Abstract
To investigate the efficacy and safety of continuous blood purification (CBP) in neonates with septic shock and acute kidney injury (AKI). This retrospective study was conducted at two tertiary care children's hospitals between January 2015 and May 2022. A total of 26 neonates with septic shock and AKI were included in this study, with a mortality rate of 50%. Fourteen neonates (53.8%) received continuous veno-venous hemodiafiltration, and 12 (46.2%) received continuous veno-venous hemofiltration. Compared with the indices before CBP, urine output increased 12 h after CBP initiation (P = 0.003) and serum creatinine decreased (P = 0.019). After 24 h of CBP, blood urea nitrogen had decreased (P = 0.006) and mean arterial pressure had increased (P = 0.007). At the end of CBP, the vasoactive-inotropic score and blood lactate were decreased (P = 0.035 and 0.038, respectively) and PH was increased (P = 0.015). Thrombocytopenia was the most common complication of CBP.
Conclusion: CBP can efficiently maintain hemodynamic stability, improve renal function, and has good safety in neonates with septic shock and AKI. However, the mortality rate remains high, and whether CBP improves the prognosis of neonates with septic shock and AKI remains unclear.
What is Known: • Over 50% of children with septic shock have severe AKI, of which 21.6% required CBP. • The clinical application of CBP in septic shock has attracted increasing attention. | |
What is New: • CBP can efficiently maintain hemodynamic stability, improve renal function, and has good safety in neonates with septic shock and AKI. • The mortality rate in neonates with septic shock and AKI receiving CBP remains high. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Septic shock is the main cause of death in critically ill neonates. Approximately 2,202 (95% confidence interval [CI] 1099–4360) neonatal sepsis cases are reported per 100,000 live births, with mortality rates between 11 and 19% [1]. Extrapolating to a global scale, we estimate an incidence of 3.0 million neonatal sepsis cases worldwide. Moreover, neonatal septic shock mortality is reported to be as high as 70–80% [2]. Although statistics confirm that sepsis and septic shock are common and frequently fatal conditions, effective treatments are lacking.
Acute kidney injury (AKI) is an independent cause of death in sepsis, and over 50% of children with septic shock have severe AKI, of which 21.6% required continuous blood purification (CBP) treatment [3, 4]. In recent years, through continuous technical improvements, CBP has gradually shifted from primarily being used for renal replacement to also being used for the treatment of non-renal diseases. Moreover, the clinical application of CBP in septic shock has attracted increasing attention [5]. However, reports on the efficacy and safety of CBP in neonates with septic shock and AKI are rare, with only a few studies with more than 20 cases. In this study, we enrolled 26 neonates with septic shock and AKI who received CBP at two large tertiary children's hospitals in China. Clinical characteristics were analyzed, and hemodynamic indices and renal function electrolytes were compared before and after CBP.
Materials and methods
After screening using the hospital's electronic medical record system, this retrospective cohort study was conducted on neonates receiving CBP who were admitted to the NICU of Quanzhou Maternity and Children’s Hospital and Shanghai Children’s Hospital between January 1, 2015, and May 31, 2022. The inclusion criteria were as follows: (i) aged < 28 days at admission, (ii) receiving CBP during hospitalization, and (iii) diagnoses of septic shock and AKI. The exclusion criteria were as follows: (i) aged ≥ 28 days at admission, (ii) septic shock without AKI, and (iii) incomplete clinical data. All data including demographic information, diagnosis, vital signs, laboratory results, medication, and CBP data were recorded. This study was approved by the Medical Ethics Committee of Quanzhou Maternity and Children's Hospital and Shanghai Children's Hospital (2020R064-E02), and written informed consent was obtained from the patients’ families.
Septic shock [6] was defined as severe infection leading to cardiovascular dysfunction (including hypotension, treatment with vasoactive medication, or impaired perfusion). AKI was diagnosed and staged based primarily on changes in blood creatinine levels and urine output [7] (Online Resource 1).
The Neonatal Critical Illness Score (NCIS), developed in China in 2001, was used to evaluate the severity of illness and involves 10 individual indicators (Online Resource 2). The vasoactive-inotropic score (VIS) was calculated using the following equation: VIS = 1 × dopamine (µg/kg/min) + 1 × dobutamine (µg/kg/min) + 100 × epinephrine (µg/kg/min) + 100 × norepinephrine (µg/kg/min) + 10 × milrinone (µg/kg/min) + 10,000 × vasopressin (u/kg/min) + 50 × levosimendan (µg/kg/min) [8].
Indications for CBP included fluid overload (> 10%), AKI stage 2 or above, serum creatinine (SCr) level, electrolyte disturbances, or a nonreactive internal environment to conventional therapies. Fresenius Multifiltrate hemofiltration machines with an Ultraflux AV paed filter (Fresenius Medical Care Co., Bad Homburg, Germany) or Plasauto iQ21 hemofiltration machines with an AEF-03 filter (Asahi Kasei Medical Co., Tokyo, Japan) were used. The circuit was flushed with packed red blood cells before being put on standby. Central venous catheters, including single and double-lumen catheters, were percutaneously placed along the right internal jugular, bilateral femoral, umbilical, or subclavian veins. The flow rates of CBP were set at 3–5 mL/kg/min for blood flow, 20–30 mL/kg/h for the replacement fluid, 15–25 mL/m2/min for the dialysate, and 2–5 mL/kg/h for the ultrafiltrate. Heparin was used as an anticoagulant to maintain an activated clotting time of 180–220 s and an active partial thromboplastin time of 80–120 s.
All statistical analyses were performed using SPSS software (version 20.0; IBM Corporation, Armonk, NY, USA). Measurement data are presented as medians (interquartile range (IQR)). Two-group and multi-group comparisons were performed using Wilcoxon and Kruskal–Wallis tests, respectively. Count data are presented as cases (%), and Fisher's exact test was used for comparison between the groups. A P-value < 0.05 was considered statistically significant.
Results
General clinical data of the neonates
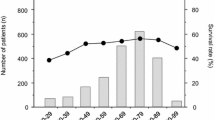
A Ntotal of 26 neonates with septic shock and AKI were included; the selection process flow chart is shown in Fig. 1. Nineteen patients (73.1%) were male and nine (34.6%) were premature. The median (IQR) age at admission was 1 (1–6) d, gestational age was 39 (35–40) weeks, birth weight was 3175 (2865–3455) g, and 5-min Apgar score was 10 (8–10). The median (IQR) NCIS was 69 (62.5–77.5) and the AKI stage was 2 (2–3). All children were treated with vasoactive drugs. The median (IQR) VIS was 73.0 (38.8–282.5), and 24 children (92.3%) required mechanical ventilation (Online Resource 3).
Septic shock-related hemodynamic indices
Before CBP, mean arterial pressure (MAP) was low [40.0 (IQR 34.5–48.0) mmHg], VIS was high [73.0 (IQR 38.8–282.5)], PH was decreased [7.21 (IQR 7.09–7.35), and blood lactate was increased [13.50 (IQR 6.95–20.08) mmol/L] in neonates with septic shock and AKI. Compared with before CBP, MAP 24 h after CBP initiation was increased [49.5 (IQR 44.3–63.3), P = 0.007]. Additionally, after CBP, VIS and blood lactate were decreased [9.0 (IQR 0.0–175.0), P = 0.035 and 3.90 (IQR 1.60–12.93) mmol/L, P = 0.038, respectively], whereas PH was increased [7.36 (IQR 7.28–7.40), P = 0.015] (Fig. 2).
Renal function and electrolytes
As shown in Fig. 3, the urine volume before CBP was 0.20 (IQR 0–0.50) ml/kg/h, which was significantly reduced, and increased 12 h after CBP initiation [0.95 (IQR 0.15–1.40) ml/kg/h, P = 0.003]. Before CBP initiation, SCr and blood urea nitrogen (BUN) were increased [107.8 (IQR 74.4–180.3) µmol/L and 10.8 (IQR 7.4–15.3) mmol/L, respectively]. Moreover, after 12 h of CBP, SCr was decreased [69.4 (IQR 42.7–95.9) μmol /L, P = 0.019], and after 24 h of CBP, BUN was decreased [6.6 (IQR 5.1–9.9) mmol/L, P = 0.006]. No significant changes in serum potassium or sodium (P > 0.05) were observed during CBP.
CBP operating conditions and related adverse events
Fourteen neonates (53.8%) received continuous veno-venous hemodiafiltration (CVVHDF) and 12 (46.2%) received continuous veno-venous hemofiltration (CVVH). The median age at CBP initiation was 6 (IQR 3–12) days, and the median duration was 47.75 (IQR 25.50–83.38) h. The 14–18G single-lumen catheters were used in 19 cases (73.1%), and 5F double-lumen catheters were used in seven cases (26.9%). Blood access for the CBP included the internal jugular vein in 19 patients (42.2%), femoral vein in 19 (42.2%), umbilical vein in three (6.7%), and subclavian vein in four (8.9%). CBP complications included thrombocytopenia [16 cases (45.7%)], bleeding or thrombosis [seven cases (20.0%)], membrane blocking [four cases (11.4%)], hypotension [four cases (11.4%)], and electrolyte disturbance [four cases (11.4%)]. Univariate analysis identified no risk factors for CBP-related death (Table 1).
Outcomes
All 26 neonates were initially treated conservatively, including active fluid resuscitation, acidosis correction, anti-infection, vasoactive drugs, and diuresis. CBP was subsequently administered when the neonates met the appropriate indications. During NICU admission, 13 of the 26 neonates with septic shock and AKI died (50%), including seven with heart failure, two with primary pulmonary hypertension, one with severe encephalopathy, one with severe hypoxemia, one with disseminated intravascular coagulation, and one with liver failure.
Discussion
Neonatal sepsis is a life-threatening organ dysfunction caused by dysregulation of the immune response to infection [9]. Septic shock is defined as severe infection that leads to cardiovascular dysfunction [6], and endotoxins play an important role in its development. Death caused by sepsis is not due to the pathogenicity of the bacteria itself but to the inflammatory cascades. Therefore, the quick removal of inflammatory mediators and endotoxins from the blood is necessary [5].
At present, CBP can not only replace renal function but also filter out excessive inflammatory mediators and endotoxins, maintain the stability of the internal environment and hemodynamics, and correct shock [10, 11]. In the present study, all 26 neonates had hemodynamic instability before CBP initiation and required vasoactive drugs. At the beginning of CBP, an increase in the dose of vasoactive drugs is required to maintain the blood pressure within the normal range because of the expansion of the cardiopulmonary bypass volume. Compared with before CBP, the VIS was increased at 6 h after CBP initiation in this study, but the difference was not statistically significant. Imberti et al. [12] observed a significant increase in the inotropic/vasoactive support required after 1 h of CBP in the overall population. However, there was no significant difference between 24 h after CBP and before CBP, which is similar to the results of this study. Imberti et al. [12] did not study VIS further, whereas we found a significant decrease in VIS at the end of CBP. This significant decrease in VIS after CBP indicates that CBP could remove a large number of endotoxins, cytokines, and inflammatory mediators for the treatment of neonatal septic shock with AKI, maintain hemodynamic stability over time, and reduce vasoactive drug dosages.
In cases where the systemic inflammatory response of septic shock is not controlled, the microcirculation of the body is disturbed, causing tissue hypoperfusion and oxygenation disorder and increasing anaerobic metabolism, resulting in a significant increase in lactic acid; thus, lactic acidosis occurs in severe cases. Lactate levels positively correlate with the severity and poor prognosis of sepsis and improving lactate clearance can improve the prognosis of children with sepsis [13,14,15]. In this study, PH increased and blood lactate levels decreased at the end of CBP, indicating that CBP can improve microcirculation, increase oxygen uptake capacity, maintain homeostasis, and improve tissue oxygenation and metabolism in neonates with septic shock and AKI. However, whether CBP improves the prognosis of children with sepsis remains unclear.
In the 26 critically ill neonates with septic shock, before CBP initiation, the urine outputs were decreased and the levels of SCr and BUN were significantly increased, indicating that the children had AKI. After CBP treatment, an increase in urine output was observed, suggesting significant improvement in renal function. Previously, it was assumed that renal ischemia–reperfusion caused by septic shock was the main driver of sepsis-related AKI. A study using large animal sepsis models suggested that renal blood perfusion is not reduced and may even increase when AKI occurs in sepsis [16]. Similarly, clinical studies have shown that renal cortical hypoperfusion is a persistent feature in critically ill patients with sepsis who develop AKI and does not appear to be caused by a reduction in macrovascular renal blood flow or cardiac output [17]. Therefore, the increased urine output and improved renal function could be due to a reduction in venous system overload that affects the kidneys. Alternatively, the improved renal function after CBP could be due to improvements in hemodynamics and renal perfusion and is thought to be related to the removal of large amounts of excess water, solutes, and inflammatory cytokines from the body.
Complications during CBP included thrombocytopenia, membrane blocking, hypotension, hypothermia, bleeding or thrombosis, bloodstream infection, and electrolyte disturbance [18]. In the present study, thrombocytopenia was the most common complication. The influence of the filters, tubes, and membranes involved in CBP is the primary cause of thrombocytopenia. For example, a decrease in platelets could be due to platelet activation and degranulation from exposure to the roller pump in the CBP machine and attachment to microbubbles or the dialysate [19]. In addition, platelet activation and aggregation have been observed during dialysis with polysulfone membranes in dialyzers sterilized using an electron beam. Moreover, a hemofilter can contribute to thrombocytopenia during CBP by either the destruction or retention of platelets during passage. In this study, the incidence of CBP-associated thrombocytopenia was 61.5% and frequent platelet transfusions were required; however, no severe bleeding was observed. The incidence of bleeding or thrombosis in this study was 26.9%. Most children had abnormal coagulation function, and all achieved systemic anticoagulation with heparin during CBP. Whether the use of regional citrate anticoagulation (RCA) during CBP can reduce bleeding or thrombotic complications remains unclear. Chen et al. [20] suggested that RCA could improve the prognosis of children receiving CBP. A recent systematic literature review [21] demonstrated no significant difference in the risk of severe bleeding complications or death between RCA and systemic anticoagulation with heparin during CBP in critically ill children. Furthermore, RCA has a potential role in prolonging circuit life and appears to be superior to systemic anticoagulation with heparin in decreasing the risk of circuit clotting. During CBP, dynamic monitoring of platelet counts and coagulation function, timely adjustment of the heparin dose, and platelet transfusion, if necessary, could help avoid or reduce bleeding or thrombosis.
Hypotension is another common complication of CBP. The cardiopulmonary bypass volume of CBP in this study was 70 or 73 mL, which was larger than that used in previous studies [18]. However, the incidence of CBP-related hypotension was 15.4%, which was lower than that reported in previous studies [18, 22, 23]. This was attributed to the use of a red blood cell suspension that prefilled the filter and pipeline to reduce hemodilution. To avoid or reduce the complications of CBP-related hypotension, it is necessary to prefill the filter and pipeline with whole blood or red blood cell suspensions before initiating CBP, monitor the vital signs of neonates, reduce the ultrafiltration rate and blood flow at the right time, and adjust the vasoactive drug dosages during CBP.
To effectively reduce complications during CBP, it is important to choose a suitable CBP machine for small infants. Previously, CBP machines designed for adults were adapted for application in children by simply modifying the operating parameters. However, these devices are off-label for infants weighing < 15 kg, which poses a challenge for safe and effective treatment. When adapted for clinical application in infants, they can cause more electrolyte disturbances, acidosis, thrombocytopenia and vasoplegia with relative hypovolemia and hypotension [24]. Moreover, adult CBP machines may result in severe clinical complications because of inaccurate fluid volume control [25, 26]. However, some findings are controversial [27]. Since the first CBP machine (CARPEDIEM) specifically designed for small infants began clinical application in 2013 [28], various similar CBP machines have been developed, including the CBP machine used in this study. The advantages of these new devices include smaller extracorporeal volumes, more graduated flow rate adjustment and precise ultrafiltration control. Recently, many studies have reported that CBP in neonates is feasible, accurate, and safe when using devices designed specifically for small infants [29, 30].
In this study, 13 patients died during NICU admission, with a mortality rate of 50%, similar to that in another study involving patients who received CBP [29]. Additionally, CBP can filter out excessive inflammatory mediators and regulate immune balance, which may improve the prognosis of neonates with septic shock. However, this study did not demonstrate an improvement in the survival of neonates with septic shock who received CBP. The latest research has demonstrated that in cases of sepsis, the establishment of effective immune monitoring methods and the selection of appropriate clearance targets, such as the pathogen itself and host immune cells, might be new targets for extracorporeal blood purification therapy, which requires further research [5, 31].
The main limitation of this study was its small cohort size. Prior to 2015, there were large differences in sepsis treatment and CBP modalities between the two centers. Therefore, we could not enlarge the sample size at present; however, we report here the largest cohort to date of neonates with septic shock and AKI who received CBP. A second limitation was the lack of a control group with septic shock and AKI that did not receive CBP; however, for ethical reasons, this control group was not established. Lastly, this study was a retrospective clinical study. Some bias in the results may be present, resulting in the need for further exploration with a large sample size and a prospective, double-blind, controlled study design.
Conclusions
In neonNates with septic shock and AKI, CBP can effectively maintain the stability of the internal environment and hemodynamics, reduce the dosage of vasoactive drugs, correct shock, and improve renal function. However, the mortality rate remains high; whether CBP improves the prognosis of neonates with septic shock and AKI remains unclear. Adverse events associated with CBP included thrombocytopenia, bleeding or thrombosis, membrane blocking, hypotension, and electrolyte disturbance.
Availability of data and materials
All data generated or analyzed during this study are included in this published article and its supplementary information files.
Abbreviations
- AKI:
-
Acute kidney injury
- BUN:
-
Blood urea nitrogen
- CBP:
-
Continuous blood purification
- CVVH:
-
Continuous veno-venous hemofiltration
- CVVHDF:
-
Continuous veno-venous hemodiafiltration
- MAP:
-
Mean arterial pressure
- NCIS:
-
Neonatal Critical Illness Score
- NICU:
-
Neonatal Intensive Care Unit
- RCA:
-
Regional citrate anticoagulation
- SCr:
-
Serum creatinine
- VIS:
-
Vasoactive-inotropic score
References
Fleischmann-Struzek C, Goldfarb DM, Schlattmann P, Schlapbach LJ, Reinhart K, Kissoon N (2018) The global burden of paediatric and neonatal sepsis: a systematic review. Lancet Respir Med 6:223–230
Baske K, Saini SS, Dutta S, Sundaram V (2018) Epinephrine versus dopamine in neonatal septic shock: a double-blind randomized controlled trial. Eur J Pediatr 177:1335–1342
Coggins SA, Laskin B, Harris MC, Grundmeier RW, Passarella M, McKenna KJ, Srinivasan L (2021) Acute kidney injury associated with late-onset neonatal sepsis: a matched cohort study. J Pediatr 231:185–192.e184
Starr MC, Banks R, Reeder RW, Fitzgerald JC, Pollack MM, Meert KL, McQuillen PS, Mourani PM, Chima RS, Sorenson S, Varni JW, Hingorani S, Zimmerman JJ (2020) Severe Acute Kidney Injury Is Associated With Increased Risk of Death and New Morbidity After Pediatric Septic Shock. Pediatr Crit Care Med J Soc Crit Care Med World Fed Pediatr Intensive Crit Care Soc 21:e686–e695
Monard C, Abraham P, Schneider A, Rimmelé T (2023) New targets for extracorporeal blood purification therapies in sepsis. Blood Purif 52:1–7
Weiss SL, Peters MJ, Alhazzani W, Agus MSD, Flori HR, Inwald DP, Nadel S et al (2020) Surviving sepsis campaign international guidelines for the management of septic shock and sepsis-associated organ dysfunction in children. Intensive Care Med 46:10–67
Nada A, Bonachea EM, Askenazi DJ (2017) Acute kidney injury in the fetus and neonate. Semin Fetal Neonatal Med 22:90–97
Sandrio S, Krebs J, Leonardy E, Thiel M, Schoettler JJ (2022) Vasoactive inotropic score as a prognostic factor during (cardio-) respiratory ECMO. J Clin Med 11:2390
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, Hotchkiss RS, Levy MM, Marshall JC, Martin GS, Opal SM, Rubenfeld GD, van der Poll T, Vincent JL, Angus DC (2016) The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 315:801–810
Broman ME, Hansson F, Vincent JL, Bodelsson M (2019) Endotoxin and cytokine reducing properties of the oXiris membrane in patients with septic shock: A randomized crossover double-blind study. PLoS One 14:e0220444
Guan M, Wang H, Tang X, Zhao Y, Wang F, Zhang L, Fu P (2022) Continuous renal replacement therapy with adsorbing filter oxiris in acute kidney injury with septic shock: a retrospective observational study. Front Med 9:789623
Imberti S, Comoretto R, Ceschia G, Longo G, Benetti E, Amigoni A, Daverio M (2023) Impact of the first 24 h of continuous kidney replacement therapy on hemodynamics, ventilation, and analgo-sedation in critically ill children. Pediatr Nephrol (Berlin, Germany)
Lee SM, Kim SE, Kim EB, Jeong HJ, Son YK, An WS (2015) Lactate clearance and vasopressor seem to be predictors for mortality in severe sepsis patients with lactic acidosis supplementing sodium bicarbonate: a retrospective analysis. PLoS One 10:e0145181
Sauer CM, Gómez J, Botella MR, Ziehr DR, Oldham WM, Gavidia G, Rodríguez A, Elbers P, Girbes A, Bodi M, Celi LA (2021) Understanding critically ill sepsis patients with normal serum lactate levels: results from U.S. and European ICU cohorts. Sci Rep 11:20076
Daga MK, Rohatgi I, Mishra R, Kumar N, Mawari G, Mishra TK, Singh S, Shukla J (2021) Lactate enhanced-quick Sequential Organ Failure Assessment 2 (LqSOFA2): A new score for bedside prognostication of patients with sepsis. Indian J Med Res 154:607–614
Langenberg C, Wan L, Egi M, May CN, Bellomo R (2006) Renal blood flow in experimental septic acute renal failure. Kidney Int 69:1996–2002
Watchorn J, Huang D, Bramham K, Hutchings S (2022) Decreased renal cortical perfusion, independent of changes in renal blood flow and sublingual microcirculatory impairment, is associated with the severity of acute kidney injury in patients with septic shock. Crit Care (London, England) 26:261
Nishimi S, Sugawara H, Onodera C, Toya Y, Furukawa H, Konishi Y, Sotodate G, Matsumoto A, Ishikawa K, Oyama K (2019) Complications during continuous renal replacement therapy in critically ill neonates. Blood Purif 47(Suppl 2):74–80
Daugirdas JT, Bernardo AA (2012) Hemodialysis effect on platelet count and function and hemodialysis-associated thrombocytopenia. Kidney Int 82:147–157
Chen Z, Wang H, Wu Z, Jin M, Chen Y, Li J, Wei Q, Tao S, Zeng Q (2021) Continuous renal-replacement therapy in critically ill children: practice changes and association with outcome. Pediatr Crit Care Med : J Soc Crit Care Med World Fed Pediatr Intensive Crit Care Soc 22:e605–e612
Buccione E, Bambi S, Rasero L, Tofani L, Piazzini T, Della Pelle C, El Aoufy K, Ricci Z, Romagnoli S, Villa G (2022) Regional citrate anticoagulation and systemic anticoagulation during pediatric continuous renal replacement therapy: a systematic literature review. J Clin Med 11:3121
Diane Mok TY, Tseng MH, Chiang MC, Lin JL, Chu SM, Hsu JF, Lien R (2018) Renal replacement therapy in the neonatal intensive care unit. Pediatr Neonatol 59:474–480
Thadani S, Fogarty T, Mottes T, Price JF, Srivaths P, Bell C, Akcan-Arikan A (2022) Hemodynamic instability during connection to continuous kidney replacement therapy in critically ill pediatric patients. Pediatr Nephrol (Berlin, Germany) 37:2167–2177
Goldstein SL, Vidal E, Ricci Z, Paglialonga F, Peruzzi L, Giordano M, Laforgia N, Ronco C (2022) Survival of infants treated with CKRT: comparing adapted adult platforms with the Carpediem™. Pediatr Nephrol (Berlin, Germany) 37:667–675
Santiago MJ, López-Herce J, Urbano J, Solana MJ, del Castillo J, Ballestero Y, Botrán M, Bellón JM (2009) Complications of continuous renal replacement therapy in critically ill children: a prospective observational evaluation study. Crit Care (London, England) 13:R184
Ricci Z, Morelli S, Vitale V, Di Chiara L, Cruz D, Picardo S (2007) Management of fluid balance in continuous renal replacement therapy: technical evaluation in the pediatric setting. Int J Artif Organs 30:896–901
Kedarnath M, Alexander EC, Deep A (2023) Safety and efficacy of continuous renal replacement therapy for children less than 10 kg using standard adult machines. Eur J Pediatr 182:3619–3629
Ronco C, Garzotto F, Brendolan A, Zanella M, Bellettato M, Vedovato S, Chiarenza F, Ricci Z, Goldstein SL (2014) Continuous renal replacement therapy in neonates and small infants: development and first-in-human use of a miniaturised machine (CARPEDIEM). Lancet (London, England) 383:1807–1813
Garzotto F, Vidal E, Ricci Z, Paglialonga F, Giordano M, Laforgia N, Peruzzi L, Bellettato M, Murer L, Ronco C (2020) Continuous kidney replacement therapy in critically ill neonates and infants: a retrospective analysis of clinical results with a dedicated device. Pediatr Nephrol (Berlin, Germany) 35:1699–1705
Battista J, De Luca D, Eleni Dit Trolli S, Allard L, Bacchetta J, Bouhamri N, Enoch C, Faudeux C, Guichoux J, Javouhey E, Kolev K, Regiroli G, Ranchin B, Bernardor J (2023) CARPEDIEM® for continuous kidney replacement therapy in neonates and small infants: a French multicenter retrospective study. Pediatr Nephrol (Berlin, Germany) 38:2827–2837
Eden G, Schmidt JJ, Büttner S, Kümpers P, Hafer C, Rovas A, Koch BF, Schmidt BMW, Kielstein JT (2022) Safety and efficacy of the Seraph® 100 Microbind® Affinity Blood Filter to remove bacteria from the blood stream: results of the first in human study. Crit Care (London, England) 26:181
Acknowledgements
We would like to thank Editage (www.editage.cn) for English language editing.
Funding
This study was funded by the 2023 Quanzhou health Science and Technology Program(2023NS064) and 2020 Shanghai “Science and Technology Innovation Action Plan” Medical Innovation Research Special Project (20Y11907000).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and data collection and analysis were performed by Jinglin Xu, Yifan Sun, Cheng Cai, and Dongmei Chen. The first draft of the manuscript was written by Jinglin Xu, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki and approved by the Medical Ethics Committee of Quanzhou Maternity and Children’s Hospital and Shanghai Children's Hospital (2020R064-E02).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Communicated by Daniele De Luca
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xu, J., Sun, Y., Zhang, W. et al. The efficacy and safety of continuous blood purification in neonates with septic shock and acute kidney injury: a two-center retrospective study. Eur J Pediatr 183, 689–696 (2024). https://doi.org/10.1007/s00431-023-05336-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-05336-y