Abstract
Demand of donor organs for transplantation in treatment of organ failure is increasing. Hence there is a need to develop new strategies for the alternative sources of organ development. Attempts are being made to use xenogenic organs by genetic manipulation but the organ rejection against human always has been a major challenge for the survival of the graft. Advancement in the genetic bioengineering and combination of different allied sciences for the development of humanized organ system, the therapeutic influence of stem cell fraction on the reconstitution of organ architecture and their regenerative abilities in different tissues and organs provides a better approach to solve the problem of organ shortage. However, the available strategies for generating the organ/tissue scaffolds limit its application due to the absence of complete three-dimensional (3D) organ architecture, mechanical strength, long-term cell survival, and vascularization. Repopulation of whole decellularized organ scaffolds using stem cells has added a new dimension for creating new bioengineered organs. In recent years, several studies have demonstrated the potential application of decellularization and recellularization approach for the development of functional bio-artificial organs. With the help of established procedures for conditioning, extensive stem cells and organ engineering experiments/transplants for the development of humanized organs will allow its preclinical evaluation for organ regeneration before translation to the clinic. This review focuses on the major aspects of organ scaffold generation and repopulation of different types of whole decellularized organ scaffolds using stem cells for the functional benefit and their confines.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Shortage of available organs for organ transplantation in end-stage organ failure is a major challenge. Annually >10,00,000 patients die for the want of the functional organ. Demand of donating organ for the treatment of end-stage organ failures has increased tremendously in recent years. Together with this, scientists from different area are trying to develop artificial organs and extra cellular matrix (ECM) using xenogenic organ scaffolds to improve the functional benefit.
Since last decades efforts have been made to develop the alternative source for organ bioengineering. An alternative, ample supply of organs from xenogenic sources such as porcine, bovine, and equine has been successfully implanted into humans [1–3]. The tissues obtained from these animals’ possess various limitations such as immune rejection, cross contamination, etc. However, the attractive aspect of xenogeneic organs as a source of ECM provides a better option to secure healthy, pathogen-free tissue to bioengineer the humanized organ system. Development of humanized organs using xenogenic sources allows unique analysis of chimerism and provides a clear distinction between transplant and host existing nearly identical antigenic properties. Using humanized organ system, the therapeutic influence of stem cell fraction on the reconstitution of organ architecture and their regenerative abilities in different tissues and organs provides a better approach to solve the organ shortage. With the help of established procedures for conditioning, extensive stem cells and organ engineering experiments/transplants can be performed in humanized organs that allow its preclinical evaluation for organ regeneration before translation to the clinic.
In 1990, the first bio-artificial skin was developed but this scaffold lacked the mechanical strength and the interconnection channel [4, 5]. Following this study, the area of creating bio-artificial organ has revolutionized to generate other body organs. Various studies have demonstrated significant improvement for the development of novel strategies to create bio-artificial organ or their scaffolds. Classically scaffolds are classified into two major class based on their self-life: one is permanent scaffold and another one is temporary scaffold. Permanent scaffolds maintain the shape and strength but temporary scaffold degrades in a period of time. Temporary scaffolds are two types: synthetic and natural. Natural polymers are biocompatibility, enzymatically degradable and it has biofunctional molecules. Natural polymers have certain limitations such as it inhibits the function of cells by uncontrolled enzymatic degradation. To solve these problems synthetic polymers were developed. Previously fabricated scaffolds were developed like gas foaming, solvent casting, fiber bonding and phase separation but they had small size, shape and generally lack the sensitivity. Recently, 3D fabricated scaffolds are developed to identify the interaction between cell–cell and cell matrix. Further different 3D fabricate scaffolds are developed; like heat mediated, light mediated, adhesive mediated, indirect, cell assemble, hybrid cell assembly but which the lack the mechanical strength, structural properties, cell survival and micro architecture. As these classical types of scaffolds pass several hurdles to be used in regenerative medicine, new strategies are needed to develop to overcome these limitations.
Every organ in human body has a scaffold or a 3D functional architecture, which provides its shape within the body. It contains many different types of cells with different functions. Tissue/organ engineering has aimed to create the organ scaffold—either through the use of synthetic materials such as polymers, or through decellularization, which uses the whole organ as a scaffold after removing its cellular components. Recently, the use of the 3D decellularized matrix of organs has shown a hope for the creation of natural 3D architecture of any organ for the development of bio-artificial organ. In a very landmark study published by Ott et al. [6], they demonstrated the complete decellularization of rat heart and repopulation of heart cells. This study was followed by many other studies for the development of different types of organ scaffolds. Recently decellularization method has evolved as a potential technology which provides native matrix for cell survival and proliferation.
Decellularization is defined as the technology used to remove all parenchyma cells, myofilaments, endothelial cells and other cellular components from the organ while retaining its three-dimension architecture and vascular tree. The use of natural vasculature and rapid separation of debris and waste fluid from organ or tissue significantly improves the quality of organ scaffold for reconstitution of new organ/tissue. Decellularization is ideal for tissue regeneration because it preserves the three-dimensional structure of the organ and the ECM—the framework between the cells—that are complex and difficult to mimic. While current methods use specific ECM proteins to transform stem cells into a particular cell type, scientists have found it difficult to imitate the natural ECM. A variety of stem cell types from various sources either alone or in combination with other cells have been tried to develop the whole functional organ to develop a new approach for organ bioengineering.
Stem cells and organ bioengineering
The advancement in stem cell research has added knowledge about the development and regeneration of an organ or tissue from a single cell. Stem cells are immature, undifferentiated cells having ability to continuously divide, self-renew themselves and differentiate into different types of cells. Adding up to the cell replacement therapy using stem cells, organ transplantation has been successfully accomplished in clinics for organ failure of the liver or kidney. However, the lack of donor organs has become the main barrier to develop the organ transplant program. Generation of biological or semi-biological organs using stem cells could be an alternative approach to solve the problem of the donor organ shortage. Notably, researchers have been hunting for ways to establish a whole organ using stem cells. Stem cells from various sources have been tried to regenerate the damages organ system still which stem cell type is used, it remains a challenge to reliably generate large quantities of well-differentiated cells.
However, stem cells possess great potential in regenerative therapies; there is still a ways to go before it can be transferred from bench to clinic. The recent breakthroughs and one specific trial, in particular, provide much closer evidence for clinical practice. Recently, the first human tissue-engineered organ using stem cells was created and transplanted successfully into a patient. In the first reported instance of using stem cells to bioengineer a functional human organ, Paolo Macchiarini and his research group used a patient’s own stem cells to generate an airway, specifically a bronchus, and successfully grafted it into the patient to replace her damaged bronchus. Macchiarini’s group bypassed the problem of immune rejection using the patient’s own stem cells. Additionally, by combining a variety of bioengineering efforts, no synthetic parts were involved in the creation of the organ; it was made entirely of cadaveric and patient-derived tissues [7, 8]. Other tissue regeneration efforts with stem cells have also recently made many breakthroughs, emphasizing the potential of using stem cells in future tissue/organ transplants.
However, in end-stage organ failure, several functional demands listed below must be considered to develop a functional transplantable bio-artificial organ.
-
Type of organ scaffold
-
Sterilization of the scaffold
-
Integrity of the vasculature and natural architecture within the scaffold
-
Assessment of immunological barriers
-
Type of cells/tissue to regenerate
-
Functional aspects of the regenerated organ
-
Type of cells for infusion
-
Route of cell delivery
-
Required induction factors
-
Assessment of long-term cell survival and engraftment
Approaches for generating whole functional organ
The knowledge of stem cells has opened new area of organogenesis. There are various strategies to use potential of stem cells for creating natural 3D functional organs.
Potential use of single adult tissue stem cell
Single stem cell is needed to purify from the tissue to prove its potential for generating the entire organ. Few studies have shown that the prostate and mammary gland can be generated in vivo from a single adult tissue stem cell [9–11]. However, because of lack of definite markers, there has been no trustworthy method to isolate mammary stem cells. These studies provide an important consequence for tissue/organ repair/regeneration and development. In other terms, we can visualize that the potential use of single stem cells in clinic will ultimately change the treatment archetype for several human disorders more than mammary gland injury and prostatic disease.
Applicability of using a blastocyst complementation system
In addition to single stem cells derived from tissues, embryonic stem cells (ESCs) have proved their potential to generate specific organs using a strategy of ESCs transplantation from one species into the blastocyst of a different species. For the first time blastocyst complementation system was reported by Chen et al. [12]. They generated B and T lymphocyte lineage cells by implanting normal mouse ESCs into the blastocysts derived from Rag2−/− mice. Later Kobayashi and colleagues [13] proved the principle findings of pancreas generation by introduction of induced pluripotent stem cells (iPSCs) into the blastocysts of pancreas-deficient Pdx1−/−mouse. Transplantation of iPSCs initially did not grow their individual pancreas and were unable to produce the insulin. Rat stem cells grew in a unique environment in the absence of mouse pancreas within the mouse and developed a rat pancreas having the capacity of insulin production when matured. The findings of this study clearly demonstrated that rat pancreas can be generated by inter-species blastocyst complementation which proves its potential to solve the problem for organ shortage for transplantation. However, the applicability of this technology in human organ developments suffers with ethical controversies and limits its use in human experiments.
Generation of organ/tissue by a combination of tissue engineering and seeded stem cells
Tissue-engineering technology has been used to unite specific stem cells with biocompatible and biodegradable polymer scaffolds to produce a cell polymer implant.
Cao and colleagues [14] for the first time made a construct by seeding the chondrocytes within polyglycolic acid–polylactic acid polymer template in the shape of a human auricle. New cartilage formed after 12 weeks of implantation under the dorsal skin of the mice. The polymer construct degraded gradually following transplantation and the cartilage was formed. The technique provided its vast applicability in particular for plastic and reconstructive surgery. But this technology, for long time, seemed to focus only on exterior instead of the interior of the functional organ due to the lack of integrated fully functioning vascular architectures into the engineered construct.
The limitations of this study were recently solved by Takebe and colleagues [15] to generate a functional human vascular network which provides a novel approach for regenerating the larger, well-vascularized organs and seemed to resolve the foremost hindrances in regenerating thick and complex tissues. They generated a vascular network construct and implanted into an immunodeficient mouse which had potential to act as functional vessels. Further studies in this trend will impede future reconstitution of vascularized human organs.
Development of whole organ via decellularization and recellularization approach
Whole organ development requires not only the stem cells but also the contiguous stem cell niche or microenvironment and extracellular matrix with complete vasculature and integrity. In recent years, decellularization and recellularization approach for whole organ construction has been emerged as exceptionally promising technology [16]. Few landmark studies on complex organs development, such as liver, heart, kidney and lung, have provided a better insight into the supremacy of the methodology. Encouraging results from animal model studies have emerged a potential hope to get the whole personalized functional organ for the end-stage organ failure patients.
Development of three-dimensional natural bio-artificial organ scaffold using decellularization technology
Since last few years organ transplantation is a source for standard care for the patients with end-stage organ failure. Biggest problem in medicine is the availability of whole organs for transplantation. There are two major problems in organ transplantation: the major risk of immune rejection, life-long use of immunosuppressors. Scarcity of organ donors increases the need to create the alternative organ source for the development of whole functional organ which can be useful for organ transplantation. This bio-artificial organ should provide microvascular structure for efficient supply of nutrient and oxygen to each and every cell, which solves the problem of availability of 3D-natural architecture and organ scaffold, immune rejection and others. Various studies have been published to demonstrate the methodologies for whole organ decellularization using different approaches (Table 1).
Methods for whole organ decellularization
Whole organ decellularization represents a novel approach to create bio-artificial natural 3D architecture. However, various methods have been used to remove the cells and its components from different organ leaving its ECM and organ scaffold. But still there is a need to find more appropriate decellularization agent further to improve the quality organ scaffold. Several studies have demonstrated the use of various types of chemical, biological and physical substance for whole organ decellularization. But which is the best still needs to be found based on the organ architecture and its further application. All the decellularization agents have certain advantages and disadvantages which can be more beneficial if combined (Table 2).
Major advantages of whole organ decellularization
Whole organ decellularization approach eliminates all immune potential cells maintaining not only the scaffold but also the vascular structures for efficient supply of oxygen and nutrients [17]. Decellularized organ scaffold provides a natural 3D platform for cells transplantations, migration, engraftment and survival within it. It also acts as a natural model for drug testing and tissue/organ. The ECM in decellularized organ scaffold provides important factors for cellular proliferation and differentiation; after cellular transplantation within the decellularized 3D organ scaffold several bioactive molecules are being released which makes the tissue architecture smooth like natural system. Because decellularized organ scaffold does not contain any cellular component, it does not have rejection problem whole introducing the cells.
Disadvantages of whole organ decellularization
Decellularization method
Although various studies have demonstrated most successful result of organ decellularization still there is certain limitation of those methods, specifically the decellularization technique and decellularized agents. This can damage the ECM and membrane tissue of the organ. Most efficient method of organ decellularization, i.e., perfusion decellularization, needs several chemical agents, which may also respond to both the structural and biochemical constituents of the organ.
Growing completely functional organ/tissue
One of the major problems with decellularized organ scaffold is to grow the functional desired cell types within this and further to transplant in vivo to get natural functional organ. In this perspective, there is a need for type of cell to be transplanted, appropriate medium and technology. Further in vivo transplantation needs to be developed.
Sources of organ/tissue for decellularization
Getting a suitable source for organ donor remains a major challenge for the development of bio-artificial organs. The previous studies have demonstrated the potential of decellularization approach using rat, porcine, monkey and pig. However, fear of zoonosis is a major challenge for the use of xenogenic organs/tissue. And there is a great need to find an alternative source to fill the gap between the shortage of available organ donors and recipients. In our earlier study we have demonstrated that goat is an ideal source for the development of bio-artificial organ [18, 19].
Immunological barriers
Using xenogenic organ scaffolds have a doubt about antigen which may cause the rejection. However, the ECM is preserved among the species, one surface antigen remains at low level named galactosyl-α (1, 3) galactose (Gal) in xenogenic tissues and is absent in primates and human which can cause acute rejection in whole organ xenograft.
Recellularization methods
Recellularization protocols for higher mammals’ fall closer to human and can be taken for further applications. However, various studies have demonstrated the recellularization approach only on small animals and that they do not fall closer to the human as the ECM composition within a single organ system varies from animal to animal [20–22]. So it is very difficult to standardize a common protocol or route of delivery or no. of cells to be infused for functional regeneration of the organ scaffold.
Revascularization of decellularized organ scaffold
Development of durable vascular network represents a major challenge for creating a bio-artificial organ where immediate blood supply is needed to maintain cell survival due to thickness of the tissue and corresponding diffusion distance. Decellularized organ scaffolds retain the vasculature and restoring blood flow accurately is less challenging, but the question remains to be answered of how long it can be retained. Because, any incompletely re-endothelialized vasculature is always at risk of thrombosis, leading to localized organ failure.
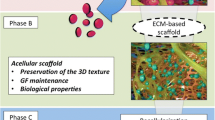
Regeneration/repopulations of whole decellularized organ scaffold
Recellularization is a process of generating functional cells within the decellularized organ scaffold to get fully functional bio-artificial organ. Seeding of specific type of cells with high proliferation and controlled differentiation potential is necessary to repopulate the decellularized organ scaffold. A variety of cell types such as embryonic stem cells, mesenchymal stem cells, endothelial cells, fetal tissue cells and induced pluripotent cells have been used in many studies described below depending upon the type of organ to intricate three-dimensional heterogeneous arrangements. Although, a variety of organs have been used for decellularization and recellularization to generate the functional organ. None of them have proved their absolute potential to replace the damaged organ/tissue. Still there are certain complications and/or issues which need to be considered and solved before its clinical applications. Each organ has different anatomies with different functions. Therefore, use of more appropriate cells remains a challenge to regenerate a complete organ. And for each organ type different strategies and functional aspects are needed to consider before developing a better solution for the current hurdles (Fig. 1).
Heart
Worldwide, more than 22 million people are currently suffering with some forms of heart failure [6]. Approximately, 3,000 heart patients are on waiting list for heart transplant [23]. The first successful heart transplantation was performed in 1967 by Dr. Christiaan Barnard. However, the patient was died after 18 days of post-transplantation due to pneumonia and heavy dose of immune-suppressants. This approach provided a new hope for the patients dying due to heart failure and other heart complications. But due to higher rate of death because of heart failure and unavailability of heart donors, alternative strategies are needed to discover to accomplish the need of new healthy heart. Decellularization and recellularization approach has emerged as a potential technology for the development of natural, functional and personalized heart.
Three major components are required for the development of complete functional heart: (a) 3D-natural architecture, (b) appropriate cell composition and (c) maturation of the construct to develop nascent pump function. Ott et al. [6] performed perfusion decellularization for cadaveric rat hearts on a modified Langendorff apparatus and further repopulated the acellular heart scaffold with cardiac and endothelial cells through coronary perfusion into a bioreactor and examined for simulated cardiac physiological functions till 28 days. Interestingly, after day 8 they found that recellularized heart construct was contracting and drug responsive. After sufficient maturation the constructs could generate pump function (equivalent to 2 % of adult or approximately 25 % of 16-week-old fetal heart function) and given the further ability to repopulate the entire vasculature with endothelial cells, this organ was equal to entire donor heart. However, major limitation of the study was that it was limited to rat hearts which can further be scaled up to hearts of human size and complexity.
Later, the similar approach was reported by Ng et al. [24] where they repopulated the decellularized heart scaffold with embryonic stem cells which failed to generate functional heart construct because of low cardiac myocyte differentiation efficiency. Further Lu et al. [25] demonstrated the engineering of functional human heart tissues by repopulating decellularized mouse hearts with human-induced pluripotent stem cell-derived cardiac myocyte progenitors (MCPs). CMPs were delivered through coronary vessels of the heart which further demonstrated cardiomyocyte proliferation, differentiation, myofilament formation, spontaneous contraction, generation of mechanical force and responsive to drugs. These studies provide a greater hope to engineer personalized human heart constructs which may find application in clinical practice after significant developments.
Liver
Since last two decades, most of the tissue-engineering approaches have involved in reconstruction of thin sheets of cells, such as skin, arteries and bladder [26–28]. Construction of thicker tissues (muscles, liver and kidney, etc.) has not been feasible due to partial diffusion of oxygen and nutrients within the engineered scaffold [29]. Baptista et al. [30] provided an important tool for the creation of a fully functional bioengineered liver by perfusion decellularization of rat liver after removing the cellular components and preserving the macrovascular tree of the entire liver. The decellularized whole liver scaffold was perfused with human fetal liver and endothelial cells through the vasculature. And it was observed that the entire area throughout the liver scaffold was repopulated by engrafting into their reputed usual locations. The cells within the repopulated liver displayed typical hepatic, endothelial and biliary epithelial markers.
In our view, these decellularized liver bio-scaffolds have a great potential to ensue an advanced in vitro natural liver cell culture system for toxicology, pharmacology and drug discovery. This may also established as an excellent tool to cram the normal tissue and organ development as well as liver pathology. Finally, the decellularization and recellularization technology may fetch us closer to the critical goal of developing bioengineered personalized livers for transplantation in end-stage liver diseases.
Kidney
The increasing prevalence of patients with end-stage kidney diseases is in greater need of functional kidney donor. However, stagnant donor organ numbers have increased the waitlist mortality to 5–10 %. Despite advancements in renal transplantation immunology [31], almost 20 % of the recipients experience episode of acute rejection within 5 years of post-transplantation whereas approximately 40 % patients die after 10 years due to graft rejection and other complications. Several attempts have been made to substitute the native kidney structure and function. Previous studies have demonstrated bioengineering of viable tubular structure to supplement the hemofiltration. More portable and compatible, renal assisting devices have reached the stage of preclinical evaluation and hold great promise to improve the quality of life of patients suffering from end-stage renal failure [32–34]. Indeed, these strategies provide a part of the functional kidney and fail to provide life-long protection and alternative to the natural kidney.
Development of a bioengineered kidney could resolve these problems by providing fully functional kidney transplants. Recently, Song et al. [21] performed perfusion decellularization of cadaveric rat kidneys and repopulated the acellular kidney scaffold by human umbilical venous endothelial cells through the renal artery and suspended rat neonatal kidney cells through the ureter. The kidney scaffold was kept under controlled environment of a bioreactor to provide whole organ culture conditions. After several days of organ culture within the perfusion bioreactor regenerated kidney constructs produced urine in vitro. Within the regenerated kidney macromolecular sieving, electrolytes and glucose reabsorption were partially restored which clearly indicates engraftment and function of repopulated endothelial cells. This landmark study provided an innovative technology for further translation into upscale kidney developments.
Lung
Several devastating lung diseases such as chronic obstructive pulmonary diseases (COPD), cystic fibrosis and idiopathic pulmonary fibrosis (IPF) are major causes of morbidity and mortality for which there is no cure. Lung transplantation is the only option for the treatment of such end-stage lung disorders. COPD has been predicted to be the third leading cause of death worldwide by the year 2020 [35, 36]. Three most important elements (cells, scaffold, and growth factors) in any organ control the process of tissue regeneration. There are various methods available for organ scaffold generation, for example, thermal-induced phase separation, gas foaming, rapid prototyping and decellularization. Among these methods, decellularization has emerged as the most promising technology for whole organ scaffold generation. Because of increasing prevalence of end-stage lung diseases, development of a decellularized whole lung scaffold is valuable as a substrate for the growth of engineered lung tissue. In these perspectives, few recent studies have demonstrated the successful generation of acellular whole lung scaffold by decellularization [22, 37–40]. Further developments in the generation of whole lung ECM can be useful for the study of lung development, and substrate cues that impact pulmonary epithelial growth and differentiation.
Trachea
Since last two decades, several attempts have been carried out for the construction of tracheal spare parts, but instead of vast efforts they have met with serious difficulties. Ossda et al. [41] and Vacanti et al. [42] published the first report for the trachea engineering. Since then various approaches have been followed for the development of bio-artificial trachea. However, the complete satisfactory approach has not been achieved for the development of tracheal substitutes. Paz et al. [43] demonstrated the feasibility of creating a structurally sound tissue-engineered tracheal replacement by combining chondrocytes seeded on a ploy ethylene glycol (PGA) scaffold with a decellularized aortic scaffold. Significant improvements were observed in native cartilage regeneration and structural stability. This study provided a foundation for further animal studies for the generation of tracheal grafts to provide a new therapy for the patients with extensive tracheal disease.
Pancreas
Current treatment of diabetes mellitus using insulin injection and islet transplantation embraced with certain limitations of daily insulin injection and low survival rate for islet transplants. To overcome these limitations, there is a need to develop a favorable biological support for islet regeneration and long-term survival. Acellular ECM derived from various cell types have been used to support the cells survival, engraftment, growth and maturation [44]. However, rather than attempting to design matrixes, decellularized whole pancreatic organ scaffold may be generated by decellularization approach which provides a natural three-dimensional platform for pancreatic development.
Bench to bedside translation of repopulated decellularized organ scaffolds
Several investigations have performed repopulation of decellularized organ scaffold using different types of cells. Whereas many key challenges remain to be solved for better recovery and clinical outcome. Further studies are needed to determine the role of biological, structural and mechanical factors responsible for the generation of natural ECM with functional recovery. Petersen et al. [38] and Ott et al. [45] for the first time demonstrated transplant survival for few hours of repopulated lung scaffold into rats with adequate oxygen and CO2 exchange and appropriate pressure/volume relationships. However, the rat died because of pulmonary edema and/or hemorrhage resulting in respiratory failure. This approach provided a clue for the development of new organ by recellularization of decellularized organ scaffolds. Following the above study, Song et al. [21] generated a bio-artificial rat kidney by decellularization and recellularization approach using human umbilical cord blood-derived endothelial cells and showed urine production along with slight macromolecular sieving and reabsorption potential.
In summary, development of bio-artificial functional organs based on the decellularization and recellularization of whole organ scaffold still remains a challenge. And more research is needed for the prediction of functional outcome ex vivo and in vivo such as long-term survival, engraftment and cost effectiveness. Finally, the concept of decellularization and recellularization has provided a new dimension for the development of bio-artificial organs which can find its clinical applications after further advancements.
References
Bailey LL, Nehlsen-Cannarella SL, Concepcion W, Jolley WB. Baboon-to-human cardiac xenotransplantation in a neonate. JAMA. 1985;254:3321–9.
Lan C, Xiao W, Xiao-Hui D, Chun-Yan H, Hong-Ling Y. Tissue culture before transplantation of frozen–thawed human fetal ovarian tissue into immunodeficient mice. Fertil Steril. 2010;93:913–9.
Van Eyck AS, Bouzin C, Feron O, Romeu L, Van Langendonckt A, Donnez J, Dolmans MM. Both host and graft vessels contribute to revascularization of xenografted human ovarian tissue in a murine model. Fertil Steril. 2010;93:1676–85.
Baksh D, Davies E, Kim S. Three-dimensional matrices of calcium polyphosphates support bone growth in vitro and in vivo. J Mater Sci. 1998;9:743.
Ishaug SL, Crane GM, Miller J, et al. Bone formation by three-dimensional stromal osteoblast culture in biodegradable polymer scaffolds. J Biomed Mater Res. 1997;36:17.
Ott HC, Matthiesen TS, Goh SK, Black LD, Kren SM, Netoff TI, Taylor DA. Perfusion-decellularized matrix: using nature’s platform to engineer a bioartificial heart. Nat Med. 2008;14:213–21.
Macchiarini P, Jungebluth P, Go T, Asnaghi MA, Rees LE, Cogan TA, Ddson A, Martorell J, Bellini S, Parnigotto PP, Dickinson SC, Hollander AP, Mantero S, Conconi MR, Birchall MA. Clinical transplantation of a tissue-engineered airway. Lancet. 2008;372:2023–30.
Hollander A, Macchiarini P, Gordijn B, Birchall M. The first stem cell-based tissue-engineered organ replacement: implications for regenerative medicine and society. Regen Med. 2009;4:147–8.
Shackleton M, Vaillant F, Simpson KJ, Stingl J, Smyth GK, Asselin-Labat ML, Wu L, Lindeman GJ, Visvader JE. Generation of a functional mammary gland from a single stem cell. Nat. 2006;439:84–8.
Stingl J, Eirew P, Ricketson I, Shackleton M, Vaillant F, Choi D, Li HI. Eaves purification and unique properties of mammary epithelial stem cells. Nat. 2006;439:993–7.
Leong KG, Wang BE, Johnson L, Gao WQ. Generation of a prostate from a single adult stem cell. Nat. 2008;456:804–8.
Chen J, Lansford R, Stewart V, Young F, Alt FW. RAG-2-deficient blastocyst complementation: an assay of gene function in lymphocyte development. Proc Natl Acad Sci USA. 1993;90:4528–32.
Kobayashi T, Yamaguchi T, Hamanaka S, Kato-Itoh M, Yamazaki Y, Ibata M, Sato H, Lee YS, Usui J, Knisely AS, Hirabayashi M, Nakauchi H. Generation of rat pancreas in mouse by interspecific blastocyst injection of pluripotent stem cells. Cell. 2010;142:787–99.
Cao Y, Vacanti JP, Paige KT, Upton J, Vacanti CA. Transplantation of chondrocytes utilizing a polymer-cell construct to produce tissue-engineered cartilage in the shape of a human ear. Plast Reconstr Surg. 1997;100:297–302.
Takebe T, Koike N, Sekine K, Enomura M, Chiba Y, Ueno Y, Zheng YW, Taniguchi H. Generation of functional human vascular network. Transpl Proc. 2012;44:1130–3.
Badylak SF, Taylor D, Uygun K. Whole-organ tissue engineering: decellularization and recellularization of three-dimensional matrix scaffolds. Ann Rev Biomed Eng. 2011;13:27–53.
Baptista PM, Orlando G, Mirmalek-Sani SH, Siddiqui M, Atala A, Soker S. Whole organ decellularization: a tool for bioscaffold fabrication and organ bioengineering. Conf Proc IEEE Eng Med Biol Soc. 2009;65:26–9.
Habibullah CM, Vijayalakshmi V, Naseem B, Habeeb MH, Shashi S, Rao M. Hepatofunctional study of UV-B (302 nm) irradiated goat hepatocytes. Am J Gastroenterol. 2000;95:2511–2.
Khan AA, Capoor AK, Parveen N, Naseem S, Vijayalakshmi V, Venkateshan V, Habibullah CM. In vitro studies on a bioreactor module containing encapsulated goat hepatocytes for the development of bioartificial liver. Ind J Gastroenterol. 2002;21:55–8.
Ross EA, Abrahamson DR, John PL, Clapp WL, Williams MJ, et al. Mouse stem cells seeded into decellularized rat kidney scaffolds endothelialize and remodel basement membranes. Organogen. 2012;8:49–55.
Song JJ, Guyette JP, Gilpin SE, Gonzalez G, Vacanti JP, Ott HC. Regeneration and experimental orthotopic transplantation of a bioengineered kidney. Nat Med. 2013;19:1–8.
Nakayama KH, Lee CCI, Batchelder CA, Tarantal AF. Tissue specificity of decellularized rhesus monkey kidney and lung scaffolds. PLoS One. 2013;8:e64134.
Bowen J. By the numbers: heart transplants in the US. WSFA stories. (Online Statistics) 2012.
Ng SL, Narayanan K, Gao S, Wan AC. Lineage restricted progenitors for the repopulation of decellularized heart. Biomat. 2011;32:7571–80.
Lu TY, Lin B, Kim J, Sullivan M, Tobita K, Salama G, Yang L. Repopulation of decellularized mouse heart with human induced pluripotent stem cell-derived cardiovascular progenitor cells. Nat Commun. 2013;4:2307.
Zacchi V, Soranzo C, Cortivo R, Radice M, Brun P, Abatangelo G. In vitro engineering of human skin-like tissue. J Biomed Mater Res. 1998;40:187–94.
Kaushal S, Amiel GE, Guleserian KJ, Shapira OM, Perry T, Sutherland FW, et al. Functional small-diameter neovessels created using endothelial progenitor cells expanded ex vivo. Nat Med. 2001;7:1035–40.
Atala A, Bauer SB, Soker S, Yoo JJ, Retik AB. Tissue-engineered autologous bladders for patients needing cystoplasty. Lancet. 2006;367:1241–6.
Griffith LG, Naughton G. Tissue engineering—current challenges and expanding opportunities. Sci. 2002;295:1009–14.
Baptista PM, Siddiqui MM, Lozier G, Rodriguez SR, Atala A, Soker S. The use of whole organ decellularization for the generation of a vascularized liver organoid. Hepatol. 2011;53:604–17.
Kawai T, et al. HLA-mismatched renal transplantation without maintenance immunosuppression. N Engl J Med. 2008;358:353–61.
Rogers SA, Hammerman MR. Prolongation of life in anephric rats following de novo renal organogenesis. Organogen. 2004;1:22–5.
Gura V, Macy AS, Beizai M, Ezon C, Golper TA. Technical breakthroughs in the wearable artificial kidney (WAK). Clin J Am Soc Nephrol. 2009;4:1441–8.
Fissell WH, Roy S. The implantable artificial kidney. Semin Dial. 2009;22:665–70.
Lopez AD, Shibuya K, Rao C, et al. Chronic obstructive pulmonary disease: current burden and future projections. Eur Respir J. 2006;27:397–412.
Eisner MD, Anthonisen N, Coultas D, et al. An official American thoracic society public policy statement: novel risk factors and the global burden of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2010;182:693–718.
Cortiella J, Niles J, Cantu A, et al. Influence of acellular natural lung matrix on murine embryonic stem cell differentiation and tissue formation. Tissue Eng Part A. 2010;16:2565–80.
Petersen TH, et al. Tissue-engineered lungs for in vivo implantation. Sci. 2010;329:538–41.
Price AP, England KA, et al. Development of a decellularized lung bioreactor system for bioengineering the lung: the matrix reloaded. Tissue Eng Part A. 2010;16:2581–91.
Petersen TH, Calle EA, Colehour MB, et al. Matrix composition and mechanics of decellularized lung scaffolds. Cells Tissue Org. 2012;195:222–31.
Osada H, Takeuchi S, Kojima K, Yamate N. The first step of experimental study on hybrid trachea: use of cultured fibroblasts with artificial matrix. J Cardiovasc Surg (Torino). 1994;35:165–8.
Vacanti CA, Paige KT, Kim WS, Sakata J, Upton J, et al. Experimental tracheal replacement using tissue-engineered cartilage. J Pediatr Surg. 1994;29:201–4.
Paz AC, Kojima K, Iwasaki K, Ross JD, Canseco JA, et al. Tissue engineered trachea using decellularized aorta. J Bioeng Biomed Sci. 2011;S2:001.
DeQuach JA, et al. Simple and high yielding method for preparing tissue specific extracellular matrix coatings for cell culture. PLoS One. 2010;5:e13039.
Ott HC, Clippinger B, Conrad C, Schuetz C, Pomerantseva I, Ikonomou L, Kotton D, Vacanti JP. Regeneration and orthotopic transplantation of a bioartificial lung. Nat Med. 2010;16:927–33.
Brown BN, Freund JM, Han LI, Rubin JP, Reing JE, et al. Comparison of three methods for the derivation of a biological scaffold composed of adipose tissue extracellular matrix. Tissue Eng. 2011;17:411–21.
Gilbert TW, Sellaro TL, Badylak SF. Decellularization of tissues and organs. Biomat. 2006;27:3675–83.
Gupta SK, Dinda AK, Potdar PD, Mishra NC. Modification of decellularized goat-lung scaffold with chitosan/nanohydroxyapatite composite for bone tissue engineering applications. BioMed Res Internat 2013;2013:1–11.
Sano MB, Neal RE, Garcia PA, Gerber D, Robertson J, Davalos RV. Towards the creation of decellularized organ constructs using irreversible electroporation and active mechanical perfusion. Biomed Eng Online. 2010;9:83.
Shupe T, Williams M, Brown A, Willenberg B, Petersen BE. Methods for the decellularization of intact rat liver. Organogen. 2010;6:134–6.
Acknowledgments
None.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Khan, A.A., Vishwakarma, S.K., Bardia, A. et al. Repopulation of decellularized whole organ scaffold using stem cells: an emerging technology for the development of neo-organ. J Artif Organs 17, 291–300 (2014). https://doi.org/10.1007/s10047-014-0780-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10047-014-0780-2