Abstract
Clinical aspects and pathology of pulmonary hypertension (PH) in patients with systemic lupus erythematosus (SLE) have been reported to be similar to those in patients with idiopathic pulmonary arterial hypertension (IPAH). To determine whether PH in these patients is similar, we compared the clinical characteristics, hemodynamics at diagnosis, and survival in groups of patients with SLE–PH and IPAH. We reviewed the case records of 20 patients with SLE–PH and 34 patients with IPAH, who had been assessed by echocardiography or right cardiac catheterization at Asan Medical Center, Seoul, Korea, from January 1995 to October 2003. Clinical features, laboratory data, chest X-rays, electrocardiogram results, pulmonary function tests, pulmonary perfusion scans, echocardiographic findings, serologic profiles, and survival were compared in the two groups of patients. The mean follow-up period was 18.1±20.6 months for patients with SLE–PH and 33.0±23.4 months for patients with IPAH. During follow-up, 12 SLE–PH (60%) and 11 IPAH (32%) patients died. For SLE–PH, the 3-year survival rate was 44.9% and the 5-year survival rate was 16.8%. For IPAH, the 3-year survival rate was 73.4% and the 5-year survival rate was 68.2% (p=0.02). There were no other significant differences in clinical characteristics and laboratory data between the two groups. In contrast to previous reports that the prognosis of patients with pulmonary arterial hypertension associated with collagen vascular disease was better than that of patients with IPAH, we found that the prognosis of patients with SLE–PH was much worse than that of patients with IPAH.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pulmonary arterial hypertension (PH) is a rare but severe complication in patients with systemic lupus erythematosus (SLE), occurring in about 0.5–14% of SLE patients [1–5].
In patients with SLE, PH may be mild or asymptomatic, and it may be difficult to diagnose because it can develop as a result of heart failure, pulmonary thromboembolism, hypoxia, or respiratory failure. PH in connective tissue diseases may be a life-threatening complication as well as a crucial factor in determining prognosis. For example, the prognosis of patients with SLE-induced PH is poor, with a two-year mortality higher than 50% [6, 7]. In Korea, PH is the third leading cause of death in SLE patients [8].
Idiopathic pulmonary arterial hypertension (IPAH) is clinically defined as a mean pulmonary arterial pressure (mPAP) greater than 25 mmHg at rest or greater than 30 mmHg during exercise after ruling out other causes of pulmonary arterial hypertension [9]. Although the pathogenesis, clinical features, laboratory parameters, pathologic findings, and management of SLE–PH have been reported to be very similar to those of IPAH, there have been few direct comparisons of patients with these two conditions. To determine the similarity or dissimilarity of SLE–PH and IPAH, we compared clinical characteristics, hemodynamics at diagnosis, and survival in groups of these patients.
Materials and methods
Patients
We reviewed the medical records of 20 patients with SLE–PH, according to the American College of Rheumatology criteria [10], as well as those of 34 patients with IPAH at Asan Medical Center from January 1995 to October 2003.
All patients met the criteria of PH based on the National Institute of Health (NIH) guidelines [11].
Patients with SLE were excluded if they had conditions that could affect pulmonary artery pressure, such as left heart failure, pulmonary thromboembolism, congenital heart disease, valvular heart disease, obstructive or restrictive pulmonary disease, or liver cirrhosis.
Methods
The diagnostic criteria used in the NIH registry include a mean pulmonary artery pressure of more than 25 mmHg at rest or more than 30 mmHg with exercise. If there were no secondary causes of increased pulmonary artery pressure, it was defined as IPAH [11]. In addition, a right ventricular systolic pressure (RVSP) that exceeded 45 mmHg by echocardiography was defined as PH in patients who did not receive right cardiac catheterization. To estimate RVSP, the systolic right atrial–ventricular pressure gradient (PG) was calculated using the modified Bernoulli equation, \(\Delta P = 4V^{2},\)where ΔP is the pressure gradient and V is the tricuspid regurgitation maximal velocity (TRVmax) measured. An estimate of right atrial pressure, 10 mmHg, was added to the pressure gradient to calculate RVSP, which was considered equal to the systolic pulmonary arterial pressure (sPAP) in the absence of right ventricular outflow obstruction [12].
Swan–Ganz catheters were used for mPAP and cardiac output measurement during cardiac catheterization. The positive hemodynamic response by nitric oxide was defined as a reduction in pulmonary vascular resistance (PVR) and mPAP of at least 20% [13–15].
The clinical features, laboratory findings, chest X-rays, electrocardiogram (ECG) results, pulmonary function tests (PFT), pulmonary perfusion scans, echocardiographic findings, cardiac catheterization, serologic profiles at the time of diagnosis, and survival were compared in the groups of patients with SLE–PH and IPAH. In addition, these patients were divided according to their PG for comparison of clinical features and survival rates.
Statistical analysis
Continuous values are reported as mean±SD and compared using the Mann–Whitney U test and Student’s t test. Survival rates in the two groups were compared using the Kaplan–Meier method, and differences in duration of symptoms, duration of diagnosis of PH to death, and mean survival time were compared using the log-rank test. Values of p<0.05 were considered significant. All tests were performed using SPSS version 10.0 for Windows.
Results
Clinical characteristics of SLE–PH patients
Of the 725 patients diagnosed with SLE from January 1995 to September 2003 at the Asan Medical Center, 181 underwent echocardiography or right cardiac catheterization, and 20 were diagnosed with PH. Their demographic and clinical characteristics are presented in Table 1. Their mean age was 36.4 years, and all were women. The mean time between the diagnosis of SLE and PH was 30.8±28.4 months, and the median duration from symptoms of PH onset to diagnosis of PH was 13.0±4.71 months. All patients reported dyspnea during exercise, and 60% presented with Raynaud’s phenomenon. Physical examination revealed increased pulmonary component of the second heart sound (P 2) in eight patients (40%), increased systolic murmur in ten (50%), and hepatomegaly, which is indicative of right heart failure, in 11 (55%). The mean systemic lupus erythematosus disease activity index (SLEDAI) was increased to 14.25. Simple chest X-ray examination revealed cardiomegaly in 16 patients (80%).
ECG revealed right axis deviation and right ventricular hypertrophy in 14 patients (70%), and PFT showed that diffusing capacity was 68.9%. Pulmonary perfusion scan revealed diffuse patch defect in 11 patients (55%) and normal findings in five patients (25%) (Table 2). All patients were positive for antinuclear antibody (ANA), and 11 patients each were positive for rheumatoid factor (RF) and antiphospholipid antibody (APL). Eight of 20 patients with SLE had anti-ribonucleoprotein antibody. Reduced complement activity was observed in 17 patients (85%).
Hemodynamic findings are shown in Table 3. Echocardiograms revealed 3.93±0.58 m/sec of TRVmax and an average of 65.3 mmHg of PG. Pericardial effusion was present in 12 patients (60%). The 6-min walk test showed an average of 375.1 m. Right cardiac catheterization was performed on ten patients, in whom sPAP was increased to 72.1 mmHg and mPAP was increased to 50 mmHg, but pulmonary capillary wedge pressure was normal. Response to nitric oxide (NO) was observed in only one of these patients (10%). Of the 20 SLE–PH patients, nine (45%) were treated with cyclophosphamide.
Comparisons of the SLE–PH and IPAH patient groups
Clinical characteristics
Compared with the IPAH group, the SLE–PH group had a significantly shorter time from symptom onset to diagnosis of PH and more frequently showed Raynaud’s phenomenon. The other clinical characteristics were similar between the two groups (Table 1). Simple chest X-rays showed more frequent cardiomegaly in the SLE–PH group, but there were no significant differences in the other variables. ECG, PFT, and perfusion scans showed no differences between the two groups (Table 2). In contrast, ANA and RF were significantly higher in the SLE–PH group. None of the four SLE patients who did not have a perfusion scan had APL including lupus anticoagulant test, aCL antibody, or anti-beta2 GP-I antibody.
Hemodynamic features
Right cardiac catheterization was performed on ten patients in the SLE–PH group and on 29 patients in the IPAH group. The latter had significantly higher sPAP (75.8±15.1 mmHg vs 97.3±24.3 mmHg, p=0.013) and mPAP (50.0±13.5 mmHg vs 61.4±19.4 mmHg, p=0.049) than the SLE–PH group. The positivity of NO-response was significantly lower in the SLE–PH group, with one of ten patients (10%), than in the IPAH group, with five of 29 patients (17%). Echocardiograms showed that TRVmax was increased in both groups and that mean pressure gradient was higher in the IPAH group (76.7 mmHg) than in the SLE–PH group (65.3 mmHg), but the difference was not statistically significant. Arterial blood gas analysis (ABGA) showed more frequent hypoxemia (PaO2<80 mmHg) in the IPAH group (62%) than in the SLE–PH group (20%, p=0.004) (Table 3).
Time from PH diagnosis to death
The SLE–PH group had a significantly shorter time from diagnosis to death (10.0±1.34 months) compared to the IPAH group (23.0±7.29 months, log-rank test, p=0.0025).
The Cox-proportional hazard ratio (RR) was 2.559 (1.066–6.147, confidence interval).
Comparison of survival rates
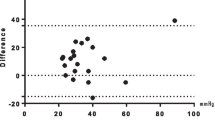
Follow-up of the 20 SLE–PH patients from the diagnosis of PH until October 2003 showed that 12 had died. Five patients died of right heart failure, four from sudden cardiac death due to arrhythmia (three ventricular fibrillation, one ventricular tachycardia), and three from infection. Their median survival duration was 13 months and their 1-, 3-, and 5-year survival rates were 50.5, 44.9, and 16.8%, respectively. In contrast, 11 of the 34 IPAH patients had died during this time. Their median survival duration was 66 months and their 1-, 3-, and 5-year survival rates were 76.5, 73.4, and 68.2%, respectively. These are significantly longer than those of the SLE–PH group (p=0.02) (Fig. 1). When we compared the survival rate of SLE–PH and IPAH patients with higher pressure gradients (>60 mmHg), we found that patients with SLE–PH had a markedly poorer 5-year survival (median, 4 months) than those with IPAH (median, 66 months, p=0.009). When we compared patients with lower pressure gradients (<60 mmHg), we again found that patients with SLE–PH had poorer 5-year survival (p<0.05).
Discussion
SLE often involves multiple visceral organs. For example, the lungs are preferentially affected in SLE, showing various symptoms, including pulmonary hypertension, pleuritis, diffuse interstitial lung disease, and pulmonary embolism [16]. IPAH has a reported prevalence of 1∼2 per 1 million in the USA and Europe, and 1,300 per 1 million during autopsy [6].
About 0.5 to 14% of the patients with SLE have PH, which is frequently mild or asymptomatic [3, 16]. Although PH was regarded as very rare for patients with SLE, the development of better diagnostic tools has shown a higher frequency [3, 7, 17]. In Korea, the prevalence of SLE–PH has not been reported to date. In this study, we determined the prevalence of SLE–PH in a single center as 20 per 725 (2.8%), which is lower than the prevalence rates in previous reports. These latter studies, however, may have overestimated the frequency of SLE–PH by including asymptomatic patients and borderline PH patients with RVSP 30 mmHg by echocardiogram [4, 18]. In contrast, we applied stricter criteria to patient selection, including only those patients with symptoms of PH and RVSP greater than 45 mmHg. Although only ten patients in the SLE–PH group received right cardiac catheterization and others only received echocardiogram, currently, using Doppler echocardiography to evaluate pulmonary artery pressure is considered a reliable method to detect PH in patients who did not receive right cardiac catheterization [19].
We found that the clinical characteristics of patients with SLE–PH were similar to those of patients with IPAH except for cardiomegaly due to pericardial effusion, as well as other SLE specific manifestations, including ANA and RF, Raynaud’s phenomenon, and serositis.
We found, however, that the time from symptom onset to diagnosis was significantly longer in the IPAH group than in the SLE–PH group. The nonspecific nature of symptoms in IPAH may have delayed its diagnosis, whereas active application of echocardiography to SLE patients in our hospital allowed earlier detection of PH in SLE. Due to the poor prognosis of patients with SLE–PH, active screening using echocardiography should be emphasized in patients with SLE.
The pathogenesis of PH has not been clearly established. In PH associated with connective tissue disease, deposition of immune complexes involving anti-DNA or RF antibodies and the associated inflammation and platelet dysfunction has been reported to lead to the dysfunction of pulmonary vascular endothelial cells, resulting in PH [2]. This has suggested that the combination of steroids and immunosuppressants may be effective therapy for PH associated with SLE [5, 20–24]. In this study, 17 (85%) SLE–PH patients had active SLE with reduced complement activity. We therefore suspected that in these patients, PH is due mainly to immunologic damage, and we treated nine of these patients with a combination of high-dose steroid and cyclophosphamide. APL is often mentioned as a cause of PH associated with pulmonary embolism [25–27]. Although perfusion scan didn’t show definite thromboembolism of main pulmonary artery, many scans disclosed patchy perfusion inhomogeneities, which are well-recognized as potentially indicative of old, partly recanalized thromboemboli. On the other hand, the rate of APL reported was similar in SLE–PH patients and SLE patients without PH [18]. We observed that 55% of SLE–PH patients were positive for APL antibody, a rate similar to those in earlier reports [28–30]. Thus, additional studies are needed to determine the role of APL antibody in the pathogenesis of PH.
In connective tissue diseases, PH is a life-threatening complication as well as a crucial factor in determining prognosis. In patients with symptomatic SLE–PH, the overall prognosis is especially poor, with a 2-year mortality rate exceeding 50% [6, 7]. In Korea, SLE–PH has been reported to be the third leading cause of death in patients with SLE [8]. We observed a median survival time of 13 months, and 1-, 3-, and 5-year survival rates of 50.5, 44.9, and 16.8%, respectively, all of which are lower than those previously reported. Direct comparison between our results and those in previous reports is difficult due to our use of different inclusion and exclusion criteria. We did show, however, that patients with SLE–PH had a higher mortality rate and a lower 5-year survival rate than patients with IPAH. In addition, the IPAH group had a higher mPAP than the SLE–PH group, although the latter had a higher mortality rate and a shorter time from PH diagnosis to death. When we regrouped PH patients by similar PAP to reduce any error of comparison resulting from PAP differences, we still found that the SLE–PH group had statistically significantly higher mortality and lower 5-year survival rate than the IPAH group.
The poorer prognosis in the SLE–PH group may have been due to the greater severity of underlying diseases. In addition, when we determined causes of death in the SLE–PH group, we found that five patients died of right heart failure, four from sudden cardiac death due to arrhythmia, and three from infection. Although the distribution was generally similar in patients with IPAH, more patients in the SLE–PH group died due to infection, suggesting that SLE–PH patients may be more susceptible to infection caused by SLE itself or immunosuppressant drugs such as cyclophosphamide.
In addition, although not statistically significant, the increased NO response in the IPAH group and the more frequent use of beraprost or warfarin in the IPAH group may have affected mortality.
SLE–PH and IPAH have been reported to be similar in pathogenesis, clinical manifestations, laboratory findings, and pathology [31–33]. Based on this, treatment of SLE–PH tends to be adopted from that of IPAH including the use of vasodilators, PGI2 analogues, bosentan, an oral nonselective endothelin receptor blocking agent, and anticoagulants, such as warfarin, all of which have been shown to prolong survival for patients with IPAH [34–36]. In addition, IPAH and PH associated with connective tissue diseases have been treated with epoprostenol (prostacyclin, prostaglandin I2), long-term infusions of which are associated with symptomatic and hemodynamic improvements and prolonged survival [37–41]. Recently, these conditions have been treated with iloprost, a derivative of prostacyclin with a longer half-life, which is actively applied through IV injection or inhalation [42–44]. Subsequent treatment with beraprost, an oral prostaglandin I2 agent, after IV epoprostenol treatment has been found effective [45, 46].
In this study, 11 SLE–PH patients were treated with beraprost and only three with warfarin. Although only three of the SLE patients were treated with warfarin in our study group, anticoagulation could be important in SLE–PH patients with an APL, as in IPAH patients [36]. However, this point needs to be verified in a larger study population in the future. Unfortunately, IV epoprostenol or Bosentan, currently the most reasonable treatment options, were not widely available for our study population.
Although 9 of the 20 SLE–PH patients were treated with an immunosuppressant, typically cyclophosphamide, there was no significant difference in survival between the treatment and nontreatment groups.
The significance of this study is that first, it applied strict inclusion criteria to SLE–PH, including only those symptomatic patients with RVSP greater than 45 mmHg.
Second, our study directly compared patients with IPAH and SLE–PH, who had similar demographics and clinical manifestations. Therefore, we established the objective evidence for similarity. Third, our study demonstrated that SLE–PH has a much poorer prognosis than IPAH, indicating the necessity of early diagnosis and more active treatment of the former.
Among the limitations of this study are its retrospective design and its survey of patients in a single center. Another limitation is that because most of the echocardiograms were performed on symptomatic patients and not on all SLE patients as a screening test, selection bias including more severe SLE patients could have occurred. Other limitations are that fewer right cardiac catheterizations were performed in the SLE–PH group than in the IPAH group and that warfarin and beraprost were used less frequently in the SLE–PH group than in the IPAH group. Although this difference was not statistically significant, it may have led to an overestimation of the difference in survival.
In summary, we have shown here that the prognosis of SLE patients with PH was much poorer than that of IPAH patients. The result suggests the necessity of early diagnosis and more active treatment of SLE patients with PH.
References
Perez HD, Kramer N (1981) Pulmonary hypertension in systemic lupus erythematosus: report of four cases and review of the literature. Semin Arthritis Rheum 11:177–181
Quismorio FP Jr, Sharma O, Koss M, Boylen T, Edmiston AW, Thornton PJ, Tatter D (1984) Immunopathologic and clinical studies in pulmonary hypertension associated with systemic lupus erythematosus. Semin Arthritis Rheum 13:349–359
Winslow TM, Ossipov MA, Fazio GP, Simonson JS, Redberg RF, Schiller NB (1995) Five-year follow-up study of the prevalence and progression of pulmonary hypertension in systemic lupus erythematosus. Am Heart J 129:510–515
Pan TL, Thumboo J, Boey ML (2000) Primary and secondary pulmonary hypertension in systemic lupus erythematosus. Lupus 9:338–342
Tanaka E, Harigai M, Tanaka M, Kawaguchi Y, Hara M, Kamatani N (2002) Pulmonary hypertension in systemic lupus erythematosus: evaluation of clinical characteristics and response to immunosuppressive treatment. J Rheumatol 29:282–287
Asherson RA, Hackett D, Gharavi AE, Harris EN, Kennedy HG, Hughes GR (1986) Pulmonary hypertension in systemic lupus erythematosus: a report of three cases. J Rheumatol 13:416–420
Asherson RA, Higenbottam TW, Dinh Xuan AT, Khamashta MA, Hughes GR (1990) Pulmonary hypertension in a lupus clinic: experience with twenty-four patients. J Rheumatol 17:1292–1298
Kim WU, Min JK, Lee SH, Park SH, Cho CS, Kim HY (1999) Causes of death in Korean patients with systemic lupus erythematosus: a single center retrospective study. Clin Exp Rheumatol 17:539–545
British Cardiac Society Guidelines and Medical Practice Committee (2001) Recommendations on the management of pulmonary hypertension in clinical practice. Heart 86(Suppl 1):I1–I13
Tan EM, Cohen AS, Fries JF, Masi AT, McShane DJ, Rothfield NF, Schaller JG, Talal N, Winchester RJ (1982) The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 25:1271–1277
Rich S, Dantzker DR, Ayres SM, Bergofsky EH, Brundage BH, Detre KM, Fishman AP, Goldring RM, Groves BM, Koerner SK et al (1987) Primary pulmonary hypertension. A national prospective study. Ann Intern Med 107:216–223
Murata I, Takenaka K, Yoshinoya S, Kikuchi K, Kiuchi T, Tanigawa T, Ito K (1997) Clinical evaluation of pulmonary hypertension in systemic sclerosis and related disorders. A Doppler echocardiographic study of 135 Japanese patients. Chest 111:36–43
Simonneau G, Galie N, Rubin LJ, Langleben D, Seeger W, Domenighetti G, Gibbs S, Lebrec D, Speich R, Beghetti M, Rich S, Fishman A (2004) Clinical classification of pulmonary hypertension. J Am Coll Cardiol 43:5S–12S
Sitbon O, Humbert M, Jagot JL, Taravella O, Fartoukh M, Parent F, Herve P, Simonneau G (1998) Inhaled nitric oxide as a screening agent for safely identifying responders to oral calcium-channel blockers in primary pulmonary hypertension. Eur Respir J 12:265–270
Ricciardi MJ, Knight BP, Martinez FJ, Rubenfire M (1998) Inhaled nitric oxide in primary pulmonary hypertension: a safe and effective agent for predicting response to nifedipine. J Am Coll Cardiol 32:1068–1073
Orens JB, Martinez FJ, Lynch JP 3rd (1994) Pleuropulmonary manifestations of systemic lupus erythematosus. Rheum Dis Clin North Am 20:159–193
Simonson JS, Schiller NB, Petri M, Hellmann DB (1989) Pulmonary hypertension in systemic lupus erythematosus. J Rheumatol 16:918–925
Li EK, Tam LS (1999) Pulmonary hypertension in systemic lupus erythematosus: clinical association and survival in 18 patients. J Rheumatol 26:1923–1929
Denton CP, Cailes JB, Phillips GD, Wells AU, Black CM, Bois RM (1997) Comparison of Doppler echocardiography and right heart catheterization to assess pulmonary hypertension in systemic sclerosis. Br J Rheumatol 36:239–243
Pines A, Kaplinsky N, Goldhammer E, Olchovsky D, Frankl O (1982) Corticosteroid responsive pulmonary hypertension in systemic lupus erythematosus. Clin Rheumatol 1:301–304
Morelli S, Giordano M, De Marzio P, Priori R, Sgreccia A, Valesini G (1993) Pulmonary arterial hypertension responsive to immunosuppressive therapy in systemic lupus erythematosus. Lupus 2:367–369
Groen H, Bootsma H, Postma DS, Kallenberg CG (1993) Primary pulmonary hypertension in a patient with systemic lupus erythematosus: partial improvement with cyclophosphamide. J Rheumatol 20:1055–1057
Sanchez O, Humbert M, Sitbon O, Simonneau G (1999) Treatment of pulmonary hypertension secondary to connective tissue diseases. Thorax 54:273–277
Gonzalez-Lopez L, Cardona-Munoz EG, Celis A, Garcia-de la Torre I, Orozco-Barocio G, Salazar-Paramo M, Garcia-Gonzalez C, Garcia-Gonzalez A, Sanchez-Ortiz A, Trujillo-Hernandez B, Gamez-Nava JI (2004) Therapy with intermittent pulse cyclophosphamide for pulmonary hypertension associated with systemic lupus erythematosus. Lupus 13:105–112
Padmakumar K, Singh RR, Rai R, Malaviya AN, Saraya AK (1990) Lupus anticoagulants in systemic lupus erythematosus: prevalence and clinical associations. Ann Rheum Dis 49:986–989
Martinuzzo ME, Pombo G, Forastiero RR, Cerrato GS, Colorio CC, Carreras LO (1998) Lupus anticoagulant, high levels of anticardiolipin, and anti-beta2-glycoprotein I antibodies are associated with chronic thromboembolic pulmonary hypertension. J Rheumatol 25:1313–1319
Colorio CC, Martinuzzo ME, Forastiero RR, Pombo G, Adamczuk Y, Carreras LO (2001) Thrombophilic factors in chronic thromboembolic pulmonary hypertension. Blood Coagul Fibrinolysis 12:427–432
Buchanan RR, Wardlaw JR, Riglar AG, Littlejohn GO, Miller MH (1989) Antiphospholipid antibodies in the connective tissue diseases: their relation to the antiphospholipid syndrome and forme fruste disease. J Rheumatol 16:757–761
Mayumi T, Nagasawa K, Inoguchi T, Yamauchi Y, Ishii Y, Tada Y, Umeda F, Niho Y (1991) Haemostatic factors associated with vascular thrombosis in patients with systemic lupus erythematosus and the lupus anticoagulant. Ann Rheum Dis 50:543–547
Cervera R, Khamashta MA, Font J, Sebastiani GD, Gil A, Lavilla P, Domenech I, Aydintug AO, Jedryka-Goral A, de Ramon E et al (1993) Systemic lupus erythematosus: clinical and immunologic patterns of disease expression in a cohort of 1,000 patients. The European working party on systemic lupus erythematosus. Medicine (Baltimore) 72:113–124
Rich S, Kieras K, Hart K, Groves BM, Stobo JD, Brundage BH (1986) Antinuclear antibodies in primary pulmonary hypertension. J Am Coll Cardiol 8:1307–1311
Yousem SA (1990) The pulmonary pathologic manifestations of the CREST syndrome. Hum Pathol 21:467–474
Humbert M, Monti G, Brenot F, Sitbon O, Portier A, Grangeot-Keros L, Duroux P, Galanaud P, Simonneau G, Emilie D (1995) Increased interleukin-1 and interleukin-6 serum concentrations in severe primary pulmonary hypertension. Am J Respir Crit Care Med 151:1628–1631
Ohar J, Polatty C, Robichaud A, Fowler A, Vetrovec G, Glauser F (1985) The role of vasodilators in patients with progressive systemic sclerosis. Interstitial lung disease and pulmonary hypertension. Chest 88:263S–265S
Chaouat A, Weitzenblum E, Higenbottam T (1996) The role of thrombosis in severe pulmonary hypertension. Eur Respir J 9:356–363
Rubin LJ, Badesch DB, Barst RJ, Galie N, Black CM, Keogh A, Pulido T, Frost A, Roux S, Leconte I, Landzberg M, Simonneau G (2002) Bosentan therapy for pulmonary arterial hypertension. N Engl J Med 346:896–903
Barst RJ, Rubin LJ, McGoon MD, Caldwell EJ, Long WA, Levy PS (1994) Survival in primary pulmonary hypertension with long-term continuous intravenous prostacyclin. Ann Intern Med 121:409–415
Shapiro SM, Oudiz RJ, Cao T, Romano MA, Beckmann XJ, Georgiou D, Mandayam S, Ginzton LE, Brundage BH (1997) Primary pulmonary hypertension: improved long-term effects and survival with continuous intravenous epoprostenol infusion. J Am Coll Cardiol 30:343–349
McLaughlin VV, Genthner DE, Panella MM, Rich S (1998) Reduction in pulmonary vascular resistance with long-term epoprostenol (prostacyclin) therapy in primary pulmonary hypertension. N Engl J Med 338:273–277
Robbins IM, Gaine SP, Schilz R, Tapson VF, Rubin LJ, Loyd JE (2000) Epoprostenol for treatment of pulmonary hypertension in patients with systemic lupus erythematosus. Chest 117:14–18
Horn EM, Barst RJ, Poon M (2000) Epoprostenol for treatment of pulmonary hypertension in patients with systemic lupus erythematosus. Chest 118:1229–1230
Gomez-Sanchez MA, de la Calzada CS, Gomez Pajuelo C, Tascon JC, Alonso M, Andreu J, Aranzana M, de la Fuente A (1991) Different hemodynamic responses between acute and chronic infusion of iloprost (prostacyclin-stable analogue) in severe pulmonary hypertension. Am Rev Respir Dis 144:1404–1405
Mok MY, Tse HF, Lau CS (1999) Pulmonary hypertension secondary to systemic lupus erythematosus: prolonged survival following treatment with intermittent low dose iloprost. Lupus 8:328–331
Hoeper MM, Schwarze M, Ehlerding S, Adler-Schuermeyer A, Spiekerkoetter E, Niedermeyer J, Hamm M, Fabel H (2000) Long–term treatment of primary pulmonary hypertension with aerosolized iloprost, a prostacyclin analogue. N Engl J Med 342:1866–1870
Saji T, Ozawa Y, Ishikita T, Matsuura H, Matsuo N (1996) Short-term hemodynamic effect of a new oral PGI2 analogue, beraprost, in primary and secondary pulmonary hypertension. Am J Cardiol 78:244–247
Ooiwa H, Miyazawa T, Yamanishi Y, Hiyama K, Ishioka S, Yamakido M (2000) Successful treatment of systemic lupus erythematosus and pulmonary hypertension with intravenous prostaglandin I2 followed by its oral analogue. Intern Med 39:320–323
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chung, SM., Lee, CK., Lee, E.Y. et al. Clinical aspects of pulmonary hypertension in patients with systemic lupus erythematosus and in patients with idiopathic pulmonary arterial hypertension. Clin Rheumatol 25, 866–872 (2006). https://doi.org/10.1007/s10067-006-0206-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-006-0206-5