Abstract
We hypothesized that patients with sepsis and AKI, especially patients without preserved renal function, and treated with continuous veno-venous hemodiafiltration (CVVHDF), have lower risk for mortality than patients treated with continuous veno-venous hemofiltration (CVVH). Patients were included if they fulfilled the diagnosis of severe sepsis or septic shock, suffered AKI and received continuous renal replacement therapy (CRRT) in intensive care unit. There were 62 patients treated by CVVH and 75 treated by CVVHDF. Mean survival time was longer in CVVHDF group with oliguric/anuric patients than in CVVH group. CVVH, and not classic risk factors, was associated with higher overall mortality in oliguric/anuric patients. In the linear regression model, hourly urine output was the strongest and positive predictor of longer survival. CVVHDF is according to our results a CRRT modality of choice for the treatment and lower mortality of septic patients with AKI where renal function is no longer preserved. CRRT has been associated with improved renal recovery, but it should be started earlier in AKI evolution with still preserved hourly urine output which is the most sensitive and prognostic marker of survival in septic patients with AKI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sepsis is a serious medical condition characterized by a whole-body inflammatory state (systemic inflammatory-response syndrome, SIRS) and the presence of a known or suspected infection that has severe consequences, including multiple organ failure (MOF). The clinical diagnosis of sepsis requires finding a focus of infection as well as at least two signs of SIRS that comprise abnormal body temperature (higher than 38 °C or less than 36 °C), heart rate >90 beats/min, respiration >20 breaths/min or arterial partial pressure of CO2 <32 mmHg, and deranged white blood cell counts (greater than 12 × 103/mm3, less than 4 × 103/mm3, or greater than 10% immature bands [1]. The progress of sepsis in severe sepsis is characterized by failure of organ systems and can be identified as an acute change in total Sequential Organ Failure Assessment (SOFA) score ≥2 points consequent to the infection. Septic shock is a subset of sepsis in which underlying circulatory and cellular/metabolic abnormalities are profound. Patients with septic shock can be identified with a clinical construct of sepsis with persisting hypotension requiring vasopressors to maintain mean arterial pressure (MAP) ≥65 mmHg and having a serum lactate level >2 mmol/L despite adequate volume resuscitation [2, 3].
Acute kidney injury (AKI) is a frequent and serious complication of sepsis in intensive care unit (ICU) patients, in all age groups [4]. Moreover, there is strong evidence that sepsis and septic shock are the most important causes of AKI in critically ill patients, account for 50% or more of cases of AKI in ICUs, and associate with a very high mortality [5, 6].
The pathophysiology of AKI in sepsis is complex and multi-factorial and includes intrarenal hemodynamic changes, endothelial dysfunction, infiltration of inflammatory cells in the renal parenchyma, intraglomerular thrombosis, and obstruction of tubules with necrotic cells and debris [5]. A growing body of evidence now suggests that the sepsis-induced immune responses involve the activation, in a sequential manner, of both pro- and anti-inflammatory mechanisms [7].
Some studies suggest that continuous renal replacement therapy (CRRT) is associated with increased ability to clear inflammatory mediators [5, 6] from septic patients with AKI. There are two methods of clearance in continuous veno-venous hemodiafiltration (CVVHDF), diffusion and convection, while only convection in continuous veno-venous hemofiltration (CVVH). Convective modalities (hemofiltration) may provide better clearance of middle molecular weight solutes like cytokines compared with diffusive modalities [7]. Nevertheless, there are only few studies examining the impact of different CRRT modalities, especially CVVH and CVVHDF on survival in septic patients with AKI.
As sepsis associated with AKI has an increased short-term mortality and increased circulating cytokines mediate the development of septic shock and sepsis-associated AKI, we hypothesized that patients with sepsis and AKI and treated with CVVHDF have lower risk for mortality than other patients treated with CVVH. Additionally, because there are no present data on possible differences in survival of oligoanuric and non-oliguric septic patients with AKI, we hypothesized that CVVHDF, a combination of two methods, is a CRRT modality of choice for the treatment and lower mortality of septic patients with AKI where renal function is no longer preserved. To test this hypotheses, we analyzed clinical course of the patients through the hospitalization and survival rate after follow-up.
Materials and methods
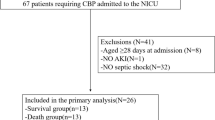
This was a retrospective, longitudinal follow-up study for 12 months duration. In total, 137 patients were recruited from the ICUs in University Hospital Center Zagreb, Croatia.
Patients were included if they fulfilled the diagnosis of severe sepsis or septic shock, suffered AKI and received CRRT in ICU. Sepsis was defined as the presence of suspected or documented infection together with systemic inflammatory response syndrome while septic shock was defined as a status of sepsis with acute circulatory failure according to the American College of Chest Physicians/Society of Critical Care Medicine/European Society of Intensive Care Medicine criteria [1]. Other inclusion criteria included renal dysfunction (defined on the basis of an estimated creatinine clearance—eGFR, mL/min was calculated daily using the simplified Modification of Diet in Renal Disease (MDRD) equation [8]. Acute kidney injury was defined by a modified definition of the Kidney Disease: Improving Global Outcomes (KDIGO) AKI Workgroup, harmonizing differences between the Risk, Injury, Failure, Loss of kidney function, and End-stage kidney disease (RIFLE) and the Acute Kidney Injury Network (AKIN) definitions [9]. Those with age less than 18 years old, presence of chronic kidney disease stage 5 (GFR <15 mL/min per 1.73/m2), end-stage renal failure on long-term dialysis or those treated with RRT before ICU admission were excluded.
Hourly fluid input and urine output data were extracted from ICU charts. At admission and after each treatment documented body weight was used. Patient follow-up continued until the last enrolled patient reached the 365-day time point. Each patient underwent a complete clinical and laboratory examination at the time of admission and during hospitalization. Selection of CVVH and CVVHDF as the primary treatment method was the choice of the involved nephrologist. Generally, patients with lower eGFR levels and a need of diffusion for reduction of serum creatinine and blood urea nitrogen (BUN) or potassium levels were referred for CVVHDF. Both modalities, CVVH and CVVHDF, were performed for each patient using the Prismaflex® CRRT and M100 membrane filters (Baxter Int., Deerfield, Illinois, USA). The patients have been followed by telemetry unit. A patient to nurse ratio was 2:1. Forty-five percent of patients were treated with CVVH and 55% with CVVHDF. Data for each patient concerning UF rates, duration of each treatment, blood, dialysate and replacement fluid pump flows and total number of treatments were obtained. Blood flow rate was maintained at between 200 and 250 mL/min, according to blood-access function and desired UF rates. Anti-coagulation was performed according to patient condition, either with low-molecular weight heparin or heparin-free anti-coagulation. The hemofilter and the extracorporeal circuit were replaced every 72 h. Ultrafiltration rates were prescribed depending on patients cardiac status, fluid overload and hourly urine output. The rates of reinfusion and dialysate were prescribed aiming at the dose of dialysis >35 mL/kg/h.
Discontinuation of treatment and discharge has been done by the treating intensive care physician (after consultation with nephrologist), based on clinically assessed volume status, symptoms, and objective data (including laboratory values). Plasma creatinine, blood urea nitrogen (BUN), serum sodium and potassium, C-reactive protein, serum albumin and white cell blood count were analyzed from blood samples at start and at the end of each treatment. Systolic and diastolic blood pressure were measured before, during and after each treatment (and in the meantime, as it was indicated). A direct measurement of volume overload has been performed using central venous catheter (CVP, expressed in mmHg).
Ethical approval: All subjects enrolled in this research have given their informed consent, which has been approved by my institutional committee on human research, and this protocol has been found acceptable by them.
Statistical analysis was performed using SPSS version 23.0 (IBM Corp., USA). Normality of data distribution was tested using Kolmogorov–Smirnov test. Preliminary analyses were performed to ensure no violation of the assumptions of normality, linearity and homoscedasticity. Descriptive characteristics were expressed as numbers and frequencies. Correlations were obtained using Pearson’s test for normally distributed variables and Spearman rank correlation for non-normally distributed variables. Normally distributed variables were presented as means + standard deviations and Student’s t test for independent samples was used for comparisons between two groups. Non-normally distributed data were presented as median and interquartile range and Mann–Whitney U test was used in comparison between two groups. Baseline-to-follow-up comparisons were done using Student’s t test for paired samples and Wilcoxon test. Categorical variables were compared using χ 2 test. Survival analysis was done with Kaplan–Meier curves which were tested with log-rank test while hazard ratios were estimated with Cox proportional hazards regression. Multiple linear regression was used to explore the influence of different variables on survival, while logistic regression was used for categorical dependent variables. We constructed three regression models to assess independent associations of multiple independent variables with patients survival. In Model 1, we included variables known to be associated with increased mortality and related to dialysis: age, body weight at baseline and the end of the treatment, duration of dialysis, hourly urine output, sex and the presence of diabetes and hypertension (yes/no). Model 2 included, in addition to all variables in Model 1 those further related to the dialysis: serum creatinine, BUN, ultrafiltration rate and central venous pressure at baseline and end of the treatment. Model 3 was additionally adjusted for established laboratory parameters of sepsis and chronic disease: c-reactive protein and serum albumins. A p value <0.05 (two-sided tests) was considered significant.
Results
There were 62 patients treated by CVVH (37/59.6%/males) and 75 CVVHDF-treated patients (42/56.0%/males) at the beginning of the study. The follow-up completed 44 CVVH-treated patients and 45 CVVHDF-treated patients. Demographic, laboratory and clinical characteristics of patients treated with CVVH and CVVHDF at start and end of the treatments are demonstrated in Table 1. There were no differences in age and gender between CVVH and CVVHDF groups and with no differences in percentage of arterial hypertension or diabetes. No significant differences were observed in body weight, duration of hospitalization and number of dialysis treatments both at start and end of the treatments. Patients treated with CVVH had bigger reinfusion and ultrafiltration rates (UFR) than CVVHDF patients (p < 0.05). The standard dialysate flow rate for patients treated with CVVHDF was 1309 mL/h. The initialization of treatments was at significantly higher values of serum creatinine and BUN in CVVHDF patients while there was no difference in hourly urine output between two groups of patients. As shown in Table 1 at start and at the end of the treatments, there were no differences in brachial BP values and CVP values as well as in laboratory markers of sepsis, CRP, WBC and albumins. There was no difference in survival between two groups of patients. When patients were divided by hourly urine output on oliguric/anuric and non-oliguric, we did not find any significant differences between two groups of patients except longer survival in non-oliguric group. On univariate analysis survival was in all patients negatively correlated with age (r = −0.329; p < 0.001), duration of dialysis (r = −0.193; p = 0.024) and serum creatinine (r = −0.209; p = 0.014) at the end of the treatments and positively with hourly urine output (r = 0.573; p < 0.001) and serum albumins (r = 0.172; p = 0.044). In oliguric/anuric patients, we did not find any significant correlations between survival and other variables. In all three linear regression models hourly urine output was the strongest and positive predictor of longer survival (β = 0.492, β = 0.496 and β = 0.492, all p < 0.001) (see Table 2). Additionally, in Model 1 (adjusted R 2 = 0.395) age (β = −0.282, p < 0.001) and duration of dialysis (β = −0.188, p = 0.007) showed negative association with survival. In Model 2 (adjusted R 2 = 0.413) age (β = −0.266, p < 0.001) and duration of dialysis (β = −0.217, p = 0.003) were negatively associated with survival. Model 3 (adjusted R 2 = 0.403) showed negative significant associations of survival with age (β = −0.266, p < 0.001) and duration of dialysis (β = 0.0.216, p = 0.004). The patients were followed for 12 months, 21 CVVH and 27 CVVHDF patients survived. Thirty-one patients have died from multi-organ failure caused by sepsis and ten patients have died from heart failure in the CVVH group while 33 patients have died from multi-organ failure caused by sepsis and 15 patients have died from heart failure in the CVVHDF group of patients. There was no difference in mean survival time between CVVH and CVVHDF patients [280.1 (95% CI 249.9, 311.6) vs. 274.7 (95% CI 239.9, 310.6) days] (Fig. 1). Demographic, laboratory and clinical characteristics of oliguric/anuric patients with treated with CVVH and CVVHDF are demonstrated in Table 3. There were no differences in age, gender and percentage of arterial hypertension and diabetes between CVVH and CVVHDF groups. There were no differences in dialysis parameters between two groups. The initialization of treatments was at significantly higher values of serum creatinine in CVVHDF patients (p = 0.03). Mean survival time was longer in CVVHDF group with oliguric/anuric patients than in CVVH group [110.4 (95% CI 53.8, 167.1) vs. 22.9 (95% CI 0.9, 51.2) days, log-rank p = 0.006] (Fig. 2). All non-oliguric patients had a significantly longer survival time compared to oliguric/anuric patients group [229.5 (95% CI 199.9, 259.1) vs. 74.2 (95% CI 36.7, 111.6) days, log-rank p < 0.001]. Non-oliguric patients treated with CVVH had significant longer survival than oliguric/anuric patients as well as patients treated with CVVHDF modality (both log-rank p < 0.001). CVVH [HR 2.06 (0.98, 4.32)] and not classic risk factors as age, dialysis parameters and inflammatory marker levels were associated with higher overall mortality in oliguric/anuric patients while in all groups of patients only age [HR 1.04 (1.02, 1.06)] was associated with higher overall mortality. We have not find significant differences in survival time in non-oliguric patients treated with CVVH and CVVHDF (Fig. 3) as well when patients were divided by different dose of dialysis and hourly urine output. There were no differences in renal survival between CVVH and CVVHDF in survived patients. Renal outcome transitioned to chronic hemodialysis in four patients in CVVH group and three patients in CVVHDF group.
Discussion
Sepsis and septic shock remain the most important cause of AKI in critically ill patients and septic-associated AKI. They account for approximately 50% of cases of AKI in the ICU [10,11,12], complicate between 15 and 20% of all ICU admissions with severe septic-associated AKI, and are responsible for triggering renal replacement therapy in 2–3% of all ICU admission [13, 14]. Mortality in patients with sepsis and AKI is still very high (between 40 and 55%), as it was demonstrated by two recent large studies [15, 16]. When compared with AKI of nonseptic origin, septic AKI patients have a significantly and unacceptably high mortality [17]. Unlike to previous reviews, AKI is a relatively common cause of long-term mortality and development of chronic renal failure (including end-stage renal failure, ESRD). There are only few present data comparing different CRRT modalities, namely CVVH and CVVHDF for treatment of septic patients with associated AKI.
In this study, we did not find significant difference in survival between septic patients with associated AKI treated with CVVH and CVVHDF at the end of the follow-up period (Fig. 1). To our knowledge, this is in agreement with only one present study [18]. Although patients treated with CVVH had higher reinfusion and UF rates than CVVHDF patients, treatments were initiated at significantly higher values of serum creatinine and BUN in CVVHDF patients with no difference in hourly urine output between two groups of patients (Table 1). Treatment was initiated at similar levels of sepsis parameters in both groups of patients. Patients treated with CVVHDF had a significant decrease in serum creatinine and BUN levels at the end of the follow-up compared to CVVH patients as a sign of combination of two basic principles of dialysis, convection and diffusion.
Hourly urine output is a sensitive and specific biomarker that provides an early warning signal for AKI and higher mortality [19, 20]. The hourly urine output in our study was a significant and independent predictor of longer survival in all patients with the same association present when they were divided by hourly urine output in non-oliguric subgroup. Regarding our results, serum creatinine and BUN were not significant predictors of better survival. When divided only by hourly urine output, patients with urine output <10 mL/h did not survived longer compared to patients with urine output >10 mL/h.
Although CRRT removes pro- and anti-inflammatory cytokines, outcomes do not seem to be affected regardless of the dose applied [21, 22] which was the same as the results in our study.
When divided on subgroups by hourly urine output and different CRRT modality, significantly higher number of patients with oliguria/anuria treated with CVVHDF survived compared to patients treated with CVVH (Fig. 2). Interestingly, there was no difference in survival in non-oliguric patients treated with different CRRT modalities (Fig. 3).
Sepsis is characterized by release of excessive amounts of pro-inflammatory cytokines in the circulation which could be downregulated with the CRRT by nonspecific extracorporeal removal of cytokines and other mediators [21,22,23]. Some studies indicate that cytokine removal with current CRRT methods and synthetic membranes is more convective than diffusive [24, 25] which is in contrast to our findings. The results from Graziani et al. [26] suggested that in septic patients with preserved diuresis some pro-inflammatory cytokines were removed from the plasma and non-oliguric patients had a better prognosis than oliguric/anuric patients. No difference in survival between non-oliguric septic patients treated with CVVH and CVVHDF could be observed through the cytokine removal from the plasma due to still preserved diuresis while in the other group of patients, kidneys lost the function of cytokine removal. It is possible that cytokine accumulation was better controlled with the combination of convection and diffusion, which is in contrast with previous results, especially when taking into account the fact that the improvement of eGFR and, therefore, renal function was more pronounced in CVVHDF patients. Furthermore, CVVH and not CVVHDF was associated with higher overall mortality in oliguric/anuric patients. However, this hypothesis needs further investigations.
When we compared patients with different hourly urine output, all oliguric/anuric patients and those treated with different CRRT methods survived significantly shorter compared to non-oliguric patients. This is an additional argument for our hypothesis of cytokine removal by still preserved renal hourly urine output in septic patients with AKI.
This is the first study which analyzed the impact of different CRRT modalities (CVVH vs. CVVHDF) and hourly urine output on survival of septic patients with AKI. Our results on better survival of septic oliguric/anuric patients treated with CVVHDF are in line with our hypothesis that CVVHDF, a combination of two methods, is a CRRT modality of choice for the treatment and lower mortality of septic patients with AKI where renal function is no longer preserved. The present study suggests that the use of CVVHDF in septic non-oliguric patients is not associated with improved survival when compared with CVVH. Furthermore, the cytokine reduction in septic patients could not be only achieved by CRRT, especially when renal function is still preserved and kidneys have the ability of cytokine removal from plasma. Based on our results, hourly urine output is the most sensitive and prognostic marker of survival in septic patients with AKI.
Our work has several limitations. First, the study was an observational, non-randomised performed in a single centre and it could be limited by a relatively small sample size. Second, cytokine levels were not measured in this study. Plasma levels of TNF alpha, IL-1b, IL-6 and IL-8, related to pro-inflammatory state have a greater accuracy than clinical signs for the diagnosis of sepsis. The effect of cytokine removal by CVVHDF, especially in oliguric/anuric patients, could not be assessed directly but only by clinical signs and better survival compared to patients treated with CVVH. Third, all the included patients already had a presence of AKI. Some could argue why we did not include patients treated with CVVHD and, therefore, analyzed the impact on survival of three different CRRT modalities. In patients with AKI and a clinical signs of sepsis, convection, and not diffusion, has been considered a method of choice [27, 28] and we wanted to analyze only the addition of diffusion to convection. Furthermore, most patients treated with CVVHD had a presence of previous chronic kidney disease so they were not eligible for this study. Fourth, patient selection bias may play a role in choosing the dialysis mode in which patients with higher serum creatinine levels received CVVHDF.
Conclusion: The identification of high-risk patients is crucial in influencing outcome of the patients with sepsis-induced AKI. CVVHDF, a combination of two methods, is according to our results a CRRT modality of choice for the treatment and lower mortality of septic patients with AKI where renal function is no longer preserved. Although rare, nonspecific treatments for septic AKI, early antibiotic administration, avoidance of hypotension (through fluid administration or vasopressors), nephrotoxic agents and fluid overload can minimize AKI risk. Continuous renal replacement therapy, based on our results, should be started earlier in AKI evolution with still preserved hourly urine output which is the most sensitive and prognostic marker of survival in septic patients with AKI. Future trials should be designed to identify high-risk patients with early injury and focus on targeted therapy.
References
Bone RC, Balk RA, Cerra FB, et al. American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference: definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med. 1992;20:864–74.
Vincent J-L, Opal SM, Marshall JC, Tracey KJ. Sepsis definitions: time for change. Lancet. 2013;381:774–5.
Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA. 2016;315:801–10.
Lafrance JP, Miller DR. Acute kidney injury associates with increased long-term mortality. J Am Soc Nephrol. 2010;21:345–52.
Zarjou A, Agarwal A. Sepsis and acute kidney injury. J Am Soc Nephrol. 2011;22:999–1006.
Uchino S, Kellum JA, Bellomo R, Doig GS, Morimatsu H, Morgera S, Schetz M, Tan I, Bouman C, Macedo E, Gibney N, Tolwani A, Ronco C. Acute renal failure in critically ill patients: a multinational, multicenter study. JAMA. 2005;294:813–8.
Wan L, Bagshaw SM, Langenberg C, Saotome T, May C, Bellomo R. Pathophysiology of septic acute kidney injury: what do we really know? Crit Care Med. 2008;36:S198–203.
Smilde TD, van Veldhuisen DJ, Navis G, Voors AA, Hillege HL. Drawbacks and prognostic value of formulas estimating renal function in patients with chronic heart failure and systolic dysfunction. Circulation. 2006;114:1572–80.
Kidney Disease Outcomes Quality Initiative. KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl. 2012;2:8.
Andrikos E, Tseke P, Balafa O, Cruz DN, Tsinta A, Androulaki M, et al. Epidemiology of acute renal failure in ICUs: a multi-center prospective study. Blood Purif. 2009;28:239–44.
Bagshaw SM, George C, Bellomo R. ANZICS database management committee early acute kidney injury and sepsis: a multicentre evaluation. Crit Care. 2008;12:R47.
Alobaidi R, Basu RK, Goldstein SL, Bagshaw SM. Sepsis-associated acute kidney injury. Semin Nephrol. 2015;35:2–11.
Bagshaw SM, Uchino S, Bellomo R, Morimatsu H, Morgera S, Schetz M, et al. Septic acute kidney injury in critically ill patients: clinical characteristics and outcomes. Clin J Am Soc Nephrol. 2007;2:431–9.
Prowle JR, Bellomo B. Sepsis-associated acute kidney injury: macrohemodynamic and microhemodynamic alterations in the renal circulation. Semin Nephrol. 2015;35:64–74.
RENAL Study Investigators, Bellomo R, Cass A, Cole L, Finfer S, Gallagher M, et al. Intensity of continuous renal- replacement therapy in critically ill patients. N Engl J Med. 2009;361:1627–38.
Palevsky PM, Zhang JH, O’Connor TZ, Chertow GM, Choudhury D, et al. Intensity of renal support in critically ill patients with acute kidney injury. N Engl J Med. 2008;359:7–20.
Silvester W, Bellomo R, Cole L. Epidemiology, management, and outcome of severe acute renal failure of critical illness in Australia. Crit Care Med. 2001;29:1910–5.
AlEnezi F, Alhazzani W, Ma J, Alanazi S, Salib M, Attia M, Thabane L, Fox-Robichaud A. Continuous venovenous hemofiltration versus continuous venovenous hemodiafiltration in critically ill patients: a retrospective cohort study from a Canadian tertiary centre. Can Resp J. 2014;21:176–80.
Prowle JR, Liu YL, Licari E, Bagshaw SM, Egi M, Haase M, et al. Oliguria as predictive biomarker of acute kidney injury in critically ill patients. Crit Care. 2011;15:R172.
Macedo E, Malhotra R, Claure-Del Granado R, Fedullo P, Mehta RL. Defining urine output criterion for acute kidney injury in critically ill patients. Nephrol Dial Transpl. 2011;26:509–15.
Joannes-Boyau O, Honore PM, Perez P, Bagshaw SM, Grand H, Canivet JL, et al. High-volume versus standard-volume haemofiltration for septic shock patients with acute kidney injury (IVOIRE study): a multicentre randomized controlled trial. Intensive Care Med. 2013;39:1535–46.
Zhang P, Yang Y, Lv R, Zhang Y, Xie W, Chen J. Effect of the intensity of continuous renal replacement therapy in patients with sepsis and acute kidney injury: a single-center randomized clinical trial. Nephrol Dial Transplant. 2012;27:967–73.
Grootendorst AF. The potential role of hemofiltration in the treatment of patients with septic shock and multiple organ dysfunction syndrome. Adv Renal Replace Ther. 1994;1:176–84.
Wakabayashi Y, Kamijou Y, Soma K, Ohwada T. Removal of circulating cytokines by continuous haemofiltration in patients with systemic inflammatory response syndrome or multiple organ dysfunction syndrome. Br J Surg. 1996;83:393–4.
Braun N, Giolai M, Rosenfeld S, Banzhaff W, Fretschner R, Weinstock C, Erley C, Muller GA, Warth H, Northoff H, Risler T. Clearance of interleukin-6 during continuous veno-venous hemofiltration in patients with septic shock: a prospective, controlled clinical study [Abstract]. J Am Soc Nephrol. 1993;4:336.
Graziani G, Bordone G, Bellato V, Finazzi S, Angelini C, Badalamenti S. Role of the kidney in plasma cytokine removal in sepsis syndrome: a pilot study. J Nephrol. 2006;19:176–82.
Goldfarb S, Golper TA. Proinflammatory cytokines and hemofiltration membranes. J Am Soc Nephrol. 1994;5:228–32.
Ronco C, Tetta C, Lupi A, Galloni E, Bettini MC, Sereni L, Mariano F, DeMartino A, Montrucchio G, Camussi G, La Greca G. Removal of platelet-activating factor in experimental continuous arteriovenous hemofiltration. Crit Care Med. 1995;23:99–107.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Rights and permissions
About this article
Cite this article
Premuzic, V., Basic-Jukic, N., Jelakovic, B. et al. Differences in CVVH vs. CVVHDF in the management of sepsis-induced acute kidney injury in critically ill patients. J Artif Organs 20, 326–334 (2017). https://doi.org/10.1007/s10047-017-0970-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10047-017-0970-9