Abstract
Purpose
There has not been a consensus on the superiority of a surgical approach for minimally invasive ventral hernia repair. This systematic review and meta-analysis (SRMA) aims to compare clinical, and patient-reported outcomes of robotic-assisted ventral hernia repair (rVHR) to traditional endo-laparoscopic ventral hernia repair (lapVHR).
Methods
We searched PubMed, EMBASE, Cochrane and Scopus from inception to 16th March 2021. We selected randomised controlled trials and propensity score matched studies comparing rVHR to lapVHR. A meta-analysis was done for the outcomes of operative time, length of hospital stay, open conversion, recurrence, surgical site occurrence and cost.
Results
A total of 5 studies (3732 patients) were included in the qualitative and quantitative synthesis. Significantly shorter operative times were reported with the lapVHR as compared to rVHR (weighted mean difference (WMD): 62.52, 95% CI: 50.84–74.19). There was also significantly less rates of open conversion with rVHR as compared to lapVHR (WMD: 0.22, 95% CI: 0.09–0.54). No significant differences in patient-reported outcomes that was discernible from the two papers that reported them.
Conclusion
Overall, rVHR is comparable to lapVHR with longer operative times but less open conversion. It is, therefore, important to have proper patient selection to maximise the utility of rVHR.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In recent years, the use of robotic-assisted laparoscopic approach has pervaded multiple specialties in surgery. Similarly, in the realm of General Surgery, there has been a likewise increase in the use of robotic assisted approaches in place of traditional endo-laparoscopic procedures [1]. However, it is debatable if the evidence in support of this rapid adoption of robotic assisted procedures is sufficient [2]. Across general surgical laparoscopic procedures, though robotic surgery seems to provide more precise techniques with added intraoperative access and tactile sensation, its increased operative times, costs and operator favorability are significant issues to contend with [3].
Within the realm of ventral hernia repair (VHR), traditional endo-laparoscopic approach with intra-peritoneal onlay mesh placement has been widely accepted as the minimally invasive standard of care for such VHR due to their reduced length of stay, reduced blood loss, perioperative outcomes such as wound site infections and physical function of patient, as compared to open mesh repair [4, 5]. Conversely, some studies have found the traditional endo-laparoscopic approach to be associated with increased early post-operative pain, recurrence and patient dissatisfaction [6, 7].
Therefore, proponents of robotic approach to VHR (rVHR) instead of the traditional endo-laparoscopic intraperitoneal mesh placement (lapVHR), quote further reduction in length of stay and reduced post-operative pain, with similar rates of complications and readmissions [8], as reasons to adopt rVHR in place of the previously favoured lapVHR. On the contrary, the issues associated with robotic-assisted laparoscopic approach discussed previously cause hesitancy in adoption of rVHR. In our regional context, cost associated with such rVHR approaches further deters its uptake. In light of the above, this SRMA aims to compare the outcomes of the endo-laparoscopic approach versus the robotic approach in VHR.
Materials and methods
The present study was based on a prespecified protocol registered with PROSPERO International Prospective Register of Systematic Reviews (CRD42021240586) and was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
Search strategy
An electrotonic systematic literature search was conducted on major databases including PubMed, Embase, Cochrane and Scopus from inception to 16th March 2021 with the assistance of a medical librarian with input from study investigators. A combination of Medical Subject Headings (MeSH) terms and non-MeSH terms using Boolean operators were used in PubMed: (("Robotics"[Mesh]) OR (Robotic[Title/Abstract] OR Robotics[Title/Abstract] OR Robot[Title/Abstract] OR Robots[Title/Abstract])) AND (("Hernia, Ventral"[Mesh]) OR (ventral hernia[Title/Abstract] OR ventral hernias[Title/Abstract] OR incisional hernia[Title/Abstract] OR incisional hernias[Title/Abstract] OR umbilical hernia[Title/Abstract] OR umbilical hernias[Title/Abstract] OR abdominal wall[Title/Abstract] OR herniorrhaphy[Title/Abstract])). The full electronic search strategy can be found as a supplementary file. Gray literature search was done by reviewing the bibliography of included studies and related review articles.
Eligibility criteria
We included randomised controlled trials (RCTs) and propensity score matched (PSM) studies comparing the outcomes of robotic versus endo-laparoscopic ventral hernia repair. No restrictions were made on language or date of publication. We included meeting abstracts if there were sufficient results to analyse to limit publication bias. We excluded animal studies, case series and case reports.
Study selection
All studies were imported into EndNote X9 and duplicate studies were removed electronically then manually searched. Two reviewers independently (M.Y., J.W.) screened and assessed the studies for potential inclusion by their titles and abstracts. Disagreements were resolved by consensus, or by appeal to a senior author (D.L.).
Risk of bias assessment
Risk-of-bias was assessed using the Cochrane risk-of-bias tool for RCTs and Newcastle–Ottawa Scale (NOS) tool for non-randomized studies. The Cochrane risk-of-bias tool evaluates seven key domains in RCTs: random sequence generation; allocation concealment; masking of participants and personnel; blinding of outcome assessment; incomplete outcome data; selective outcome reporting; and other sources of bias. For nonrandomized studies, we used the NOS instrument which compromises of three domains: selection, comparability, outcome. Studies with 7–9 points were considered to be at low risk of bias, studies with 4–6 points were considered to be at moderate risk of bias and studies with 0–3 points were considered to be at high risk of bias.
Data extraction and outcomes of interest
Two reviewers (M.Y., J.W.) independently extracted the data from the studies of study population (mean age, sex, mean body mass index (BMI), type of ventral hernia, mean hernia width, follow-up), interventions and outcomes of interest which include clinical outcomes [operative time, length of hospital stay, open conversion, recurrence, surgical site occurrence (SSO)], patient-reported outcomes and cost. SSO includes surgical site infection, seroma, wound dehiscence and enterocutaneous fistula. Cost is defined by cost incurred by the initial operation as well as cost during entire stay and those of complications arising from the initial operation were included. It is unclear from the three papers that reported open conversion rates if rVHR cases were converted to lapVHR before open conversion or directly to open conversion. Any disagreements were resolved by consensus, or by appeal to a senior author (D.L.). Any unclear or missing results were clarified with the first and/or senior authors of the respective studies via email.
Statistical analysis
Risk ratios (RR) were used as a summary measure of efficacy for dichotomous data and mean differences (MD) between groups were used for continuous variables. A 95% confidence interval was reported for both measures. If the study provided medians and ranges instead of means ± SD, the means ± SD were imputed, as described by Hozo et al. [9]. If the study provided medians and interquartile ranges instead of means ± SD, the means ± SD were imputed, as described by Wan et al. [10]. The random-effect model was used. Statistical heterogeneity was evaluated using the I2 statistic. I2 values of 0–25%, 25–50% and > 50% were considered to be low, moderate, substantial heterogeneity, respectively. A p value < 0.05 was considered to be significant. The meta-analysis was performed using STATA 14.0.
Results
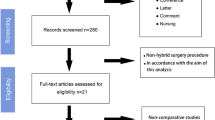
A total of 2058 records were initially identified through database searching. 6 studies met the eligibility criteria as discussed previously. Out of these studies, 1 propensity score matched study was excluded as the authors did not report any outcomes of interest [11]. 5 studies were finally included in the qualitative and quantitative synthesis (Fig. 1). Out of these five studies (3732 patients), 2775 patients had undergone lapVHR and 957 patients had undergone rVHR. Characteristics of the patients included are found in Table 1.
Clinical outcomes
-
1.
Operative time
Operative time was reported in 3 studies (2287 patients) [12,13,14]. We found that there was a significant increase in operative time with the use of rVHR compared to lapVHR (WMD: 62.52, 95% CI 50.84–74.19) (Fig. 2a). There was low level of heterogeneity (I-squared = 0.0%, p = 0.968).
-
2.
Length of hospital stay
Length of hospital stay was reported in 4 studies (3517 patients) [12,13,14,15]. We found a numerical trend towards shorter length of hospital stay for rVHR compared to lapVHR; however, this was not significant (WMD: − 0.32, 95% CI − 1.04 to 0.41) (Fig. 2d). There was significant heterogeneity (I-squared = 77.4%, p = 0.004).
-
3.
Open conversion
Rates of open conversion was reported by 3 studies (3442 patients) [12, 14, 15]. We found a significantly lower rate of open conversion with rVHR as compared to lapVHR (WMD: 0.22, 95% CI 0.09–0.54) (Fig. 2b). There was low-level heterogeneity (I-squared = 0.0%, p = 0.539).
-
4.
Recurrence
Hernia recurrence was reported in 2 papers studied (339 patients) [16, 17]. There was a numerical trend toward less recurrence in rVHR as compared to lapVHR which was not significant (WMD: 0.65, 95% CI 0.21–1.99) (Fig. 2e). There was low-level heterogeneity (I-squared 0.0%, p = 0.800).
-
5.
Surgical site occurrence
All five studies reported surgical site occurrence (SSO) as an outcome (3732 patients) [13,14,15,16,17]. There was a numerical trend favoring rVHR compared to lapVHR; however, this was not significant (WMD: 0.73, 95% CI 0.39–1.39) (Fig. 2c). There was low-level heterogeneity (I-squared 33.4%, p = 0.199).
Cost
Cost incurred was reported in 2 studies (2212 patients) [14, 16]. Cost incurred in rVHR was numerically higher compared to lapVHR; however, this was not significant (WMD: 1396.75, 95% CI − 1733.65 to 4527.16) (Fig. 2f). There was significant heterogeneity (I-squared 76.7%, p = 0.038).
Patient-reported outcomes
A meta-analysis could not be conducted for patient-reported outcomes as the studies report using different patient-reported scales at varying timepoints. The two studies that reported patient-reported outcomes did not yield significant differences between rVHR and lapVHR [12, 13, 16] (Table 2). Specifically, no significant differences were noted in terms of pain scoring metrics. Quality of life metrics that are specific to abdominal wall (AW-QOL) reported minor differences with lapVHR scoring higher than rVHR. It is important to note that no differences were noted by Olavarria et al., in terms of VHR satisfaction as well as cosmetic satisfaction at the 1-year post-operative period.
Quality assessment and risk of bias
Risk of bias assessment is presented in Supplementary Table 2. Of the non-randomized studies, two studies were of high quality [14, 15]. One of the non-randomized studies was deemed to be at high risk of bias [17]. As for the randomized studies, the RCT by Olavarria et al. [12] presented with low risk across all biases from the Cochrane Risk-of-Bias tool. Meanwhile the study by Petro et al. [13] had unclear risk in terms or selection and detection bias. There was also a high risk of reporting bias. The remaining categories were assessed to have low risk of bias.
Discussion
Analysis of RCTs and PSM studies that compared the use of robotic assisted laparoscopic approach to traditional endo-laparoscopic approach in the context of VHR yielded significantly increased operative time but less open conversion for robotic assisted laparoscopic VHR groups.
The significant difference in operative time between the two approaches has been previously discussed in various large studies. A retrospective analysis by the Americas Hernia Society Quality Collaborative (AHSQC) reported that a significantly higher percentage of patients undergoing robotic laparoscopic approach required more than 2 h operative time [8]. These findings were not limited to larger ventral hernias, as corroborated by Chen et al. [18], in their study targeting small-sized ventral hernias. Apart from ventral hernias, such increased operative time were found in comparisons in the context of inguinal hernias [19]. This reflects what is likely to be increased operative time caused by the general implementation of robotic-assisted surgeries rather that delays that stem from the robotic practice specific to VHR. Suggested causes of such delays include time needed for docking and changing instruments on the robot. Otherwise, this could be due to the learning curve associated with the robotic practice [8]. On the contrary, a retrospective evaluation of 368 robotic-assisted cases by Gonzalez et al. [20] suggests that surgeons could effectively achieve comparable operative times to traditional endo-laparoscopic operative times. It must be noted that there are often technical differences with rVHR versus lapVHR such as sewing meshes in place rather than tacking them in place, as well as sewing the defect close in most rVHR procedures. However, further prospective studies that compare specific operative methods as well as assess for a discernible surgical learning curve are needed.
It is also noted that less conversion to open was noted in the robotic-assisted cohorts. Main causes of conversion have been noted to be large hernia size, poor surgical anatomy such as in the context of dense adhesions as well as intra operative complications such as bowel injury [20]. The robotic-assisted approach reduces the requirement for open conversion with superior direct visualization of suture planes as compared to traditional endo-laparoscopic counterparts, thereby allowing surgeons to navigate complicated anatomy. Furthermore, this visualization along with improved dexterity conferred by wristed instrumentation is hypothesized to reduce intraoperative complications [21, 22].
The patient-reported outcomes from both RCTs showed that rVHR does not yield better QOL or pain scores post operatively. This is contrary to popular belief that rVHR is associated with reduced post-operative pain [6]. This post-operative pain had previously been attributed to suturing without tacking of the mesh in rVHR, with tacking of the mesh being noted by authors such as Bansal et al. to increase post-operative pain [23]. Though, the findings seem to contradict previous knowledge, it must be qualified that these studies were limited in their long-term follow-up results. With complications such as chronic pain prevalent in up to 28% of patients undergoing VHR, it can only be assumed that longer term follow-up studies are required [24,25,26].
Similar to what is suggested by current literature on inguinal hernia repair [27, 28], we found numerically lower cost in endo-laparoscopic approach; however, there were no significant differences. This could be due to study by Song et al., which included patients with higher complication rates as well as longer hospital stay, all of which compounded the cost incurred in the endo-laparoscopic approach group. This could have negated higher immediate procedural costs incurred by rVHR group such as for robotic equipment.
Limitations and strengths
Data in the literature on endo-laparoscopic versus robotic ventral hernia repair only started to mature in the recent few years. A recently published network meta-analysis by Goettman et al. [29] compared open, endo-laparoscopic and robotic VHR instead. They found that recurrence was reduced in the robotic approach compared to the endo-laparoscopic and open approach. It is important to note that they had a shorter follow-up time in the robotic group compared to the other arms. In comparison, although our current study included limited number of studies, we focused on high-quality studies comparing lapVHR versus rVHR with comparable follow-up time in both groups which will provide higher level clinical evidence. In addition to clinical outcomes, we also attempted to consider the patient-reported outcomes as well as cost. We would recommend more well-conducted RCTs to further elucidate the safety of the various approaches.
Three of the five studies were specifically focused on mesh placement in the intra-peritoneal space with or without closure of the hernia defect [12, 13, 17]. The last two papers did not specify the mesh location. This could possibly introduce some clinical heterogeneity into the patient cohort. This heterogeneity could, therefore, skew results if more complex robotic procedures are compared with standard laparoscopic procedures.
A further limitation would be the lack of discussion as to whether 2D or 3D lapVHR techniques were compared with. These could be further delineated and compared in further studies as well.
Conclusion
In conclusion, this SRMA demonstrates that rVHR is comparable to lapVHR, but careful patient selection is required in view of increased operative times. Meanwhile, previously held notions of increased cost incurred during rVHR as well as improved patient-reported outcomes after rVHR were not significant.
Availability of data and materials
Data may be made available upon reasonable request.
Code availability
Code may be made available upon reasonable request.
References
Sheetz KH, Claflin J, Dimick JB (2020) Trends in the adoption of robotic surgery for common surgical procedures. JAMA Netw Open 3(1):e1918911–e1918911. https://doi.org/10.1001/jamanetworkopen.2019.18911
Coakley KM, Sims SM, Prasad T et al (2017) A nationwide evaluation of robotic ventral hernia surgery. Am J Surg 214(6):1158–1163. https://doi.org/10.1016/j.amjsurg.2017.08.022
Ahmad A, Ahmad ZF, Carleton JD, Agarwala A (2017) Robotic surgery: current perceptions and the clinical evidence. Surg Endosc 31(1):255–263. https://doi.org/10.1007/s00464-016-4966-y
Rogmark P, Petersson U, Bringman S et al (2013) Short-term outcomes for open and laparoscopic midline incisional hernia repair: a randomized multicenter controlled trial: the ProLOVE (Prospective Randomized Trial on Open Versus Laparoscopic Operation of Ventral Eventrations) Trial. Ann Surg 258:1. https://journals.lww.com/annalsofsurgery/Fulltext/2013/07000/Short_term_Outcomes_for_Open_and_Laparoscopic.7.aspx
Eker HH, Hansson BME, Buunen M et al (2013) Laparoscopic vs open incisional hernia repair: a randomized clinical trial. JAMA Surg 148(3):259–263. https://doi.org/10.1001/jamasurg.2013.1466
Liang MK, Clapp M, Li LT, Berger RL, Hicks SC, Awad S (2013) Patient satisfaction, chronic pain, and functional status following laparoscopic ventral hernia repair. World J Surg 37(3):530–537. https://doi.org/10.1007/s00268-012-1873-9
Carter SA, Hicks SC, Brahmbhatt R, Liang MK (2014) Recurrence and pseudorecurrence after laparoscopic ventral hernia repair: predictors and patient-focused outcomes. Am Surg 80(2):138–148. https://doi.org/10.1177/000313481408000221
Prabhu AS, Dickens EO, Copper CM et al (2017) Laparoscopic vs robotic intraperitoneal mesh repair for incisional hernia: an americas hernia society quality collaborative analysis. J Am Coll Surg 225(2):285–293. https://doi.org/10.1016/j.jamcollsurg.2017.04.011
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 5(1):13. https://doi.org/10.1186/1471-2288-5-13
Wan X, Wang W, Liu J, Tong T (2014) Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 14(1):135. https://doi.org/10.1186/1471-2288-14-135
Altieri MS, Yang J, Xu J, Talamini M, Pryor A, Telem DA (2018) Outcomes after robotic ventral hernia repair: a study of 21,565 patients in the state of New York. Am Surg 84(6):902–908. https://doi.org/10.1177/000313481808400639
Olavarria OA, Bernardi K, Shah SK et al (2020) Robotic versus laparoscopic ventral hernia repair: multicenter, blinded randomized controlled trial. BMJ 2020:370. https://doi.org/10.1136/bmj.m2457
Petro CC, Zolin S, Krpata D et al (2021) Patient-reported outcomes of robotic vs laparoscopic ventral hernia repair with intraperitoneal mesh: the PROVE-IT randomized clinical trial. JAMA Surg 156(1):22–29. https://doi.org/10.1001/jamasurg.2020.4569
Song C, Liu E, Shi L, Marcus D (2017) Comparative effectiveness for ventral hernia repairs among an obese patient population. Surg Endosc 31:S126–S136
LaPinska M, Kleppe K, Webb L, Stewart TG, Olson M (2021) Robotic-assisted and laparoscopic hernia repair: real-world evidence from the Americas Hernia Society Quality Collaborative (AHSQC). Surg Endosc 35(3):1331–1341. https://doi.org/10.1007/s00464-020-07511-w
Dhanani NH, Olavarria OA, Holihan JL et al (2020) Robotic versus laparoscopic ventral hernia repair: one-year results from a prospective, multicenter, blinded randomized controlled trial. Ann Surg 9000;Publish Ahead of Print. https://journals.lww.com/annalsofsurgery/Fulltext/9000/Robotic_versus_Laparoscopic_Ventral_Hernia_Repair_.93726.aspx
Walker PA, May AC, Mo J et al (2018) Multicenter review of robotic versus laparoscopic ventral hernia repair: is there a role for robotics? Surg Endosc 32(4):1901–1905. https://doi.org/10.1007/s00464-017-5882-5
Chen YJ, Huynh D, Nguyen S, Chin E, Divino C, Zhang L (2017) Outcomes of robot-assisted versus laparoscopic repair of small-sized ventral hernias. Surg Endosc 31(3):1275–1279. https://doi.org/10.1007/s00464-016-5106-4
Waite K, Herman M, Doyle P (2016) Comparison of robotic versus laparoscopic transabdominal preperitoneal (TAPP) inguinal hernia repair. J Robot Surg 10:239–244
Gonzalez A, Escobar E, Romero R et al (2017) Robotic-assisted ventral hernia repair: a multicenter evaluation of clinical outcomes. Surg Endosc 31(3):1342–1349. https://doi.org/10.1007/s00464-016-5118-0
Vorst AL, Kaoutzanis C, Carbonell AM, Franz MG (2015) Evolution and advances in laparoscopic ventral and incisional hernia repair. World J Gastrointestinal Surg 7(11):293–305. https://doi.org/10.4240/wjgs.v7.i11.293
Ballantyne GH, Moll F (2003) The da Vinci telerobotic surgical system: the virtual operative field and telepresence surgery. Surg Clin North Am 83(6):1293–1304. https://doi.org/10.1016/S0039-6109(03)00164-6
Bansal VK, Misra MC, Babu D et al (2012) Comparison of long-term outcome and quality of life after laparoscopic repair of incisional and ventral hernias with suture fixation with and without tacks: a prospective, randomized, controlled study. Surg Endosc 26(12):3476–3485. https://doi.org/10.1007/s00464-012-2390-5
Poelman MM, Schellekens JF, Langenhorst BLAM, Schreurs WH (2010) Health-related quality of life in patients treated for incisional hernia with an onlay technique. Hernia 14(3):237–242. https://doi.org/10.1007/s10029-009-0619-6
Snyder CW, Graham LA, Vick CC, Gray SH, Finan KR, Hawn MT (2011) Patient satisfaction, chronic pain, and quality of life after elective incisional hernia repair: effects of recurrence and repair technique. Hernia 15(2):123–129. https://doi.org/10.1007/s10029-010-0750-4
Gronnier C, Wattier-jean-michel V, Favre H, Piessen G, Mariette C (2012) Risk factors for chronic pain after open ventral hernia repair by underlay mesh placement. World J Surg 36:1548–1554. https://doi.org/10.1007/s00268-012-1523-2
Donkor C, González A, Gallas M, Helbig MW, Weinstein C, Rodríguez J (2017) Current perspectives in robotic hernia repair. Robotic Surg Res Rev 4:57–67
Escobar J, Ramos M, Seetharamaiah R, Donkor C, Rabaza J, Gonzalez A (2016) Feasibility of robotic inguinal hernia repair, a single-institution experience. Surg Endoscopy 2016:30. https://doi.org/10.1007/s00464-015-4717-5
Goettman M, Riccardi ML, Vang L, Dughayli M, Faraj C (2020) Robotic assistance in ventral hernia repair may decrease the incidence of hernia recurrence. J Minimal Access Surg 16:335–340
Acknowledgements
The authors would like to thank Annelissa Chin, the senior medical librarian, for her assistance in the development of the search strategy.
Funding
This study was not funded.
Author information
Authors and Affiliations
Contributions
All authors (RK, MY, JW, NS, SW, DL) made substantiable contributions to the conception of the work, the acquisition, analysis, interpretation of data, drafted the work and revised it critically for important intellectual content, approved the version to be published and agree to be accountable for all aspects of the work in ensuring that questions to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts of interest to declare.
Ethics approval
Not applicable.
Human and animal rights
This article does not contain any studies with human participants or animals performed by any of the authors. As this was a systematic review and meta-analysis of published studies.
Informed consent
Informed conset was not necessary.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mohan, R., Yeow, M., Wong, J.Y.S. et al. Robotic versus laparoscopic ventral hernia repair: a systematic review and meta-analysis of randomised controlled trials and propensity score matched studies. Hernia 25, 1565–1572 (2021). https://doi.org/10.1007/s10029-021-02501-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-021-02501-w