Abstract
Purpose
The use of closed incision negative pressure wound therapy (ciNPWT) in abdominal wall reconstruction is heavily debated. The current literature shows mixed results for its efficacy in preventing surgical site occurrences (SSOs), and many of the studies are limited by small sample size or a lack of generalizability. We sought to assess whether the use of prophylactic ciNPWT has an effect on reducing the rate of SSOs.
Methods
Following institutional review board approval, a retrospective analysis of a prospectively collected abdominal wall reconstruction database of a single surgeon at a single institution was completed. Two hundred and seventy patients were reviewed. Univariate and multivariate logistic regressions were performed to assess the effect of each variable on the rate of SSOs.
Results
Two hundred and fifty-eight patients (95.56%) met inclusion criteria. One hundred and fifty-nine (61.63%) of these patients received ciNPWT. The median duration of ciNPWT was 6 days. Multivariate logistic regression analysis showed no significant difference in the prevalence of SSOs between groups (OR = 0.843, 95% CI [0.445–1.594], p = 0.598). It did, however, show a significant decrease in the rates of seroma (7.07% vs. 0.63%, p = 0.004). Moreover, skin resection was associated with a decreased rate of SSO (OR = 0.295, 95% CI [0.096–0.911], p = 0.034).
Conclusions
ciNPWT was not associated with a decrease in SSOs following abdominal wall reconstruction but did show a statistically significant decrease in postoperative seromas. Future, large prospective analyses may help further discover the utility of ciNPWT in reducing SSOs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Surgical site occurrences (SSOs), defined as a surgical site infection (SSI), seroma, hematoma, wound dehiscence, enterocutaneous fistula, cellulitis, non-healing incisional wound, fascial disruption, skin or soft tissue necrosis, wound serous or purulent drainage, stitch abscess, infected mesh or exposed mesh [1], are possible complications of abdominal wall reconstruction (AWR), with overall rates ranging from 29 to 63.6% [2,3,4,5,6]. Contributors to the high rates include: (1) comorbidities in this patient population such as obesity, diabetes, smoking, and poor nutrition; (2) the need for complex surgical techniques including component separation, the use of mesh, skin resection, and the creation of adjacent skin flaps; (3) the possibility of contamination as a result of enterotomies or infected mesh from a previous procedure [6].
Closed incisional negative pressure wound therapy (ciNPWT) has been described as a method to reduce SSOs following AWR. While the underlying mechanism is not fully understood, current hypotheses that explain how it decreases the rate of SSOs include decreasing lateral stresses around the incision, changing the direction of the stresses to a distribution more typical of intact tissue, increasing the force required to disrupt the closed incision, increasing perfusion, and increasing lymphatic clearance [7,8,9]. ciNPWT is not unique to AWR and has been shown to reduce complication rates in other conditions, such as open fractures and diabetic foot amputations, though there is a lack of high-level evidence [10, 11]. In the AWR population, previous studies have demonstrated reductions in rates of SSOs in patients using ciNPWT [12,13,14], however, the results are mixed and there still remains a paucity in strong evidence supporting its routine use [15].
To that end, the primary goal of this study was to investigate the effectiveness of ciNPWT following AWR to provide an evidence-based analysis of its efficacy in reducing SSOs within 30 days.
Methods
Study design and data collection
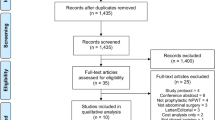
A retrospective analysis of the prospectively collected database from September 13, 2013 to March 10, 2020 was performed. Two hundred and seventy patients were analyzed. Patients were excluded if they did not have primary closure of the abdominal wall (n = 4) or follow-up within 30 days (n = 8). The remaining 258 patients were included. Patient demographics, history of smoking (smoked > 30 days before surgery vs. never smoked), body mass index (BMI), immunosuppression status (at time of surgery), medical comorbidities, operative details, Ventral Hernia Working Group (VHWG) [16], Kanters [17] grading scales, and SSOs within 30 days were collected. ciNPWT was not used in patient prior to April 2016. Then, for a brief period of time, it was used in patients who were at risk for delayed wound healing, followed by current practice where it is used uniformly based on the Chopra et al paper detailing the cost effectiveness of the therapy [18]. The primary outcome of interest was SSO, which we defined as infection (soft tissue abscess and/or cellulitis), seroma, hematoma, dehiscence, skin necrosis, enterocutaneous fistula, mesh infection, hernia recurrence, and/or bulge within 30 days under the premise that the effect of ciNPWT in helping to reduce incision-related occurrences would lead to an overall decrease in all SSOs as per the “vicious cycle” concept espoused by Holihan et al. [19].
Statistical analysis
Variables were compared using Pearson’s χ2 or Fisher’s exact test, when applicable, for categorical variables, Mann–Whitney U tests for non-normally distributed numerical variables, and Student’s t test for normally distributed continuous variables. The normality of continuous variables was assessed with a Q–Q plot. Predictors of SSOs were assessed using a univariate logistic regression. Furthermore, a multivariate logistic regression was performed to account for baseline differences between groups. The median of the first half of the data is presented as Q1, while the median of the second half is presented as Q3, for applicable data. All data were analyzed using SPSS Version 27.0 (IBM Corp. Released 2020. IBM SPSS Statistics for Mac, Version 27.0. Armonk, NY: IBM Corp) statistical software. A p value < 0.05 was considered statistically significant.
Results
Study population and characteristics
One hundred and fifty-nine (61.63%) patients received ciNPWT, while the remaining 99 (38.27%) patients received standard dressing, which consisted of bacitracin ointment with xeroform and standard gauze, with standard surgical tape. There was no significant difference in age between the active and control group (56 [46, 65] vs. 58 [51, 65], p = 0.269). Patients who received ciNPWT had significantly higher rates of diabetes (14.10% vs. 27.05%, p = 0.015), skin resection (85.86% vs. 94.34%, p = 0.020), and skin flaps (58.60% vs. 86.90%, p < 0.001). However, BMI (32 [28, 36] vs. 33 [29, 37], p = 0.306), VHWG grade (p = 0.259), immunosuppression status (21.21% vs 19.50%, p = 0.738), and Kanters grade (p = 0.434) did not vary significantly amongst the two groups. There were no active smokers at the time of surgery, and history of smoking with a quit date > 30 days prior to the operation did not vary significantly between groups (47.50% vs. 61.57%, p = 0.522). Of those who received ciNPWT, the median duration of use was 6 days, with Q1 being 5 and Q3 being 7. Demographic variables are shown in Table 1.
Prevalence of surgical site occurrences
65 (25.50%) of 258 patients had an SSO within 30 days of surgery. None of these variables, including age (p = 0.254), diabetes (23.08% vs. 21.76%, p = 0.825), history of smoking with a quit date > 30 days prior to the operation (55.39% vs. 48.19%, p = 0.315), and immunosuppression status (12.31% vs. 22.80%, p = 0.068), were statistically significant between groups. Table 2 shows the association of variables of interest with having an SSO.
The use of ciNPWT was not associated with a significantly lower overall prevalence of SSO (27.27% vs. 23.89%, p = 0.544). However, ciNPWT was associated with a statistically significant decrease in the rate of seroma (7.07% vs. 0.63%, p = 0.004). Table 3 shows the association of the individual occurrences of each outcome within our definition of SSO along with whether or not ciNPWT was used.
Within our univariate analysis, the only factor that was significantly associated with increased rates of SSO was BMI (OR = 1.052, 95% CI [1.010–1.095], p = 0.015). Notably, age (OR = 1.001, 95% CI [0.979–1.023], p = 0.948) and the use of ciNPWT (OR = 0.837, 95% CI [0.472–1.485], p = 0.544) did not have significant associations with increased rates of SSO (Table 4). However, multivariate analysis showed significant reductions in the rates of having an SSO when the patient was taking immunosuppressive medications (OR = 0.411, 95% CI [0.171–0.988], p = 0.047) and when they had skin resected during the operation (OR = 0.295, 95% CI [0.096–0.911], p = 0.034). However, the use of ciNPWT did not show a significant association with having an SSO (OR = 0.843, 95% CI [0.445–1.594], p = 0.598) (Table 4).
Discussion
There are currently no published randomized controlled trials on the use of closed incisional negative pressure wound therapy for abdominal wall reconstruction, leaving a lack of high-level evidence for its efficacy. Thus, there is a need for strong retrospective studies to help address this question in the meantime, and our report focuses on this gap in the literature to further elucidate the potential benefits of its use.
Many groups have published evidence about the effectiveness of ciNPWT with mixed results, varying based on which negative outcome is reduced [2, 6, 13,14,15, 20, 21]. Condé-Green et al. found a reduction in skin dehiscence and overall wound complications (including skin dehiscence, skin/fat necrosis, and infection) with the use of ciNPWT, but did not find significant reductions in skin/fat necrosis, infection, hernia recurrence, seroma, or hematoma [2]. Similarly, de Vries et al. found significant reductions in the rates of superficial and incisional wound infections in their ciNPWT group, but did not find them in surgicial site infections overall, enterocutaneous fistulas, seromas, hematomas, or skin necrosis [6]. A matched cohort study comparing patients who received ciNPWT after incisional hernia repair with those who did not by Hopkins et al. found a decrease in incidence of SSI in their matched cohort but no differences in SSO, overall complications, readmission, or emergency department visits [20]. Although many of these studies are limited by their small sample size, some larger studies do exist. A meta-analysis by Tran et al. from 2006 to 2016 compared 11 studies, including a mixed surgical cohort of 1723 patients that underwent abdominal wall reconstruction. This analysis showed a significant decrease in surgical site infection (SSI) and wound dehiscence in patients who received ciNPWT. However, they reported no significant difference between patients who received ciNPWT and their counterparts who did not, in the rates of seroma, hematoma, reoperation, or readmission [14]. Amongst these studies ciNPWT was found to reduce varying complications. While the reduction of SSIs was common it was not unanimous, and other complications including skin dehiscence and SSO varied greatly.
Several studies did not include bulge or early hernia recurrence in their analyses, which are both potential adverse outcomes of abdominal wall reconstruction. These potential adverse outcomes are included within our definition of SSO because of the “vicious cycle” that can occur with these repairs. For example, cellulitis can lead to a superficial abscess which can become a mesh infection, leading to need for reoperation, mesh removal, and hernia recurrence. A large multicenter database study by Holihan et al. showed that SSI can more than double the chance of hernia recurrence and quadruple the chance for reoperation [19]. Further, a retrospective study of 255 patients by Cobb et al. additionally found that the only predictor of hernia recurrence was the presence of an SSI [22].
When critically examining the mixed results of many of these studies with their associated limitations, which often include a small sample size, multiple surgeons/institutions, variations in study population and technique, and narrow definitions of SSO, there is an obvious need for stronger retrospective studies and randomized controlled trials to further elucidate the effectiveness of ciNPWT for AWR. These limitations were addressed in our paper by retrospectively analyzing a relatively large sample size, only including one surgeon at one institution, and by including a broader definition of SSO.
Within our population of abdominal wall reconstruction patients, ciNPWT was not associated with a significant decrease in the rate of overall SSOs (27.27% vs. 23.89%, p = 0.544). It was, however, associated with a significant decrease in the rate of seroma (7.07% vs. 0.63%, p = 0.004). Moreover, it was not associated with any other statistically significant reductions of variables within our definition of SSO. Being immunosuppressed and having skin resected were associated with statistically significant reductions in the rate of SSO in our population, irrespective of whether they received ciNPWT or standard dressing.
In our study, 65 (25.19%) of 258 patients had an SSO within 30 days of surgery. Of the 159 patients who received ciNPWT, 38 (23.90%) of them went on to have an SSO, while 27 (27.27%) of the 99 patients who did not receive ciNPWT had an SSO. These rates, even within the control group, are below many of those previously reported in the literature, despite including a broader definition of SSOs. This includes results reported by de Vries et al. of a 47% rate of SSI in their overall population, as well as a 51% rate in their control group and a 24% in their NPWT group [6]. Condé-Green et al. found the rate of wound complications to be 63.6% in their control group compared to 22% in their NPWT group [2]. The reported rates in their control groups are significantly higher than ours, possibly suggesting that the effect of ciNPWT may be diminished in our study due to the lower baseline SSO rate within the control group.
The effect of skin resection on rates of SSO has not been thoroughly examined. Our results suggest skin resection and aggressive skin management may play an important role in decreasing the rates of SSO. While skin resection can be difficult to quantify, our technique involves aggressively resecting any necrotic, poorly perfused, tenuous, undermined, or marginal skin [23, 24]. This may help to explain the discrepancy in our rates of SSOs compared to other studies.
Finally, the relationship of immunosuppression and poor wound healing has been well documented in the literature, with most citing decreased wound healing while immunosuppressed [25,26,27,28,29,30]. In our study, however, multivariate logistic regression showed a decrease in the rate of SSO when the patient was immunosuppressed. This is contradictory to previous findings, warranting further investigation.
Limitations
Limitations of our study are those commonly seen in retrospective studies. These include the potential for misclassification bias, for confounding bias by having other risk factors not measured that may have an effect on our outcome, and for lack of generalizability due to this being a single surgeon, single institution study. Lastly, due to study design, it is only powered to find associations, not causations.
Conclusion
The use of negative pressure wound therapy on closed incisions in abdominal wall reconstruction was not associated with a significant difference in the overall rate of surgical site occurrences for patients within our study. However, it was associated with a significantly decreased rate of seromas. The rates of SSOs in both our control and ciNPWT groups were lower than many reported rates in the literature. This can potentially be explained by our single-surgeon’s technique, specifically aggressive skin management. Skin resection was associated with a significant decrease in the rates of SSO in our study and warrants further investigation. Other future investigations may benefit from analyzing if the amount of skin resected has an effect on the rate of surgical site occurrences and further studying if the number of days ciNPWT is used impacts the rate of SSOs.
Availability of data and material
Data utilized for this study was from an IRB approved database that is maintained by the corresponding author and his approved co-investigators.
Code availability
All statistic software was provided by the Ohio State University.
References
DeBord J, Novitsky Y, Fitzgibbons R, Miserez M, Montgomery A (2018) SSI, SSO, SSE, SSOPI: the elusive language of complications in hernia surgery. Hernia. https://doi.org/10.1007/s10029-018-1813-1
Condé-Green A, Chung TL, Holton LH 3rd, Hui-Chou HG, Zhu Y, Wang H et al (2013) Incisional negative-pressure wound therapy versus conventional dressings following abdominal wall reconstruction: a comparative study. Ann Plast Surg 71(4):394–397. https://doi.org/10.1097/SAP.0b013e31824c9073
Basta MN, Fischer JP, Kovach SJ (2015) Assessing complications and cost-utilization in ventral hernia repair utilizing biologic mesh in a bridged underlay technique. Am J Surg 209(4):695–702. https://doi.org/10.1016/j.amjsurg.2014.04.017
Kim H, Bruen K, Vargo D (2006) Acellular dermal matrix in the management of high-risk abdominal wall defects. Am J Surg 192(6):705–709. https://doi.org/10.1016/j.amjsurg.2006.09.003
Rosen MJ, Krpata DM, Ermlich B, Blatnik JA (2013) A 5-year clinical experience with single-staged repairs of infected and contaminated abdominal wall defects utilizing biologic mesh. Ann Surg 257(6):991–996. https://doi.org/10.1097/SLA.0b013e3182849871
de Vries FEE, Atema JJ, Lapid O, Obdeijn MC, Boermeester MA (2017) Closed incision prophylactic negative pressure wound therapy in patients undergoing major complex abdominal wall repair. Hernia 21(4):583–589. https://doi.org/10.1007/s10029-017-1620-0
Wilkes RP, Kilpad DV, Zhao Y, Kazala R, McNulty A (2012) Closed incision management with negative pressure wound therapy (CIM): biomechanics. Surg Innov 19(1):67–75. https://doi.org/10.1177/1553350611414920
Atkins BZ, Tetterton JK, Petersen RP, Hurley K, Wolfe WG (2011) Laser Doppler flowmetry assessment of peristernal perfusion after cardiac surgery: beneficial effect of negative pressure therapy. Int Wound J 8(1):56–62. https://doi.org/10.1111/j.1742-481X.2010.00743.x
Kilpadi DV, Cunningham MR (2011) Evaluation of closed incision management with negative pressure wound therapy (CIM): hematoma/seroma and involvement of the lymphatic system. Wound Repair Regen 19(5):588–596. https://doi.org/10.1111/j.1524-475X.2011.00714.x
Novak A, Khan WS, Palmer J (2014) The evidence-based principles of negative pressure wound therapy in trauma & orthopedics. Open Orthop J 8:168–177. https://doi.org/10.2174/1874325001408010168
Nam D, Sershon RA, Levine BR, Della Valle CJ (2018) The use of closed incision negative-pressure wound therapy in orthopaedic surgery. J Am Acad Orthop Surg 26(9):295–302. https://doi.org/10.5435/jaaos-d-17-00054
Gassman A, Mehta A, Bucholdz E, Abthani A, Guerra O, Maclin MM Jr et al (2015) Positive outcomes with negative pressure therapy over primarily closed large abdominal wall reconstruction reduces surgical site infection rates. Hernia 19(2):273–278. https://doi.org/10.1007/s10029-014-1312-y
Singh D (2018) The role of closed incision negative pressure therapy in abdominal wall reconstruction: a current review of the evidence. Plast Reconstr Surg 142(3 Suppl):156s–162s. https://doi.org/10.1097/prs.0000000000004872
Tran BNN, Johnson AR, Shen C, Lee BT, Lee ES (2019) Closed-incision negative-pressure therapy efficacy in abdominal wall reconstruction in high-risk patients: a meta-analysis. J Surg Res 241:63–71. https://doi.org/10.1016/j.jss.2019.03.033
Anghel EL, Kim PJ (2016) Negative-pressure wound therapy: a comprehensive review of the evidence. Plast Reconstr Surg 138(3 Suppl):129s-s137. https://doi.org/10.1097/prs.0000000000002645
Breuing K, Butler CE, Ferzoco S, Franz M, Hultman CS, Kilbridge JF et al (2010) Incisional ventral hernias: review of the literature and recommendations regarding the grading and technique of repair. Surgery 148(3):544–558. https://doi.org/10.1016/j.surg.2010.01.008
Kanters AE, Krpata DM, Blatnik JA, Novitsky YM, Rosen MJ (2012) Modified hernia grading scale to stratify surgical site occurrence after open ventral hernia repairs. J Am Coll Surg 215(6):787–793. https://doi.org/10.1016/j.jamcollsurg.2012.08.012
Chopra K, Gowda AU, Morrow C, Holton L 3rd, Singh DP (2016) The economic impact of closed-incision negative-pressure therapy in high-risk abdominal incisions: a cost-utility analysis. Plast Reconstr Surg 137(4):1284–1289. https://doi.org/10.1097/prs.0000000000002024
Holihan JL, Alawadi Z, Martindale RG, Roth JS, Wray CJ, Ko TC et al (2015) Adverse events after ventral hernia repair: the vicious cycle of complications. J Am Coll Surg 221(2):478–485. https://doi.org/10.1016/j.jamcollsurg.2015.04.026
Hopkins B, Eustache J, Ganescu O, Cipolla J, Kaneva P, Fried GM et al (2020) S116: Impact of incisional negative pressure wound therapy on surgical site infection after complex incisional hernia repair: a retrospective matched cohort study. Surg Endosc. https://doi.org/10.1007/s00464-020-07857-1
Tadisina KK, Chopra K, Sabino J, Maddox JS, Samra S, Banda A et al (2013) Negative pressure wound therapy for abdominal wall reconstruction. Eplasty 13:ic60
Cobb WS, Warren JA, Ewing JA, Burnikel A, Merchant M, Carbonell AM (2015) Open retromuscular mesh repair of complex incisional hernia: predictors of wound events and recurrence. J Am Coll Surg 220(4):606–613. https://doi.org/10.1016/j.jamcollsurg.2014.12.055
Janis JE, Khansa I (2015) Evidence-based abdominal wall reconstruction: the maxi–mini approach. Plast Reconstr Surg 136(6):1312–1323. https://doi.org/10.1097/prs.0000000000001831
Khansa I, Janis JE (2018) Management of skin and subcutaneous tissue in complex open abdominal wall reconstruction. Hernia 22(2):293–301. https://doi.org/10.1007/s10029-017-1662-3
Guo S, Dipietro LA (2010) Factors affecting wound healing. J Dent Res 89(3):219–229. https://doi.org/10.1177/0022034509359125
Bootun R (2013) Effects of immunosuppressive therapy on wound healing. Int Wound J 10(1):98–104. https://doi.org/10.1111/j.1742-481X.2012.00950.x
Broughton G 2nd, Janis JE, Attinger CE (2006) The basic science of wound healing. Plast Reconstr Surg 117(7 Suppl):12s–34s. https://doi.org/10.1097/01.prs.0000225430.42531.c2
Janis JE, Harrison B (2014) Wound healing: part I. Basic science. Plast Reconstr Surg 133(2):199e–207e. https://doi.org/10.1097/01.prs.0000437224.02985.f9
Janis J, Harrison B (2014) Wound healing: part II. Clinical applications. Plast Reconstr Surg 133(3):383e–392e. https://doi.org/10.1097/prs.0000000000000077
Khansa I, Harrison B, Janis JE (2016) Evidence-based scar management: how to improve results with technique and technology. Plast Reconstr Surg 138(3 Suppl):165s–178s. https://doi.org/10.1097/prs.0000000000002647
Funding
No funding was received for this article.
Author information
Authors and Affiliations
Contributions
APS: study design, data collection and interpretation, drafting article, and final approval. BAS: study design, data collection and interpretation, drafting article, and final approval. HE: study design, data interpretation, drafting article, and final approval. JEJ: study design, data collection and interpretation, revising article, and final approval.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Janis receives royalties from Thieme and Springer Publishing. The remaining authors have nothing to disclose.
Ethics approval
This research protocol was granted IRB approval by The Ohio State University; IRB #2015H0105.
Informed Consent
Following institutional review board approval, patients were prospectively recruited and consented to participate in research for an abdominal wall reconstruction database operated on by a single surgeon.
Human and animal rights
This study does not contain any studies with animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Seaman, A.P., Sarac, B.A., ElHawary, H. et al. The effect of negative pressure wound therapy on surgical site occurrences in closed incision abdominal wall reconstructions: a retrospective single surgeon and institution study. Hernia 25, 1549–1555 (2021). https://doi.org/10.1007/s10029-021-02427-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-021-02427-3