Abstract
Background: In 2003 the Dutch Guidelines for treatment of inguinal hernia (IH) were published. For treatment of IH in adults, the evidence-based guidelines recommend the use of a mesh repair technique. In order to be able to evaluate the effects of these guidelines, a baseline analysis of inguinal hernia surgery before the introduction of these guidelines had to be performed. The second analysis will be performed two years (January–March 2005) after the publication of the Guidelines. Objective: To make an inventory of IH surgery in the Netherlands, before the introduction of guidelines for IH treatment, to serve as a baseline for future evaluation of the impact of the implementation of these guidelines. Methods: A retrospective descriptive study was performed in 2003 using patient and operation charts including IH repairs performed in The Netherlands over a three-month period (January-March 2001). Results: 97/133 (73%) hospitals cooperated with the study, generating data from a total of 4386 IH in 3979 patients (3284 adults, 695 children). Mesh techniques were used in 2839 (78%) adult inguinal hernias while 800 (22%) patients were treated with non-mesh techniques. 484 (14.7%) adult patients were operated on during the study period for a recurrent hernia from previous years. Early recurrence (<1 year) occurred in 2.2% of all patients. Wound infection was documented in 0.8% of all IH. The mortality rate was 0.1%. 1257 of the 3284 (38.3%) adults, and 566 of the 695 children (81.4%), were operated on in ambulatory care. Conclusions: In the episode prior to implementation of the Dutch evidence-based Guidelines for treatment of inguinal hernia, 2839 (78%) adult patients were treated with mesh repair and 484 (13.3%) patients were treated for a recurrent hernia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In 2003 a Dutch committee developed evidence-based guidelines for the treatment of inguinal hernia (IH) in children and adults [1, 2]. The main recommendations of the guidelines were to use a mesh-based repair technique in adult patients, preferably in day surgery, and to consider local anaesthesia when performing open anterior repair. For primary one-sided IH, the Guidelines recommend a Lichtenstein repair technique. For recurrences after an anterior repair and bilateral hernia, an endoscopic repair technique is recommended, provided a trained team is available. The Guidelines furthermore consist of 20 chapters with recommendations concerning all aspects of IH surgery from diagnosis to postoperative treatment.
It is expected that the Guidelines will improve quality, efficiency and transparency in IH surgery [1, 2]. To be able to evaluate the implementation of these Guidelines, a baseline analysis of IH surgery was performed. The results of this baseline analysis are to be compared with a second analysis that will take place in 2005, in order to establish a possible effect of the implementation of the guidelines on IH surgery in the Netherlands. Increased use of mesh technique will hopefully result in a decrease in recurrence operations.
The goal of this study was to set a baseline analysis and at the same time to perform an inventory of IH surgery in the Netherlands. It was of primary interest to assess the operating techniques and the percentage of operations performed for recurrences. The secondary goal was to make an inventory of other aspects, like frequency of ambulatory care surgery, type of anaesthesia, level of surgical expertise, and complications.
Patients and methods
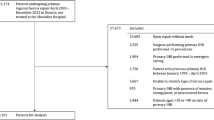
A retrospective descriptive study of IH repairs performed in The Netherlands in the period January–March 2001 was performed. All patients had been operated on at least a year prior to the data collection. All Dutch hospitals (133) were asked to participate, and if they agreed (97), to provide data on all patients operated on in the study period. Various hospital registration systems were used to identify all of the patients (derived from all performed operative procedures). All data was retrieved from on-site visits in 2003 with original patient and operation charts by one of the authors (DL, TA, MR).
The following data were obtained; age, type of hospital (academic centres, teaching hospitals and non-teaching hospitals), admission or day surgery, operation for primary or recurrent hernia with previous operation technique, unilateral/bilateral hernia, the number of years after previous repair (in recurrent hernia), acute versus elective surgery, and the number and type of complications. The type of hernia, the operation technique, the expertise of the surgeon, and the type of anaesthesia were obtained from the operation report. Patients with a bilateral hernia were evaluated as two separate hernias in two different patients. Children (<18 years) and adults (≥18 years) were analysed separately. Femoral hernias were excluded from this inventory.
The numbers involving surgeons or residents performing the operation are solely based on the data from (academic and district) teaching hospitals (43/97 participating hospitals).
Statistical analysis
Data were expressed as mean±standard deviation (SD). Comparison of data was performed using the Student t-test for paired and unpaired data when appropriate. Proportions were compared using chi-square analysis with Yates’ correction. For all tests, a P-value <0.05 was considered significant.
Results
The study included 97 of the 133 (73%) hospitals in The Netherlands in 2001 (6/8 academic centres, 37/46 teaching hospitals and 54/79 non-teaching hospitals). This resulted in a total of 4386 IH in 3979 patients (3284 adults, 695 children). The mean age of the adults was 57.6 years (range 18.5–96.5), and of the children 4.2 years (range 0.1–17.9).
Children (<18 years)
General findings
695 children were operated on, with a total of 747 hernias. 566 children (81.4%) underwent their operation in day surgery, 136 (18.2%) of the operations were performed in a paediatric hospital. The patient, hernia and surgical characteristics are outlined in Table 1.
Operating techniques
Hernia sac resection was performed in 719 (96.3%) of the cases. The Bassini and Shouldice techniques were used in ten and six cases respectively (total 2.1%). In five (0.7%) patients a mesh technique was used (Lichtenstein (three), Grid Iron (one) and a plug (one)); the mean age in these patients was 15.6 years (12.9–17.7), and these comprised three direct and two indirect hernias. The technique was unknown or data were missing in seven cases (0.9%).
35 (4.7%) of the patients underwent acute or semi-acute surgery for strangulated or incarcerated hernia. A contralateral exploration was performed in 45/410 (10.9%) children (≤4 years). In clinics with paediatric surgeons this percentage was 38.5% (37/96). The mean age of these children was 0.7 years (0.1–3.9).
Complications
44 (5.9%) complications were registered. 14 (1.9%) patients were found to have a recurrence within 12 months, all after hernia sac resection. They all underwent a second operation within twelve months. Haematoma/seroma occurred in 12 cases (1.6%). There were 13 (1.7%) reports of pain, and the pain lasted longer than three months in two of these patients (0.3%). Two patients (0.3%) had a wound infection, and in one case (0.1%) there was postoperative bleeding which did not need another operation.
Adults (≥18 years)
General findings
A total of 3639 hernia repairs in 3284 patients were performed. 2017 of the 3639 (55.4%) repairs were performed in non-teaching hospitals and 1622 of the 3639 (44.6%) in teaching hospitals (including academic centres). The patient, hernia and surgical characteristics are outlined in Table 2.
Operating techniques
The IH repair techniques used are displayed in Table 3. In 2839 (78.0%) of all IH operations a mesh repair technique was used and in 800 (22.0%) a conventional (non-mesh) technique; 86.2% of patients with a recurrent IH were operated on using a mesh repair technique this time.
In teaching hospitals (including academic centres), more hernias (1350/1622, 83.2%) were treated with mesh than in non-teaching hospitals (1481/2017, 73.4%, p<0.01). Endoscopic repair techniques were performed more frequently in teaching hospitals (303/1622, 18.7%) than in non-teaching hospitals (182/2017, 9.0%, p<0.01).
Of the 355 patients (710 hernias) with a bilateral hernia, 621 (87.5%) were treated with a mesh technique and 89 (12.5%) without the use of mesh techniques. 79 patients with bilateral hernias (158 hernias, 22.3%) underwent endoscopic repair. In Bilateral hernias an endoscopic repair technique 158/710 (22.3%) was used more often than in unilateral hernias 323/710 (11%), p<0.01. 71 (2.0%) patients underwent acute surgery for strangulated or incarcerated hernia.
The previous technique used in recurrent IH is outlined in Table 4. The interval between the last IH operation and the operated recurrence is reported in Table 5. In patients operated on for recurrence, 42% had undergone the prior operation more than ten years ago. Admitted adult patients were older than patients treated in day surgery; 60.7±16 years versus 52.2±15 years (p<0.01). The average duration of hospitalisation was 1.7±1.7 days (1–40).
Complications
In 813 (22.3%) cases, one or more (total 916) complications occurred during or after operation, as shown in Table 6. Four patients died during hospital admission (bowel perforation after Lichtenstein, bladder perforation after Lichtenstein, bronchospasm after Stoppa and a cardiac arrest one day post-surgery after Lichtenstein). 111 (3.4%) patients underwent a re-operation: 74 (2.2%) because of a recurrence (within one year), 22 (0.7%) because of hematoma, seven (0.2%) because of neuralgia, three (0.1%) because of a wound infection, and five (0.2%) for other reasons. In one patient with a deep infection, the mesh was removed. The three bowel perforations originated after respectively a TEP, a Lichtenstein and a PHS repair technique.
Discussion
The present study of 4386 inguinal hernia repairs in 3979 patients performed between January and March 2001 in The Netherlands will be used as baseline analysis to be able to evaluate the implementation of the Dutch Guidelines for inguinal hernia repair. This is the first study evaluating the different techniques used for treatment of inguinal hernias in 73% of Dutch hospitals.
In the series of paediatric inguinal hernia the most remarkable and worrying fact was the high incidence of early recurrences. In univariate analysis, surgeon’s experience, patients’ age and type of hospital were no significant risk factors for early recurrence. However these recurrences should be considered as technical failures. There was no significant difference between the paediatric hospitals (1.5%) and the other hospitals (2.0%). The subject of contralateral exploration remains controversial [3]. In this study 10.9% of all children ≤4 years underwent a contralateral exploration. In paediatric clinics this percentage was much higher (38.5%). This is probably related to the higher prevalence of prematurely born or high-risk patients, and the low mean age (0.7 years, range 0.1–3.9).
The Dutch Guidelines recommend that contralateral exploration should not be performed routinely but can be considered in patients with a high risk of double-sided hernia (prematures, children with VP drainage), a high risk of strangulation, or a high risk of general anaesthesia (prematures) [1].
A wide variety of operating techniques were used in 3284 adult patients. A mesh-based technique was used in 78% of the operations. This percentage is in concordance with data reported from other countries [4, 5, 6]. Because the Guidelines recommend a mesh technique (preferably Lichtenstein) in all adults, it is assumed that there will be a decrease in the variety of techniques used and an increase in the number of operations performed with the use of a mesh technique.
In recent years many articles have discussed the treatment of inguinal hernia repair [7, 8, 9, 10]. One cannot expect that all surgeons are up-to-date with details from all studies, but it is remarkable to see that 7.2% of operations are still performed using the Bassini technique, which was demonstrated to be inferior to the Shouldice technique as far back as 1996 [11].
Furthermore, there is a significant difference in frequency of use of mesh techniques by teaching hospitals and non-teaching hospitals (83.5% versus 73.8%, p<0.01). Moreover, the endoscopic techniques are also performed more often in teaching hospitals (303/1602, 18.9%) than in non-teaching hospitals (182/1990, 9.1%), p<0.01. This suggests, as one may expect, that more attention is paid to new developments in inguinal hernia treatment in teaching hospitals.
The guidelines recommend ambulatory care surgery for every patient, as it is as safe and effective as admission, but less expensive [12, 13]. The vast majority of patients in this study were still admitted into the hospital (63.6%). This is an opportunity for improvement. It has been shown in the literature that even a selected group of older patients and patients with ASA III can be operated on in ambulatory care surgery [14, 15, 16]. In some countries 80% of patients are treated on an ambulatory basis, which is probably related to reimbursement policies. In The Netherlands in 2001 there was no real incentive to perform an inguinal hernia repair in day-care due to reimbursement [17].
An important objective of the guidelines is to reduce the number of recurrences. The percentage of patients treated for recurrent hernia in this study is 13.3%. This is in line with data from Denmark, but higher than data from Scotland, countries in which comparable studies have been performed [4, 5]. It has to be taken into account that these percentages only reflect operated recurrent hernias, whereas many patients with asymptomatic recurrences may not have undergone surgery.
No technique is perfect, as demonstrated by the 78 patients with a recurrence after mesh repair. Since just how many patients per technique were at risk of recurrence is unknown, it is difficult to draw conclusions; however, it is a fact that recurrences occur with all techniques [18].
The Guidelines recommend that the use of local anaesthesia in patients with a primary unilateral hernia should be considered [1]. In this study, only 6.9% of the patients underwent surgery under local anaesthesia. In most cases this concerned patients with high comorbidity. The preference and the experience of the surgeon with local anaesthesia is an important factor in the decision to use local anaesthesia. Studies have shown no difference in economics and patient recovery after local or general anaesthesia [19].
Despite the fact that this was a retrospective study, with the risk of underestimation, the total percentage of complications was high (22.3%). The percentage of pain reports was 8.6% in the follow-up. 1.7% of patients suffered from pain after three months or more. These percentages are low compared to studies in which prospective questionnaires were used [20, 21], probably demonstrating the drawback of retrospective studies.
It is worrying that 2.2% of patients developed a recurrence within one year. No significant differences can be found in operational techniques, levels of surgical expertise, or the types of hospital between this and non-recurrent patients.
Surprisingly, two of the three reported bowel perforations were caused by an anterior technique. This only occurred in an endoscopic procedure once. Bladder perforation occurred only once after a Lichtenstein procedure and never occurred after an endoscopic correction, even though this complication has been feared when performing this technique.
Despite the fact that the results may be subject to bias, as it is a retrospective analysis of patient charts, it generates a large amount of reliable information and good insights into the practice of inguinal hernia surgery in a recent period.
Conclusion
Before implementation of the Dutch evidence-based guidelines for treatment of inguinal hernia, 2839 (78%) adult patients were treated with mesh repair and 484 (13.3%) patients were treated for a recurrent hernia. Implementation of the evidence-based Guidelines for inguinal hernia will hopefully demonstrate an improvement in patient care, with more use of mesh techniques (resulting in a lower recurrence rate) and more use of day surgery and local anaesthesia (resulting in more cost-effectiveness and safety).
References
Association of Surgeons of the Netherlands (2003) Dutch guidelines for inguinal hernia. Van Zuiden Communications BV, Alphen
Simons MP, de Lange D, Beets GL, van Geldere D, Heij HA, Go PM (2003) The ‘Inguinal Hernia’ guideline of the Association of Surgeons of the Netherlands. Ned Tijdschr Geneeskd 147:2111–2117
Burd RS, Heffington SH, Teague JL (2001) The optimal approach for management of metachronous hernias in children: a decision analysis. J Pediatr Surg. 36:1190–1195
Bay-Nielsen M, Kehlet H, Strand L, Malmstrom J, Andersen FH, Wara P, Juul P, Callesen T (2001) Quality assessment of 26,304 herniorrhaphies in Denmark: a prospective nationwide study. Lancet 358:1124–1128
Hair A, Duffy K, McLean J, Taylor S, Smith H, Walker A, MacIntyre IM, O’Dwyer PJ (2000) Groin hernia repair in Scotland. Br J Surg 87:1722–1726
Nilsson E, Haapaniemi S, Gruber G, Sandblom G (1998) Methods of repair and risk for reoperation in Swedish hernia surgery from 1992 to 1996. Br J Surg 85:1686–1691
Grant AM (2002) Open mesh versus non-mesh repair of groin hernia: meta-analysis of randomised trials based on individual patient data Hernia 6:130–136
Grant AM (2002) Laparoscopic versus open groin hernia repair: meta-analysis of randomised trials based on individual patient data. Hernia 6:2–10
Collaboration EH (2000) Mesh compared with non-mesh methods of open groin hernia repair: systematic review of randomized controlled trials. Br J Surg 87:854–859
EU Hernia Trialists Collaboration (2002) Repair of groin hernia with synthetic mesh: meta-analysis of randomized controlled trials. Ann Surg 235:322–332
Simons MP, Kleijnen J, van Geldere D, Hoitsma HF, Obertop H (1996) Role of the Shouldice technique in inguinal hernia repair: a systematic review of controlled trials and a meta-analysis. Br J Surg 83:734–738
Mitchell JB, Harrow B (1977) Costs and outcomes of inpatient versus outpatient hernia repair. Am J Surg 133:146–148
Ruckley CV, Cuthbertson C, Fenwick N, Prescott RJ, Garraway WM (1978) Day care after operations for hernia or varicose veins: a controlled trial. Br J Surg 65:456–459
Davies KE, Houghton K, Montgomery JE (2001) Obesity and day-case surgery. Anaesthesia 56:1112–1115
Jarret PE (2001) Day care surgery. Eur J Anaesthiol 23:32–35
Prabhu A, Chung F (2001) Anaesthetic strategies towards developments in day care surgery. Eur J Anaesthesiol 23:36–42
Go PM (2003) Laparoscopic cholecystectomy in day care; implementation of a guideline for clinical practice. Ned Tijdschr Geneeskd 147:1335–1336
Neumayer L, Giobbie-Hurder A, Jonasson O, Fitzgibbons R, Jr., Dunlop D, Gibbs J, Reda D, Henderson W (2004) Open mesh versus laparoscopic mesh repair of inguinal hernia. N Engl J Med 350:1819–1827
O’Dwyer PJ, Serpell MG, Millar K, Paterson C, Young D, Hair A, Courtney CA, Horgan P, Kumar S, Walker A, Ford I (2003) Local or general anesthesia for open hernia repair: a randomized trial. Ann Surg 237:574–579
Courtney CA, Duffy K, Serpell MG, O’Dwyer PJ (2002) Outcome of patients with severe chronic pain following repair of groin hernia. Br J Surg 89:1310–1314
Page B, Paterson C, Young D, O’Dwyer PJ (2002) Pain from primary inguinal hernia and the effect of repair on pain. Br J Surg 89:1315–1318
Acknowledgements
The authors would like to thank all personnel of the participating hospitals for their cooperation in this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
de Lange, D.H., Aufenacker, T.J., Roest, M. et al. Inguinal hernia surgery in The Netherlands: a baseline study before the introduction of the Dutch Guidelines. Hernia 9, 172–177 (2005). https://doi.org/10.1007/s10029-005-0317-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-005-0317-y