Abstract
Purpose
Abdominal surgeries are common surgical procedures worldwide. Incisional hernias commonly develop after abdominal wall surgery. Surgery is the definite treatment for most incisional hernias but carries a higher rate of complications. Although frequently used, the real benefit of using drain tubes to reduce surgical complications after incisional hernia repair is uncertain.
Methods
PubMed and Embase databases were searched for studies that compared the outcomes of drain vs. no-drain placement and the risk of complications in patients undergoing incisional hernia repair. Primary endpoints were infection, seroma formation, length of hospital stay, and readmission rate.
Results
From a total of 771 studies, we included 2 RCTs and 4 non-RCTs. A total of 40,325 patients were included, of which 28 497 (71%) patients used drain tubes, and 11 828 (29%) had no drains. The drain group had a significantly higher infection rate (OR 1.89; CI 1.13–3.16; P = 0.01) and mean length of hospital stay (Mean Difference—MD 2.66; 95% CI 0.81–4.52; P = 0.005). There was no difference in seroma formation and the readmission rate.
Conclusion
This comprehensive systematic meta-analysis concluded that drain tube placement after incisional hernia repair is associated with increased infection rate and length of hospital stay without affecting the rate of seroma formation and readmission rate. Prospective randomized studies are required to confirm these findings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Abdominal surgeries are common surgical procedures worldwide. However, approximately 20% of these procedures are associated with complications related to wound healing, which may eventually lead to the development of incisional hernias. An incisional hernia can develop at the site of the previous surgical incision due to improper closure of the abdominal wall, and open abdominal surgery carries an important risk [1]. Incisional hernias can be asymptomatic or present with symptoms such as pain, discomfort, bowel obstruction, incarceration, and strangulations [2]. Therefore, the repair of incisional hernias has become a common procedure in the field of general surgery, with an estimated incidence rate of 15% to 20% following laparotomy [2]. Recurrence after initial hernia repair is a common complication. Although surgery remains the definitive treatment for incisional hernias, it frequently leads to complications such as seroma formation and infections [3].
Drains are used in many surgical fields to reduce the fluid collection in the surgical site and reduce seroma formation. Nevertheless, their effectiveness in preventing complications following incisional hernia repair remains a topic of uncertainty. In a retrospective analysis conducted by White et al. on patients who underwent incisional hernia repairs, they observed a higher occurrence of wound infections among individuals who had drains inserted compared to those who did not [4]. Prior systematic review did not find enough studies for evaluation and cited only one randomized controlled study comparing two groups, both using different types of drains [5].
Due to insufficient evidence, there is no standard routine care concerning using drains after incisional hernia repair. In Australia, for instance, a survey showed a divided opinion among surgeons, with some advocating for drains and others not using them [6]. The situation became even more complex when a legal case in Australia ruled in favor of drain usage, causing controversial opinions among experts [7]. This case brought more attention to the topic as there is insufficient evidence. The existing studies in the literature present a conflicting array of studies with varied outcomes on this matter, further complicating the issue [8,9,10,11,12]. Therefore, we perform a systematic meta-analysis to evaluate the influence of drains on the incidence of complications after incisional hernia repair.
Methodology
Search strategy
This systematic meta-analysis was conducted according to the recommendations from the Cochrane Collaboration and the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement guidelines [13]. Two authors (V.S. and F.R.E) independently reviewed the literature, and disagreement was solved by the third author (B.O.T). Systematic search from PubMed and EMBASE databases for published studies were performed using the following heading terms: ‘Incisional Hernia Repair,’ ‘Incisional Hernia,’ ‘Postoperative Hernia,’ Surgical Drain,’ ‘Drain,’ ‘Suction,’ and ‘Drainage.’ There were no restrictions on the publication year. The pre-specified research protocol has been registered and is available at PROSPERO (CRD42023452567).
Selection criteria
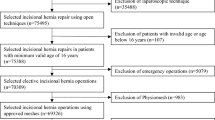
We include studies that met the following criteria: (1) Studies with only incisional hernia repair, (2) Comparing the use of the drain vs. no-drain tubes to reduce complications, (3) Studies that reported at least one of the outcomes of interest, (4) in English, Portuguese, and Spanish. Reviews, case reports, and editorials were excluded.
Endpoints
We extracted baseline characteristics and the endpoints reported in Table 1 and 2. for the analysis using pre-specified criteria for the search, data extraction, and quality assessment. We perform a systematic meta-analysis on the following endpoints: infection rate, seroma formation, abscesses formation, hematoma, wound dehiscence, evisceration, length of hospital stay, and readmission rate.
Quality assessment
The risk of bias and quality assessment of each individual study was performed independently by two authors (B.O.T and VS). Quality assessment of randomized controlled trials was performed with Cochrane’s tool for assessing bias in randomized trials [14], wherein studies are categorized as high risk, low risk, or moderate in five domains: randomization, deviation from intended intervention, missing outcome data, measurement of the outcome, and selection of the reported results. Non-randomized studies were appraised using the Cochrane Collaboration tool for assessing the risk of bias in non-randomized studies (ROBINS-I) [15]. Each study was categorized as critical, serious, moderate, and low risk in all seven domains: confounding, selection, classification, deviations from intended interventions, missing data, measurement of the outcomes, and selection of reported results. Publication bias was investigated with funnel-plot analysis of the primary outcomes.
Statistical analysis
The systematic meta-analysis was performed per recommendations from the Cochrane Collaboration and PRISMA statement guidelines. Treatment effects for binary endpoints were compared using pooled HR or odds ratios (OR) with 95% confidence intervals. Weighted mean differences were used to pool continuous outcomes. Heterogeneity was evaluated with the Cochran Q test and I2 statistics; P values inferior to 0.10, and I2 > 25% were considered significant for heterogeneity. A fixed-effect model was used for endpoints with I2 < 25% (low heterogeneity). DerSimonian and Laird random-effects models were used in pooled outcomes with high heterogeneity. Review Manager 5.4 (Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark) was used for statistical analysis.
Results
Study selection and characteristics
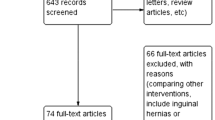
Our search yielded 771 results; 17 studies remained for full-text review after duplicate removal and exclusion of studies that did not meet inclusion criteria based on abstract and title screening, Fig. 1. Finally, we included 6 studies, 2 randomized controlled studies, and 4 non-randomized controlled studies, comprising 40,325 patients. A drain tube was placed in 71% of patients, and 29% had no drains. The age range varied from 55 to 63 for patients with drain and 52 to 62 years old for patients without drain. The mean BMI ranged from 28.4 to 31.5 in the drain group and 27.9 to 30.9 BMI in the non-drain group. The proportion of current smokers at the time of the procedure in both groups was 13%, Table 1.
Pooled analysis
All six studies reported infection rate, five studies reported seroma formation, and three studies reported readmission rates and length of hospital stay. Meta-analysis showed an increased incidence of surgical infection in the patients who had drain (OR 1.89; CI 1.13—3.16; P = 0.01), Fig. 2. The length of hospital stay was also significantly higher in the drain group (Mean Difference—MD 2.66; 95% CI 0.81–4.52; P = 0.005), Fig. 3. There was no difference in seroma formation rate between the groups (OR 1.22; CI 0.80—2.19; P = 0.27), Fig. 4. Analysis of the readmission rate did not find a difference between the groups (OR 0.99; 95% CI 0.59–1.66; P = 0.96), Fig. 5.
Quality assessment
This meta-analysis included two RCTs with low risk of bias and four non-RCTs with moderate risk.
The appraisal of each individual study is reported in Fig. 6a for RCTs and Fig. 6b for non-RCTs. Overall, randomized controlled trials were classified as having a low risk of bias, and non-RCTs as moderate risk of bias.
Discussion
This systematic meta-analysis of 6 studies and 40,325 patients compare drain tubes vs. no-drain usage following incisional hernia repair and the risk of surgical complications. The main findings were as follows: (1) The odds of postoperative infection are approximately 90% higher in patients who had a drain tube placed following incisional hernia repair (OR 1.89; P = 0.01); (2) patients in the drain group spent twice as much time in the hospital after the surgical procedure (MD 2.66; P = 0.005); (3) seroma formation rate and readmission rate are comparable between the groups.
Drains are often used after incisional hernia repair, expecting the reduction of surgical complications; however, some studies reported increased infection rates with their use [4]. There is no clear evidence in the literature to support the use of drains for incisional hernia repair; therefore, no specific recommendation is available to guide surgeons. Moreover, the use of the drain following incisional hernia repair widely varies among surgeons [6]. Willemin et al., in their RCT, reported a decreased overall complication rate in the drain group, but when analyzing each subcategory of the complications, no significant difference between drain and the non-drain group was found, which emphasizes that the reduction of the overall complication was not directly related to the drain usage.
The RCTs [9, 10] did not exhibit significant differences in infection occurrence between patients with drain vs. the non-drain groups. In addition, Tejerizo et al. reported similar outcomes in their retrospective analysis, including 102 patients showing no difference between the groups. On the other hand, Sahm et al., in a registry-based analysis with 39,523 patients, demonstrated an increased infection rate in the drain group, although the patients in this group had more preoperative risk factors than the non-drain group. In addition, multivariate analysis demonstrated increased intraoperative complications in those who used the drain. Similarly, Luo et al., in a study with 410 patients, including different surgical techniques for incisional hernia repair, demonstrated an increased infection rate in patients with a drain placed compared to those without a drain (10.8% vs. 3.6%, P = 0.005), respectively, concordant to the previous study [4]. However, stratifying these patients according to the complexity level of their hernias, “Complex incisional hernia (CIH),” complexity risk criteria: smoker, obesity, and lower abdominal wound. CIH level 1 if they met 1/3 criteria, CIH level 2 if 2/3 criteria met, CIH level 3 if they met all 3 criteria, and simple hernia without any risk criteria. The infection rate difference only remains statistically significantly higher in the drain group vs. the non-drain group in the CIH level 1 subgroup (P = 0.006). Lous et al. analyzed the drain’s impact according to its location in their study [8]. Location of the drains, whether in contact with mesh or subcutaneous, might influence the occurrence of complications. They reported an increased surgical site occurrence (SSO) when drains are placed in direct contact with the mesh compared to subcutaneously placed drains. This is an important finding that raised the question of whether the use of the drains and also the location where they are placed (whether or not in contact with mesh) could impact surgical complications. Most of the previous studies did not specify the location of the drain. Future studies should assess this question. This meta-analysis showed increased odds of infection rate in the patients with drain tubes (OR 1.89).
The use of the drains is associated with increased fluid evacuation from the incision site, although their effectiveness in preventing seroma formation is uncertain. Drain usage following robotic retromuscular ventral hernia repair (rVHR) was found to reduce the seroma formation (P < 0.0001) at 30 days postoperative compared to no-drain placement [16]. Whestphalen et al., a randomized controlled study, did not find significant differences in seroma formation in the drain vs. non-drain group following incisional hernia repair. [9] In the same way, Luo et al. reported no difference between the groups. Conversely, Sahm et al. reported increased seroma formation in drained patients; despite selection bias, this study represents a real-life practice scenario since surgeons tend to use drains in more complex hernias and high-risk patients. Our pooled analysis found no statistical difference in seroma formation with or without drain usage (P = 0.27).
Several studies reported prolonged hospital stay in the group who used drains [8, 11], while some did not find a statistically significant difference in the hospital stay comparing drain vs. no-drain following incisional hernia repair [10]. In this meta-analysis, we found that drain tubes were associated with an increased length of hospital stay (P = 0.005). However, no difference was seen in the readmission rate.
This is the first meta-analysis with studies evaluating post-surgical outcomes between patients using drain vs. no drain following incisional hernia repair. Few limitations need to be considered in this study. Most importantly, four of the six included studies were not randomized, moreover, some studies included different surgical techniques. Comorbidity conditions such as age, DM, obesity, COPD, and the proportion of smokers were similar between the groups in each study, except for Sahm et al., where patients with a drain placed had significantly higher comorbidity. Hernia size was similar between the groups in most studies, except for Lou et al., more patients with large hernias (> 10 cm) in the non-drain group and two studies [12, 17] reported more patients with large hernias in the drain group. These retrospective studies are susceptible to retrospective data collection bias. The difference in surgical technique was expected since different surgical approaches are currently acceptable for incisional hernia repair.
Conclusion
This meta-analysis, including 6 studies and 40,325 patients, investigated the impact of drain placement following incisional hernia repair. We found that drain usage does not impact seroma formation and readmission rate. Conversely, its usage was associated with increased infection and length of hospital stay. Additional prospective randomized studies with larger patient populations and controlling the comorbidity and risk factors are needed to confirm these findings and further elucidate the subject.
References
Berrevoet F (2018) Prevention of incisional hernias after open abdomen treatment. Front Surg 5:11. https://doi.org/10.3389/fsurg.2018.00011
Hope WW, Tuma F (2023) Incisional hernia. In: StatPearls [Internet]. StatPearls Publishing, Treasure Island, FL. https://www.ncbi.nlm.nih.gov/books/NBK435995/. Accessed 12 Jun 2023
den Hartog D, Dur AH, Tuinebreijer WE, Kreis RW (2008) Open surgical procedures for incisional hernias. Cochrane Database Syst Rev 2008(1):CD006438. https://doi.org/10.1002/14651858.cd006438.pub2
White TJ, Santos MC, Thompson JS (1998) Factors affecting wound complications in repair of ventral hernias. Am Surg 64:276–280
Gurusamy KS, Allen VB et al (2013) Wound drains after incisional hernia repair. Cochrane Database Syst Rev (12):CD005570. https://doi.org/10.1002/14651858.CD005570
Luo Y, Mohammed Jinnaah S, Masood D, Hodgson R (2020) Drain tube use in incisional hernia repair: a national survey. Hernia 25(2):427–433. https://doi.org/10.1007/s10029-019-02115-3
Wysocki AP, McGowan B (2018) To drain or not to drain: Supreme Court has the answer. ANZ J Surg 88(1–2):115. https://doi.org/10.1111/ans.14285
Louis V, Diab S, Villemin A, Brigand C, Manfredelli S, Delhorme JB, Rohr S, Romain B (2023) Do surgical drains reduce surgical site occurrence and infection after incisional hernia repair with sublay mesh? A non-randomised pilot study. Hernia 27(4):873–881. https://doi.org/10.1007/s10029-023-02768-1
Westphalen AP, Araújo ACF, Zacharias P, Rodrigues ES, Fracaro GB, Lopes Filho GDJ (2015) Repair of large incisional hernias. To drain or not to drain. Randomized clinical trial. Acta Cir Bras 30(12):844–851. https://doi.org/10.1590/s0102-865020150120000009
Willemin M, Schaffer C, Kefleyesus A, Dayer A, Demartines N, Schäfer M, Allemann P (2022) Drain versus no drain in open mesh repair for incisional hernia, results of a prospective randomized controlled trial. World J Surg 47(2):461–468. https://doi.org/10.1007/s00268-022-06725-4
Luo Y, Masood D, Mohammed Jinnaah S, Tacey M, Hodgson R (2020) Do drain tubes help reduce risks of post-operative complications in complex incisional hernia repair (as defined by a recent court ruling)? ANZ J Surg 90(6):1080–1085. https://doi.org/10.1111/ans.15875
Tejerizo JBT, Bartoli JD, Dreizzen E (2021) Utilidad del drenaje en las eventroplastias con malla. Rev Hispanoam Hernia 9(1):10–14. ISSN-e 2255-2677. https://doi.org/10.20960/rhh.00277
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. https://doi.org/10.1136/bmj.n71
Sterne JAC, Savović J, Page MJ et al (2019) RoB 2: a revised tool for assessing risk of bias in randomized trials. BMJ 366:l4898. https://doi.org/10.1136/bmj.l4898
Sterne JA, Hernán MA, Reeves BC et al (2016) ROBINS-I: a tool for assessing risk of bias in non-randomized studies of interventions. BMJ 355:i4919. https://doi.org/10.1136/bmj.i4919
Miller BT, Tamer R, Petro CC et al (2023) Retromuscular drain versus no drain in robotic retromuscular ventral hernia repair: a propensity score-matched analysis of the abdominal core health quality collaborative. Hernia 27:409–413. https://doi.org/10.1007/s10029-022-02696-6
Sahm M, Pross M, Hukauf M, Adolf D, Köckerling F, Mantke R (2023) Drain versus no drain in elective open incisional hernia operations: a registry-based analysis with 39,523 patients. Hernia. https://doi.org/10.1007/s10029-023-02862-4
Funding
There was no funding for research and publication of this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. V. Sanha, B. O. Trindade and Dr. F. A. R. Elvir declare no conflict of interest.
Registration
See the registration, PROSPERO 2023 (CRD42023452567).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sanha, V., Trindade, B.O. & Elvir, F.A.R. Do surgical drains reduce the postoperative surgical complications following incisional hernia repair? A systematic meta-analysis. Hernia 28, 377–384 (2024). https://doi.org/10.1007/s10029-024-02961-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-024-02961-w