Abstract
Purpose
To analyze severe complications after groin hernia repair with respect to age, ASA score, hernia anatomy, method of repair and method of anesthesia, using nationwide registers.
Summary background data
The annual rate of 20 million groin hernia operations throughout the world renders severe complications, although rare, important both for the patient, the clinician, and the health economist.
Methods
Two nationwide registers, the Swedish Hernia Register and the National Swedish Patient Register were linked to find intraoperative complications, severe cardiovascular events and severe surgical adverse events within 30 days of groin hernia surgery.
Results
143,042 patients, 8 % women and 92 % men, were registered between 2002 and 2011. Intraoperative complications occurred in 801 repair, 592 patients suffered from cardiovascular events and 284 patients from a severe surgical event within 30 days of groin hernia surgery. Emergency operation was a risk factor for both cardiovascular and severe surgical adverse events with odds ratios for cardiovascular events of 3.1 (2.5–4.0) for men and 2.8 (1.4–5.5) for women. Regional anesthesia was associated with an increase in cardiovascular morbidity compared with local anesthesia, odds ratio 1.4 (1.1–1.9). In men, bilateral hernia and sliding hernia approximately doubled the risk for severe surgical events; odds ratio 1.9 (1.1–3.5) and 2.2 (1.6–3.0), respectively. Methods other than open anterior mesh repair increased the risk for surgical complications.
Conclusions
Awareness of the increased risk for cardiovascular or surgical complications associated with emergency surgery, bilateral hernia, sliding hernia, and regional anesthesia may enable the surgeon to further reduce their incidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Groin hernia repair is a common procedure with recognized postoperative complications such as hematoma, seroma, infection, and urine retention [1]. In 8 % of all groin hernia repairs registered in the Swedish Hernia Register (SHR), one or more complications occurred [2], a frequency close to the 10 % postoperative complication rate reported by Pollack and Nyhus [3]. However, apart from mortality [4], little is known about the incidence of serious intra- or post-operative surgical adverse events or of cardiovascular complications following groin hernia surgery. The high rate of groin hernia surgery renders these complications, although rare, important both from clinical and socio-economic points of view, even if risk for the individual patient is low.
Previous studies suggest that incidence and panorama of severe complications differ between repair techniques [2, 5, 6] and methods of anesthesia [7, 8]. The aim of this study was to analyze the incidence of intraoperative complications, cardiovascular complications, and severe surgical events within 30 days of groin hernia surgery, with respect to gender, hernia anatomy, method of repair and choice of anesthesia, using large nationwide registers.
Materials and methods
Registers and data acquisition
The Swedish Hernia Register, established in 1992, is a voluntary quality register which now covers more than 95 % of all groin hernia operations performed on patients aged 15 years or older in Sweden [9]. Data are registered prospectively after each operation and include parameters such as mode of admission, patient characteristics (ASA score), hernia type (primary/recurrent, anatomy), method of repair, anesthesia, whether or not an intraoperative complication occurred and complication noted by the operating unit within 30 days of groin hernia surgery [4, 9]. Each year 5 evaluators randomly visit 10 % of aligned units to check the validity of the data registered, and screen to see if there are operations not registered. The register has been shown to include some 98 % of operations eligible [10].
The Swedish National Patient Register (NPR) is a mandatory register collecting information regarding in-patient care, and includes surgical procedure and discharge diagnosis according to ICD-9 or ICD-10 [11]. The register was established in 1964 and achieved complete coverage of in-patient operations in Sweden in 1989. Since 2001 outpatient visits such as day-case surgery have also been included. The completeness of the register has been shown to be high, and in 2007 drop-outs not registered in the register were estimated to be less than 1 % [12].
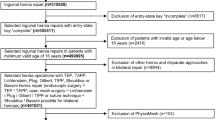
Patients
Three principally different types of complications were assessed: (1) severe cardiovascular complications, (2) severe adverse surgical events and (3) intraoperative complications registered in SHR irrespective of degree of severity. By using the unique Swedish person identity number [13], all patients registered in the SHR between 2002 and 2011 were cross-checked with the NPR to identify discharge diagnoses and reoperations within 30 days of groin hernia surgery, no matter where in Sweden the reoperation, or care given, took place. Postoperative cardiovascular events were identified retrieving ICD diagnoses for pulmonary emboli (I26), myocardial infarction (I21 and I22), and stroke (G45, G46, and I60–I68) within 30 days of groin hernia repair. Severe adverse surgical events were defined as either one of the following ICD diagnoses (T81.1, T81.2, T81.7 S35, S36), describing vascular and visceral injury, post-procedural shock and accidental puncture or laceration or as any of the intervention codes JWC, JWE and JWF coding for reoperation due to visceral or vascular injury. In the SHR intraoperative complications were registered as “yes” or “no”.
If registered twice in the SHR, whether for reoperation of a recurrence, bilateral hernia or hernia repair on the contralateral side, only the index operation was included in the study to avoid double-registration of complications after bilateral hernia repair. Combined hernias with a femoral component were registered as “femoral hernia”, all other hernias as “inguinal”. Method of repair was classified as open anterior mesh repair, laparoscopic technique, open posterior repair and sutured repair. Anterior mesh repair includes the Lichtenstein operation and plug techniques. Laparoscopic groin hernia repair used either the TransAbdominal PrePeritoneal technique (TAPP) or the Total ExtraPeritoneal Technique (TEP). No distinction is made between the two laparoscopic techniques in the analyses. However, in Sweden 90 % of the laparoscopically performed groin hernia operations are performed as using TEP. Due to the considerable difference in anatomy, method of operation and mode of admission, gender is planned to be analyzed separately.
Statistics
The SPSS, 21 was used for statistical analyses. Odds ratios (OR) were obtained using multivariate logistic regression analyses. ASA scores (included in the SHR register from 2003 onwards) were missing for 11 % of registered operations, and hence the multivariate analyses included some 89 % of operations registered. In case a value was missing for any of the covariates, the patient was excluded from the multivariate analyses. Significance was set at a p value < 0.05. When patients suffered from more than one “cardiovascular complication” or “severe surgical events” he/she is only counted once in the multivariate analyses for respective complication category. However, the same patient might be included in all three complication categories if he/she suffers from both cardiovascular and severe adverse surgical events. Interaction between gender and each of the other covariates was tested in separate analyses. Approval for the study was obtained from the Regional Ethics Committee in Stockholm.
Results
During the study period (2002–2011) 162,713 groin hernia operations were registered in 143,041 patients: 12,001 (8 %) women and 131,041 men (92 %). Operations due to infection or pain or where information of hernia anatomy was missing, in total 1049 operations, were excluded from further analyses. Additionally, 76 operations were excluded because of missing information concerning method of operation, ending up with 141,916 eligible operations. Characteristics of the repairs registered are shown in Table 1. Emergency operations were carried out in 17 % of women compared to 5 % of men, and patients operated as an emergency were older than electively treated patients. The proportion of femoral hernia operations in women was 23 % (2670/11,623) compared to 1 % (1324/128,944) in men. Statistically significant interactions were seen between gender and all of the remaining covariates with “cardiovascular complication” as well as “severe surgical events” as dependent variables (all p < 0.05).
Incidences of complications within 30 days of surgery are shown in Table 2. According to discharge diagnosis found in the NPR, 592 patients suffered from at least one cardiovascular event: 183 myocardial infarctions, 353 cerebrovascular lesions, and 73 pulmonary emboli. Intraoperative complications were registered in 801 repairs, and serious surgical adverse events occurred after 284 groin hernia repairs, detected either by discharge diagnosis and or by re-operation code. In three cases both ICD-code and intervention code were registered for the same patient. Since ASA score was included in 2003, the multivariate analyses include patients registered 2003 and onwards. ASA score was missing in 11 % (1242/11,623) of women and 12 % (15,025/130,190) of men.
Cardiovascular events according to NPR
Odds ratios for cardiovascular events are analyzed and listed separately for men and women in Table 3. Compared to their younger peers, patients above 60 years had a significantly increased risk of suffering from a cardiovascular event within 30 days of groin hernia surgery; OR 24.7 (3.3–182.8) for women and 4.4 (3.2–6.0) for men. Patients with ASA scores 3 and above had an increased risk for cardiovascular complications compared to patients with ASA scores 1–2; OR 3.3 (1.9–5.7) in women and 4.6 (3.8–5.7) in men.
No difference was found between inguinal and femoral hernias in men. However, in women the risk of suffering from severe cardiovascular complication was increased in patients with femoral hernia, OR 1.9 (1.0–3.5).
Sutured repair in men and women were associated with an almost doubled risk for cardiovascular event compared to open anterior mesh.
Compared to local anesthesia, a significant increase in cardiovascular events was seen after regional anesthesia in men [OR 1.4 (1.1–1.9)]; whereas, no difference was seen between local and general anesthesia.
Intraoperative surgical complication as registered in the SHR
Intraoperative complications registered in the SHR, and severe surgical events indicated by ICD and re-operation codes found in the NPR are analyzed separately. 28 of 801 patients registered as having intraoperative complications in SHR also had an ICD or reoperation code indicating severe surgical complication.
As shown in Table 4, laparoscopic and suture repair were associated with increased risk of intraoperative complications in men compared to open anterior mesh, OR 1.7 (1.2–2.4) and 1.7 (1.3–2.2). In both men and women, emergency surgery for hernia, bilateral hernia, and ASA scores above 2, were associated with a significantly increased intraoperative complication rate compared to their respective counterparts (Table 4). In men but not in women, sliding hernia was also associated with an increased risk of intraoperative complications.
Severe surgical complication, as registered in the NPR
Table 5 shows the OR for severe adverse surgical events noted in the NPR. In contrast to high age, ASA score greater than 2 was associated with a threefold increased risk in women and twofold increased risk in men. In women, high age was also significantly associated with an increase in severe surgical events. In men, bilateral hernia, sliding hernia, and recurrent hernia were all associated with a significantly increased risk for adverse surgical event, whereas hernia anatomy had no significant impact (see Supplementary Table 1). Patients treated as an emergency had twice as many surgical complications compared to electively operated patients. In men, suture repair and posterior open repair were significantly associated with increased risk for adverse surgical events compared to open anterior mesh repair.
Gender
In multivariate regression analysis including gender (data not shown) male gender was associated with a significantly increased risk for cardiovascular events compared to women [OR 1.4 (1.0–2.0), p = 0.038]. Male gender was also associated with increased risk for intraoperative complications [OR 1.6 (1.1–2.2), p = 0.007]. As for severe surgical complications registered in the NPR, no difference in risk was observed with respect to gender (see Supplementary Table 2). In multivariate analysis with the surgical complication and cardiovascular complications as dependent variables, there were several statistically significant interactions between gender and the other covariates (see Supplementary Table 2). This motivates subgroup analysis, with stratification for men and women.
Discussion
Cardiovascular, intraoperative, and severe adverse surgical events are rare after groin hernia surgery, but due to the enormous volume of hernia surgery these adverse events deserve attention. Our study shows that age above 60 years, ASA score of 3 and above, and emergency surgery were associated with an increased risk for cardiovascular complications within 30 days of surgery. Bilateral repair, sliding hernia, recurrent operation, ASA score above 2, and methods of repair other than open anterior mesh were all associated with increased risk for surgical complications, either intraoperative or severe postoperative surgical events.
Strength and weaknesses of this study
The strength of this study is the national coverage of both the SHR [9] and NPR [12] creating a nationwide study, unselected and complete in its inclusion of intraoperative groin hernia complications, ICD-10 diagnoses, and re-interventions within 30 days of groin hernia surgery.
The present study investigates the risk for cardiovascular events after groin hernia surgery in relation to age, ASA score, method of repair, and anesthesia, but the risk was not considered in the context of corresponding risk in the background population. Groin hernia is indeed a disease of the elderly, as are cardiovascular events. To address this weakness an additional study is planned where cardiovascular complications are analyzed in more detail and put into the context of the background population. Separate multivariate analyses, were performed for men and women, if not stated otherwise, since hernia incidence, [14] anatomy [15] and re-operation risks [16] differ according to gender. Multivariate analyses used in the present study is a strength since it limits the influence of strong associations between factors such as that femoral hernia is more common in older women, etc. Whenever a value was missing for any variable, the patient was excluded from the multivariate analysis. The degree of severity of intraoperative complications is not known, but for a surgeon to register an intraoperative complication it has to be clinically relevant.
In register studies such as this association is found and discussed. However, as with other observational studies, it is not possible to determine the exact cause and effect. There might be other important factors, left out from the analyses that would otherwise have an effect on its result.
Cardiovascular events
Only 0.4 % of adult patients with groin hernia repair in Sweden 2002–2011 suffered from a cardiovascular complication within 30 days of surgery. The increased risks for cardiovascular and surgical complications after emergency hernia surgery, seen in this study, are in line with the literature [4, 17, 18]. This is no surprise since emergency surgery often takes place outside office-hours, and patients may have a somatic status severely deranged after hours or days of bowel obstruction.
Age and male gender are known risk factors for cardiovascular events [19] in accordance with the findings in this study. We found a significantly increased number of cardiovascular events after regional anesthesia compared to local and general anesthesia, as has been noted in previous studies [20, 21]. Bay-Nielsen et al. showed that 55 % of patients dying within 7 days of groin hernia surgery had received regional anesthesia, even though regional anesthesia was only used in 18 % of patients. Furthermore, all fatalities after regional anesthesia were cardiac deaths with suspected or confirmed myocardial infarction [7]. Prospective studies confirm that bradycardia and cardiac arrest is a fatal and important complication associated with spinal anesthesia, with up to seven arrests for every 10,000 patients [22]. The proportion of patients with regional anesthesia in the SHR has dropped from approximately 80 % in 1992 to 10 % in 2012 [9], in accordance with guidelines from The European Hernia Society where it is stated that spinal anesthesia is to be avoided for groin hernia surgery [23].
Surgical complications
Registered in the NPR the incidence of severe surgical adverse events was 0.2 % (284/141,496), comparable with findings in other studies [24]. Intraoperative complications according to SHR occurred in 0.6 % (801/140,567) of operations. A recurrent hernia had an almost twofold increased risk for severe surgical complication, reflecting the results of other studies [25], and is probably the result of a distorted anatomy.
Many studies, the largest being a randomized controlled trial [25] with more than 2000 patients, have noted an increased risk for severe injury when using the laparoscopic approach [5, 23, 24, 26]. In this study, the OR for intraoperative complications registered in the SHR was 1.7 (1.2–2.4), for laparoscopy compared to open anterior mesh. Sutured technique also had an increased risk compared to the open anterior technique. For severe surgical events noted in the NPR, open posterior repair and suture repairs were associated with increased risk compared to open mesh repair, see Table 4.
Bilateral operation
The advantages of bilateral hernia repair has been advocated to include less stress for the patient, less time off work, and less expense [27]. Amid et al. presented excellent results with no increase in postoperative morbidity after bilateral groin hernia repair performed under local anesthesia [27], a result confirmed in other studies [28]. In the present study, however, bilateral hernia repair doubled the risk for severe surgical complication compared to unilateral repair. It is important to stress that this concerns severe adverse surgical events which is extremely rare in groin hernia surgery and hence should not be doubled for bilateral operations. It is also important to stress that the present study has not compared the risk of serious complications when bilateral surgery is performed at the same time or divided on two separate occasions. For intraoperative complications, bilateral hernia was associated with a sixfold increased risk in women and a twofold increased risk in men compared to unilateral hernia repair. Other authors have found similar results. Gass et al. [29] reported of TEP performed for both bilateral and unilateral repair and found a significantly increased incidence of intraoperative complication in bilateral repair compared to unilateral (3.1 vs 1.9 %) [29]. Bilateral operations are increasingly more common today because of the easy access to the contralateral side with the use of laparoscopic technique. The above study, however, clearly questions this strategy and further studies are required.
Sliding hernias are of special concern regarding risk for visceral injury. When the colon or, less commonly, the urinary bladder forms a part of the hernia sac without being covered by the peritoneum, the risk for injury is increased. Case reports report various organs contained in sliding hernias. In most cases, however, it is the sigmoid colon, the urinary bladder, and the caecum or appendix [30]. There are few reports on the outcome after repair for sliding groin hernias, and the incidence of visceral injury is thus poorly understood although a complication rate of 16 % after sliding hernia repair has been reported [31]. This concurs with the doubling of the risk for surgical complications in sliding hernias compared to non-sliding hernias observed in the present study.
The above study show that individuals above the age of 60 years or with ASA score above, 2 have a higher risk of suffering from severe cardiovascular complications after groin hernia repair. Therefore, the operation should be planned carefully both by the anesthesiologist and surgeon. If feasible, use local anesthesia on older patients or on patients with high comorbidity. In order to decrease the risk of severe adverse surgical events it is possible that two surgeons should perform attend operations of higher risk such as emergency operations, recurrent hernia operations, and when one might suspect sliding hernias to be present.
In conclusion, age 60 years and above, male gender, high ASA score, regional anesthesia and emergency surgery were associated with an increased risk for cardiovascular complications. All methods other than open anterior mesh repair were associated with increased risk for surgical complication as were sliding hernia, bilateral hernia, emergency hernia, recurrent hernia and emergency operation.
References
Bendavid R (1998) Complications of groin hernia surgery. Surg Clin North Am 78(6):1089–1103
Lundstrom KJ, Sandblom G, Smedberg S et al (2012) Risk factors for complications in groin hernia surgery: a national register study. Ann Surg 255(4):784–788
Pollak R, Nyhus LM (1983) Complications of groin hernia repair. Surg Clin North Am 63(6):1363–1371
Nilsson H, Stylianidis G, Haapamaki M et al (2007) Mortality after groin hernia surgery. Ann Surg 245(4):656–660
O’Reilly EA, Burke JP, O’Connell PR (2012) A meta-analysis of surgical morbidity and recurrence after laparoscopic and open repair of primary unilateral inguinal hernia. Ann Surg 255(5):846–853
Paajanen H, Scheinin T, Vironen J (2010) Commentary: Nationwide analysis of complications related to inguinal hernia surgery in Finland: a 5 year register study of 55,000 operations. Am J Surg 199(6):746–751
Bay-Nielsen M, Kehlet H (2008) Anaesthesia and post-operative morbidity after elective groin hernia repair: a nation-wide study. Acta Anaesthesiol Scand 52(2):169–174
Nordin P, Zetterstrom H, Gunnarsson U et al (2003) Local, regional, or general anaesthesia in groin hernia repair: multicentre randomised trial. Lancet 362(9387):853–858
Haapaniemi S (2001) A Swedish thesis on groin hernia surgery. Hernia 5(4):204–205
www.socialstyrelsen.se/register/halsodataregister/patientregistret
Ludvigsson JF, Andersson E, Ekbom A et al (2011) External review and validation of the Swedish national inpatient register. BMC Public Health 11:450
Ludvigsson JF, Otterblad-Olausson P, Pettersson BU et al (2009) The Swedish personal identity number: possibilities and pitfalls in healthcare and medical research. Eur J Epidemiol 24(11):659–667
IM, R., Epidemiologic, economic, and sociologic aspects of hernia surgery in the United States in the 1990s. The Surgical clinics of North America Vol. 6. 1998
Mahadevan, V., Essential anatomy of the abdominal wall, in Management of Abdominal Hernias, L.K. Kingsnorth A, Editor. 2013, Springer: London Heidelberg New York. pp. 25–53
Koch A, Edwards A, Haapaniemi S et al (2005) Prospective evaluation of 6895 groin hernia repairs in women. Br J Surg 92(12):1553–1558
Derici H, Unalp HR, Bozdag AD et al (2007) Factors affecting morbidity and mortality in incarcerated abdominal wall hernias. Hernia 11(4):341–346
Kulah B, Gulgez B, Ozmen MM et al (2003) Emergency bowel surgery in the elderly. Turk J Gastroenterol 14(3):189–193
Jousilahti P, Vartiainen E, Tuomilehto J et al (1999) Sex, age, cardiovascular risk factors, and coronary heart disease: a prospective follow-up study of 14 786 middle-aged men and women in Finland. Circulation 99(9):1165–1172
Nordin P, Hernell H, Unosson M et al (2004) Type of anaesthesia and patient acceptance in groin hernia repair: a multicentre randomised trial. Hernia 8(3):220–225
Ozgun H, Kurt MN, Kurt I et al (2002) Comparison of local, spinal, and general anaesthesia for inguinal herniorrhaphy. Eur J Surg 168(8–9):455–459
Pollard JB (2001) Cardiac arrest during spinal anesthesia: common mechanisms and strategies for prevention. Anesth Analg 92(1):252–256
Simons MP, Aufenacker T, Bay-Nielsen M et al (2009) European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 13(4):343–403
Neumayer L, Giobbie-Hurder A, Jonasson O et al (2004) Open mesh versus laparoscopic mesh repair of inguinal hernia. N Engl J Med 350(18):1819–1827
Matthews RD, Anthony T, Kim LT et al (2007) Factors associated with postoperative complications and hernia recurrence for patients undergoing inguinal hernia repair: a report from the VA Cooperative Hernia Study Group. Am J Surg 194(5):611–617
McCormack, K., N.W. Scott, P.M. Go, et al., Laparoscopic techniques versus open techniques for inguinal hernia repair. Cochrane Database Syst Rev, 2003(1): p. CD001785
Amid PK, Shulman AG, Lichtenstein IL (1996) Simultaneous repair of bilateral inguinal hernias under local anesthesia. Ann Surg 223(3):249–252
Serpell JW, Johnson CD, Jarrett PE (1990) A prospective study of bilateral inguinal hernia repair. Ann R Coll Surg Engl 72(5):299–303
Gass M, Rosella L, Banz V et al (2012) Bilateral total extraperitoneal inguinal hernia repair (TEP) has outcomes similar to those for unilateral TEP: population-based analysis of prospective data of 6505 patients. Surg Endosc 26(5):1364–1368
Bendavid R (2002) Sliding hernias. Hernia 6(3):137–140
Adams RA, Wysocki AP (2010) Outcome of sliding inguinal hernia repair. Hernia 14(1):47–49
Acknowledgments
The above paper is an original study, not previously published, however, included in a thesis: Mortality and Morbidity after groin hernia surgery—the role of nationwide registers in finding and analyzing rare outcomes. ISBN:978-91-7459-755-4. Neither one of the authors stated above have any financial or personal relationships that could inappropriately influence the author’s decisions, work, or manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
HN declares no conflict of interest
GS declares no conflict of interest
UA declares no conflict of interest
PN declares no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Nilsson, H., Angerås, U., Sandblom, G. et al. Serious adverse events within 30 days of groin hernia surgery. Hernia 20, 377–385 (2016). https://doi.org/10.1007/s10029-016-1476-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-016-1476-8