Abstract
Purpose
Ventral hernia repair can be performed safely using meshes which are primarily stable upon dynamic intermittent straining (DIS) at recommended overlap. In specific clinical situations, e.g., at bony edges, bridging of the hernial orifice with reduced overlap might be necessary. To gain insight into the durability of various applications, two different meshes with the best tissue grip known so far were assessed.
Methods
The model uses dynamic intermittent strain and comprises the repetition of submaximal impacts delivered via a hydraulically driven plastic containment. Pig tissue simulates a ventral hernia with a standardized 5 cm defect. Commercially available meshes classified as primarily stable at recommended overlap were used to bridge this defect at recommended and reduced overlap.
Results
Using Parietex Progrip®, the peritoneum adds sufficient stability at least to a 2.5 cm overlap. Using Dynamesh Cicat®, four gluing spots with Glubran® are sufficient to stabilize a 3.75 cm overlap. A 2.5 cm overlap is stabilized with eight bonding spots Glubran® and 8 bonding spots combined with four sutures stabilize a 1.25 cm overlap. Here again, an intact peritoneum stabilizes the reconstruction significantly.
Conclusions
Based on a pig tissue model, a total of 23 different conditions were tested. A DIS class A mesh can be easily stabilized bridging a 5 cm hernial orifice with reduced overlap. Caution must be exerted to extend these results to other DIS classes and larger hernial orifices. Further DIS investigations can improve the durability of hernia repair.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The repair of ventral or incisional hernias frequently fails despite advanced mesh augmentation techniques [1]. Mesh augmentation still leaves recurrence rates between 7 and 23% [2–4]. Applying gradually increasing forces, meshes remain structurally intact and in a stable position up to an intraabdominal pressure of 120–150 mmHg [5, 6]. During coughing actions, higher intraabdominal pressures are reached lasting only a few seconds but may occur up to 400 times in the first few hours after surgery and can occur in almost half of our patients [7–9]. A new model delivering dynamic intermittent strain (DIS) up to 250 mmHg repeatedly can assess the influence of coughing actions on the stability of ventral hernia repair [10]. First results demonstrate a rapid deterioration of the ventral hernia repair in the majority of applications tested [11]. Since approximately 4500 different ways of ventral hernia repair exist to date, a classification was proposed distinguishing stable, intermediate and unstable repairs upon DIS testing [11]. DIS class A meshes are defined as being primarily stable bridging a 5 cm orifice with an overlap of 5 cm. In this paper, the two meshes known to exhibit high safety levels (DIS class A meshes) are evaluated at recommended and reduced overlap. Safe bridging techniques are required when the overlap has to be reduced in large hernias, at bony edges, during recurrent repair and in other difficult clinical situations.
Materials and methods
Study design
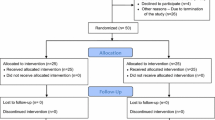
Bridging with reduced overlap was assessed considering DIS class A meshes, the impact of various fixation techniques and an intact or opened peritoneum. Intermittent dynamic strain (DIS) was used to test 23 different mesh repairs of a 5 cm hernial defect in porcine abdominal wall as described before [10, 11, Fig. 1]. The major aim was to find durable repair techniques.
Device mounted with the EPDM membrane in situ being fixed to the pig belly by screws and bolts reliably. The white mark on the left indicates the direction of the linea alba. The dots on the mesh are used to observe the direction and length of migration in relation to the linea alba before dislocation may occur
Dynamic intermittent strain class A meshes are defined as being primarily stable bridging a 5 cm orifice with an overlap of 5 cm. Two different meshes were used which have been tested to withstand 425 dynamic intermittent strains using recommended overlap without fixation [11, parameters of the experimental design are given in Table 1]. In the tests, a 15 cm circular mesh bridged a round defect with a diameter of 5 cm with an overlap varying from 1.25 up to 5 cm in all directions. Thus, transmuscular–transperitoneal defects with a diameter of 5 cm are bridged primarily stable without fixation lifting the mesh in the DIS class A [11]. The one mesh, namely Parietex Progrip® (Covidien Deutschland, Neustadt/Donau, Germany), was tested in an underlay, subperitoneal (IPOM) and a retromuscular, sublay position. In all experiments, the Parietex Progrip® denticles were oriented to point towards the skin side of the preparations (for further information on the mesh, please refer to http://www.medtronic.com/content/dam/covidien/library/us/en/product/hernia-repair/parietex-progrip-self-fixating-mesh-vac-pack.pdf). For comparative analysis, the orientation of the textile without the denticles was identical to that of the textile with denticles according to the instructions given by the manufacturer (for further details of the experimental design see Table 1). For Parietex Progrip® in the sublay position, the peritoneum was left intact in three series for comparison. Sutures were tested for fixation. The other mesh used was Dynamesh Cicat® (FEG Textiltechnik, Aachen, Germany) which was especially designed for the sublay position [12]. The mesh was oriented in accordance with the instructions for use (for further information on the mesh please refer to http://www.dahlhausen.cn/tradepro/cms/site/PDF/dynamesh-hernia_en.pdf). For Dynamesh Cicat®, additional fixation techniques with glue and sutures were investigated. A comprehensive overview of the series conducted is given in Table 1.
Experimental model
Dynamic intermittent strain (DIS, details given in [10]) was examined in a model using pigs tissue. The DIS model uses a hydraulically driven plastic bag contained in an aluminum cylinder and controlled by LabView 2013. In 24 different experiments, Dynamesh Cicat® (FEG Textiltechnik, Aachen, Germany) and Parietex Progrip® and textile (Covidien Deutschland, Neustadt/Donau, Germany) were investigated (Table 1). One type of suture was tested: Surgipro® 4 metric with the GS-21 taper needle (Covidien Deutschland, Neustadt/Donau, Germany). As bonding fixation, Glubran® glue was supplied by Dahlhausen (Köln, Germany). Regarding the number of fixation points, single crowns were tested with evenly distributed 4, 8 and 12 fixation points, spaced 1.3 and 2.5 cm apart from each other, respectively, and more than 1.0 cm inwards from the edges of the meshes. For experiments with only 4 fixations, perpendicular positions were used with the adhesive points placed inwards more than 1.0 cm from the edges. The position of the gluing spots was chosen accordingly. The size of the bonding spots was normalized as 0.8 cm in diameter. For optimal stacking, it was necessary to ensure that the glue was completely dry. According to the manufacturer, this stadium is supposed to be reached within 2 min. However, to ensure that the glue was certainly completely dry, we waited at least three times as long before weight-bearing or transfer to the dynamic testing device was intended.
Commercially available full thickness pig bellies were selected as described earlier [11]. Since the tissue elasticity markedly influences the likelihood of dislocation, medium range pig bellies were selected [11]. Skin and subcutaneous tissue provide irreproducible elasticity and were replaced by an elastic silicone membrane EPDM 90 shore (Kuhn & Kaiser, Erndtebrück, Germany) with a prefabricated central defect corresponding to the tissue orifice. The experimental setup is depicted in Fig. 1. One kind of lubricant, namely commercially available Vaseline® (Sanofi-Aventis, Frankfurt/M., Germany) was generally used as described before [10, 11].
Statistical analysis
Once the model was set in action, the movement of the meshes was observed until the full circumference of the tissue defect was fully exposed or 425 cycles of dynamic intermittent impacts were completed [for details see 10, 11]. The final count of the impacts delivered was noted from the LabView screen. Every fifth experiment was fully analyzed to assess the variability of peak pressures and the reproducibility was generally found to be above 96% (range 180–250 mmHg; mean ± SD: 212 ± 23 mmHg).
The data acquired are typically skewed. Therefore, description was done using non-parametric statistics and box-and-whisker-plots were chosen for depiction. Kruskal–Wallis and Mann–Whitney U tests were used for the analysis of group homogeneity and for exploring significant differences as described before [11]. Since box-and-whisker-plots fail to discriminate small differences, likelihood curves of dislocation resembling survival curves were derived from the original data and are given in addition for clarification.
Results
The influence of reduced overlap on Parietex Progrip®
Parietex Progrip® was found to be a stable repair even without fixation with an overlap of 5 cm bridging a 5 cm hernial orifice. The mesh was tested with gradually reduced overlap bridging a transmural–transperitoneal defect in the sublay position (Tables 1, 2; Fig. 2). The mesh exhibited excellent stability even at an overlap of 3.75 cm. Grip faded at an overlap of 2.5 cm with a 60% likelihood to stay in place beyond the 100th impact. Instability was observed rapidly at an overlap of 1.25 cm with no reconstruction left intact beyond 50 impacts. The difference between the stable and the unstable reconstructions is significant (p = 0.00018).
Top box-and-whisker-plots of the cycles with complete dislocation for Parietex Progrip® lubricated with Vaseline® bridging a 5 cm transmural-transperitoneal defect with an overlap (OL) ranging from 5 to 1.25 cm in the sublay position. Bottom likelihood curves of the same DIS tested hernia repairs (OL 5 cm = 5-Sub, 3.75 cm = 3-Sub, 2.5 cm = 2-Sub, 1.25 cm = 1-Sub)
The influence of position on Parietex Progrip®
In contrast to mesh behavior in the sublay position, meshes started earlier to migrate in response to repeated dynamic movements at reduced overlap bridging a transmural-transperitoneal defect in the underlay-IPOM position (Fig. 3). In general, meshes without fixation stay stable with an overlap of 5 cm. Reducing the overlap to 3.75, a reduced stability is observed with 90% of the reconstructions surviving the 259th impact. Further reducing the overlap led to earlier dislocations (Fig. 3). The difference between the 5 and the 2.5 cm overlap is significant (p = 0.00906). Overlapping the hernial orifice by 1.25 cm gave similar unstable results in the sublay and the IPOM position with a tendency towards even lower reconstruction stability in the latter case since all meshes were dislocated before 10 impacts.
Top box-and-whisker-plots of the cycles with complete dislocation for Parietex Progrip® lubricated with Vaseline® bridging a 5 cm transmural-transperitoneal defect with an overlap (OL) ranging from 5 to 1.25 cm in the subperitoneal IPOM position. Bottom likelihood curves of the same DIS tested hernia repairs (OL 5 cm = 5-IPOM, 3.75 cm = 3-IPOM, 2.5 cm = 2-IPOM, 1.25 cm = 1-IPOM)
The influence of closing the peritoneum on Parietex Progrip®
In five additional series of experiments, each with three repetitions, the influence of peritoneum left intact was assessed using transmuscular hernial orifices of 5 cm with the peritoneum left intact. In a first series, a 5 cm overlap was chosen to ascertain reproducible experimental conditions. In all three investigations, the Parietex Progrip® meshes were strongly attached to the tissue exhibiting no signs of mesh dislocation after 425 DIS impacts with peak pressures above 200 mmHg. On the average, a slight mesh migration up to 0.5 cm was observed being directed caudally. In the other two series with Parietex Progrip® bridging a transmuscular defect with the peritoneum intact, overlap was reduced to 2.5 cm with and without 4 corner sutures. As a suture, Surgipro® 4 metric (Covidien) with the GS-21 taper needle was applied. In both series, the meshes stayed stable in place. Mesh migration occurred being limited to 0.3 cm with and 0.5 cm without corner sutures. These results were compared with three additional reproduction experiments bridging a 5 cm transmural-transperitoneal defect as described in the first chapter of the results section. Under these conditions, 425 DIS impacts were withstood twice, mesh dislocation occurring once at impact number 61. In both successful repairs, mesh migration occurred by 1.1 and 1.8 cm starting early at cycle numbers 3 and 5 and being directed to the right and cranial. In the last series, mesh textile without the denticules was used applying 4 corner stitches to keep the mesh in place. Again, the meshes bridged a defect of 5 cm punched through the musculature leaving the peritoneum intact. Using an overlap of 2.5 cm with 4 sutures, mesh textile exhibited migration but no dislocation in all three investigation throughout the 425 DIS impacts with peak pressures above 200 mmHg. As a suture, Surgipro® 4 metric with the GS-21 taper needle was applied. A mesh migration by approximately 0.5 cm was observed.
The influence of reduced overlap on Dynamesh Cicat®
Dynamesh Cicat® in the sublay position bridged a 5 cm hernial orifice safely without fixation using a 5 cm overlap. At reduced overlap, destabilization occurred rapidly (Fig. 4). Using a circular overlap of 3.75 cm, two phases were observed: about 80% safety up to 100 impacts and a further deterioration between 100 and 200 impacts yielding 40% intact repairs beyond the 180th DIS strain. Overlaps of 2.5 and 1.25 cm were unable to sufficiently withstand DIS strain without fixation. After 25–50 DIS strains, no reconstruction was left intact with 1.25 and 2.5 cm overlap, resp. Using the Kruskal–Wallis test, the differences are significant (p < 0.001).
Top box-and-whisker-plots of the cycles with complete dislocation for Dynamesh Cicat® in sublay position with no fixation at reduced overlap (OL). Bottom likelihood curves of the DIS tested hernia repairs using Dynamesh Cicat® in sublay position. The curves correspond to the overlap given in the box plots above. NF without fixation
The influence of fixation on Dynamesh Cicat® used for bridging with reduced overlap
A total of six experimental series were conducted in an effort to heal the effects of reduced overlap by the means of fixation (Figs. 5, 6). In the first 3 series, four Glubran® bonding spots were applied while bridging with an overlap of 3.75, 2.5 and 1.25 cm (Fig. 5). An overlap of 3.75 cm was stabilized with 4 point fixation with Glubran® whereas overlaps with 2.5 cm failed in a similar two-phase fashion as observed with an unfixed 3.75 cm overlap (Figs. 4, 5). Using an overlap of 1.25 cm and 4 point Glubran® fixation, a rapid deterioration of the repair occurred similar to that of the unfixed meshes (Figs. 4, 5). Kruskal–Wallis testing demonstrated significant differences (p < 0.001).
Top box-and-whisker-plots of the cycles with complete dislocation for Dynamesh Cicat® in a sublay position with four points Glubran® (4PG) as bonding spots at reduced overlap (OL). Bottom likelihood curves of the DIS tested hernia repairs. The curves correspond to the overlaps given in the box plots above
Top box-and-whisker-plots of the cycles with complete dislocation for Dynamesh Cicat® in a sublay position with eight points Glubran® (8PG) as bonding spots at reduced overlap (OL). Bottom likelihood curves of the DIS tested hernia repairs. The curves correspond to the overlaps given in the box plots above. Surgipro® 4 metric with the GS-21 taper needle was used as suture (4S)
Increasing the number of bonding points to eight 0.8 cm Glubran® spots significantly strengthened the repair (Fig. 6). No failure occurred at an overlap of 2.5 cm whereas the reconstructions with 1.25 cm overlap gradually lost stability with no repair surviving beyond 325 DIS strains. Placing four single knot sutures in addition to eight Glubran® spots, the 100% safety level was reached, again the differences being significant (p < 0.001).
The influence of closing the peritoneum on Dynamesh Cicat®
Using an overlap of 2.5 cm and no fixation, a series of experiments was conducted with the peritoneum left intact during preparation. The statistical data are given in Table 2. An intact peritoneum prevented slippage of Dynamesh Cicat®. Compared to the data attained with a transperitoneal hernial orifice and an overlap of 2.5 cm (Fig. 4), the increase in durability was significant (p = 0.00018).
Discussion
Recurrences are frequently observed after ventral hernia repair despite advanced mesh augmentation techniques [4]. Using slow pushing or bending forces, an overlap of 5 cm is sufficient for most meshes to successfully bridge a 5 cm hernial orifice [5]. In contrast to this, dynamic intermittent strain (DIS) mimicing intraabdominal forces above 150 mmHg is badly withstood by most mesh repairs despite an overlap of 5 cm [11]. A new classification is based on the ability of meshes to stay in position without fixation upon DIS impacts simulating coughing actions postoperatively. Using a new classification, DIS class A meshes stay in place at recommended overlap [11]. Mesh migration might precede clinical hernia recurrence since intraoperative observations during the repair of recurrences can disclose dislocated meshes with displaced tacks (Fig. 7). Since the best way to heal the tendency to slip is unclear to date, a series of experiments was conducted on DIS class A meshes as described previously [11]. DIS class A meshes are defined as being primarily stable bridging a 5 cm hernia orifice with an overlap of 5 cm.
Left panel intraoperative view of a 57-year-old COPD patient demonstrating midline hernial recurrence 1 year after IPOM repair, observed from the right patient side: the right lateral edge of the mesh runs just along the median incision (marked with an arrow) and is held upwards. A wet drape covers the bowel. Right panel the mesh is explanted. The tip of the instrument points towards a tack, which is oriented parallel to the mesh and unable to resist dislocating forces. Similar changes can be observed along all borders of the mesh
Over a long period of time, a sufficient overlap is recognized as a critical influence on the durability of mesh repair [5, 13]. Recent research identified mesh placement and again the overlap as the crucial parameters to reduce stress within the repaired abdominal wall both in animals and humans [14–16]. Both meshes were investigated with DIS testing and safely bridged a 5 cm defect using a 5 cm overlap (Figs. 2, 3, 4). Reducing the overlap to 3.75 cm markedly reduced the stability in Dynamesh Cicat® and to a lesser extent in Parietex Progrip®. The differences observed are statistically not significant (p = 0.0919). These data mandate future clinical studies to ascertain the superior performance of these meshes as compared to those in other DIS classes.
Parietex Progrip® is more stable in the sublay as compared to the IPOM position (Figs. 2, 3). This is in accordance with previously published results on other meshes used for hernia repair [11]. Differences are more pronounced in the 3.75 and in the 2.5 cm groups (p < 0.05). The mesh was placed with the denticules pointing towards the fascia and musculature in the sublay and towards the peritoneum in the IPOM position. It can be assumed that the smooth face of the peritoneum provides less grip as compared to the abrasive surface of muscle and fascia. Based on the influence of phospholipids as found in peritoneal fluid, it cannot be ascertained at the moment that the results hold true for other lubricants or other mesh orientations [11].
Dynamesh Cicat® in the sublay position rapidly looses grip at reduced overlap (Fig. 4). Fixation with four bonding spots Glubran® is sufficient to stabilize Dynamesh Cicat® with an overlap of 3.75 cm. A total of 8 spots stabilize an overlap of 2.5 cm (Figs. 5, 6). It might be speculated that 12 points Glubran® may be sufficient for the 1.25 cm overlap group since 8 points Glubran® and 4 sutures again reach 100% levels (Fig. 6). At this moment, there is no proof for this assumption since a multitude of clinical data exists showing numerous influences on fixation strength [17–20]. The results presented here demonstrate that DIS testing provides an opportunity to rapidly reach data on the fixation strength of a specific device for a certain mesh.
In both meshes, the destabilization caused by a reduced overlap can be healed by leaving the peritoneum intact (Tables 1, 2). Peritoneal closure although frequently performed during surgery has only once been described as a deliberately attempted technique to prevent mesh migration [21]. Mesh slippage is rarely reported but seemingly occurs predominantly at open peritoneum [22]. Since peritoneal closure is discussed to increase postoperative pain, it is important to note that an intact peritoneum can drastically reduce mesh dislocation in ventral hernia repair using DIS class A meshes [23]. In IPOM procedures, closure of the peritoneum is hard to obtain and implies a reduction of the peritoneal bulge.
The interobserver variation was assessed using an overlap of 3.75 cm bridging a hernial orifice of 5 cm with Dynamesh CICAT® in a sublay position with the peritoneum left open (data not shown). The interobserver variation ranges in this case around 10% probably due to varying baseline pressures and biological characteristics of the pigs bellies used [11]. However, the endpoint stability in both series of experiments reached 40% after 300 dynamic impact strains. In this way, different hernia closure techniques may be compared with this model taking a variability of about 10% into account.
Caution should be exerted to extrapolate the data to larger hernial orifices. In a pilot study using a mesh designed for IPOM placement, a 7.5 cm transmuscular–transperitoneal hernial orifice was bridged with an overlap of 3.75 cm. Four corner stitches were applied to stabilize a round 15 cm Dynamesh IPOM® (FEG Textiltechnik, Aachen, Germany) bridging a 7.5 cm defect with a circular overlap of 3.75 cm. Under these conditions, dislocation occurred early without fixation. After the transmuscular application of four Maxon® No. 1 sutures, dislocation still occurred since the partial pullout of the sutures gave way to pronounced mesh migration. Under these conditions, Parietex Progrip® might demonstrate a significant advantage since the Progrip® technology has similar bonding power as four Glubran® spots (Figs. 2, 5). According to Van’t Riet et al. [24], a maximum of 7 sutures should be necessary to securely fasten a hernia mesh to bridge a 5 cm hernial orifice in pig tissue. Since this work was done on tissue stripes pulling only in one direction, circumferential strain either biplanar or ball-related might give different results [6]. Again, DIS testing is a rapid way to reach comparative data on meshes, hernia diameters and fixation devices. Such data are very valuable in the clinical setting since varying orifices may require an individualized approach to specifically address clinical problems [25, 26]. In the future, DIS testing might be one way to strive towards both reduced recurrence rates and more patient comfort.
Conclusion
Dynamic intermittent strain permits the assessment of DIS class A meshes bridging a 5 cm defect with recommended and reduced overlap according to their stability towards intermittent impacts >150 mmHg. On the bench, various conditions can be tested demonstrating peritoneal closure and various fixation techniques as a good way to stabilize ventral hernia repair. Regarding the clinical situation, the closure of the peritoneum might be superior to various fixations and can thus be recommended for different overlaps. In the future, dynamic intermittent strain should be applied to larger hernial orifices to further improve the durability of ventral hernia repair.
References
Albino FP, Patel KM, Nahabedian MY, Sosin M, Attinger CE, Bhanot P (2013) Does mesh location matter in abdominal wall reconstruction? A systematic review of the literature and a summary of recommendations. Plast Reconstr Surg 132:1295–1304
den Hartog D, Dur AHM, Tuinebreijer WE, Kreis RW (2008) Open surgical procedures for incisional hernias. Cochrane Database Syst Rev 3. Art. No.: CD006438. doi:10.1002/14651858.CD006438.pub2
Nguyen MT, Berger RL, Hicks SC, Davila JA, Li LT, Kao LS et al (2014) Comparison of outcomes of synthetic mesh vs suture repair of elective primary ventral herniorrhaphy: a systematic review and meta-analysis. JAMA Surg 149:415–421
Köckerling F, Schug-Paß C, Adolf D, Reinpold W, Stechemesser B (2015) Is pooled data analysis of ventral and incisional hernia repair acceptable? Front Surg 2:15. doi:10.3389/fsurg.2015.00015
Lyons M, Mohan H, Winter DC, Simms CK (2015) Biomechanical abdominal wall model applied to hernia repair. Br J Surg 102:e133–e139
Sahoo S, DeLouier KR, Erdemir A, Derwin KA (2015) Clinically relevant mechanical testing of hernia graft constructs. J Mech Behav Biomed Mater 41:177–188
Turner RD, Bothamley GH (2014) How to count coughs? Counting by ear, the effect of visual data and the evaluation of an automated cough monitor. Respir Med 108:1808–1815
Werner JG, Castellon-Larios K, Thongrong C, Knudsen BE, Lowery DS, Antor MA, Bergese SD (2015) Desflurane allows for a faster emergence when compared to sevoflurane without affecting the baseline cognitive recovery time. Front Med 2:75–80
An LJ, Gui B, Su Z, Zhang Y, Liu HL (2015) Magnesium sulfate inhibits sufentanil-induced cough during anesthetic induction. Int J Clin Exp Med 8:13864–13868
Siassi M, Mahn A, Vollmer M, Huber G, Morlock M, Kallinowski F (2014) Development of a dynamic model for ventral hernia mesh repair. Langenbecks Arch Surg 399:857–862
Kallinowski F, Baumann E, Harder F, Siassi M, Mahn A, Vollmer M, Morlock MM (2015) Dynamic intermittent strain can rapidly impair ventral hernia repair. Biomech J 48:4026–4036. doi:10.1016/j.jbiomech.2015.09.045i
Müllen A, Obolenski B, Schneemelcher S (2010) Textile net implant for supplying incisional hernia during open or laparoscopic surgical intervention to e.g. close hernial opening, has overlay pattern comprising pattern elements movably arranged parallel to each other. DE 102010023413 A1
Binnebösel M, Rosch R, Junge K, Flanagan TC, Schwab R, Schumpelick V et al (2007) Biomechanical analyses of overlap and mesh dislocation in an incisional hernia model in vitro. Surgery 142:365–371
Guerin G, Turquier F (2013) Impact of the defect size, the mesh overlap and the fixation depth on ventral hernia repairs: a combined experimental and numerical approach. Hernia 17:647–655
Podwojewski F, Otténio M, Beillas P, Guerin G, Turquieer F, Mitton D (2013) Mechanical response of animal abdominal walls in vitro: evaluation of the influence of a hernia defect and a repair with a mesh implanted intraperitoneally. J Biomech 46:561–566
Podwojewski F, Otténio M, Beillas P, Guerin G, Turquieer F, Mitton D (2014) Mechanical response of human abdominal walls ex vivo: effect of an incisional hernia and a mesh repair. J Mech Behav Biomed Mater 38:126–133
Rieder E, Stoiber M, Scheikl V, Poglitsch M, DalBorgo A, Prager G, Schima H (2011) Mesh fixation in laparoscopic incisional hernia repair: glue fixation provides attachment strength similar to absorbable tacks but differs substantially in different meshes. J Am Coll Surg 212:80–86
Muysoms F, Vander Mijnsbrugge G, Pletinckx P, Boldo E, Jacobs I, Michiels M, Ceulemans R (2013) Randomized clinical trial of mesh fixation with “double crown” versus “sutures and tackers” in laparoscopic ventral hernia repair. Hernia 17:603–612
Harslof SS, Wara P, Friis-Andersen H (2014) Fixation devices in laparoscopic ventral hernia repair: a review. Surg Technol Int 24:203–213
Christoffersen MW, Brandt E, Helgstrand F, Westen M, Rosenberg J, Kehlet H, Standfelt P, Bisgaard T (2015) Recurrence rate after absorbable tack fixation of mesh in laparoscopic incisional hernia repair. Br J Surg 102:541–547
Malik A, Macdonald AD, de Beaux AC, Tulloh BR (2014) The peritoneal flap hernioplasty for repair of large ventral and incisional hernias. Hernia 18:39–45
Tse G, Stutchfield BM, Duckworth AD, de Beaux AC, Tulloh B (2010) Pseudo-recurrence following laparoscopic ventral and incisional hernia repair. Hernia 14:583–587
Oguz H, Karaqule E, Turk E, Moray G (2015) Comparison of peritoneal closure techniques in laparoscopic preperitoneal inguinal hernia repair: a prospective randomized study. Hernia 19:879–885
Van’t Riet M, Van Steenwijk PJ, Kleinrensink GJ, Steyerberg EW, Bonjer HJ (2002) Tensile strength of mesh fixation methods in laparoscopic incisional hernia repair. Surg Endosc 16:1713–1716
Sorour MA (2014) Interposition of the omentum and/or the peritoneum in the emergency repair of large ventral hernias with polypropylene mesh. Int J Surg 12:578–586
Christoudias G, Nunziata M (2015) A simplified laparoscopic approach to ventral hernia repair: a new “finned” mesh configuration with defect closure. Surg Endosc. doi:10.1007/s00464-015-4480-7 [Epub ahead of print]
Acknowledgements
The project was funded by the institutional support of ASKLEPIOS Proresearch project number 2805, clinical research and development, Lohmühlenstraße 5, 20099 Hamburg, Germany. Further institutional support was granted by Heidelberger Stiftung Chirurgie, project number D.10052599, Chirurgische Universitätsklinik Heidelberg, Im Neuenheimer Feld 110, 69120 Heidelberg, Germany. In addition, financial support was supplied by Covidien contracted as project number SS3438 with ASKLEPIOS Proresearch. Materials were supplied in part by Dahlhausen and Covidien. We thank Angela Assing for supporting the data acquisition. We thank Mia Stine Matzkow for review of the language used.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
FK reports grants from Covidien and non-financial support from Dahlhausen, during the conduct of the study. AM reports grants from Covidien and non-financial support from Dahlhausen during the conduct of the study. FK and AM declare conflicts of interest not directly related to the submitted work. FH, TGS, MV declare no conflict of interests
Ethical approval
All applicable international, national, and/ or institutional guidelines for the care and use of animals were followed.
Statement of human and animal rights
I hereby undersign and certificate that the procedures and the experiments I have conducted respect the ethical standards in the Helsinki Declaration of 1975, as revised in 2000, as well as the national law. Experiments with laboratory animals were not conducted.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Kallinowski, F., Harder, F., Silva, T.G. et al. Bridging with reduced overlap: fixation and peritoneal grip can prevent slippage of DIS class A meshes. Hernia 21, 455–467 (2017). https://doi.org/10.1007/s10029-017-1583-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-017-1583-1