Abstract
Context
The utility of laparoscopic repair in the treatment of incisional hernia repair is still contentious.
Objectives
The aim was to conduct a meta-analysis of RCTs investigating the surgical and postsurgical outcomes of elective incisional hernia by open versus laparoscopic method.
Data sources
A search of PubMed, Medline, Embase, Science Citation Index, Current Contents, and the Cochrane Central Register of Controlled Trials published between January 1993 and September 2013 was performed using medical subject headings (MESH) “hernia,” “incisional,” “abdominal,” “randomized/randomised controlled trial,” “abdominal wall hernia,” “laparoscopic repair,” “open repair”, “human” and “English”.
Study eligibility criteria, participants and interventions
Prospective RCTs comparing surgical treatment of only incisional hernia (and not primary ventral hernias) using open and laparoscopic methods were selected.
Study appraisal and synthesis methods
Data extraction and critical appraisal were carried out independently by two authors (AA and MAM) using predefined data fields. The outcome variables analyzed included (a) hernia diameter; (b) operative time; (c) length of hospital stay; (d) overall complication rate; (e) bowel complications; (f) reoperation; (g) wound infection; (h) wound hematoma or seroma; (i) time to oral intake; (j) back to work; (k) recurrence rate; and (l) postoperative neuralgia. These outcomes were unanimously decided to be important since they influence the practical and surgical approach towards hernia management within hospitals and institutions. The quality of RCTs was assessed using Jadad’s scoring system. Random effects model was used to calculate the effect size of both binary and continuous data. Heterogeneity amongst the outcome variables of these trials was determined by the Cochran Q statistic and I 2 index. The meta-analysis was prepared in accordance with PRISMA guidelines.
Results
Sufficient data were available for the analysis of twelve clinically relevant outcomes. Statistically significant reduction in bowel complications was noted with open surgery compared to the laparoscopic repair in five studies (OR 2.56, 95 % CI 1.15, 5.72, p = 0.02). Comparable effects were noted for other variables which include hernia diameter (SMD −0.27, 95 % CI −0.77, 0.23, p = 0.29), operative time (SMD −0.08, 95 % CI −4.46, 4.30, p = 0.97), overall complications (OR −1.07, 95 % CI −0.33, 3.42, p = 0.91), wound infection (OR 0.49, 95 % CI 0.09, 2.67, p = 0.41), wound hematoma or seroma (OR 1.54, 95 % CI 0.58, 4.09, p = 0.38), reoperation rate (OR −0.32, 95 % CI 0.07, 1.43, p = 0.14), time to oral intake (SMD −0.16, 95 % CI −1.97, 2.28, p = 0.89), length of hospital stay (SMD −0.83, 95 % CI −2.22, 0.56, p = 0.24), back to work (SMD −3.14, 95 % CI −8.92, 2.64, p = 0.29), recurrence rate (OR 1.41, 95 % CI 0.81, 2.46, p = 0.23), and postoperative neuralgia (OR 0.48, 95 % CI 0.16, 1.46, p = 0.20).
Conclusions
On the basis of our meta-analysis, we conclude that laparoscopic and open repair of incisional hernia is comparable. A larger randomized controlled multicenter trial with strict inclusion and exclusion criteria and standardized techniques for both repairs is required to demonstrate the superiority of one technique over the other.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Generally every surgical procedure that requires access through the abdominal wall, no matter how small, carries a risk of development of incisional hernia. Approximately four million laparotomies are performed in the United States annually, 2–30 % of them resulting in incisional hernia [1]. Between 100,000 and 150,000 ventral incisional hernia repairs are performed annually in the United States [2]. Incisional hernias are mostly related to failure of the fascia to heal and involve technical and biological factors. Approximately 50 % of all incisional hernias develop or present within the first 2 years following surgery, and 74 % occur within 3 years. Incisional hernias may cause pain, increase in size over time, and may also result in severe complications such as bowel incarceration and strangulation.
A vast majority of open surgical repair of incisional hernias are achieved using a prosthetic mesh. Even though it is a tensionless repair, it is still associated with early or late complications such as mesh infection, chronic pain, seroma, hematoma, mesh shrinkage, etc. [3]. The recurrence rate following mesh repair is still as high as approximately 32 % over a 10-year follow-up period [4].
In order to improve upon the recurrence rate of open mesh repair of incisional hernia, LeBlanc, in 1993, reported the first case of laparoscopic incisional hernia repair using a synthetic mesh [5, 6]. This technique supposedly reduces the surgical insult, allowing better visualization of the defect, reducing the risk of bleeding, infectious complications, seroma formation and recurrence rate. Since the introduction of this technique, a number of randomized control trials (RCTs) comparing laparoscopic and open methods have been published analyzing various aspects of these approaches. The objective of this meta-analysis was to determine the clinical outcomes, safety and effectiveness of laparoscopic repair compared with open repair for elective surgical treatment of incisional hernia only, with the exclusion of RCTs which also includes the primary abdominal wall hernia repair.
Materials and methods
Search strategy and data collection
RCTs were identified by conducting comprehensive search of electronic databases, PubMed, Medline, Embase, Science Citation Index, Current Contents and the Cochrane Central Register of Controlled Trials published between January 1993 and September 2013 using medical subject headings (MESH); “hernia,” “incisional,” “abdominal,” “randomized/randomised controlled trial,” “abdominal wall hernia,” “laparoscopic repair,” and “open repair”; “Human”; and “English”. We further searched the reference lists of all included primary studies and existing meta-analysis by hand for additional citations. Data extraction, critical appraisal and quality assessment of the identified studies were analytically done by two authors (AA, MAM). The authors were not blinded to the source of the document or authorship for the purpose of data extraction. Standardized data extraction forms [7] were used by authors to independently and blindly summarize all the data available in the RCTs meeting the inclusion criteria. The data obtained were entered directly into MS Excel. Double data entry method was used to avoid errors in data extraction. The data were compared and discrepancies were addressed with discussion until consensus was achieved. The analysis was prepared in accordance with the preferred reporting of systematic reviews and meta-analyses (PRISMA) statement [8]. Random effect model was used for analysis of all the variables.
Inclusion and exclusion criteria
Two reviewers (AA and MAM) individually considered the abstracts of the identified articles for prospective eligibility. We retrieved all the eligible full text articles, which were later reviewed in detail and checked against our inclusion and exclusion criteria. Appropriateness was determined by these independent reviewers and by discussion in case of inconsistency. The RCTs must have reported on at least one clinically relevant outcome pertaining to the intraoperative and postoperative period. Outcomes assessed were those considered to exert influence over practical aspects of surgical practice. All studies reporting on outcomes of this nature were considered and final analyses were run on outcome variables where numbers were sufficient to allow statistical analysis. Additional exclusion criteria included studies that investigated the effect of open versus laparoscopic repair in a mixture of primary and incisional hernia repair and duplicate publications.
Type of participants
Only adult (>18 years) patients requiring elective surgical intervention purely for the repair of incisional hernia were the target population for this meta-analysis.
Types of intervention
Two different elective surgical approaches for the management of purely incisional hernia (excluding primary ventral hernia), namely laparoscopic and conventional open surgical repair (suture or mesh), were being assessed for the differences in short and long-term surgical outcomes.
Types of outcome measures analyzed
The 12 outcome variables analyzed included (a) hernia diameter; (b) operative time; (c) length of hospital stay; (d) overall complication rate; (e) bowel complications; (f) reoperation; (g) wound infection; (h) wound hematoma or seroma; (i) time to oral intake; (j) back to work; (k) recurrence rate; and (l) postoperative neuralgia. These outcomes were unanimously decided to be important since they influence the practical and surgical approach towards hernia management within hospitals and institutions.
Methodological quality
We used the Jadad scoring system to evaluate the methodological quality of the identified RCT’s [9, 10]. Each study was allocated a score from zero to five, zero being the lowest quality and five being the highest quality based on reporting of randomization, blinding, and withdrawals reported during the study period.
Statistical analysis and risk of bias across studies
Meta-analyses were performed using odds ratios (ORs) for binary outcome and standardized mean differences (SMDs) for continuous outcome measures. The slightly amended estimator of OR was used to avoid the computation of reciprocal of zeros among observed values in the calculation of the original OR [11]. Random effects model based on the inverse variance weighted method approach was used to combine the data [12]. Heterogeneity among studies was assessed using the Q statistic proposed by Cochran and I 2 index introduced by Higgins and Thompson [12–16]. If the observed value of Q was greater than the associated x 2 critical value at a given significant level, in this case 0.05, we conclude the presence of statistically significance between-studies variation. In order to pool continuous data, mean and standard deviation of each study is required. However, some of the published clinical trials did not report the mean and standard deviation, but rather reported the size of the trial, the median and range. Using these available statistics, estimates of the mean and standard deviation were obtained using formulas proposed by Hozo et al. [17]. Funnel plots were created to determine the presence of publication bias in the present meta-analysis. Both total sample size and precision (reciprocal of standard error) were plotted against the treatment effects (OR for dichotomous variables and SMD for continuous variables) [12, 18–20]. All estimates were obtained using a computer program written in R [21]. All plots were obtained using the metafor-package [22]. In the case of tests of hypotheses, the paper reports p values for different statistical tests on the study variables. In general, the effect is considered to be statistically significant if the p value is small. If one uses a 5 % significance level then the effect is significant only if the associated p value is ≤5 %.
Results
Included studies
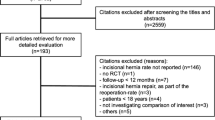
Cross-searching of electronic databases yielded a total of 239 abstracts and hand searches of reference lists provided a further two citations. After exclusion of 167 duplicate/non-relevant citations, 74 unique citations of potential relevance were retrieved for review. The process by which these citations were excluded is described in Fig. 1. No further potentially relevant unpublished studies were identified through a citation search of a previous published meta-analysis on this subject. The six studies [23–28] that met the inclusion criteria are detailed in Table 1. They collectively demonstrated moderate methodological quality based on Jadad score with an average score of 2.7 (out of 5), with a range of 2–3. Four studies reported on withdrawals [25–28], five described an appropriate method of randomization [24–28], whereas none of the trials reported on blinding (Table 1).
Excluded studies
Seven studies [29–35] were excluded from our meta-analysis although they were included in the previous meta-analyses. These studies included not just incisional hernia repair but also primary ventral hernia repair. We strongly feel that the pathology behind the causation of primary ventral hernias is entirely different from that of incisional hernias. Also the risk of complications such as iatrogenic enterotomies, conversion to open surgery, bleeding, etc. is much higher with incisional hernia due to the complexity of surgery compared to primary ventral hernia repair in a virgin abdomen. Analyzing these two different types of hernias as a “single entity” will give misleading and erroneous results in terms of complications, operating time, recurrence rate and reoperation to name but a few variables for both open and the laparoscopic groups.
Clinical outcomes
Statistically significant reductions in bowel complications were noted with open surgery compared to the laparoscopic repair based on five studies [23, 25–28] (OR 2.56, 95 % CI 1.15, 5.72, p = 0.02) (Fig. 2). Comparable effects were noted for other variables which include hernia diameter (SMD −0.27, 95 % CI −0.77, 0.23, p = 0.29) (Fig. 3), operative time (SMD −0.08, 95 % CI −4.46, 4.30, p = 0.97) (Fig. 4), overall complications (OR −1.07, 95 % CI −0.33, 3.42, p = 0.91) (Fig. 5), wound infection (OR 0.49, 95 % CI 0.09, 2.67, p = 0.41) (Fig. 6), wound hematoma or seroma (OR 1.54, 95 % CI 0.58, 4.09, p = 0.38) (Fig. 7), reoperation rate (OR 0.32, 95 % CI 0.07, 1.43, p = 0.14) (Fig. 8), time to oral intake (SMD −0.16, 95 % CI −1.97, 2.28, p = 0.89) (Fig. 9), length of hospital stay (SMD −0.83, 95 % CI −2.22, 0.56, p = 0.24) (Fig. 10), back to work (SMD −3.14, 95 % CI −8.92, 2.64, p = 0.29) (Fig. 11), recurrence rate (OR 1.41, 95 % CI 0.81, 2.46, p = 0.23) (Fig. 12), and postoperative neuralgia (OR 0.48, 95 % CI 0.16, 1.46, p = 0.20) (Fig. 13).
Forest plot of bowel complications (Forest plots: Forest plot draws the 95 % confidence intervals for the odds ratios or weighted standardized mean differences as horizontal lines. Confidence intervals show arrows when they exceed specified limits. In the forest plot, squares indicate the estimated treatment effects with the size of the squares representing the weight attributed to each study. The pooled estimated OR or SMD is obtained by combining all the ORs or SMDs of the studies using the inverse variance weighted method, represented by the diamond and the width of the diamond depicts the 95 % confidence interval)
Heterogeneity
The Q test and I 2 Index are commonly used methods in meta-analysis for detecting heterogeneity. An I 2 index equaling 0 % suggests no between-study variability occurring within the analysis and that all variations observed are result of sampling error. Conversely, the degree to which an I 2 index approaches 100 % suggests the extent to which the observed variation can be attributed to between-study variability rather than an exclusive sampling error. In general there was a high degree of heterogeneity detected for most of the outcomes in the included studies except for bowel complications, recurrence rate, reoperation and neuralgia (Table 2).
Publication bias
Most of the funnel plots demonstrate asymmetry and thus suggest the presence of publication bias for a majority of outcomes (Fig. 14). However, the number of studies included for all these variables were too few to sensitively detect publication bias.
Discussion
In the modern surgical era, laparoscopic repair has increasingly been utilized in the management of incisional hernia. First described by LeBlank [5, 6], the technique has evolved and is now replacing open repairs where possible. Large multi-centered series have described outstanding outcomes with laparoscopic techniques citing less complications and recurrence rates of less than 10 % [36–40].
There have been several meta-analyses comparing the outcomes of laparoscopic and open repairs but all of them have erroneously included not just the incisional hernia but also the primary ventral hernia repair as well [41–43]. Our meta-analysis focuses on RCTs comparing the outcome of laparoscopic versus open hernia repair for incisional hernia only and excluding primary ventral hernia repair. Our search revealed only six RCTs [23–28] which focused exclusively on the outcomes of the two procedures purely for incisional hernia.
There was no difference in the demographics of the patient population included in our analysis. The mean patients’ age in the laparoscopic and open repair groups displayed little variation. The BMI of all the patients in these six studies [23–28] fell within a median range of 28–31.2, indicating that most of these patients were clinically obese or overweight.
We observed that laparoscopic technique was used to repair larger hernia diameters at times (Fig. 3). There could be a number of explanations for this discrepancy. First of all the laparoscopic technique quite often detects more than one hernia defects whether large or small with ease. Second, it is entirely possible that by inflating the abdomen in the laparoscopic technique, the size of these defects may become exaggerated. Therefore, by measuring the size of all visible defects during laparoscopy, small or large, and documenting it as a combined defect, large-diameter hernias are reported during laparoscopic repair. Whereas an open repair in a non-distended abdomen only measures the largest defect which the surgeon can feel at the time of dissecting the tissue and possibly missing the adjacent smaller defects. Itani et al. [26] and Rogmark et al. [28] studies showed markedly large hernias were repaired using laparoscopic techniques compared to their open counterpart.
The operative time taken by laparoscopic as well as the open repair was comparable in our meta-analysis based on five [24–28] out of six studies. No information on the time delay due to complications during the procedure was available.
For our analysis, we considered enterotomies, serosal tears and postoperative small bowel obstruction as bowel complications (during intra- and postoperative periods). Bowel complications in a variety of forms were reported by all the six RCTs [23–28]. Pooling of this data revealed a statistically significant increase in bowel complications in the laparoscopic group. Unrecognized enterotomies, associated with blind first trocar entry can potentially have a significant mortality rate in the laparoscopic group [44–47]. The issue of bowel injury has been addressed in detail by Forbes et al. [42]. The severity of bowel injury is determined by the type of intestine injured, i.e. small or large, the time delay between the occurrence, detection and treatment, and the amount of soiling that occurs [48, 49]. Unrecognized enterotomies or recognized bowel injuries lead to conversion to open repair as discussed in Itani et al. [26] and Asencio et al. [25]. Rogmark et al. [27] also reported bowel injuries but this did not directly lead to conversion.
The overall complication rate was comparable in the two groups based on six RCTs [23–28]. However, surgical site infections, hematomas, seromas and superficial wound infections, etc. were noted more often in the open group than the laparoscopic group, which is completely in line with other laparoscopic procedures like cholecystectomy and appendectomy [50]. Nonetheless when all these variables (i.e. wound infection, wound hematoma and seroma) were analyzed separately, the results were once again comparable for both groups. We feel that since there are no set criteria for the measurement of seroma formation, and that it can be interpreted differently as in most of the RCTs, it is imperative to prevent and differentiate between asymptomatic and clinically noteworthy seromas. Olmi et al. [23] reported that subcutaneous drain placement was required by 97.6 % of the open group patients, as was also highlighted in all the other trials [24–28]. However, very few drains were used in the laparoscopic group. Drains being a potential source of infection may be the cause of increased incidence of wound or mesh infection in the open group [34]. Olmi et al. [23], Rogemark et al. [28] and Itani et al. [26] all showed significantly higher wound infection rates for open repairs compared to laparoscopic repairs. Wound infection rates were comparable in two groups in Eker et al. [27] study whereas Asencio et al. [25] noticed no wound infection in either group.
Reoperation rate was reported by four [23–25, 28] out of six studies. Analysis showed comparable outcomes for both groups. Rogemark et al. [28] RCTs showed the largest number of reoperations i.e. seven reoperations in six patients for various reasons such as small bowel obstruction, postoperative bleeding/hematoma, necrosis of the umbilicus, neuralgia and deep wound infections.
The time taken to oral intake was statistically insignificant for both groups based on only two studies [24, 25]. As the number of patients analyzed for this variable is so small, any meaningful conclusion is not possible.
Only two studies [23, 24] out of six RCTs documented shorter length of hospital stay following laparoscopic repair compared to the open group. As documented by several other studies [30, 37, 41, 51], we concluded that since there is a need for intensive soft tissue dissection and raising multiple subcutaneous skin flaps in open technique, this may lead to prolonged hospital stay and complications in this group. The economic factor associated with a shorter postoperative hospital stay can be a potential advantage of the laparoscopic procedure as discussed by Olmi et al. [23] and Earle et al. [52]. However, four out of six RCTs [25–28] found comparable length of hospital stay for both these procedures.
Olmi et al. [23] and Itani et al. [26] reported that patients in the laparoscopic group took less time to recover and went back to work quicker. Comparable findings were reported by Carbajo et al. [30]. Rogmark et al. [28] on the other hand reported time taken to full recovery, instead of time taken to return to work. SF-36 subscales favored the laparoscopic repair group in this study but one of the limitations pointed out by Rogmark et al. [28] was that the patients were only followed up to 31 days in both groups and not followed until full recovery. For example, at day 31, 59 % of the patients in the laparoscopic group had fully recovered as compared to 38 % in the open group. The authors concluded that the laparoscopic group recovered comparatively faster, as also reflected by our results. Ascenio et al. [25] and Itani et al. [26] used the EQ5D tariffs [53] and MOS SF-36 [54] scores, respectively, for the two groups during follow-up. The authors concluded that the difference between the scores for the two groups was statistically insignificant. Similarly, Pring et al. [34] failed to show any difference in time taken to return to work in both laparoscopic and open groups. We concluded that these results might have been prejudiced by the partiality of the care provider or the outcome evaluator. In our meta-analysis, only two [23, 26] out of six studies reported back to work data which failed to show any difference between the two groups. Unfortunately as the number of patients analyzed for this variable was so small, any meaningful conclusion was not possible.
All six RCTs [23–28] reported the recurrence rate. Pooling of the data revealed no difference between the two groups. The reasons for recurrent hernia were (a) the mesh overlapped the defect by less than 2 cm [23], (b) poor fixation of the mesh; (c) the mesh migrated into the defects [25], (d) surgical site infection with abscess [26] and (e) post-op trocar site hernia [27]. There have been numerous arguments theoretically describing the superiority of laparoscopic repair over open repair. Sauerland et al. [43] propose that as the laparoscopic repair lets the surgeon inspect the whole previous incision, multiple hernias can be repaired simultaneously with a bigger mesh. However, as the laparoscopic repair does not require closure of the hernia orifice, it relies completely on the strength and adequate size of the mesh and its fixation. Still, the data available on the recurrence rate may be erroneous due to short follow-up in all of these RCTs. Furthermore as the number of patients recruited in all the RCTs is very small, the true recurrence rate may be underestimated. Additionally, the completeness and method of the follow-up of these trials may be subjective (e.g. telephone interview, etc), once again providing misleading results.
Several studies [6, 40, 49] use less postoperative pain or neuralgia as strong supporting evidence for laparoscopic technology. Extensive tissue dissection in open repair and transfacial sutures may be responsible for more pain in open repair whereas direct tacking of the mesh on to the peritoneum may be responsible for pain in laparoscopic repair. Liberal use of local anesthesia or infiltration of the same in the abdominal cavity may reduce the incidence of this complication [55]. Our analysis based on two RCTs [23, 28] showed no significant difference in the postoperative neuralgia between laparoscopic and open repair groups. This finding was not in line with other laparoscopic procedures like appendectomy or cholecystectomy where less pain is observed following laparoscopic techniques. Once again a small number of patients analyzed for this variable may be responsible for obscuring the true difference between the two procedures.
Limitations
There are a number of limitations both statistical and clinical in this paper. First, publication bias was detected on the funnel plot analysis for a number of outcomes [56] (Fig. 14). A second possible limitation within this meta-analysis is the presence of heterogeneity detected within several outcomes (Table 2). Although some degree of heterogeneity is inevitable in a medical meta-analysis due to the realities of clinical practice [57], the degree of between-study heterogeneity present may undermine the quality and legitimacy of the results obtained [58]. Third, the exclusion of studies published in languages other than English is another potential limitation to the present work. Next, the small number of studies included in this meta-analysis remains a largely unavoidable limitation of this and many other meta-analyses conducted in surgical fields [59].
Conclusions
We believe that objective assessment is required to evaluate the long-term effectiveness of the two procedures. Recurrence rates should be measured for a lengthier period of time (e.g. 5 and 10 years) and not just for 2 years. More extensive data on cost benefit and cost effective analyses for both open and laparoscopic repair of incisional hernia should be available which is not addressed by any of the RCTs except for Olmi et al. [23]. Also, larger RCTs recruiting greater numbers of patients with strict inclusion and exclusion criteria and standardized techniques are crucial for meaningful comparison, effectiveness of the procedures and accuracy of results. Finally, more standardized tests should be used to assess the quality of life and chronic pain, so that impartial conclusions can be made regarding the superiority of one procedure over the other both in short and long term.
References
Rutkow IM (2003) Demographic and socioeconomic aspects of hernia repair in the United States in 2003. Surg Clin North Am 5:1045–1051
Read RC, Yoder G (1989) Recent trends in the management of incisional herniation. Arch Surg 124:485–488
Tsereteli Z, Pryor BA, Heniford BT, Park A, Voeller G, Ramshaw BJ (2008) Laparoscopic ventral hernia repair (LVHR) in morbidly obese patients. Hernia 12:233–238
Burger JW, Luijendijk RW, Hop WC, Halm JA, Verdaasdonk EG, Jeekel J (2004) Long-term follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernia. Ann Surg 240:578–585
LeBlanc KA, Booth WV (1993) Laparoscopic repair of incisional abdominal hernias using expanded polytetrafluoroethylene: preliminary findings. Laparosc Endosc 3:39–41
LeBlanc KA, Whitaker JM, Bellnager DE, Rhynes VK (2003) Laparoscopic incisional and ventral hernioplasty: lessons learned from 200 patients. Hernia 7:118–124
Moher D, Cook DJ, Eastwood S (1999) Improving the quality of reports of meta-analyses of randomized controlled trials: the QUOROM statement. Quality of reporting of meta-analyses. Lancet 354:1896–1900
Moher D, Liberati A, Tetzlaff J, The PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analysis: the PRISMA statement. PLoS Med 6:e1000097
Jadad AR, Moore RA, Carroll D (1996) Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 17:1–12
Haynes RB, Sackett DL, Guyatt GH, Tugwell P (2006) Clinical epidemiology: how to do clinical practice research, 3rd edn. Lippincott Williams & Wilkins, Philadelphia
Agresti A (1996) An introduction to categorical data analysis. Wiley, New York
Sutton AJ, Abrams KR, Jones DR, Sheldon TA, Song F (2000) Methods for meta-analysis in medical research. Wiley, London
Cochran WG (1954) The combination of estimates from different experiments. Biometric 10:101–129
Hedges LV, Olkin I (1985) Statistical methods for meta analysis. Academic Press, Orlando
Higgins JPT, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558
Huedo-Medina TB, Sanchez-Meca J, Marin-Martinez F, Botella J (2006) Assessing heterogeneity in meta analysis: Q statistic or I 2 index? Am Psychol Assoc 11:193–206
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range and size of a sample. BMC Med Res Methodol 5:13
Egger M, Smith GD, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634
Tang JL, Liu JLY (2000) Misleading funnel plot detection of bias in meta-analysis. J Clin Epidermiol 53:477–484
Span J, Carière E, Croockewitt S, Smits P (2006) Publication bias, effects on the assessment of rosiglitasone. Br J Clin Pharmacol 62:732
R: a language and environment for statistical computing [Computer Program]. Version 1. Vienna: R foundation for statistical computing, 2008
Viechtbauer W (2010) Conducting meta-analyses in R with the metaphor package. J Stat Softw. http://www.metafor-project.org/doku.php/metafor
Olmi S, Scaini A, Cesana GC, Erba L, Croce E (2007) Laparoscopic versus open incisional hernia repair: an open randomized controlled study. Surg Endosc 21:555–559
Navarra G, Musolino C, De Marco ML, Bartolotta M, Barbera A, Centorrino T (2007) Retromuscular sutured incisional hernia repair: a randomized controlled trial to compare open and laparoscopic approach. Surg Laparosc Endosc Percutan Tech 17:86–90
Asencio F, Aguiló J, Peiró S, Carbó J, Ferri R, Caro F, Ahmad M (2009) Open randomized clinical trial of laparoscopic versus open incisional hernia repair. Surg Endosc 23:1441–1448
Itani KM, Hur K, Kim LT, Anthony T, Berger DH, Reda D, Neumayer L (2010) Comparison of laparoscopic and open repair with mesh for the treatment of ventral incisional hernia: a randomized trial. Arch Surg 145:322–328
Eker HH, Hansson BM, Buunen M, Janssen IM, Pierik RE, Hop WC, Bonjer HJ, Jeekel J, Lange JF (2013) Laparoscopic vs. open incisional hernia repair: a randomized clinical trial. JAMA Surg 13:259–263
Rogmark P, Petersson U, Bringman S, Eklund A, Ezra E, Sevonius D, Smedberg S, Osterberg J, Montgomery A (2013) Short-term outcomes for open and laparoscopic midline incisional hernia repair: a randomized multicenter controlled trial: the ProLOVE (prospective randomized trial on open versus laparoscopic operation of ventral eventrations) trial. Ann Surg 258:37–45
Barbaros U, Asogulu O, Seven R, Erbil Y, Dinccag A, Deveci U, Ozarmagan S, Mercan S (2006) The comparison of laparoscopic and open ventral hernia repairs : a prospective randomized study. Hernia 11:51–56
Carbajo MA, Martín del Olmo JC, Blanco JI, de la Cuesta C, Toledano M, Martín F, Vaquero C, Inglada L (1999) Laparoscopic treatment vs open surgery in the solution of major incisional and abdominal wall hernias with mesh. Surg Endosc 13:250–252
Itani KMF, Neumayer L, Reda D, Kim L, Anthony T (2004) Repair of ventral incisional hernia: the design of a randomized trial to compare open and laparoscopic surgical techniques. Am J Surg 188(6A Suppl):22–29
Misra MC, Bansal VK, Kulkarni MP, Pawar DK (2006) Comparison of laparoscopic and open repair of incisional and primary ventral hernia: results of a prospective randomized study. Surg Endosc 20:1839–1845
Moreno-Egea A, Carrasco L, Girela E, Martín JG, Aguayo JL, Canteras M (2002) Open vs laparoscopic repair of spigelian hernia: a prospective randomized trial. Arch Surg 137:1266–1268
Pring CM, Tran V, O’Rourke N, Martin IJ (2008) Laparoscopic versus open ventral hernia repair: a randomized controlled trial. ANZ J Surg 78:903–906
Poelman M, Apers J, van den Brand H, Cense H, Consten E, Deelder J (2013) The INCH-trial: a multicentre randomized controlled trial comparing the efficacy of conventional open surgery and laparoscopic surgery for incisional hernia repair. BMC Surg 13:8
Ben-Haim M, Kuriansky J, Tal R, Zmora O, Mintz Y, Rosin D, Ayalon A, Shabtai M (2002) Pitfalls and complications with laparoscopic intraperitoneal expanded polytetrafluoroethylene patch repair of postoperative ventral hernia. Surg Endosc 16:785–788
Bencini L, Sanchez LJ (2004) Learning curve for laparoscopic ventral hernia repair. Am J Surg 187:378–382
Ujiki MB, Weinberger J, Varghese TK, Murayama KM, Joehl RJ (2004) One hundred consecutive laparoscopic ventral hernia repairs. Am J Surg 188:593–597
Moreno-Egea A, Torralba JA, Girela E, Corral M, Bento M, Cartagena J, Vicente JP, Aguayo JL, Canteras M (2004) Immediate, early, and late morbidity with laparoscopic ventral hernia repair and tolerance to composite mesh. Surg Laparosc Endosc Percutan Tech 14:130–135
Rosen M, Brody F, Ponsky J, Walsh RM, Rosenblatt S, Duperier F, Fanning A, Siperstein A (2003) Recurrence after laparoscopic ventral hernia repair. Surg Endosc 17:123–128
Goodney PP, Birkmeyer CM, Birkmeyer JD (2002) Short-term outcomes of laparoscopic and open ventral hernia repair: a meta-analysis. Arch Surg 137:1161–1165
Forbes SS, Eskicioglu C, McLeod RS, Okrainec A (2009) Meta-analysis of randomized controlled trials comparing open and laparoscopic ventral and incisional hernia repair with mesh. Br J Surg 96:851–858
Sauerland S, Walgenbach M, Habermalz B, Seiler CM, Miserez M (2011) Laparoscopic versus open surgical techniques for ventral or incisional hernia repair. Cochrane Database of Syst Rev, (3) Art. No.: CD007781. doi:10.1002/14651858.CD007781.pub2
Elieson MJ, LeBlanc KA (2007) Enterotomy and mortality rates of laparoscopic incisional and ventral hernia repair: a review of the literature. JSLS 11:408–414
Toro A, Mannino M, Cappello G, Di Stefano A, Di Carlo I (2012) Comparison of two entry methods for laparoscopic port entry: technical point of view. Diagn and Ther Endosc 2012:305428
LeBlanc KA, Allain BW Jr, Laparoscopic repair of ventral wall abdominal hernia. Updated: Apr 12, 2012. Cited Apr 21, 2014. Available from: http://laparoscopy.blogs.com/prevention_management_3/2010/10/laparoscopic-repair-of-ventral-wall-abdominal-hernia.html
Gillian GK, Geis WP, Grover G (2002) Laparoscopic incisional and ventral hernia repair (LIVH): an evolving outpatient technique. JSLS 6:315–322
Bishoff JT, Allaf ME, Kirkels W, Moore RG, Kavoussi LR, Schroder F (1999) Laparoscopic bowel injury: incidence and clinical presentation. J Urol 161:887–890
Henniford BT, Park A, Ramshaw BJ, Voeller G (2003) Laparoscopic repair of ventral hernias: nine years’ experience with 850 consecutive cases. Ann Surg 238:391–400
Siddiqui K, Khan AF (2006) Comparison of frequency of wound infection: open vs laparoscopic cholecystectomy. J Ayub Med Coll Abbottabad 18:21–24
Mc Greevy JM, Goodney PP, Birkmeyer CM et al (2003) A prospective study comparing the complication rates between laparoscopic and open ventral hernia repairs. Surg Endosc 17:1778–1780
Earle D, Seymour N, Fellinger E, Perez A (2006) Laparoscopic versus open incisional hernia repair: a single-institution analysis of hospital resource utilization for 884 consecutive cases. Surg Endosc 20:71–75
Group EuroQol (1990) EuroQol—A new facility for the measurement of health-related quality of life. Health Policy 16:199–208
Nordlund A, Ekberg K, Kristenson M (2005) EQ-5D in a general population survey—a description of the most commonly reported EQ-5D health states using the SF-36. Qual Life Res 14:1099–1109
Bellows CF, Berger DH (2006) Infiltration of suture sites with local anesthesia for management of pain following laparoscopic ventral hernia repairs: a prospective randomized trial. JSLS 10:345–350
Duval S, Tweedie R (2000) Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 56:455–463
Ioannidis JP, Patsopoulos NA, Evangelou E (2007) Uncertainty in heterogeneity estimates in meta-analyses. BMJ 335:914–916
Ioannidis JP, Lau J (1998) Can quality of clinical trials and meta-analyses be quantified? Lancet 352:590–591
Smith GD, Egger M (1998) Incommunicable knowledge? Interpreting and applying the results of clinical trials and meta-analyses. J Clin Epidemiol 51:289–295
Acknowledgments
We gratefully acknowledge and thank MJB for presenting the abstract of this paper at The Royal Australasian College of Surgeons Annual Scientific Congress, Sands Expo and Convention Centre, Marina Bay Sands, Singapore in 2014. The citation for published abstract is “ANZ Journal of Surgery 2014; 84 (Suppl 1): 67”.
Conflict of interest
AA, FR, MBH, RMY, SK, BM and MAM declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Awaiz, A., Rahman, F., Hossain, M.B. et al. Meta-analysis and systematic review of laparoscopic versus open mesh repair for elective incisional hernia. Hernia 19, 449–463 (2015). https://doi.org/10.1007/s10029-015-1351-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-015-1351-z