Abstract
Background
Single-port laparoscopic surgery (SPLS) has been introduced for totally extraperitoneal (TEP) inguinal hernia repair. Clinically, however, the benefits of single-port TEP (SP TEP) are unclear. This study aimed to compare short-term surgical outcomes between SP TEP and conventional laparoscopic TEP(CL TEP) inguinal hernia repair.
Methods
Between January 2013 and February 2015, 99 men with primary unilateral inguinal hernia were randomized to the single-port or conventional 3-port TEP procedures. The primary end point was postoperative pain. Secondary end points were complications, postoperative hospital stay, days to return to daily normal activities, cosmesis, and quality of life (QOL).
Results
We randomized 50 patients to SP TEP and 49 to CL TEP repair. The SP TEP group patients had significantly lower pain scores (visual analog scale) 7 days postoperation (p = 0.017). However, there were no significant differences between the two groups in postoperative pain scores 24 h (p = 0.44) and 4 weeks (p = 0.677) after operation and analgesic requirements on the operation day (p = 0.303) and 7 days after the operation (p = 0.204). Operation time, postoperative hospital stay, and complications were comparable between the two groups. The days to return to daily normal activities, QOL, and cosmetic satisfaction were not different between the two groups.
Conclusion
The outcomes of SP TEP hernia repair for operation time and morbidities were comparable to CL TEP, and postoperative pain was lower at 7 days than in CL TEP hernia repair. The SP TEP technique can be recommended as an alternative treatment for inguinal hernia repair in experienced hands.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inguinal hernia repair is a commonly performed general surgery. The surgical management of inguinal hernia has changed with improvements in surgical techniques and technologies [1]. Laparoscopic treatment for inguinal hernia has been reported to result in less postoperative pain, faster recovery, early return to daily activities, and enhanced cosmetic results [2]. This approach has become the first choice for inguinal hernia repair at many centers. Owing to the trend of performing minimally invasive surgeries, single-port laparoscopic surgery (SPLS) has been established many other areas of surgery as a subtype of laparoscopic surgery, maximizing the benefits of such surgery. Recently, SPLS for inguinal hernia repair has been reported, and studies have compared SPLS for inguinal hernia repair with conventional laparoscopic treatment for inguinal hernia. Several studies have reported that outcomes of single-port laparoscopic totally extraperitoneal inguinal hernia repair (SP TEP) and conventional laparoscopic TEP (CL TEP) are comparable [3–5] and that SP TEP has superior cosmetic results [6, 7]. However, the longer operation time required and its efficiency with regard to postoperative pain require further investigation. Only a few prospective randomized controlled trials have reported the use of SPLS for the treatment of inguinal hernia [8, 9]. Therefore, we designed this prospective study to compare single-port with conventional laparoscopic TEP hernia repair with regard to postoperative pain, operation time, time for recovery, cosmetic outcomes, and quality of life, using two blinded randomized groups of patients.
Materials and methods
Patients
This prospective double-blinded randomized controlled trial was performed at Daejeon St. Mary Hospital, which is affiliated with The Catholic University of Korea. Male patients aged ≥18 years, with an American Society of Anesthesiologists (ASA) score of 1 or 2 and a primary unilateral hernia diagnosed by ultrasound, were eligible for random assignment to SP or CL TEP hernia repair. The exclusion criteria were indication for an emergency surgery; a large amount of ascites; irreducible, recurrent, or bilateral hernia; and previous surgery in the lower abdomen, including appendectomy, indicated by scars over the surgical field. Randomization was carried out using opaque sealed envelopes containing computer-generated randomization sequences prepared by a study-independent statistician. Patients were not aware of their treatment group prior to the pain score survey taken 24 h postoperation. The wounds of all patients allocated to SP TEP or CL TEP were covered using a large bandage after skin closure; the shape and size of the bandage was the same for all patients, and the bandage was changed after the pain score survey taken 24 h postoperation. Written informed consent was received from all patients who were eligible to participate. The study was approved by the ethics committee of Daejeon St. Mary’s Hospital, The Catholic University of Korea (IRB code: DC12EISI0046).
Surgical technique
All surgeries were performed by a single surgeon who had prior experience performing 30 CL TEP inguinal hernia repairs and 100 SP TEP inguinal hernia repairs. Prophylactic antibiotics were given to all patients before the operation. The patient was placed in a supine position with the arm opposite the side of the hernia in adduction during general anesthesia. After completion of indirect hernia sac dissection, the sac was isolated or ligated and divided. In cases of direct hernia, the pseudo-sac of the transversalis fascia was anchored on the pubic bone by tacks (Tacker, Covidien plc, Dublin, Ireland). In both techniques, a 13 × 9 cm Parietex (Covidien plc) mesh was inserted and positioned to cover the myopectineal orifices. The mesh was fixed to the Cooper’s ligament and the anterolateral abdominal wall with tacks.
CL TEP
The CL TEP procedure was performed using three trocars. A subumbilical incision of 1.5 cm in length was made, beginning from the deepest part of the umbilicus. After dissection of the subcutaneous tissue to expose the anterior rectus sheath, a transverse incision was made on the anterior rectus sheath. The preperitoneal space was created using balloon dissection. Pneumoperitoneum was produced through a blunt tip trocar with a pressure of 8 mmHg. Two additional trocars were placed between the umbilicus and pubis midline. The surgical procedure was performed after the patient was placed in the Trendelenburg position with the side of the hernia tilted up. The preperitoneal dissection was performed using a laparoscope and two instruments, usually a grasper and a suction device with hooked tip (Surgiwand, Covidien, Mansfield, MA, USA).
SP TEP
The same type of umbilical incision was made for the insertion of the port device, which was a single-port comprising a wound retractor (Xsmall; Applied Medical, Rancho Santa Margarita, CA, USA) and a surgical glove. Three trocars were inserted in advance into the glove fingers. An 11 mm trocar was placed in the middle finger, and 5 mm trocars were placed in the index and little fingers of the glove. A rigid 30 degree 5 mm laparoscope was inserted through the 11 mm trocar. The preperitoneal dissection was performed using a laparoscope and two instruments. We used the conventional straight and rigid types of laparoscopic instruments. Patient positioning, the operative team’s position, and the procedures performed in the preperitoneal space were the same as those in the CL TEP inguinal hernia repair.
End points
The primary endpoint was the pain score 24 h postoperation. The secondary outcomes included surgical outcomes, such as analgesic requirement, operative time, length of stay, postoperative morbidities, days to return to activities of daily life (ADL), cosmetic results, and quality of life (QOL) assessment.
Follow-up and outcome measures
All patients were assessed postoperatively for pain and morbidities, and they were discharged if they presented with acceptable levels of pain and morbidities. The intravenous analgesic (Tramodol 50 mg) was used for immediate postoperative pain control, and these cases were recorded. Urinary retention was defined as a case requiring Nelaton or Foley insertion for voiding. Postoperative pain was measured by a 10 cm Visual Analogue Scare (VAS) at 24 h, 1, and 4 weeks postoperation. In cases of early discharge (i.e., within 24 h after the operation), the patients were instructed to fill out the score assessment sheet at home. At 1 week after the operation, all patients were assessed for postoperative pain, complications, and days to return to ADL in the outpatient clinic. Analgesic tablets (aceclofenac 200 mg) for pain control were provided, if required, and those cases were recorded. At 4 weeks postoperation, patients completed a questionnaire regarding cosmetic satisfaction. The patients could choose one of the following responses: very satisfied [5], satisfied [4], average [3], dissatisfied [2], and very dissatisfied [1]. In addition, postoperative complications were assessed; QOL was measured preoperatively and 4 weeks postoperatively with EuroQol.
Statistical analysis
According to our review, the mean 24 h postoperative VAS pain score was 3.4 ± 1.7 [10], and this finding could be considered clinically significant only if the mean pain score of SP TEP hernia repair was 1.0 units less than that of CL TEP hernia repair [11].
Using a 2-sided p < 0.05 as significant, achieving a power of 80 %, the calculated sample size was 46 patients in each arm. Comparisons were made by χ 2 test or Fisher exact test, where appropriate, for categorical data and the independent sample t test or Mann–Whitney U test for continuous data.
All analyses were made using SPSS version 17 (Chicago, IL). Primary analysis was performed on an intention to treat basis. No interim analyses were performed.
Results
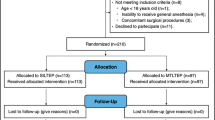
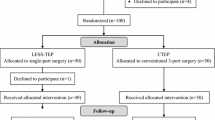
Between January 2013 and February 2015, 191 patients who presented with inguinal hernia were assessed for study eligibility. Figure 1 shows the profile of the trial according to the CONSORT statement. Sixty-one patients did not meet the inclusion criteria, and 31 withdrew consent. A total of 99 patients were randomly assigned to SP TEP (n = 50) or CL TEP (n = 49). Demographic features and hernia characteristics are shown in Table 1. There were no significant differences between the two groups with regard to age, BMI, or hernia characteristics. The operative data and complications are summarized in Table 2. No additional incisions for trocars or conversions to open surgery were required in the two groups. The two groups did not differ significantly with regard to the mean operative time, postoperative length of stay, or incidence of perioperative complications. The most common intraoperative complication was peritoneal tearing, and there was 1 case of peritoneal tearing occurring during the insertion of a spacemaker for balloon dissection in the CL TEP group. One patient in the CL TEP group required drain insertion as blood was oozing from inside the internal ring after sac extraction. There were no major postoperative complications, and none of the patients had wound infection. Postoperative follow-up results for the two groups are presented in Table 3. The SP TEP group had a significantly lower pain score at 1 week after the operation (1.7 vs. 2.6, p = 0.017). The analgesic requirement 1 week postoperation was lower for the SP TEP group, but the difference was not statistically significant (p = 0.204). During the postoperative recovery period, other parameters—including the pain score at 24 h and 4 weeks postoperation, days to return to ADL, cosmetic results, and QOL—were all comparable between the two groups. During the mean follow-up of 20 months, there were no cases of recurrence in the two groups.
Discussion
Laparoscopic TEP hernia repair has been accepted as an efficacious surgical alternative to standard tension-free hernia repair for inguinal hernias. Recent studies have shown that laparoscopic TEP has advantages over open surgery and has led to improvements in postoperative pain and recovery time; moreover, no differences in recurrence rates were noted when compared with open tension-free repair [11–13]. If there are no differences in recurrence rates and morbidities between surgical techniques, patients can choose the surgical technique that best preserves their QOL—that is, the one that involves less postoperative pain, an early return to normal activity, better cosmetic outcomes, etc. [6]. SPLS has been developed for reducing port-related morbidities and better cosmetic results. In 2009, Jacob et al. reported the first successful single-incision TEP inguinal hernia repair [14]. In SP and CL TEP hernia repair, the surgical procedure within the extraperitoneal space is technically the same; only the number of incisions for trocars differs. An increase in the number of ports is associated with a possible increase in morbidity and pain related to the ports [15]. Therefore, we aimed to evaluate the difference in early postoperative pain as a primary end point and assessed variables, such as analgesic requirement and time to return to ADL. Moreover, SP TEP is technically more difficult because of movement limitations and instrument collision. We compared operation times and complication rates between the two groups.
In this study, there were no significant differences in 24 h postoperative pain scores. The results did not demonstrate any benefit in terms of a reduction in early postoperative pain. We expected that the SP TEP technique would decrease early postoperative pain because of the reduced number of skin incisions. At the outpatient clinic, 7 days postoperation there were no wound infections in the two groups, and patients did not complain of pain at the incision site. The mean pain score 1 week postoperation was significantly lower (p = 0.017) for the SP TEP group than the CL TEP group, and the analgesic requirement was lower for the SP TEP group. However, these differences were not statistically significant. In addition, reduced pain was not associated with a shorter return to ADL. Two studies compared SP and CL TEP inguinal hernia repair [7, 16] with regard to analgesic use, and four studies compared these procedures [7, 8, 10, 16] with regard to return to ADL. Our results are consistent with their results. Two studies showed significant differences in postoperative pain. In the first randomized clinical trial by Tsai et al., the mean pain score 2 h postoperation during rest was significantly higher in the conventional TEP group than in the laparoendoscopic single-site surgery (LESS) TEP group [8]. This evidence may simply result from the reduced number of skin incisions in LESS. However, the median operative time was longer for the LESS TEP group (63.5 min) than in the conventional TEP group (50.5 min) (p = 0.001). They concluded that the LESS TEP technique is associated with longer operative time but offers the minor benefit of a reduction in immediate postoperative pain [8]. Tai et al. performed a retrospective comparative study, and their results for postoperative pain were similar to ours. The pain score 1 week postoperation was significantly lower in the LESS group. Since the mean operative time was significantly longer in the single-port TEP series, they believed the LESS TEP technique was not an efficacious surgical alternative to the standard TEP technique for inguinal hernia [10]. In our study, there were no significant differences in operative length between the two groups. We believe the single-port surgery experience of the surgeon might have affected the result. He is a single-port laparoscopic surgeon at the minimally invasive surgery center at our institution. Before initiating this study, he had performed three times more SP TEP hernia repairs than CL TEP hernia repairs. This could be a limitation of this study. However, in an analysis of 512 single-incision laparoscopic TEP procedures, Kim et al. reported that the mean operative time for unilateral hernia (41.6 min) was comparable to the operative time of 30–60 min in CL TEP studies. They believed there were two reasons for the similar operative times, which were same as in our analysis: other single-port surgery experiences and overcoming the learning period [17]. In other words, the operative time might not differ according to the surgeon’s experience.
In this study, the morbidity rate was similar in both groups. Peritoneal tear and seroma were the most common intra- and postoperative complications, respectively, in both groups. In the CL TEP group, peritoneal tearing developed during the insertion of a balloon dissector in one case. According to a previous study, balloon dissectors were used for preperitoneal space making during SP TEP in more than half of the published studies [18]. However, inserting a balloon dissector into the preperitoneal space is a blind procedure that has an insidious risk of morbidity based on the patient’s condition. We performed preperitoneal dissection using a laparoscope and two instruments in the SP group. Based on our experience, preperitoneal dissection with an instrument under direct vision is not time consuming and is safe. In addition, it can be cost-effective. In this study, we did not analyze and compare the costs of SP TEP and CL TEP inguinal hernia repair. However, when other conditions were the same (e.g., duration of hospital stay or number/types of medication), single-port TEP saved as much as $110 (i.e., the difference in cost between a balloon dissector plus two 5 mm trocars (CL TEP) and three 5 mm mini-trocars plus a wound retractor (SP TEP)). Aside from the difference in cost-effectiveness, the materials and methods are the same in both techniques [1].
Until now, four studies have evaluated and compared the cosmetic results between SP and CL TEP inguinal hernia repair: two showed no significant difference [8, 10]; one reported superior cosmetic results in the SP group [7]; and the other reported that wounds in the SP group were less detectable by others compared to wounds in the CL group (p = 0.04) although both groups were very satisfied overall with their wounds and had minimal discomfort [6]. In our study, there was no significant difference in patient cosmetic satisfaction 1 month postoperation between the SP TEP and CL TEP patients. However, without alternative scar comparisons, the self-reported questionnaire might fail to show any cosmetic advantages of LESS [8]. The postoperative cosmetic satisfaction score could change with the ability to see other cosmetic outcomes [19]. In the telephone survey results of the retrospective comparative study, both groups of patients were very satisfied with their wounds and had minimal discomfort. All patients in the SP group said they would stick with their choice of SP, and 60 % of the CL group said they would choose SP instead [6]. Although we did not access the data, most eligible patients who refused to participate in our study chose SP TEP. Thus, patients seemed to prefer the SPLS technique when similar surgical outcomes were anticipated. This selection bias could have potentially excluded subjects who might have experienced more favorable outcomes that are highly subjective, such as pain and satisfaction [19].
We acknowledge that this study has several limitations, including a small sample size and a lack of long-term outcomes, including chronic pain. Further, selection bias for surgical candidates and the proficiency of the SPLS operator could be limitations as well.
In conclusion, in this randomized double-blind controlled clinical trial, the short-term outcomes of SP TEP hernia repair were comparable to those of CL TEP inguinal hernia repair, and 7 days postoperative pain was less for SP TEP hernia repair than for CL TEP hernia repair. However, reduced pain was not associated with lower analgesic requirement or early return to daily activity. The SP TEP technique can be offered as an alternative to CL TEP inguinal hernia repair when it is performed by an experienced SPLS surgeon. Further large-scale prospective studies with long-term follow-up results are needed to confirm the potential of SP TEP inguinal hernia repair.
References
Choi BJ, Lee KJ, Lee SC (2014) Direct application of single-port laparoscopic totally extraperitoneal (TEP) inguinal hernia repair by an experienced single-port laparoscopic surgeon who was inexperienced in conventional TEP hernia repair: initial experience with 100 cases. J Laparoendosc Adv Surg Tech A 24:333–338
Memon MA, Cooper NJ, Memon B, Memon MI, Abrams KR (2003) Meta-analysis of randomized clinical trials comparing open and laparoscopic inguinal hernia repair. Br J Surg 90:1479–1492
Cugura JF, Kirac I, Kulis T, Sremac M, Ledinsky M, Beslin MB (2012) Comparison of single incision laparoscopic totally extraperitoneal and laparoscopic totally extraperitoneal inguinal hernia repair: initial experience. J Endourol 26:63–66
Kim JH, Lee YS, Kim JJ, Park SM (2013) Single port laparoscopic totally extraperitoneal hernioplasty: a comparative study of short-term outcome with conventional laparoscopic totally extraperitoneal hernioplasty. World J Surg 37:746–751
Wakasugi M, Masuzawa T, Tei M, Omori T, Ueshima S, Tori M, Akamatsu H (2015) Single-incision totally extraperitoneal inguinal hernia repair: our initial 100 cases and comparison with conventional three-port laparoscopic totally extraperitoneal inguinal hernia repair. Surg Today 45:606–610
Yang GP, Tung KL (2015) A comparative study of single incision versus conventional laparoscopic inguinal hernia repair. Hernia 19:401–405
de Araujo FB, Starling ES, Maricevich M, Tobias-Machado M (2014) Single site and conventional totally extraperitoneal techniques for uncomplicated inguinal hernia repair: a comparative study. J Minim Access Surg 10:197–201
Tsai YC, Ho CH, Tai HC, Chung SD, Chueh SC (2013) Laparoendoscopic single-site versus conventional laparoscopic total extraperitoneal hernia repair: a prospective randomized clinical trial. Surg Endosc 27:4684–4692
Wijerathne S, Agarwal N, Ramzy A, Lomanto D (2014) A prospective randomized controlled trial to compare single-port endo-laparoscopic surgery versus conventional TEP inguinal hernia repair. Surg Endosc 28:3053–3058
Tai HC, Lin CD, Chung SD, Chueh SC, Tsai YC, Yang SS (2011) A comparative study of standard versus laparoendoscopic single-site surgery (LESS) totally extraperitoneal (TEP) inguinal hernia repair. Surg Endosc 25:2879–2883
Langeveld HR, van’t Riet M, Weidema WF, Stassen LP, Steyerberg EW, Lange J, Bonjer HJ, Jeekel J (2010) Total extraperitoneal inguinal hernia repair compared with Lichtenstein (the LEVEL-Trial): a randomized controlled trial. Ann Surg 251:819–824
Belyansky I, Tsirline VB, Klima DA, Walters AL, Lincourt AE, Heniford TB (2011) Prospective, comparative study of postoperative quality of life in TEP, TAPP, and modified Lichtenstein repairs. Ann Surg 254:709–714 (discussion 714–705)
Myers E, Browne KM, Kavanagh DO, Hurley M (2010) Laparoscopic (TEP) versus Lichtenstein inguinal hernia repair: a comparison of quality-of-life outcomes. World J Surg 34:3059–3064
Jacob BP, Tong W, Reiner M, Vine A, Katz LB (2009) Single incision total extraperitoneal (one SITE) laparoscopic inguinal hernia repair using a single access port device. Hernia 13:571–572
Takata MC, Duh QY (2008) Laparoscopic inguinal hernia repair. Surg Clin North Am 88:157–178, x
Sherwinter DA (2010) Transitioning to single-incision laparoscopic inguinal herniorrhaphy. JSLS 14:353–357
Kim JH, An CH, Lee YS, Kim HY, Lee JI (2015) Single incision laparoscopic totally extraperitoneal hernioplasty (SIL-TEP): experience of 512 procedures. Hernia 19:417–422
Siddiqui MR, Kovzel M, Brennan SJ, Priest OH, Preston SR, Soon Y (2014) The role of the laparoendoscopic single site totally extraperitoneal approach to inguinal hernia repairs: a review and meta-analysis of the literature. Can J Surg 57:116–126
Ma J, Cassera MA, Spaun GO, Hammill CW, Hansen PD, Aliabadi-Wahle S (2011) Randomized controlled trial comparing single-port laparoscopic cholecystectomy and four-port laparoscopic cholecystectomy. Ann Surg 254:22–27
Acknowledgments
The statistical consultation was supported by Catholic Research Coordinating Center of the Korea Health 21 R&D Project (A070001), Ministry of Health and Welfare, Republic of Korea.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
BJC declares no conflict of interest. WJJ declares no conflict of interest. IKL declares no conflict of interest. SCL declares no conflict of interest.
Ethical approval
The study was approved by the ethics committee of Daejeon St. Mary’s Hospital, The Catholic University of Korea (IRB code: DC12EISI0046).
Informed consent
An informed consent form was signed prior to enrollment in this study by all participants.
Rights and permissions
About this article
Cite this article
Choi, B.J., Jeong, W.J., Lee, I.K. et al. Single-port versus conventional three-port laparoscopic totally extraperitoneal inguinal hernia repair: a randomized controlled trial. Hernia 20, 789–795 (2016). https://doi.org/10.1007/s10029-016-1499-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-016-1499-1