Abstract
Although the suppression of sympathetic activity is an essential mission for the current heart failure treatment strategy, little is known about the relationship between the rotation speed setting and autonomic nervous activity during continuous-flow left ventricular assist device (LVAD) treatment. We evaluated 23 adult patients with sinus rhythm (36 ± 13 years) who had received continuous-flow LVAD and been followed at our institute between March 2013 and August 2014. Heart rate variability measurement was executed along with hemodynamic study at 3 rotation speeds (low, middle, and high) at 5 weeks after LVAD implantation. Lower rotation speed was associated with higher ratio of low-frequency over high-frequency spectral level (LF/HF), representing enhanced sympathetic activation (p < 0.05 by repeated analyses of variance). Among hemodynamic parameters, cardiac index was exclusively associated with LFNU = LF/(LF + HF), representing relative sympathetic activity over parasympathetic one (p < 0.05). After 6 months LVAD support at middle rotation speed, 19 patients with higher LFNU eventually had higher plasma levels of B-type natriuretic peptide and achieved less LV reverse remodeling. A logistic regression analysis demonstrated that lower LFNU was significantly associated with improvement of LV reverse remodeling (p = 0.021, odds ratio 0.903) with a cut-off level of 55 % calculated by the ROC analysis (AUC 0.869). In conclusion, autonomic activity can vary in various rotation speeds. Patients with higher LFNU may better be controlled at higher rotation speed with the view point to suppress sympathetic activity and achieve LV reverse remodeling.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sympathetic activation is one of the major neurohormonal changes seen in patients with heart failure (HF), and inappropriately elevated sympathetic stimulation has a primary role in the deterioration of failing heart through multiple mechanisms: transduction abnormalities of the β-adrenergic signal, induction of tachyarrhythmias, activation of renin–angiotensin–aldosterone system, facilitation of myocardial remodeling, and acceleration of myocardial cell death [1, 2]. Considering the above mechanisms, β-blockers have been established as an essential tool for the standard regimen for the treatment of HF or even the prevention of HF development owing to its sympatholytic effect [3, 4].
Ventricular assist device (VAD) is a powerful therapeutic tool in patients with stage D HF by unloading left ventricle and ameliorating end-organ hypoperfusion, and has also been demonstrated to improve cardiac autonomic innervation [5]. Although adjustment of rotation speed in consideration of various clinical aspects is essential for patients’ management during VAD support [6], the relationship between rotation speed and sympathetic nerve activity remains unknown. Therefore, we here tried to clarify the effect of rotation speed for sympathetic nerve system and discussed how to find the optimal rotation speed especially on the view point of autonomic nerve activity.
Methods
Patients selection
We retrospectively enrolled 23 adult patients with stage D HF who had received continuous-flow LVADs (EVAHEART, 5; DuraHeart, 5; Jarvik 2000, 2; HeartMate II, 10; HeartWare, 1) and been followed at the University of Tokyo Hospital between Mar 2013 and Aug 2014. All patients gave written informed consent and were listed for heart transplantation before LVAD implantation. All patients had sinus rhythm. No patient received concomitant right VAD implantation. No complications such as systemic/device infection, retention of pleural effusion, stroke, or significant electrolyte imbalance occurred. Rotation speed was adjusted considering patients’ hemodynamics and transthoracic echocardiographic information such as interventricular shift and opening of aortic valve. Doses of β-blocker, angiotensin converting enzyme inhibitor (ACEI), and aldosterone antagonist were titrated considering patients’ hemodynamics before and after the operation. The study protocol was approved by the Ethics Committee of Graduate School of Medicine, the University of Tokyo [application number 779 (1)].
Evaluated baseline characteristics
Patients’ demographic, laboratory, and echocardiographic data were obtained at 5 weeks after LVAD implantation as baseline characteristics. LV ejection fraction (LVEF) was calculated by the biplane Simpson methods on transthoracic echocardiography. The doses of anti-HF medications were evaluated as following: to compare different types of β-blocker, the dose of bisoprolol was normalized to approximately equivalent dose of carvedilol [7]. In the same manner, the doses of ACEI were normalized to approximately equivalent dose of enalapril [8].
Hemodynamic study at 5 weeks after LVAD implantation
All patients underwent hemodynamic study along with transthoracic echocardiography at 5 weeks after LVAD implantation, and 3 rotation speeds (low, middle, and high rotation speeds) were tested. Considering patients’ hemodynamics and echocardiographic parameters, “low rotation speed” was defined by decreasing rotation speed as low as possible. “High rotation speed” was defined by increasing rotation speed as high as possible in the same manner. “Middle rotation speed” was defined as median value between low and high rotation speed. Of them, plasma catecholamine levels were measured at each rotation speed after 5-min rest without any stimulation in 11 patients.
Heart rate variability (HRV) spectral analysis at 5 weeks after LVAD implantation
HRV parameters were measured at each rotation speed just before the above-described hemodynamic study. All HRV parameters were measured for 2 min at 9:00–12:00 am after 15-min rest at the supine position under fixed 0.25 Hz of respiratory rate along with fasting condition [9]. All patients had sinus rhythm without any mechanical pacing support. Electrocardiographic signals from bipolar leads attached at patients’ precordium were transformed to digital ones to calculate the R–R intervals at a sampling rate of 512 Hz. Power spectral analysis of HRV was performed by the MemCalc power spectral density method (MemCalc/Win, Suwa Trust) that used the maximum entropy method for spectral analysis and the nonlinear least-squares method for fitting analysis [10]. The low-frequency (LF) component was defined as 0.04–0.15 Hz, and the high-frequency (HF) component was defined as 0.15–0.40 Hz. The HF power denotes the parasympathetic activity, whereas the ratio of LF over HF component (LF/HF) represents sympathetic activity [9]. To evaluate proportional sympathetic activity over parasympathetic one, normalized unit (NU) was calculated by the following formula: LFNU = LF/(LF + HF) [11].
Variables evaluated at 6 months after LVAD implantation as midterm outcome
Of all, 19 patients were followed ≥6 months after LVAD implantation. Echocardiography was executed along with measurement of plasma B-type natriuretic peptide (P-BNP) concentration at 6 months after the operation, and the midterm endpoint was defined as meeting all 3 following variables: (1) any decreases in P-BNP; (2) any decreases in LV diastolic diameter (LVDd); and (3) any increases in LV ejection fraction (LVEF) compared with those of baseline. The equivalent doses of anti-HF medications were also evaluated as described above. Rotation speed was maintained at the middle rotation speed during the study period considering hemodynamic and echocardiographic results.
Statistical analysis
All statistical analyses were performed by using PASW Statistics 18 (SPSS Inc, Chicago, IL, USA). We showed categorical variables as frequencies and percentages, and compared using Chi-square test or Fisher’s exact test as appropriate. We also represented continuous variables as mean ± standard deviation unless otherwise specified, and compared using unpaired t test or Mann–Whitney U test as appropriate. Each HRV parameter was compared with that of low rotation speed by ad hoc Dunnett’s test when repeated analysis of variance was approved significance. We adopted the Pearson’s product-moment correlation coefficients to analyze the relationship between LFNU and hemodynamic parameters or LFNU and midterm clinical parameters. A logistic regression analysis and a receiver operating curve analysis were performed to analyze the relationship between LFNU and improvement of parameters indicating LV reverse remodeling. Time courses of 3 parameters associated with LV reverse remodeling were stratified by LFNU and compared between 5 weeks and 6 months by paired t test. All hypothesis tests reported were two-tailed, and used a p value <0.05 as significant.
Results
Patients background (Table 1)
In the present study, 23 adult patients (36 ± 13 years and 83 % male) were enrolled. There were no patients with end-organ dysfunction or severe valve disease during the study period.
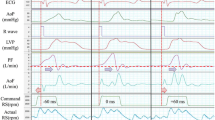
Hemodynamic and HRV parameters at each rotation speed (Fig. 1)
Systolic blood pressure and mean right atrial pressure remained unchanged regardless of any rotation speeds. Lower cardiac index (CI) and higher pulmonary capillary wedge pressure were associated with lower rotation speed (Fig. 1a–d). Lower HF levels were observed at lower rotation speed. LF/HF ratio and LFNU, both representing sympathetic nerve activity, were higher at lower rotation speed (Fig. 1e–h).
Hemodynamic (a–d) and HRV parameters (e–h) at each rotation speed. sBP systolic blood pressure, CI cardiac index, mRAP mean right atrial pressure, PCWP pulmonary capillary wedge pressure, HR heart rate, HF high frequency, LF/HF ratio of low-frequency over high-frequency power, LF NU , normalized unit of LF calculated by the formula: LF/(LF + HF). *p < 0.05 by Dunnett’s test compared with that of low rotation speed when repeated analyses of variance approved significance
Serum catecholamine levels at each rotation speed (Fig. 2)
All 3 plasma catecholamine (noradrenaline, adrenaline, and dopamine) levels were significantly increased at lower rotation speed in 11 patients (p < 0.05) (Table 2).
HRV and hemodynamic parameters (Table 3)
Among hemodynamic parameters at all 3 rotation speed (N = 69), only CI was significantly associated with LFNU (p = 0.001 and r = −0.381).
HRV and midterm clinical parameters (6 months observation)
Of all 23 patients, 19 were treated with LVAD at fixed middle rotation speed adjusted considering hemodynamic and echocardiographic results for ≥6 months. The midterm endpoint, i.e., improvement of all 3 parameters associated with LV reverse remodeling, were eventually achieved in 6 recipients during the study period. A logistic regression analysis demonstrated that lower LFNU level was significantly associated with achievement of improved LV reverse remodeling (p = 0.021, odds ratio 0.903). A receiver operating characteristic analysis showed the cut-off point of LFNU was 55 % for achievement of the midterm endpoint (area under the curve, 0.869; sensitivity, 0.714; specificity, 0.917). The cut-off level significantly stratified time course of 3 parameters indicating improvement of LV reverse remodeling during the study period (p < 0.05 for all) (Fig. 3). Patients’ background stratified by LFNU 55 % was shown in Table 4. Higher HR, P-BNP, and lower LVEF were observed in patients with LFNU >55 %, i.e., higher sympathetic activity group, although not statistically significant. There were no differences between doses of anti-HF agents regardless of LFNU levels.
Discussion
By using HRV spectral analyses, we demonstrated here that autonomic nerve activity was varied at each rotation speed during LVAD support, and higher LF/HF and LFNU levels, indicating sympathetic nerve activation were associated with lower rotation speed accompanied by lower CI. Sympathetic activation was also validated by elevated catecholamine concentration at lower rotation speed. Patients with LFNU >55 % had higher P-BNP level and achieved less LV reverse remodeling during midterm LVAD support.
Lower rotation speed and sympathetic activation
Although there have been no studies discussing the relationship between rotation speed and autonomic activity during LVAD support, we demonstrated for the first time that lower rotation speed was significantly associated with sympathetic nerve activation. Sympathetic activation was defined as higher LF/HF level or LFNU calculated by the HRV analyses [12]. We use the power spectral analyses of HRV, which is an established non-invasive method to assess autonomic cardiac modulation and provides information on both sympathetic and parasympathetic activity of the sinus node [9]. The activated sympathetic tone was validated by the elevated plasma catecholamine concentration at lower rotation speed (Fig. 2) [13].
The lower rotation speed was associated with lower CI due to decreased LVAD flow (Fig. 1b), and lower CI was significantly associated with higher LFNU level among hemodynamic parameters (Table 3). Neither congestion nor elevated cardiac pressure seemed to be a trigger for sympathetic activation. The results were consistent with the previous authors’ reports: significantly decreased cardiac output stimulates baroreceptor and activates sympathetic tone, which results in venous constriction to increase venous return, increased cardiac contractility and heart rate, arterial constriction to elevate vascular resistance, and activation of renin–angiotensin–aldosterone system or arginine–vasopressin system [14–16].
Sympathetic activation and adverse clinical course during LVAD support
This mechanism has emerged in the course of human evolution to maintain hemodynamic homeostasis, but is often affected adversely by inappropriately activated sympathetic tone in patients with HF especially during chronic phase [2]. In patients with chronic HF, inappropriate sympathetic activation induces transduction abnormalities of the β-adrenergic signal that results in reduced maximal functional capacity and myocardial protection from adrenergic stimulation [17], permits LV remodeling and accelerated myocardium death [18], encourages fatal ventricular tachyarrhythmias [19]. These mechanisms again stimulate sympathetic activity, and then the vicious cycle emerges in patients with chronic HF. Considering the above etiology, there is now a well-established evidence, derived from many large-scale clinical randomized control studies [3, 4], that long-term β-blocker treatment in patients with HF substantially improves their LV function, clinical condition, and prognosis by suppressing the vicious cycle.
Doses of β-blocker were well titrated in all patients during LVAD support. Although there was no correlation between LFNU level and dose of β-blockers, higher LFNU level (≥55 %) at the maintenance rotation speed was significantly associated with midterm adverse outcome on the view point of LV reverse remodeling: higher P-BNP level, less decreases in LVDd, and less increases in LVEF compared with those of baseline (Fig. 3). Residual inappropriate sympathetic activity due to accordingly lower rotation speed might have progressed HF regardless of sufficient β-blocker treatment during LVAD support.
Optimal rotation speed setting considering autonomic activity
How should we optimize the rotation speed during LVAD support? Generally, lower rotation speed is recommended because ventricular tachyarrhythmia or aortic insufficiency sometimes develops at higher rotation speed [6]. To achieve optimal rotation speed, routine hemodynamic and echocardiographic studies are strongly recommended as we already did in all patients [6, 20]. We decided the maintenance rotation speed at the median value between lowest and highest rotation speed tested during the hemodynamic study.
However, we demonstrated that patients with LFNU >55 % at the maintenance rotation speed, i.e., middle rotation speed, could not achieve improvement of LV reverse remodeling. Relative activation of sympathetic tone appeared to be associated with worse clinical course during LVAD support. Since we adjusted rotation speed at the middle one in consideration of hemodynamics, the hemodynamic parameters at the maintenance speed were comparable between patients with higher LFNU and those with lower LFNU (Table 4). Higher rotation speed may be recommended in such patients with higher LFNU to achieve optimal LV unloading. Therefore, HRV analyses may be an additional novel tool to optimize rotation speed especially in the view point of autonomic activation during LVAD treatment.
Limitations
-
1.
Since the present study was performed at a single center among a small size sample in a retrospective manner, statistical power may not be strong. Prospective study discussing the long-term result under optimized rotation speed considering the results of HRV analyses would be a future concern.
-
2.
We analyzed the relationship between rotation speed and autonomic nerve activity only at rest condition. Analyses during exercise may approach daily condition.
-
3.
We evaluated short-term HRV parameters at each rotation speed. Whether the observed trend of HRV parameters remains for longer period would be a future concern.
-
4.
We evaluated only patients with sinus rhythm. HRV analyses cannot be adopted in patients with atrial fibrillation or pacing rhythm in general.
Conclusion
Autonomic activation can vary at various rotation speeds during LVAD support. HRV analyses may be an additional novel tool to optimize rotation speed considering autonomic nerve activity.
Reference
Floras JS. Sympathetic activation in human heart failure: diverse mechanisms, therapeutic opportunities. Acta Physiol Scand. 2003;177:391–8.
Metra M, Nodari S, D’Aloia A, Bontempi L, Boldi E, Cas LD. A rationale for the use of beta-blockers as standard treatment for heart failure. Am Heart J. 2000;139:511–21.
The Cardiac Insufficiency Bisoprolol Study II. (CIBIS-II): a randomised trial. Lancet. 1999;353:9–13.
Packer M, Bristow MR, Cohn JN, Colucci WS, Fowler MB, Gilbert EM, Shusterman NH. The effect of carvedilol on morbidity and mortality in patients with chronic heart failure. U.S. Carvedilol Heart Failure Study Group. N Engl J Med. 1996;334:1349–55.
George RS, Birks EJ, Cheetham A, Webb C, Smolenski RT, Khaghani A, Yacoub MH, Kelion A. The effect of long-term left ventricular assist device support on myocardial sympathetic activity in patients with non-ischaemic dilated cardiomyopathy. Eur J Heart Fail. 2013;15:1035–43.
Slaughter MS, Pagani FD, Rogers JG, Miller LW, Sun B, Russell SD, Starling RC, Chen L, Boyle AJ, Chillcott S, Adamson RM, Blood MS, Camacho MT, Idrissi KA, Petty M, Sobieski M, Wright S, Myers TJ, Farrar DJ. Clinical management of continuous-flow left ventricular assist devices in advanced heart failure. J Heart Lung Transplant. 2010;29:S1–39.
Hori M, Nagai R, Izumi T, Matsuzaki M. Efficacy and safety of bisoprolol fumarate compared with carvedilol in Japanese patients with chronic heart failure: results of the randomized, controlled, double-blind, Multistep Administration of bisoprolol IN Chronic Heart Failure II (MAIN-CHF II) study. Heart Vessel. 2014;29:238–47.
McKelvie RS, Yusuf S, Pericak D, Avezum A, Burns RJ, Probstfield J, Tsuyuki RT, White M, Rouleau J, Latini R, Maggioni A, Young J, Pogue J. Comparison of candesartan, enalapril, and their combination in congestive heart failure: randomized evaluation of strategies for left ventricular dysfunction (RESOLVD) pilot study. The RESOLVD Pilot Study Investigators. Circulation. 1999;100:1056–64.
Heart rate variability. Standards of measurement, physiological interpretation, and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Eur Heart J. 1996;17:354–81.
Sawada Y, Ohtomo N, Tanaka Y, Tanaka G, Yamakoshi K, Terachi S, Shimamoto K, Nakagawa M, Satoh S, Kuroda S, Iimura O. New technique for time series analysis combining the maximum entropy method and non-linear least squares method: its value in heart rate variability analysis. Med Biol Eng Comput. 1997;35:318–22.
Pagani M, Lombardi F, Guzzetti S, Rimoldi O, Furlan R, Pizzinelli P, Sandrone G, Malfatto G, Dell’Orto S, Piccaluga E, et al. Power spectral analysis of heart rate and arterial pressure variabilities as a marker of sympatho-vagal interaction in man and conscious dog. Circ Res. 1986;59:178–93.
Akselrod S, Gordon D, Ubel FA, Shannon DC, Berger AC, Cohen RJ. Power spectrum analysis of heart rate fluctuation: a quantitative probe of beat-to-beat cardiovascular control. Science. 1981;213:220–2.
Cohn JN, Levine TB, Olivari MT, Garberg V, Lura D, Francis GS, Simon AB, Rector T. Plasma norepinephrine as a guide to prognosis in patients with chronic congestive heart failure. N Engl J Med. 1984;311:819–23.
Skorecki KL, Brenner BM. Body fluid homeostasis in man. A contemporary overview. Am J Med. 1981;70:77–88.
Frye RL, Braunwald E. Studies on Starling’s law of the heart. I. The circulatory response to acute hypervolemia and its modification by ganglionic blockade. J Clin Invest. 1960;39:1043–50.
Imamura T, Kinugawa K, Hatano M, Fujino T, Inaba T, Maki H, Kinoshita O, Nawata K, Kyo S, Ono M, Komuro I. Low cardiac output stimulates vasopressin release in patients with stage d heart failure. Circ J. 2014;78:2259–67.
Bristow MR. Mechanism of action of beta-blocking agents in heart failure. Am J Cardiol. 1997;80:26L–40L.
Eichhorn EJ, Bristow MR. Medical therapy can improve the biological properties of the chronically failing heart. A new era in the treatment of heart failure. Circulation. 1996;94:2285–96.
Lown B, Verrier RL. Neural activity and ventricular fibrillation. N Engl J Med. 1976;294:1165–70.
Imamura T, Kinugawa K, Kato N, Muraoka H, Fujino T, Inaba T, Maki H, Kinoshita O, Hatano M, Kyo S, Ono M. Late-onset right ventricular failure in patients with preoperative small left ventricle after implantation of continuous flow left ventricular assist device. Circ J. 2014;78:625–33.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Imamura, T., Kinugawa, K., Nitta, D. et al. Lower rotation speed stimulates sympathetic activation during continuous-flow left ventricular assist device treatment. J Artif Organs 18, 20–26 (2015). https://doi.org/10.1007/s10047-014-0800-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10047-014-0800-2