Abstract
Purpose
Inguinal hernioplasty could be used as an indicator of the surgical quality offered in different health institutions and countries, thereby establishing a scientific basis from which the procedure can be critically assessed and ultimately improved. Quality assessment of hernioplasties could be conducted using two different methods: either analyzing dedicated regional/national databases (DD) or reviewing administrative databases (AD).
Methods
A retrospective study of inguinal hernioplasties was carried out in the Emilia-Romagna hospitals between 2000 and 2009. Data were obtained by analyzing Hospital Discharge records regional Databases (HDD). Descriptive and multivariate statistical analysis was performed.
Results
126,913 inguinal hernioplasty procedures were performed. The annual rate was on average 34 per 10,000 inhabitants. An increase of the case mix complexity and relevant changes in procedure technique were recorded. From multivariate analysis, the following independent factors related to a hospitalization longer than 1 day emerged: procedures in urgent setting (OR 3.6, CI 3.4–3.7), Charlson’s score ≥2 (OR 3.4, CI 3.1–3.7), laparoscopy (OR 2.1, CI 1.9–2.3), no mesh use (OR 2.1, CI 2–2.3), age >65 years (OR 1.9, CI 1.8–1.9), associated interventions (OR 1.9, CI 1.8–1.9), bilateral hernia (OR 1.7, CI 1.6–1.8), recurrent hernia (OR 1.2, CI 1.1–1.2) and female gender (OR 1.2, CI 1.2–1.3). Factors related to non-prosthetic hernioplasty were: bilateral hernia (OR 2.7, CI 2.5–2.9), female gender (OR 1.8, CI 1.8–2.0), emergency setting (OR 1.6, CI 1.5–1.8), recurrences (OR 1.5, CI 1.4–1.6) and associated interventions (OR 1.5, CI 1.4–1.6).
Conclusion
Inguinal hernia should be treated as an outpatient procedure in the majority of patients. Precise guidelines are necessary. HDD demonstrated to be a good and trustworthy system to collect clinical data. When precise guidelines are lacking, legal/institutional indications play a pivotal role in shifting the hernia surgery toward a one-day surgery regimen.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inguinal hernioplasty is one of the most commonly performed surgical procedures in general surgery [1]. In 1989, prosthetic inguinal repair was introduced [2] which further improved the outcome and recovery from this procedure, allowing day surgery treatment and reducing the recurrence rate [3].
Inguinal hernioplasty could be used as an indicator of the surgical quality offered in different health institutions and countries, thereby establishing a scientific basis from which the procedure could be critically assessed and ultimately improved. Quality assessment of hernioplasties has been conducted using two different methods: either analyzing dedicated regional/national databases (DD) [4, 5] or reviewing administrative databases (AD), such as those formed by Hospital Discharge records regional Databases (HDD) [1]. Indeed, the source of data is crucial for the assessment of clinical outcomes, as detailed information is needed if individual patients’ circumstances and surgical risks are to be properly taken into account. DD is based on a prospective collection of detailed information regarding clinical characteristics of individual patients and offers precise clinical data with detailed outcome analyses and follow-up investigations. However, the organization of such a database and its maintenance are complex and expensive endeavors, requiring ample resource, and the population of interest is typically limited in size. On the other hand, the alternative would be an administrative database, based on the collection and analysis of the administrative data from hospital admission and discharge paperwork. The benefits of such a system include availability and accessibility, having low maintenance costs and allowing large population studies by including nearly 100 % of patients who had undergone a specific surgical procedure. Nonetheless, such databases are limited by incomplete clinical and limited follow-up data.
The aim of our study was to monitor the outcomes of inguinal hernia surgical repair in the Emilia-Romagna region (Italy, 4,432,418 inhabitants), evaluating the data contained in the HDD for ten consecutive years (2000–2009).
Methods
Data extraction
From HDD, we selected all the hernioplasty procedures carried out in public and private hospitals between 2000 and 2009, regarding patients older than 14 years and resident in our region, based on diagnosis and procedure codes (Table 1).
For any procedure, Charlson’s comorbidity score [6] has been calculated based on the presence of concomitant disease in the index or in previous admissions (up to 1 year previously).
Data concerning in-hospital and 30-day mortality were obtained linking the hospital discharge records and the regional registry of mortality through the unique patient’s code.
Recurrent hernias were identified either by ICD9CM codes (550.01, 550.03, 550.11, 550.13, 550.91, 550.93) or by bilateral interventions in patients already operated for inguinal hernia, or by any hernioplasty in patients already operated for bilateral hernia. Indications for laparoscopic procedures include recurrences and bilateral hernia. Emergency admissions were identified by codes 550.0X and 550.1X.
Statistical analysis
The age- and gender-adjusted hospitalization rate for hernioplasty has been estimated for each year of the period considered, using a direct standardization method with Emilia-Romagna 2000 (year) population as reference. All preoperative and intraoperative variables were first analyzed using univariate analysis to evaluate their changes over the period (tested by the Cochran-Armitage Trend Test) and to determine whether any single factor had influenced any event of interest, procedures performed without the use of prosthesis and length of stay (LOS) more than 1 day (tested by Mantel–Haenszel Chi square test).
Variables that achieved a p value <0.05 in the univariate analysis were examined using multivariate analysis by forward stepwise logistic regressions to evaluate independent risk factors for main outcomes [27]. Different models were run for each event, including as covariates: age >65 years old, gender, Charlson score ≥2, urgent setting, relapses, bilateral hernia, use of mesh, laparoscopic/open approach, association with other surgical intervention, public/private hospitals and the years as variables. The analyses were performed using SAS version 9.1.
Results
From 2000 to 2009, 126,913 inguinal hernia repair procedures have been performed in Emilia-Romagna hospitals. The age–gender standardized rate was on average 34 admissions per 10,000 inhabitants, as shown in Fig. 1. The age-adjusted prevalence for males (31 admission per 10,000 males) was higher than that observed for females (3 admission per 10,000 females). Almost half (46 %) of the hernioplasty procedures were performed on patients aged more than 65 years, increasing from 46.6 % in 2000 to 48.2 % in 2009 (p < 0.0001). 2.1 % of patients had relevant comorbidities (Charlson’s score ≥2), with a statistically significant (p < 0.0001) increase from 2000 (1.8 %) to 2009 (2.3 %). Indirect hernia was the most common type (56.5 %) and had a significant increasing trend (p < 0.0001) in the decade (from 51.5 to 59.8 %).
The procedure for bilateral hernia repair interested the 7.4 % of the patients and decreased from 10.6 to 5.6 % (p < 0.0001), as well as the hernioplasties codified as recurrence reduced to 26.1 % over time. On the other hand, increased percentage both of hernioplasties performed with additional surgical procedures (cholecystectomy, large and small bowel resection, procedure on testicles) and those in emergency has been recorded. Surgeons opted for the laparoscopic approach for inguinal hernia repair in 1.5 % of the cases, with a significant increase during the period from 1 to 2 % (p < 0.0001). Almost three-quarters of the procedures were performed in public hospital, even if a significant reduction of 5.5 % was recorded from 2000 to 2009.
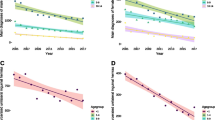
The two outcomes of interest, length of stay longer than 1 day and no-prosthetic hernia repair, had a significant p < 0.0001 decrease over the period (Fig. 2).
Length of stay longer than 1 day represented the most part (56.5 %) of admissions for hernioplasty in 2000, but this percentage decreased dramatically, up to half in 2004. A progressive decrease, even if lower than the previous period, was recorded during subsequent years.
Similarly, the percentage of no-prosthetic procedures reduced from 6.7 to 4 %.
Multivariate analysis has confirmed the association between the years after 2004 and the outcomes of interest: length of stay longer than 1 day (OR: 0.4 p < 0.0001) and no-prosthetic hernia repair (OR: 0.8 p < 0.0001), adjusting for case mix (Table 2). Both of the outcomes were associated with patient’s and intervention’s complexity, as indicated in Table 3.
The mean in-hospital mortality was 0.1 % (n = 188) and remained relatively stable over the period; the 30-day mortality rate was on average 0.2 % and was significantly higher for patients older than 80 years of age (1.8 %) than for those younger (0.1 %; OR 16.8, 95 % CI 13.4–21, p < 0.0001).
Discussion
The evaluation system assessing the quality and organization of the health-care industry is still very controversial. The concept of “Clinical Governance” has been introduced within the Great Britain National Health System (NHS) to assess the quality and service throughout the country, both through NHS itself and through patient feedback [7, 8].
Significantly revamping the system would require an organization-wide transformation; the key point of the transformation would involve implementing true quality assessment and finding the best system with which to conduct such an assessment. This is true, especially for evaluating the surgical branch of the health system, because it is difficult to analyze the surgical procedures and their outcomes and to find the surgical procedure that is really representative of the “surgical quality” in general. Among surgical procedures proposed as indicators of the performance of the surgical system, hernioplasty has been used quite frequently, being a surgical procedure widely performed in general surgery.
In general, the available literature discusses two major systems for efficiently collecting data about a specific surgical procedure. The first system is the DD in which all surgeons operating in a country/region/area register every procedure they perform including patient data, the technique used and the postoperative outcome (like in the Danish Hernia Database or Swedish Hernia Register) [5, 9–12, 24–26]. The second system involves AD that collect data from all public and private hospitals of a given region or country, obtaining such information from hospital admission and discharge charts. On one hand, the main advantage of the AD system is the ability to retrospectively record almost 100 % of the surgical procedures performed using the coding system based on the ICD-9-CM. AD are also readily available and accessible at low costs. However, they often result in inaccurate data registration as well as inexact follow-up and recurrence/complication information; additionally, they often lack case mix adjustment. Contrastingly, the DD system collects detailed data regarding the clinical characteristics and circumstances of individual patients. This system features a high level of accuracy for clinical data, follow-up assessment and outcome analysis because each step of the data collection process is completed by specialists. However, the organization and management of such a system is often complicated, expensive, time-consuming and resource-demanding. Furthermore the DD system typically involves a limited number of enrolled patients.
Although there have been previous studies involving “hernia audits” in regional populations [5, 13], nationwide studies have rarely been conducted.
Some of the main concerns of scientific interest involve the nature of the initial hospital admission and the postoperative recovery time. In certain European countries, such as England [14], there are strict surgical guidelines for hernia cases.
This study covers 126,913 inguinal hernia surgeries and, to the extent of our knowledge, is the largest study ever published. The data were obtained from an AD and the aim of the study was to investigate the postoperative outcomes of inguinal hernia surgery in Emilia-Romagna.
The distribution of surgeries demonstrates a distinct prevalence of inguinal hernias occurring in patients in their fifth and sixth decades of life. These data demonstrate that the hernia pathology is consistently evident during a period of several years in a given population. It is also clear that this pathology tends to affect the middle-aged and elderly.
Inguinal hernias are much more common in men. 91.1 % of the patients were male, which presents a sharp lopsidedness with important statistical implications. The Swedish Hernia Register (SHR) enrolled 90,648 patients between 1992 and 2003 [9] and the percentage of women experiencing inguinal hernia was only 8 %. In another DD from Scotland, the percentage of women was 7 % [15].
The overall proportion of patients having a Charlson’s score >2 demonstrates a significant increase. Typically, with a favorable preoperative risk assessment and attentive preoperative care, patients are more likely to undergo surgery. Surprisingly, operated patients with a high comorbidity index do not necessarily experience noticeably lengthened postoperative recovery periods.
Bilateral hernia repair significantly decreased over time suggesting a progressive change in both the patients’ and surgeons’ preferences. Bilateral hernia repair is an instance in which laparoscopic techniques have proven to be very effective as demonstrated in literature. However, laparoscopy was employed in a very small percentage of these procedures.
The incidence of direct hernias remained relatively stable, while there was a significant increase in the incidence of indirect hernias. This increase is associated with a decrease in the coding of unspecified types. A possible explanation for this shift could be better anatomic identification of indirect hernias and a more accurate coding performed by surgeons. These data do not differ significantly between AD and DD. In fact in the Swedish Hernia Register [9], the rates of direct hernias were calculated to be 35.5 and 24.5 % in normal and emergency settings, respectively. Indirect hernias ranged from 53.7 to 49.1 % in normal and emergency settings, respectively. Lastly, unspecified hernias ranged from 9 to 9.7 %. These data imply difficulties in recording precise anatomical classifications by either AD or DD methods.
The number of operations performed with the use of a mesh has increased. The use of mesh also depends on the type of surgery performed. Meshes have been used more frequently in unilateral hernia repairs. Surprisingly, a lower percentage of mesh use has been observed in recurrences than in primary hernias. In urgent settings, the use of meshes is lower than in non-urgent settings. Obviously, in an urgent setting there is a higher likelihood of encountering an infected or potentially contaminated field and the use of prostheses could be more dangerous than non-tension-free hernia repair techniques. All these data have been confirmed by a multivariate analysis.
The percentage of interventions performed using laparoscopic techniques is still very low. In Denmark, the rate of laparoscopic hernia repair is 5 %, in England 9 %, in Sweden 23 % and in Scotland 4 % [4, 10, 13, 15, 24]. Interesting data concerns the indications for laparoscopy. In Italy, there are no standardized national guidelines designating the circumstances in which laparoscopy should be used for hernia repair. In other countries, such as England and the Netherlands, the appropriate indications for using the laparoscopic approach are events involving bilateral and/or recurrent cases [14, 16–20]. Considering the results of the present study and the overstated indications, national guidelines should be made to foster and enforce a more straightforward compliance with standardized indications for laparoscopic hernia repair. Several studies have demonstrated that many surgeons are often unfamiliar with these techniques [16]. Moreover, laparoscopic techniques have higher rates of serious complications and are more costly than open techniques; these drawbacks are not sufficiently offset by benefits to make it cost-effective [21]. These data emphasize the need for a set of standardized guidelines as well as adequate training.
The association between hernioplasty and other procedures increased throughout the course of the study period. This differs between laparoscopic and open surgical procedures, reflecting the infrequent use of laparoscopy.
In our region since 2000 (Bollettino Ufficiale Regionale N. 79/4.5.2000), inguinal hernia repair was classified as an outpatient procedure. This legal distinction, the widespread use of prosthetic materials and increased cooperation between the National Sanitary System and private hospitals lead to a relative surge in the number of operations performed with one-day recovery times. As a part of a wide program addressed to optimize economical resources, the Emilia-Romagna region has reduced the number of available hospital beds and introduced financial incentives to curb hospital use. By adopting this policy, the Emilia-Romagna region has succeeded in reducing the use of acute hospital beds for patients in selected diagnosis-related groups.
Present data demonstrate also the need for a precise set of standardized guidelines to further improve the quality of the National Sanitary System and to reduce the admission time. The same phenomenon was observed in England. In fact, in 1993, the Royal College of Surgeons published a set of national guidelines which stated that at least 30 % of all hernia repairs should be conducted as one-day cases [22, 23]. In a period of 7 years, from 1993 to 1999, the percentage of hernioplasties with 1-day admissions increased from 18 to 70 % [23]. In Italy, however, no such national guidelines exist. With pathology like inguinal hernias, there should be a set of case-sensitive guidelines to help surgeons decide which treatment would be the most appropriate and cost-effective.
The percentage of emergency hernioplasties (6.4 %) is similar in other countries: Scotland (5 %), Denmark (4 %) and Sweden (5.9 %) [9, 10, 15, 24–26].
In-hospital mortality remained relatively constant. The risk of death 30 days post-surgery was significantly higher for patients older than 80 years. Other studies evaluated this cutoff at 60 years of age and demonstrated mortality rates of 0.02 % and 0.4 % for patients younger and older than 60 years, respectively. The reported mortality rate for operations performed in emergency settings is 7 % [10]. The Danish Hernia Database reported a 30-day mortality rate of 3.1 % [9, 24, 25].
Data from the present study demonstrated that inguinal hernia should be treated as an outpatient procedure in the majority of patients. For this purpose, precise guidelines are necessary to improve the quality of the procedure and to avoid money wasting. However when precise guidelines are lacking, the introduction of legal/institutional indications plays a pivotal role in shifting the hernia surgery toward the one-day surgery regimen.
References
Phillips W, Goldman M (2004) Groin Hernia. From “Health care needs assessment, the epidemiologically based needs assessment reviews” First Series, Vol 1, 2nd edn., Radcliffe Publishing UK
Lichtenstein IL, Shulman AG, Amid PK, Montlor MM (1989) The tension-free hernioplasty. Am J Surg 157:188–193
Scott N, Go PMNYH, Graham P, McCormack K, Ross SJ, Grant AM (2001) Open mesh vs non-mesh for groin hernia repair. Cochrane database of systematic reviews, issue 3. Art. No.:CD002197
Nilsson E, Haapaniemi S (1998) Hernia registers and specialization. Surg Clin North Am 78:1141–1155
Bay-Nielsen M, Kehlet H (1999) Establishment of a national Danish hernia data base: preliminary report. Hernia 3:81–83
Charlson ME, Pompei P, Ales K, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis 40:373–383
Halligan A, Donaldson L (2002) The meaning and implementation of clinical governance. G Ital Nefrol 19(suppl 21):S8–S13
Thompson RG, Donaldson LJ (1990) Medical audit and the wider quality debate. J Public Health Med 12:149–151
Koch A, Edwards A, Haapaniemi S, Nordin P, Kald A (2005) Prospective evaluation of 6,895 groin hernia repair in women. Br J Surg 92:1553–1558
Bay-Nielsen M, Kehlet H, Strand L et al (2001) Quality assessment of 26,304 herniorrhaphies in Denmark: a prospective nationwide study. Lancet 358:1124–1128
Haapaniemi S (2001) Quality assessment in groin hernia surgery—the role of a register. Medical dissertation no. 695. University of Linkoping: Linkoping
Nilsson E, Haapaniemi S (2002) Assessing the quality of hernia repair. In: Fitzgibbons RJ Jr, Greenburg AG (eds) Nyhus and Condon’s Hernia (5th edn). LippincottWilliams and Wilkins, Philadelphia, pp 567–573
O’Riordan DC, Kingsnorth AN (1998) Audit of patient outcomes after herniorrhaphy. Surg Clin North Am 78:1129–1139
National guideline cleringhouse. Work loss data institute. Hernia. Corpus Christi (TX): work loss data institute; 2006
Hair A, Duffy K, McLean J et al (2000) Groin hernia repair in Scotland. Br J Surg 87:1722–1726
McCormack, Wake B, Perez J et al (2005) Laparoscopic surgery for inguinal hernia repair: systematic review of effectiveness and economic evaluation. Health Technology Assessment Vol 9: No. 14
National institute for clinical excellence. (2004) Laparoscopic surgery for inguinal hernia repair. NICE technology appraisal guidance no. 83. National institute for clinical excellence, London
Association of surgeons of the Netherlands (2003) Dutch guidelines for inguinal hernia repair. Van Zuiden Communications BV, Alphen
Simmons MP, deLange D, Beetsw GL, van Geldere D, Heij HA, Go PM (2001) The “Inguinal Hernia” guideline of the association of surgeons of the Netherlands. Ned Tijdschr Geneeskd 147:2111–2117
de Lange DH, Aufenacker ThJ, Roest M, Simmermacher RKJ, Gouma DJ, Simons MP (2005) Inguinal hernia surgery in the Netherlands: a base line study before the introduction of the Dutch guidelines. Hernia 9:172–177
McCormack K, Scott NW, Go PM, Ross S, Grant AM On behalf of the EU hernia trialists collaboration (2003) Laparoscopic techniques versus open techniques for inguinal repair (review). Cochrane database of systematic reviews, issue 1. Art. No. CD001785
Report of a working party convened by the Royal College of Surgeon of England. Clinical guidelines on the management of groin hernias in adult. London: RCS, 1993
Mokete M, Earnshaw JJ (2001) Evolution of an inguinal hernia surgery practice. Postgrad Med J 77:188–190
Bay-Nielsen M, Nilsson E, Nordin P, Kehlet H (2004) Swedish Hernia Database the Danish Hernia Database. Chronic pain after open mesh and sutured repair of indirect inguinal hernia in young males. Br J Surg 91(10):1372–1376
Rosenberg J, Bisgaard T, Kehlet H, Wara P, Asmussen T, Juul P, Strand L, Andersen FH, Bay-Nielsen M.(2011) Danish Hernia Database. Danish Hernia Database recommendations for the management of inguinal and femoral hernia in adults. Dan Med Bull;58(2):C4243
Lundström KJ, Sandblom G, Smedberg S, Nordin P (2012) Risk factors for complications in groin hernia surgery: a national register study. Ann Surg 255(4):784–788
Schmidt CO, Kohlmann T (2008) When to use the odds ratio or the relative risk? Int J Public Health. 53(3):165–167
Acknowledgments
We dedicate this work to Orazio Campione, Professor of Surgery and Head of Emergency Surgery Department of the S.Orsola-Malpighi Hospital (University of Bologna, Italy) from 1995, who passed away prematurely in August 2003. We also want to thank Daniel Lazzareschi, from the department of Integrative Biology of the Berkeley University (USA), for the precious work of text editing.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ansaloni, L., Coccolini, F., Fortuna, D. et al. Assessment of 126,913 inguinal hernia repairs in the Emilia-Romagna region of Italy: analysis of 10 years. Hernia 18, 261–267 (2014). https://doi.org/10.1007/s10029-013-1091-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-013-1091-x