Abstract
Objectives
To compare outcomes of laparoscopic repair to open repair of umbilical and paraumbilical hernias.
Methods
We performed a systematic review in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement standards. The review protocol was registered with International Prospective Register of Systematic Reviews (Registration Number: CRD42016052131). We conducted a search of electronic information sources, including MEDLINE; EMBASE; CINAHL; the Cochrane Central Register of Controlled Trials (CENTRAL); the World Health Organization International Clinical Trials Registry; ClinicalTrials.gov; and ISRCTN Register, and bibliographic reference lists to identify all randomised controlled trials (RCTs) and observational studies comparing outcomes of laparoscopic repair to open repair of umbilical and paraumbilical hernias. We used the Cochrane risk of bias tool and the Newcastle–Ottawa scale to assess the risk of bias of RCTs and observational studies, respectively. Random effects models were applied to calculate pooled outcome data.
Results
We identified three RCTs and seven retrospective cohort studies, enrolling a total of 16,549 patients. Our analyses indicated that open repair was associated with a higher risk of wound infection [Odds ratio (OR) 2.35, 95% CI 1.23–4.48, P = 0.010], wound dehiscence (OR 4.99, 95% CI 1.12–22.28, P = 0.04) and recurrence (OR 4.06, 95% CI 1.54–10.71, P = 0.005), longer length of hospital stay (MD 26.85, 95% CI 8.15–45.55, P = 0.005) and shorter operative time [Mean difference (MD) − 23.07, 95% CI − 36.78 to − 9.35, P = 0.0010] compared to laparoscopic repair. There was no difference in the risk of haematoma (OR 2.03, 95% CI 0.22–18.73, P = 0.53) or seroma (OR 0.67, 95% CI 0.19–2.32, P = 0.53) between the two groups.
Conclusions
The best available evidence (randomised and non-randomised studies) suggests that laparoscopic repair of umbilical or paraumbilical hernias may be associated with a lower risk of wound infection, wound dehiscence and recurrence rate, shorter length of stay but longer operative time. Results from a limited number of RCTs showed no difference in recurrence rates. The quality of the best available evidence is moderate, and selection bias is the major concern due to non-randomised design in most of the available studies. Therefore, considering the level of available evidence, the most reliable approach for repair of umbilical or paraumbilical hernia should be based on surgeon’s experience, clinical setting, patient’s age and size, hernia defect size and anatomical characteristics. High quality RCTs are required.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Umbilical and paraumbilical hernias account for 10–12% of abdominal wall hernias [1]. The best surgical technique for the repair of umbilical and paraumbilical hernias remains controversial. A simple primary suture repair can be used for small defects. Umbilical and paraumbilical hernias have historically been repaired without mesh. The technique of overlapping abdominal wall fascia in a ‘‘vest-over-pants’’ manoeuvre was described by Mayo [2] and remained the most renowned surgical technique for a long time. The Mayo repair has been shown to be associated with high recurrence rates of up to 28% [3]. On the other hand, suture hernioplasty without double breasting of the fascia was commonly used by surgeons. However, the relatively high recurrence rates associated with these techniques increased the popularity of mesh repair. The introduction of mesh repair has improved the recurrence rates after umbilical and paraumbilical hernia repairs [4, 5].
Laparoscopic umbilical hernia repair was first described in the 1990s [3]. The use of laparoscopic repair of ventral hernias has increased in recent years [6]. The literature suggests that the laparoscopic approach has the advantages of reduced recurrence rates, postoperative pain, shorter hospital stay and a diminished morbidity rate, although it is potentially associated with relatively prolonged operative time [6,7,8]. Specifically, the laparoscopic and open repairs of umbilical and paraumbilical hernias have been compared by some authors. However, there is no comprehensive review and meta-analysis in the current literature comparing outcomes of both techniques.
We aimed to perform a comprehensive systematic review and conduct a meta-analysis of outcomes to compare laparoscopic repair to open repair of umbilical and paraumbilical hernias.
Methods
This systematic review was performed according to an agreed predefined protocol which was registered with the International Prospective Register of Systematic Reviews (Registration Number: CRD42016052131). The review was conducted and presented according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement standards [9].
Eligibility criteria
All observational studies and randomised controlled trials (RCTs) investigating outcomes of open versus laparoscopic repair of umbilical or paraumbilical hernia were included. Laparoscopic mesh repair was considered as the intervention of interest and open repair (mesh repair, suture repair or Mayo repair) was considered as the comparator. Adults over 18 years of age undergoing surgery for repair of primary umbilical or paraumbilical hernia were considered as participants of interest. We excluded studies including incisional, recurrent or epigastric hernia.
Outcome measures
Wound complications including wound infection, wound dehiscence, haematoma and seroma were considered as primary outcome measures. The secondary outcome measures included visceral injury, bleeding, incisional hernia, port-site hernia, recurrence, mortality, length of hospital stay (in hours) and operative time (in minutes).
Literature search strategy
Two authors (AS, Shahin H) independently searched the following electronic databases: MEDLINE, EMBASE, CINAHL, and the Cochrane Central Register of Controlled Trials (CENTRAL). The last search was run on 25 December 2016. Thesaurus headings, search operators and limits in each of the above databases were adapted accordingly. The literature search strategy is outlined in Appendix. In addition, World Health Organization International Clinical Trials Registry (http://apps.who.int/trialsearch/), ClinicalTrials.gov (http://clinicaltrials.gov/) and ISRCTN Register (http://www.isrctn.com/) were searched for details of ongoing and unpublished studies. The bibliographic lists of relevant articles and reviews were interrogated for further potentially eligible studies. No language restrictions were applied in our search strategies.
Study selection
The title and abstract of articles identified from the literature searches were assessed independently by two authors (AS, Shahin H). The full texts of relevant reports were retrieved and those articles that met the eligibility criteria of our review were selected. Any discrepancies in study selection were resolved by discussion between the authors. An independent third author (Shahab H) was consulted in the event of disagreement.
Data collection
We created an electronic data extraction spreadsheet which was pilot tested in randomly selected articles and was adjusted accordingly. Our data extraction spreadsheet included: study-related data (first author, year of publication, country of origin of the corresponding author, journal in which the study was published, study design, study size and clinical condition of the study participants), baseline demographic and clinical information of the study populations [age, gender, body mass index (BMI), hernia defect size and previous hernia] and primary and secondary outcome data. Data collection was performed independently by two authors (AS, Shahin H), and disagreements were resolved by discussion. If no agreement could be reached a third author (Shahab H) was consulted.
Methodological quality and risk of bias assessment
Two authors (Shahin H and AK) independently assessed the methodological quality and risk of bias of the included articles using the Cochrane tool and the Newcastle–Ottawa scale (NOS) [10] for assessing the risk of bias of randomised trials and observational studies, respectively. The Cochrane tool assesses domains including selection bias, performance bias, detection bias, attrition bias, reporting bias and other sources of bias, and for each individual domain, classifies studies into low, unclear, and high risk of bias. The NOS uses a star system with a maximum of nine stars to evaluate a study in three domains (eight items): the selection of the study groups, the comparability of the groups and the ascertainment of outcome of interest. For each item of the scale, we judged each study as low risk (one star awarded) or high risk (no star awarded). We determined studies that received a score of nine stars to be of low risk of bias, studies that scored seven or eight stars to be of moderate risk, and those that scored six or less to be of high risk of bias. Disagreements were resolved by discussion between the reviewers. If no agreement could be reached, a third author (Shahab H) acted as an adjudicator. A risk of bias graph was constructed to present the results.
Data synthesis and statistical analyses
For dichotomous outcome variables (wound infection, wound dehiscence, haematoma, seroma, visceral injury, bleeding, incisional hernia, port-site hernia, reoccurrence and mortality), we calculated the odds ratio (OR) of open versus laparoscopic repair as the summary measure. For continuous parameters (length of stay and operation time), we calculated the mean difference (MD) between the two groups.
Individual patient was used as the unit of analysis. Information about dropouts, withdrawals, and other missing data were recorded, and if not reported, we contacted the study authors where possible. We based our analysis on intention-to-treat data from the individual clinical studies.
We used the Review Manager 5.3 software for data synthesis [11]. Because of the anticipated clinical between-study heterogeneity, we used the random effects model for analysis, and the results were reported in a forest plot with 95% confidence intervals (CIs).
Heterogeneity among the studies was assessed using the Cochran’s Q test (χ 2). We quantified inconsistency by calculating I 2 and interpreted it using the following guide: 0–50% may represent low heterogeneity, 50–75% may represent moderate heterogeneity and 75–100% may represent high heterogeneity. We planned to construct funnel plots and evaluate their symmetry to visually assess publication bias for outcomes reported by at least ten studies. To quantify the bias captured by the funnel plot and to formally assess reporting bias, we planned to calculate the Egger’s regression intercept for outcomes reported by at least ten studies using the Comprehensive Meta-Analysis (CMA) software (Biostat, Englewood, NJ). We also planned to calculate the intercept from a linear regression of normalised effect estimate (estimate divided by its standard error) against precision (reciprocal of the standard error of the estimate).
Sensitivity and subgroup analyses
To explore potential sources of heterogeneity and assess the robustness of our results, additional analyses were conducted for outcomes that were reported by at least four studies. For each outcome, we repeated the primary analysis using the random effects and fixed effect model. In addition, we calculated the risk ratio (RR) and risk difference (RD) for each dichotomous variable. We assessed the effect of each study on the overall effect size and heterogeneity by repeating the analysis after removing one study at a time. Also, we planned to perform separate analyses for RCTs with low risk of selection bias in terms of randomisation and allocation concealment, and for observational studies with low or moderate risk of bias to assess the change in direction of the effect size. Moreover, we performed separate analyses for randomised trials and observational studies. Where possible, we also planned to perform subgroup analyses based on type of open repair: mesh repair, suture repair or Mayo repair.
Results
Results of the search
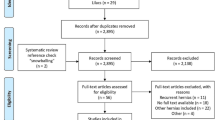
Searches of electronic databases identified 734 articles of which ten studies were eligible for this review. These included three RCTs [12,13,14] and seven retrospective cohort studies [15,16,17,18,19,20,21], enrolling a total of 16,549 patients. Laparoscopic mesh repair was compared with open mesh repair in ten studies, [12,13,14,15,16,17,18,19,20,21] with open suture repair in eight studies, [14,15,16,17,18,19,20,21] and with Mayo repair in one study [19]. A total of 2264 patients underwent laparoscopic repair and 14,285 patients underwent open repair. The median follow-up period was 24 months. The literature search flow chart, baseline characteristics of the included studies and baseline characteristics of the included population are demonstrated in Fig. 1; Tables 1 and 2, respectively.
Methodological quality and risk of bias
The summary and results of methodological quality assessment of the seven observational studies [15,16,17,18,19,20,21] and three RCTs [12,13,14] are demonstrated graphically in Fig. 2.
Outcome synthesis
Wound dehiscence
Wound dehiscence was reported in four studies, [13, 18, 19, 21] enrolling 1279 patients (Fig. 3). The risk of wound dehiscence was higher in open repair group compared to laparoscopic repair group (OR 4.99, 95% CI 1.12–22.28, P = 0.04). A low level of heterogeneity among the studies existed (I 2 = 0%, P = 0.59).
Wound infection
Wound infection was reported in nine studies, [12,13,14, 16,17,18,19,20,21] enrolling 1897 patients (Fig. 3). The risk of wound infection was higher in open repair group compared to the laparoscopic repair group (OR 2.35, 95% CI 1.23–4.48, P = 0.010). A low level of heterogeneity among the studies existed (I 2 = 14%, P = 0.32) (Table 2).
Haematoma
Haematoma was reported in six studies, [12, 17,18,19,20,21] enrolling 1692 patients (Fig. 3). There was no significant difference in the risk of haematoma between the open repair and laparoscopic repair groups (OR 2.03, 95% CI 0.22–18.73, P = 0.53). A high level of heterogeneity among the studies existed (I 2 = 80%, P = 0.0006).
Seroma
Seroma was reported in eight studies, [12,13,14, 17,18,19,20,21] enrolling 1774 patients (Fig. 3). There was no significant difference in the risk of seroma between the open repair and laparoscopic repair groups (OR 0.67, 95% CI 0.19–2.32, P = 0.53). A high level of heterogeneity among the studies existed (I 2 = 80%, P < 0.0001).
Recurrence
Recurrence was reported in nine studies, [12,13,14, 16,17,18,19,20,21] enrolling 1897 patients (Fig. 3). The risk of recurrence was higher in open repair group compared to laparoscopic repair group (OR 4.06, 95% CI 1.54–10.71, P = 0.005). A low level of heterogeneity among the studies existed (I 2 = 42%, P = 0.10).
Length of stay
Length of stay was reported in eight studies, [12,13,14,15,16, 19,20,21] enrolling 15,488 patients (Fig. 3). The length of stay was longer in open repair group compared to laparoscopic repair group (MD 26.85, 95% CI 8.15–45.55, P = 0.005). A high level of heterogeneity among the studies existed (I 2 = 99%, P < 0.0001).
Operative time
Operative time was reported in seven studies, [12, 14,15,16, 19,20,21] enrolling 15,151 patients (Fig. 3). The operative time was shorter in open repair group compared to laparoscopic repair group (MD − 23.07, 95% CI − 36.78 to − 9.35, P = 0.0010). A high level of heterogeneity among the studies existed (I 2 = 99%, P < 0.0001).
The other outcomes (visceral injury, bleeding, incisional hernia, port-site hernia, or mortality) were not reported by the included studies.
Additional analyses
Sensitivity analyses
We conducted additional analyses for the outcomes that were reported by at least four studies. Removing one study at a time did not change the direction of the effect size and the overall heterogeneity for any of the outcomes except wound dehiscence. The use of random effects or fixed effect model did not affect the direction of the effect size in any of the outcomes. Moreover, the direction of the effect size for all of the outcomes remained unchanged when ORs or RDs were calculated. The separate analyses for studies with low or moderate risk of bias did not affect the direction of the effect sizes.
Randomised controlled trials
Three RCTs, [12,13,14] enrolling a total of 419 patients, were included. Compared to laparoscopic repair, open repair was associated with a higher risk of wound infection (OR 4.67, 95% CI 1.55–14.09, P = 0.006), wound dehiscence (OR 19.47, 95% CI 1.12–337.23, P = 0.04), haematoma (OR 21.10, 95% CI 4.99–89.33, P < 0.0001) and seroma (OR 2.69, 95% CI 1.14–6.35, P = 0.02). Open repair was associated with longer length of stay (MD 43.68, 95% CI 2.66–84.70, P = 0.04) and shorter operative time (MD − 20.86, 95% CI − 28.52 to − 13.20, P < 0.00001). There was no significant difference in the risk of recurrence between the two groups (OR 1.52, 95% CI 0.70–3.30, P = 0.29).
Subgroup comparisons
The available data allowed synthesis for the following comparisons: (1) open mesh repair versus laparoscopic mesh repair, and (2) open suture repair versus laparoscopic mesh repair.
Open mesh repair versus laparoscopic mesh repair
Six studies, [12, 13, 18,19,20,21] enrolling 1094 patients, compared open mesh repair with laparoscopic mesh repair. Open mesh repair was associated with a higher risk of wound infection (OR 3.87, 95% CI 1.81–8.27, P = 0.0005), longer length of stay (MD 50.61, 95% CI 24.54–76.68, P = 0.0001) and shorter operative time (MD − 35.03, 95% CI − 36.79 to − 33.27, P < 0.00001). There was no significant difference in the risk of wound dehiscence (RD 0.02, 95% CI − 0.05 to 0.08, P = 0.65), haematoma (RD 0.04, 95% CI − 0.13, 0.21, P = 0.64), seroma (OR 1.56, 95% CI 0.45–5.44, P = 0.48) and recurrence (OR 2.35, 95% CI 0.82–6.72, P = 0.11) between the open mesh repair and laparoscopic mesh repair groups.
Open suture repair versus laparoscopic mesh repair
Five studies, [14, 18,19,20,21] enrolling 689 patients, compared open suture repair with laparoscopic mesh repair. Open suture repair was associated with a higher risk of wound infection (OR 4.38, 95% CI 1.69–11.35, P = 0.002) and recurrence (OR 20.64, 95% CI 6.86–62.14, P < 0.00001) and shorter operative time (MD − 30.83, 95% CI − 58.77 to − 2.89, P = 0.03). There was no significant difference in the risk of wound dehiscence (OR 4.60, 95% CI 0.76–27.82, P = 0.10), haematoma (OR 3.83, 95% CI 0.61–23.85, P = 0.15), seroma (OR 0.48, 95% CI 0.09–2.69, P = 0.40) and length of stay (MD − 3.16, 95% CI − 11.19 to 4.87, P = 0.44) between the open suture repair and laparoscopic mesh repair groups.
Discussion
We performed a systematic review of the literature and meta-analysis of reported outcomes to compare laparoscopic repair with open repair of umbilical and paraumbilical hernias. We included three RCTs [12,13,14] and seven retrospective cohort studies, [15,16,17,18,19,20,21] enrolling a total of 16,549 patients. The results of our analyses suggest that laparoscopic repair is associated with lower risk of wound infection, wound dehiscence and recurrence, shorter hospital stay and longer operative time compared to open repair. We did not find any difference in the risk of haematoma and seroma between the two groups. The between-study heterogeneity was low for wound infection, wound dehiscence and recurrence but a high level of between-study heterogeneity existed for the other outcomes. The directions of the effect sizes remained consistent throughout our sensitivity analyses for all of the outcomes except for wound dehiscence, making our results statistically robust for the rest of the outcomes included in sensitivity analyses. Our results remained consistent when randomised trials were analysed separately.
Our study is the first systematic review in the current literature comparing laparoscopic and open repair of umbilical and paraumbilical hernias. Zhang et al. [22] compared the laparoscopic and open repairs of incisional and ventral hernias in a systematic review of 11 studies, enrolling 1003 patients. Al Chalabi et al. [23] compared the laparoscopic and open repairs of incisional hernias in a systematic review of five studies, enrolling 611 patients. Consistent with our findings, Zhang et al. [22] and Al Chalabi et al. [23] found a lower risk of wound infection in laparoscopic repair. The laparoscopic approach is associated with lesser surgical trauma, uses smaller incisions than open surgery and eliminates the need for tissue undermining and wound drainage [24, 25]. Moreover, less pronounced proinflammatory response caused by laparoscopic surgery results in a better preservation of the systemic immune function postoperatively [26, 27]. All of these may explain the lower risk of wound infection associated with laparoscopic repair.
The laparoscopic repair of umbilical and paraumbilical hernias was associated with shorter length of stay but longer operation time in this study. Multiple additional steps required for laparoscopic procedures such as positioning, set-up of laparoscopic equipment, insufflation of the abdominal cavity and placement of multiple ports prior to proceeding with repair may explain the longer operative time compared to open repair [21]. Most patients who underwent surgery for umbilical hernia repair, whether open or laparoscopic, are discharged on the same day. Therefore, although we found shorter length of stay associated with laparoscopic repair, this difference may not be significant in clinical settings as long as most repairs are done as day case surgery.
The recurrence rate was lower in laparoscopic repair group in our analysis. This may be due to tension-free nature of the repair with a generous mesh overlap of the hernia defect but perhaps more importantly the identification of clinically undiagnosed satellite defects that can be repaired at the same time. A low level of between-study heterogeneity for this outcome provides a relatively robust basis for definite conclusions for recurrence rate.
The laparoscopic repair of umbilical or paraumbilical hernia is associated with some disadvantages. It is associated with the risk of intestinal or bladder injury intraoperatively [28]. Moreover, adhesions to the abdominal scar can potentially increase the risk of bowel injury around the neck of the hernia during dissection [29]. An incidental enterotomy may occur during initial trocar placement or may result from adhesiolysis, requiring endoscopic suturing, conversion to open surgery or sometimes postponing the mesh repair of the ventral hernia in case of spillage of bowel contents [30]. The hernia sac is usually retained in place in the laparoscopic approach; this can potentially increase the risk of postoperative seroma formation. Furthermore, in emergency situations laparoscopic repair may be associated with some disadvantages including need for high level of concentration and meticulous manoeuvres such as inserting and withdrawing the instrument in and out of the working trocars, working in limited operating space with distended bowel loops, longer operative time, and hesitation in placing a large underlay synthetic mesh inside the peritoneal cavity in acute abdominal condition with distended bowel loops.
Unfortunately, none of the included studies in this review reported cost-effectiveness as outcome; therefore, we cannot make definitive conclusions about this outcome.
The reported outcomes of our review should be viewed and interpreted in the context of inherent limitations. Most of the included studies in this review were non-randomised observational studies which are inevitably subject to selection bias. The available data was insufficient to make conclusions about other outcomes such as visceral injury, bleeding, incisional hernia, port-site hernia, and mortality. Some of the included studies in our review included few participants, and therefore occurrence of few outcome events in these studies might have led to imprecise effects estimates. This may subject our results to type 2 error due to not achieving the information size required to reject the null hypothesis. The median follow-up period was 24 months in this study; it can be argued that this is not sufficient for some outcomes such as recurrence to occur, subjecting our results to potential type 2 error again. Lack of data about hernia defect size and anatomical characteristics of the included population in the included studies did not allow assessing the outcomes based on these parameters. Therefore, different defect sizes and anatomical characteristics of the included population can potentially subject our results to confounding bias. Moreover, we could not control effect of different laparoscopic techniques or surgeon experience on the outcomes, subjecting our results to potential bias. A high level of between-study heterogeneity existed for outcomes such as haematoma, seroma, length of stay and operative time, affecting the robustness of our results for these outcomes. The number of eligible studies for this review was less than 10, not allowing for formal assessment of publication bias as planned in our protocol; therefore, the reporting bias cannot be excluded in this study.
Conclusions
The best available evidence (randomised and non-randomised studies) suggests that laparoscopic repair of umbilical or paraumbilical hernia may be associated with a lower risk of wound infection, wound dehiscence and recurrence rate, shorter length of stay but longer operative time. Results from a limited number of RCTs showed that laparoscopic repair is associated with lower risks of wound infection, wound dehiscence, haematoma and seroma; shorter length of stay and longer operative time but showed no difference in recurrence rates. The quality of the best available evidence is moderate and selection bias is the major concern due to non-randomised design in most of the available studies. Therefore, considering the level of available evidence, the most reliable approach for repair of umbilical or paraumbilical hernia should be based on surgeon’s experience, clinical setting, patient’s age and size, hernia defect size and anatomical characteristics. Therefore, high quality RCTs, which are adequately powered, are required to provide more robust basis for definite conclusions. Future studies should compare the outcomes of each technique in different hernia defect sizes (small versus large) and different clinical settings (emergency versus elective). Moreover, future studies should value outcomes such as severity of postoperative pain, time to return to daily activities, quality of life and cost-effectiveness of either technique.
References
Misra MC, Bansal VK, Kulkarni MP, Pawar DK (2006) Comparison of laparoscopic and open repair of incisional and primary ventral hernia: results of a prospective randomized study. Surg Endosc 20(12):1839–1845
Mayo WJ (1901) An operation for the radical cure of umbilical hernia. Ann Surg 34:276–280
Kulaçoğlu H (2015) Current options in umbilical hernia repair in adult patients. Ulus Cerrahi Derg 31(3):157–161
Gray SH, Hawn MT, Itani KMF (2008) Surgical progress in inguinal and ventral incisional hernia repair. Surg Clin N Am 88:17–26
Arroyo A, Garcia P, Perez F, Andreu J, Candela F, Calpena R (2001) Randomized clinical trial comparing suture and mesh repair of umbilical hernia in adults. Br J Surg 88:1321–1323
McGreevy JM, Goodney PP, Birkmeyer CM, Finlayson SR, Laycock WS, Birkmeyer JD (2003) A prospective study comparing the complication rates between laparoscopic and open ventral hernia repairs. Surg Endosc 17(11):1778–1780
Jaqab RB (2008) Laparoscopic ventral hernia repair: a new method for fixation of the mesh with sutures. Surg Laparosc Endosc Percutan Tech 18:277–279
Muqim R, Jan QE, Zarin M, Khan MT, Iqbal J, Khan IN et al (2008) Laparoscopic repair of ventral hernia, an early experience at Khyber teaching hospital, Peshawar. World J Laparosc Surg 1:35–38
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 15 May 2014
Higgins JP, Altman DG, editors. Chapter 8: Assessing risk of bias in included studies. In: Higgins JP, Green S, editors. Cochrane handbook for systematic reviews of interventions. Version 5.0.1 (updated September 2008). http://hiv.cochrane.org/sites/hiv.cochrane.org/files/uploads/Ch08_Bias.pdf. Accessed 15 May 2016
Purushotham B, Madhu S (2015) Comparative study between laparoscopic and open repair of umbilical and para umbilical hernia. Int Surg J 2(2):204–213
Malik AM (2015) Laparoscopic versus open repair of paraumbilical hernia. Is it a good alternative? J Pak Med Assoc 65(8):865–868
Othman IH, Metwally YH, Bakr IS, Amer YA, Gaber MB, Elgohary SA (2012) Comparative study between laparoscopic and open repair of paraumbilical hernia. J Egypt Soc Parasitol 42(1):175–182
Cassie S, Okrainec A, Saleh F, Quereshy FS, Jackson TD (2014) Laparoscopic versus open elective repair of primary umbilical hernias: short-term outcomes from the American College of Surgeons National Surgery Quality Improvement Program. Surg Endosc 28(3):741–746
Colon MJ, Kitamura R, Telem DA, Nguyen S, Divino CM (2013) Laparoscopic umbilical hernia repair is the preferred approach in obese patients. Am J Surg 205(2):231–236
Shaikh I, Willder JM, Kumar S (2013) Same day discharge, surgical training and early complications after open and laparoscopic repair of primary paraumbilical hernia. Hernia 17(4):505–509
Solomon TA, Wignesvaran P, Chaudry MA, Tutton MG (2010) A retrospective audit comparing outcomes of open versus laparoscopic repair of umbilical/paraumbilical herniae. Surg Endosc 24(12):3109–3112
Lau H, Patil NG (2003) Umbilical hernia in adults. Surg Endosc 17(12):2016–2020
Gonzalez R, Mason E, Duncan T, Wilson R, Ramshaw BJ (2003) Laparoscopic versus open umbilical hernia repair. JSLS. 7(4):323–328
Wright BE, Beckerman J, Cohen M, Cumming JK, Rodriguez JL (2002) Is laparoscopic umbilical hernia repair with mesh a reasonable alternative to conventional repair? Am J Surg 184(6):505–508 (discussion 508-509)
Zhang Y, Zhou H, Chai Y, Cao C, Jin K, Hu Z (2014) Laparoscopic versus open incisional and ventral hernia repair: a systematic review and meta-analysis. World J Surg 38(9):2233–2240
Al Chalabi H, Larkin J, Mehigan B, McCormick P (2015) A systematic review of laparoscopic versus open abdominal incisional hernia repair, with meta-analysis of randomized controlled trials. Int J Surg 20:65–74
Marusch F, Gastinger I, Schneider C et al (2001) Importance of conversion for results obtained with laparoscopic colorectal surgery. Dis Colon Rectum 44:207–214
Belizon A, Sardinha CT, Sher ME (2006) Converted laparoscopic colectomy: what are the consequences? Surg Endosc 20:947–951
Gupta A, Watson DI (2001) Effect of laparoscopy on immune function. Br J Surg 88:1296–1306
Wichman MW, Hüttl TP, Winter H et al (2005) Immunological effects of laparoscopic vs open colorectal surgery. Arch Surg 140:692–697
Heniford BT, Park A, Ramshaw BJ, Voeller G (2003) Laparoscopic repair of ventral hernias. Nine years’ experience with 850 consecutive hernias. Ann Surg 238:391–400
Rudmik LR, Schieman C, Dixon E (2006) Laparoscopic incisional hernia repair: a review of the literature. Hernia 10:110–119
Perrone JM, Soper NJ, Eagon JC et al (2005) Perioperative outcomes and complications of laparoscopic ventral hernia repair. Surgery 138:708–715 (discussion 715–716)
Author information
Authors and Affiliations
Contributions
Shahab H and Shahin H have equally contributed to this paper and a joined first authorship is proposed. Conception and design: Shahab H, Shahin H. Literature search and study selection: AS, Shahab H, Shahin H. Data collection: AS, Shahab H, Shahin H. Analysis and interpretation: Shahab H, Shahin H. Writing the article: Shahab H, Shahin H. Critical revision of the article: Shahab H, Shahin H, AS, AK, DS, LJ. Final approval of the article: Shahab H, Shahin H, AS, AK, DS, LJ. Statistical analysis: Shahab H, Shahin H.
Corresponding author
Ethics declarations
Conflict of interest
Shahab H declares no conflict of interest. Shahin H declares no conflict of interest. AS declares no conflict of interest. AK declares no conflict of interest. DS declares no conflict of interest. LJ declares no conflict of interest.
Ethical approval
Not required.
Human and animal rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
This article does not include patients, and therefore informed consent was not applicable.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Appendix
Rights and permissions
About this article
Cite this article
Hajibandeh, S., Hajibandeh, S., Sreh, A. et al. Laparoscopic versus open umbilical or paraumbilical hernia repair: a systematic review and meta-analysis. Hernia 21, 905–916 (2017). https://doi.org/10.1007/s10029-017-1683-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-017-1683-y