Abstract
Purpose
Although ventral incisional hernia (VIH) repair in patients is often evaluated in terms of hernia recurrence rate and health-related quality of life, there is no clear consensus regarding optimal operative treatment based on these parameters. It was proposed that health-related quality of life depends largely on abdominal muscle function (AMF), and the present review thus evaluates to what extent AMF is influenced by VIH and surgical repair.
Methods
The PubMed and EMBASE databases were searched for articles following a systematic strategy for inclusion.
Results
A total of seven studies described AMF in relation to VIH. Five studies examined AMF using objective isokinetic dynamometers to determine muscle strength, and two studies examined AMF by clinical examination-based muscle tests.
Conclusion
Both equipment-related and functional muscle tests exist for use in patients with VIH, but very few studies have evaluated AMF in VIH. There are no randomized controlled studies to describe the impact of VIH repair on AMF, and no optimal surgical treatment in relation to AMF after VIH repair can be advocated for at this time.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ventral incisional hernia (VIH) is a common complication to abdominal surgery occurring in 11–23 % of patients undergoing laparotomy [1]. These hernias may cause pain, limitation of daily life function, complications including intestinal strangulation and poor cosmesis [2, 3] calling for early elective reconstructive surgery. Different surgical techniques for VIH repair exist, including open or laparoscopic access, various types of placement and fixation of a prosthetic mesh, and different release procedures for larger hernias as the recently reported components separation by minimally invasive techniques [4]. Laparoscopic repair of VIHs leads to a shorter hospital stay [5] and a faster return to daily physical activities [6] compared with open repair. However, currently, there is no consensus on the optimal technique for VIH repair.
The main concern when investigating long-term outcome of VIH repair is the rate of hernia recurrence, which has a reported incidence of 19–30 % depending on surgical technique [7, 8]. Health-related quality of life improves after VIH repair [9], but not much attention has been given to the impact of hernia surgery on the objective measurements of the function of the abdominal wall. This may be of particular interest in patients with giant VIHs. The present paper reviews the literature on abdominal muscle function (AMF) in patients with VIH.
Anatomy of the abdominal wall
The anterior abdominal wall is comprised of four muscles: the rectus abdominis, the external and internal abdominal obliques, and the transversus abdominis. The external abdominal oblique muscle originates from the lower eight ribs and inserts in the iliac crest and the pubic bone. The internal abdominal oblique muscle is profound from the external oblique. It originates from the anterior 2/3 of the iliac crest and the lateral 2/3 of the inguinal ligament and inserts on the three lower ribs. The function of the oblique muscles is to rotate the trunk and perform lateral flexion of the spine. The innermost muscles of the abdominal wall are the transversus abdominis, which originate from the thoracolumbar fascia, the lower six costal cartilages, the anterior 2/3 of the iliac crest and the lateral 1/3 of the inguinal ligament and insert in the linea alba. The transversus abdominis is the main muscle to retain the abdominal contents, as well as they are important in forced expiration. The rectus abdominis muscles are mainly involved in ventral flexion of the spine. They originate from the symphysis and insert in the xyphoid process and ribs 5, 6, and 7. The medial insertions of the three lateral abdominal muscles create the rectus sheath, which surrounds the rectus abdominis muscles. The dorsal lamina of the rectus sheath runs from the costae to approximately 4 cm caudal to the umbilicus. Below this arcuate line, no dorsal sheet exists. In the midline, the two rectus abdominis muscles are connected by the linea alba that forms the medial continuation of the rectus sheet.
When the pressure inside the abdomen becomes higher than the abdominal wall can resist, a hernia is formed at the weakest point of the abdominal wall. After midline laparotomy, the weakest point in the abdominal wall is often the incisional scar, and therefore, herniation frequently occurs here. Several risk factors for developing VIH have been identified, including inappropriate surgical technique, smoking, obesity, diabetes, wound infection, and use of immunosuppressive medication [10, 11]. Several studies have shown that the connective tissue in patients with incisional hernias has an altered collagen composition, which is believed––but never proven––to add further to the formation of the hernias [12, 13].
Taken together, the abdominal wall is a complex unit providing movement of the trunk, protection of intraperitoneal contents, and contribution to vital functions including respiration, miction, and defecation. This unit is dysfunctional when a VIH is acquired, yet not much is known about AMF before and after VIH repair. It was hypothesized that quality of life and AMF are highly correlated, and as a consequence, AMF is an important measure for evaluation of the outcome from different VIH repair techniques. Hence, the purpose of this paper was to review the literature published regarding AMF in patients with VIH.
Method
A search in both the PubMed and EMBASE databases was conducted to identify relevant studies. Search criteria included the terms (ventral hernia OR incisional hernia) AND (abdominal wall strength OR muscle strength). The abstracts of studies found by this literature search were reviewed, and criteria of relevance included reports on coupled measures of AMF and patients with VIH. Articles concerning AMF in relation to other surgical procedures than VIH repair were also identified and assessed for relevance. Reference lists and the function “Related articles” in PubMed of relevant hits were reviewed in order to locate studies not identified during the initial search. Only articles in English were included, and there was no limit as to the year of publication.
There are several ways to measure the force that can be generated by muscles, and determination of work output both with static and dynamic muscular work can be done. In this article, the term ‘strength’ will be used as a general term including all the different ways to express the force generated by the abdominal muscles.
Results
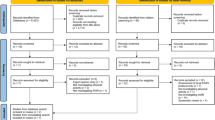
The literature search identified 183 articles, eight of which were duplicates. Of the remaining 175 studies, seven were assessed relevant. A flow chart of the search results according to the PRISMA guidelines [14] is shown in Fig. 1.
There were different ways to measure the function of the abdominal wall (Table 1). Three studies explored the application of the Biodex® isokinetic dynamometer (Biodex Corporation, Shirley, NY, USA). In this test system, the patient is strapped to a chair and performs dynamic truncal muscular flexion and/or extension at a certain pre-determined constant angle speed. The outcome is reported by the system as a peak torque, which is the force generated around the axis, measured in Newton meters. This system was used for validation of the dynamometer in a recent study performed on two groups: patients with giant VIH (>10 cm fascia defect) and healthy volunteers [15]. The tests were carried out in two series with 1 week between the measurements and showed significant test–retest reliability. This method has been applied in clinical praxis to examine the differences in AMF in 24 patients undergoing VIH repair using different surgical techniques [16]. No significant differences between groups of patients who had undergone surgery for giant VIH with the onlay, sublay, or intraperitoneal method were found using the Biodex® System-4. All patients were tested 1 year following the surgical procedure indicating that the late post-operative AMF was independent of type of operation. No pre-operative tests were conducted.
Comparison of AMF in healthy volunteers and patients with hernia has also been done using the Biodex® isokinetic dynamometer (Model 2000, Multi-joint System-3) dividing the subjects into three different groups [17]: patients who had undergone VIH repair either by an open non-mesh technique or by laparoscopic repair with an intraperitoneal mesh, and a control group comprised of healthy volunteers. The peak torque of the abdominal wall flexor muscles was greater in patients who had undergone open surgery compared with patients who were operated on by laparoscopic techniques and significantly greater when considering male patients only. Healthy volunteers had a mean AMF of 238 % compared with both of the operatively treated groups of patients.
The Cybex® dynamometer (Lumex Inc., Ronkonkoma, NY) is another device for mechanical measurement of AMF and is largely equivalent with the Biodex® system. One group reported their experiences with the components separation technique using that equipment [18]. Only two patients underwent measurement of AMF, demonstrating approximately a 40 % gain in truncal flexion force generation after the procedure as compared with the pre-operative measurement. The Cybex® dynamometer has also been used to examine AMF after VIH repair by the use of a free vascularized composite anterolateral thigh flap in four patients [19]. Only post-operative measurements were done, and examination revealed a decrease in peak torque power of the trunk flexion compared to literature references.
Clinical examination as the only way to measure AMF was reported in two articles. One study evaluated the usefulness of determining AMF by three different physical tests: double leg lowering, trunk raising, and supine reaching [20]. All three tests were performed by three different examiners on 35 patients waiting for surgical repair of their VIH. In 10 of these cases, tests were repeated 4 months post-operatively, though no direct comparison with the pre-operative tests was made. Outcome of the study showed that the double-leg-lowering test and the trunk-raising test were reproducible, and therefore, methods by which objective measurement of AMF can be done. Pre- and post-operative tests were not compared. The results from the two tests were categorized, forming a 10-point AMF score that is claimed—but not validated—to be a reliable way to objectively determine AMF.
Janda’s test is performed with the patient in supine position and with immobilized lower extremities. The patient is then asked to raise the trunk and keep a straight position. A score of zero indicates no palpable muscle contraction, and five indicate raise of the trunk with hands touching the ears and elbows spread laterally. The entire grading system is displayed in Table 2. The test was used in a clinical setting in an older study reporting the ‘sliding door technique’ for VIH repair [21]. This technique takes the component separation one step further and completely releases the rectus abdominis muscle from both its anterior and posterior sheath, after which direct suture of the rectus muscles and sheaths is done in three layers. Janda’s muscle test was only performed post-operatively in seven of ten patients, with an average score of three.
Discussion
To our knowledge, this is the first literature review on AMF in patients with VIH. We found different means of measuring AMF in patients with VIH described in seven studies. Two studies reported on the usefulness of test systems in VIH patients who did not undergo surgery, and two studies included both pre- and post-operative examinations of which only one specifically compared the results [18, 20].
Objective mechanical measurement of AMF was assessed by test machines or clinical examinations. The greatest upside of mechanical tests involving machines is the objective approach that is associated with less subjective interpretation bias. The quantification of muscle strength opens up for more exact assessment of the AMF in future studies on VIH repair. The obvious downside of these tests is the equipment costs as well as the limited flexibility for conducting tests in different locations. On the other hand, clinical objective examination tests can be carried out almost anywhere and are inexpensive at the expense of less accuracy and reproducibility. The loss of accuracy may be particularly important, as these tests may not be accurate enough to detect changes induced by surgical repair of VIH. The assessment of AMF by clinical examination in patients with VIH is thus considered inferior to the use of fixated dynamometers.
The Biodex® system was the dynamometer most extensively evaluated in the current review [15–17]. This system has also been reported reliable for determination of AMF in patients with diastasis recti [22]. The 10-point abdominal wall strength score for VIH patients proposed by Parker et al. [20] may be a valuable tool in the future, but since it has only been used in a single center, no conclusions regarding the applicability of the score system can yet be drawn. The Cybex® dynamometer was used in two studies on a total of six patients [18, 19]. To our knowledge, this equipment and the Janda’s muscle test [21] have not been critically evaluated for use in VIH patients, and further studies are required to assess whether these tests are valid methods for measurement of AMF in VIH patients.
Laparoscopic VIH repair is superior to open surgery in several respects. Interestingly, Den Hartog et al. reported open surgery superior in relation to AMF [17]. Contrary to open surgery, conventional laparoscopic VIH repair does not normally include a closure of the fascial defect. The intraperitoneal mesh that is placed under laparoscopy may bulge under increased abdominal pressure [23]. Hypothetically, open VIH repair with approximation of the fascial borders in the midline may restore the abdominal wall anatomy and enhance AMF supporting the findings of Den Hartog et al. This study, however, was limited by a low number of patients and the lack of a pre-operative assessment of AMF raising the risk that the findings of the study could be coincidental. Moreover, the pre-operative sizes of the fascial defects were not reported, and this could also influence on pre- and post-operative AMF since the extent of the anatomical and functional changes varies according to the hernia size.
The studies describing the sliding door technique and the use of a composite free anterolateral thigh flap have limited clinical implications, as no pre-operative control tests of AMF were performed. To our knowledge, neither the sliding doors technique nor an anterolateral thigh flap is used as standard for VIH repair anywhere today.
Objective measurements of AMF have also been done in relation to other surgical procedures. A pedicled transverse rectus abdominis musculocutaneous (TRAM) flap including part of the anterior rectus fascia may be used for breast reconstruction. Evaluation of AMF after this invasive procedure has been done in several published studies. The B200 IsoStation machine was thus used to assess AMF in 21 patients before and 1 year after surgery [24]. A significant loss of strength was demonstrated in static trunk flexion after bilateral TRAM flaps suggesting that this apparatus has a place for assessment of AMF in relation to VIH repair.
In a recent study, Paiuk et al. examined AMF in 22 patients before and after midline incisions due to colorectal cancer [25]. A custom-made wall-mounted dynamometer and a digital manometer (Micro RPM, Micro Medical Limited, UK) were used to measure the force generated when the patients leaned forward, sitting in a chair with the dynamometer placed at the xiphoid process. Results showed a significant 10 % decrease in isometric trunk flexion strength in male patients 6 weeks after surgery, which is not surprising when considering the trauma exerted. In female patients, a drop in isometric trunk flexion strength was also found, but since only seven female patients were included, this was not a significant drop. No late follow-up measurements were reported.
AMF was measured by Janda’s muscle test and the Cybex® 6000 machine in patients after laparoscopic and open cholecystectomy, and the results were compared with measurements obtained in healthy volunteers [26]. Both types of surgery impaired AMF, but contrary to VIH repair, the laparoscopic group was less impaired than the group subjected to open surgery. The muscular trauma associated with division of the right rectus abdominis muscle during open cholecystectomy may account for this finding.
In conclusion, several objective mechanical tests and clinical examinations are available for the assessment of AMF. Objective assessments with fixated dynamometers appear as the optimal method to assess changes in AMF induced by VIH repair. Unfortunately, there are only few studies in patients with VIH and only one that compares pre- and post-operative AMF. Randomized clinical trials are warranted to compare AMF and quality of life before and after VIH repair following allocation to different surgical techniques. Such studies would provide data to validate how to achieve optimal post-operative AMF and whether this outcome reflects patients’ satisfaction.
References
Cassar K, Munro A (2002) Surgical treatment of incisional hernia. Br J Surg 89:534–545
Courtney CA, Lee AC, Wilson C, O’Dwyer PJ (2003) Ventral hernia repair: a study of current practice. Hernia 7:44–46
Nieuwenhuizen J, Kleinrensink GJ, Hop WC, Jeekel J, Lange JF (2008) Indications for incisional hernia repair: an international questionnaire among hernia surgeons. Hernia 12:223–225
Giurgius M, Bendure L, Davenport DL, Roth JS (2012) The endoscopic component separation technique for hernia repair results in reduced morbidity compared to the open component separation technique. Hernia 16:47–51
Sauerland S, Walgenbach M, Habermalz B, Seiler CM, Miserez M (2011) Laparoscopic versus open surgical techniques for ventral or incisional hernia repair. Cochrane Database Syst Rev (3):CD007781. doi:10.1002/14651858.CD007781
Rosen M, Garcia-Ruiz A, Malm J, Mayes JT, Steiger E, Ponsky J (2001) Laparoscopic hernia repair enhances early return of physical work capacity. Surg Laparosc Endosc Percutan Tech 11:28–33
Helgstrand F, Rosenberg J, Kehlet H, Strandfelt P, Bisgaard T (2012) Reoperation versus clinical recurrence rate after ventral hernia repair. Ann Surg 256:955–958
Ballem N, Parikh R, Berber E, Siperstein A (2008) Laparoscopic versus open ventral hernia repairs: 5 year recurrence rates. Surg Endosc 22:1935–1940
Mussack T, Ladurner R, Vogel T, Lienemann A, Eder-Willwohl A, Hallfeldt KK (2006) Health-related quality-of-life changes after laparoscopic and open incisional hernia repair: a matched pair analysis. Surg Endosc 20:410–413
Sugerman HJ, Kellum JM Jr, Reines HD, DeMaria EJ, Newsome HH, Lowry JW (1996) Greater risk of incisional hernia with morbidly obese than steroid-dependent patients and low recurrence with prefascial polypropylene mesh. Am J Surg 171:80–84
Beltran MA, Cruces KS (2008) Incisional hernia after McBurney incision: retrospective case–control study of risk factors and surgical treatment. World J Surg 32:596–601
Si Z, Bhardwaj R, Rosch R, Mertens PR, Klosterhalfen B, Klinge U (2002) Impaired balance of type I and type III procollagen mRNA in cultured fibroblasts of patients with incisional hernia. Surgery 131:324–331
Henriksen NA, Yadete DH, Sorensen LT, Agren MS, Jorgensen LN (2011) Connective tissue alteration in abdominal wall hernia. Br J Surg 98:210–219
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 62:1006–1012
Gunnarsson U, Johansson M, Strigard K (2011) Assessment of abdominal muscle function using the Biodex system-4. Validity and reliability in healthy volunteers and patients with giant ventral hernia. Hernia 15:417–421
Johansson M, Gunnarsson U, Strigard K (2011) Different techniques for mesh application give the same abdominal muscle strength. Hernia 15:65–68
den Hartog D, Eker HH, Tuinebreijer WE, Kleinrensink GJ, Stam HJ, Lange JF (2010) Isokinetic strength of the trunk flexor muscles after surgical repair for incisional hernia. Hernia 14:243–247
Shestak KC, Edington HJ, Johnson RR (2000) The separation of anatomic components technique for the reconstruction of massive midline abdominal wall defects: anatomy, surgical technique, applications, and limitations revisited. Plast Reconstr Surg 105:731–738
Kuo YR, Kuo MH, Lutz BS, Huang YC, Liu YT, Wu SC, Hsieh KC, Hsien CH, Jeng SF (2004) One-stage reconstruction of large midline abdominal wall defects using a composite free anterolateral thigh flap with vascularized fascia lata. Ann Surg 239:352–358
Parker M, Goldberg RF, Dinkins MM, Asbun HJ, Daniel Smith C, Preissler S, Bowers SP (2011) Pilot study on objective measurement of abdominal wall strength in patients with ventral incisional hernia. Surg Endosc 25:3503–3508
Kuzbari R, Worseg AP, Tairych G, Deutinger M, Kuderna C, Metz V, Zauner-Dungl A, Holle J (1998) Sliding door technique for the repair of midline incisional hernias. Plast Reconstr Surg 101:1235–1242
Stark B, Emanuelsson P, Gunnarsson U, Strigard K (2012) Validation of Biodex system 4 for measuring the strength of muscles in patients with rectus diastasis. J Plast Surg Hand Surg 46:102–105
Schoenmaeckers EJ, Wassenaar EB, Raymakers JT, Rakic S (2010) Bulging of the mesh after laparoscopic repair of ventral and incisional hernias. JSLS 14:541–546
Dulin WA, Avila RA, Verheyden CN, Grossman L (2004) Evaluation of abdominal wall strength after TRAM flap surgery. Plast Reconstr Surg 113:1662–1665
Paiuk I, Wasserman I, Dvir Z (2012) Effects of abdominal surgery through a midline incision on postoperative trunk flexion strength in patients with colorectal cancer. Hernia. doi:10.1007/s10029-012-1027-x
Balogh B, Zauner-Dung A, Nicolakis P, Armbruster C, Kriwanek S, Piza-Katzer H (2002) Functional impairment of the abdominal wall following laparoscopic and open cholecystectomy. Surg Endosc 16:481–486
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jensen, K.K., Kjaer, M. & Jorgensen, L.N. Abdominal muscle function and incisional hernia: a systematic review. Hernia 18, 481–486 (2014). https://doi.org/10.1007/s10029-014-1242-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-014-1242-8