) A case report of statin-induced immune-mediated necrotizing myopathy treatment challenges. Case Rep Rheumatol 31(2022):4647227. https://doi.org/10.1155/2022/4647227
Keogh MJ, Findlay JM, Leach S, Bowen J (2010) Statin-associated weakness in myasthenia gravis: a case report. J Med Case Rep 20(4):61. https://doi.org/10.1186/1752-1947-4-61
Roy TM, Walker JF, Farrow JR (1991) Respiratory failure associated with myasthenia gravis. J Ky Med Assoc 89(4):169–173
Ranjit E, Sapra A, Etherton A, Wasey W, Bhandari P (2020) “Shawl Sign” as a paraneoplastic dermatosis. Cureus 12(4):e7498. https://doi.org/10.7759/cureus.7498
Merlant M, Fite C, Kottler D, Maisonobe L, Dossier A, Deschamps L, Descamps V (2019) Myopathie nécrosante auto-immune à anticorps anti-HMGCR induite par les statines et révélée par un tableau évocateur de dermatomyosite [Dermatomyositis-like syndrome revealing statin-induced necrotizing autoimmune myopathy with anti-HMGCR antibodies]. Ann Dermatol Venereol 146(8–9):550–556. https://doi.org/10.1016/j.annder.2018.12.010(Epub 2019 Mar 29)
Akivis Y, Kurup M, John S (2022) Statin-induced necrotizing autoimmune myositis. J Med Cases 13(10):513–516. https://doi.org/10.14740/jmc4010. (Epub 2022 Oct 31)
Gagliardo CM, Noto D, Giammanco A, Maltese S, Vecchio L, Lavatura G, Cacciatore V, Barbagallo CM, Ganci A, Nardi E, Ciaccio M, Lo Presti R, Cefalù AB, Averna M (2023) Statin-induced autoimmune myositis: a proposal of an “experience-based” diagnostic algorithm from the analysis of 69 patients. Intern Emerg Med 18(4):1095–1107. https://doi.org/10.1007/s11739-023-03278-9. (Epub 2023 May 5)
Kassardjian CD, Lennon VA, Alfugham NB, Mahler M, Milone M (2015) Clinical features and treatment outcomes of necrotizing autoimmune myopathy. JAMA Neurol 72(9):996–1003. https://doi.org/10.1001/jamaneurol.2015.1207
Mammen AL (2016) Statin-associated autoimmune myopathy. N Engl J Med 374(7):664–669. https://doi.org/10.1056/NEJMra1515161
Meyer A, Troyanov Y, Drouin J, Oligny-Longpré G, Landon-Cardinal O, Hoa S, Hervier B, Bourré-Tessier J, Mansour AM, Hussein S, Morin V, Rich E, Goulet JR, Chartrand S, Hudson M, Nehme J, Makhzoum JP, Zarka F, Villeneuve E, Raynauld JP, Landry M, O’Ferrall EK, Ferreira J, Ellezam B, Karamchandani J, Larue S, Massie R, Isabelle C, Deschênes I, Leclair V, Couture H, Targoff IN, Fritzler MJ, Senécal JL (2020) Statin-induced anti-HMGCR myopathy: successful therapeutic strategies for corticosteroid-free remission in 55 patients. Arthritis Res Ther 22(1):5. https://doi.org/10.1186/s13075-019-2093-6
Acknowledgements
The authors would like to acknowledge the described patient for providing permission to publish his story and highlight his journey and resilience.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to declare.
Ethical standards
The authors confirm that they have no funding, financial relationships, or other conflicts of interest to declare. No financial support was received for this study. All authors have reviewed and approved this manuscript for submission. Written informed consent was obtained by the patient to publish the case for research purposes.
Consent to publish
Written informed consent was obtained from the patient for publication of this report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Garabet, R., Herr, S., Griffin, N. et al. Statin-induced immune-mediated necrotizing myopathy with concomitant increase of anti-HMGCR and anti-ACHR antibodies. Rheumatol Int 44, 955–959 (2024). https://doi.org/10.1007/s00296-024-05559-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-024-05559-8