Abstract
Purpose
The incidence of chronic groin pain (CGP) and its impact on quality of life (QoL) after hernia repair are not clear with follow-up either being short or retrospective. We present 10-year prospective follow-up of a randomized trial for bilateral and recurrent hernia repair focusing on CGP and its impact on QoL.
Methods
Patients enrolled between 1997 and 2000 were contacted by telephone and asked about the presence of CGP. Those patients with CGP were sent two validated questionnaires: a SF-12v2 Health Survey and a Pain Impact Questionnaire (PIQ-6) (QualityMetric, USA).
Results
One hundred and twenty patients were recruited into the original study, and of these, 14 complained of CGP and were sent a PIQ-6 and a SF-12 v2 health survey. Overall, there was a higher incidence of CGP in the laparoscopic group compared with the open group (15 vs. 8 %, ns), but the severity of the pain in the laparoscopic group was less (2 vs. 3.5, p = 0.0558). QoL was significantly reduced in patients with CGP compared with the US norm. The laparoscopic group scored higher in 5 out of 8 of the QoL categories compared with the open group, but this was not significant. Overall age-adjusted scores revealed those under 65 years of age felt they had poorer physical health, and this reduced their QoL compared to normal values.
Conclusion
CGP following laparoscopic surgery for inguinal hernia repair is less severe than open repair, but this does not translate into a significant improvement in QoLin this study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With the advent of prosthetic meshes, recurrence following hernia repair has significantly improved. Rates are reported from 0 to 5 % [1] depending on the length of follow-up with no comparable difference between laparoscopic and open repair [1, 2]. Focus has now turned to chronic groin pain (CGP) that has become clinically more important with the reduction in recurrence rates. The incidence of CGP 3 months after surgery has been reported in 33 % of patients [3], and this continues to persist at 1 year with a resultant decrease in QoL [4]. Laparoscopic repair results in lower postoperative pain, and an earlier return to work compared to open repair [5, 6] in the first year after surgery with follow-up in comparative studies rarely exceeding 3 years. We therefore present 10-year prospective follow-up of our randomized trial that compared TAPP and open (mesh) repair for bilateral and recurrent inguinal hernia focusing on the incidence of CGP and its impact on QoL.
Materials and methods
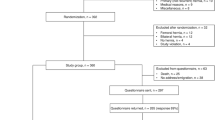
Between 1997 and 2000, 120 patients were enrolled and randomized to either TAPP or open repair, and the short-term results have been previously published [6]. In 2010, all patients were followed up. Twenty-eight patients were deceased from unrelated causes. Sixty-three patients were contacted by telephone and asked about the presence of CGP, hernia recurrence and revisional surgery as appropriate. Twenty-nine patients could not be contacted by telephone and underwent a full review of their medical notes (Fig. 1). Of the 62 patients who were contacted by telephone, 14 complained of CGP and were sent two validated questionnaires, SF-12v2™ Health Survey and Pain Impact Questionnaire, PIQ-6™ (QualityMetric, USA) [7].
Statistical analysis was undertaken using a Fisher’s exact test or a paired t test as appropriate.
Results
Laparoscopic versus open repair (Fig. 1)
The median age of the laparoscopic group at the time of operation was 61.5 years (range 20–80 years; IQR 51.7–67.5) compared with the open group of 61 years (range 25–88 years; IQR 52–74). There was a significantly higher mortality rate in the open group compared with the laparoscopic group (8/60 vs. 20/60, p = 0.0166). The recurrence rate was 7 % in the TAPP group and 8 % in the open group. The overall incidence of CGP at 10 years was 12 %, but this was higher in the laparoscopic group (15 vs. 8 % ns).
Primary versus recurrent inguinal hernia (Fig. 2)
There was a 2:1 ratio of patients who had a primary bilateral hernia compared with recurrent hernia. There was no significant difference between the rate of recurrence or incidence of CGP between the two groups in the follow-up period.
Interpretation of those patients with chronic groin pain
Fourteen patients complained of CGP at telephone follow-up, and 13 of these (93 %) returned their health surveys. Three patients (33 %) in the laparoscopic group and 2 patients (50 %) in the open group attended the chronic pain clinic during the 10-year follow-up period (Table 1).
Pain scores: PIQ-6
The results of the pain severity score (scored from 0 to 5, 0 = none, 5 = very severe) and the PIQ SUM scores are summarized in Tables 1 and 2. The mean pain severity score for the laparoscopic group was 2 compared with 3.5 in the open group but this was not significant (p = 0.0558). Interestingly, four patients in the TAPP group registered no pain at all in the previous 4 weeks, and a further three had only mild pain. This is in contrast to the open group who all rated their pain as mild or moderate.
The mean PIQ-6 SUM score (Table 2) was 53 ± 11 for the group as a whole, 51 ± 12 for the laparoscopic group and 56 ± 7 for the open group (p = 0.4). There were four patients of working age (<65 years), and their pain scores were not significantly different than those over 65 years.
Quality of life: SF-12 v2
In patients with CGP, the QoL was significantly reduced compared with the US norm in all categories of the SF12 v2 except vitality (Table 3). There was however no significant difference between the mean scores for each category in patients who underwent laparoscopic repair compared with open repair (Table 4). Overall, for each category, the mean score was less than 50, that is, less than the norm for the US population. Of the physical component summary (PCS) scores, 15 % were above the norm and 38 % were below (Fig. 3). Of the mental component summary (MCS) scores, 23 % were above the norm, and the 46 % were below the norm (Fig. 4). Of the population, 30 % were at risk for depression compared with the norm of the 20 % in the general population in the US.
In the laparoscopic group, 22 % of patient scores were above the norm for PCS score and 33 % were below the norm compared with 0 % above and 50 % below in the open group (Fig. 3). For the MCS score, 33 % of patient scores were above the norm and 33 % were below the norm in the laparoscopic group compared with 0 % above and 25 % below in the open group (Fig. 4).
When adjusted for age, those under the age of 65 had a lower PCS compared with the US norm (mean score of 44.6, expected norm of 48.78), while those over 65 had a greater PCS compared with the norm (mean score of 42.43, expected norm of 41.14). This difference was not significant. There was no correlation between age and MCS (Table 5).
Discussion
Ten years after surgery for recurrent or bilateral hernias, the incidence of CGP was 12 %. The incidence of pain after TAPP was higher, but the severity of pain in this group was less compared with the open group (p = 0.0558). Overall QoL was significantly reduced in those patients with CGP compared with the US norm, and while this was less so in the laparoscopic group, this difference was not significant. The physical aspect of the QoL score (PCS) was lower than the norm in the under 65 s but higher in the over 65 s.
This is a prospective follow-up study, of at least 10 years, of a randomized controlled trial. There is no recall bias, and therefore, the estimation of CGP is likely to be reliable in those who were contacted. However, just under 50 % of the patients could not be followed up prospectively since they had either died or were lost to follow-up, and therefore, a full-note review was undertaken. Although there was no evidence in the notes that these patients suffered with CGP, it is well known that pain is often underreported [4]. This would increase the incidence of pain in both groups but particularly the open group which had a greater number of deceased or lost-to-follow-up patients (Fig. 1).
The incidence of CGP contradicts the results of our original study where 13 % of those patients who had an open repair had CGP at 3 months compared with only 1 % in the laparoscopic group. This increase in pain at 3 months following open repair is well documented and an advantage of laparoscopic repair. The high incidence of CGP in this follow-up study is similar to the published literature that reports CGP as high as 30 % following open mesh repair and 20 % following laparoscopic repair at 5 years [8, 9]. The results of Grant et al. [9] demonstrated that the incidence of pain at 1 year was greater in the open group compared with laparoscopic group, but at 5-year follow-up period, the incidence of pain in both groups was equal. The results of this study show that the incidence of CGP persists even at 10 years and is equal but unlike the study by Grant showed that the severity of the pain was less in the laparoscopic group in keeping with the study by Eklund et al. [8]. There was no statistical difference in the severity of pain but the high mortality rate among the open group may explain this as the incidence and in turn the severity of pain could have been underestimated.
Despite a lower severity of pain in laparoscopic group, this did not translate into a better QoL in this study. CGP at 3 months after hernia repair has been shown to impact significantly on QoL [3] with higher QoL scores after laparoscopic repair in the initial postoperative period [10, 11]. However, there is debate as to whether this benefit persists after the first year. Retrospective analysis of 216 patients who underwent open or laparoscopic repair using a Short-Form 36 (SF-36) demonstrated no statistical difference in QoL scores between the two groups, but those who had a TAPP reported better physical function with less fatigue and energy [12]. Myers et al. [13] prospectively assessed the QoL of patients undergoing a TEP or open repair with a median follow-up of 32 months. They reported that the QoL scores were significantly better in 5 of 8 categories of the SF-36 and that overall physical and mental scores were significantly better in the TEP group. The results of this study suggest that these benefits are lost by 10 years, and while the QoL scores were better in five of the eight categories who had a TAPP, they were not significant. Overall, the PCS and MCS were better in the laparoscopic group, but these were not significant. The PCS was reduced in the under 65 s compared with the expected norm despite there being no difference in the SUM pain scores between the over and under 65 s. This suggests that the presence of CGP detrimentally affects the young more significantly and supports the results of Bay-Nielsen et al. [4] who demonstrated that CGP was higher and QoL lower in the under 65 s following hernia repair.
Conclusion
The incidence of CGP was 12 % at 10 years with no statistical difference between laparoscopic and open repair. However, the severity of the pain was less in the laparoscopic group. This CGP has a significant impact on QoL in both groups but more so in the under 65 s whose CGP restricts physical activity more than the over 65 s.
Patients should be counseled on the persistence of CGP following hernia repair and that this may impact detrimentally on their QoL but especially those under 65 years of age. However, further studies of long-term follow-up are needed to assess the impact of CGP on QoL to determine whether one mode of repair is significantly better.
References
Butters M, Redecke J, Koninger J (2007) Long-term results of a randomised clinical trial of Shouldice, Lichenstein and transabdominal peritoneal hernia repairs. Br J Surg 94:562–565
Bittner R, Sauerland S, Schmedt CG (2005) Comparison of endoscopic techniques vs. Shouldice and other open nonmesh techniques for inguinal hernia repair. Surg Endosc 19:605–615
Courtney CA, Duffy K, Serpell MG, O’Dwyer PJ (2002) Outcome of patients with severe chronic pain following repair of groin hernia. Br J Surg 89:1310–1314
Bay-Nielsen M, Perkins FM, Kehlet H (2001) Pain and functional impairment 1 year after inguinal herniorrhaphy: a nationwide questionnaire study. Ann Surg 233:1–7
Schmedt CG, Sauerland S, Bittner R (2005) Comparison of endoscopic procedures vs. Lichtenstein and other open mesh techniques for inguinal hernia repair. Surg Endosc 19:188–199
Mahon D, Decadt B, Rhodes M (2003) Prospective randomized trial of laparoscopic (transabdominal preperitoneal) vs. open (mesh) repair for bilateral and recurrent inguinal hernia. Surg Endosc 17(9):1386–1390
Becker J, Schwartz C, Saris-Baglama RN et al (2007) Using item response theory (IRT) for developing and evaluating the pain impact questionnaire (PIQ-6TM). Pain Med 8(S3):S129–S144
Eklund A, Rudberg C, Leijonmarck C-E, Rasmussen I, Spangen L, Wickbom G, Wingren U, Montgomery A (2007) Recurrent inguinal hernia: randomized multicenter trial comparing laparoscopic and Lichenstein repair. Surg Endosc 21:634–640
Grant A, Scott N, O’Dwyer P (2004) Five-year follow-up of a randomized trial to assess pain and numbness after laparoscopic or open repair of groin hernia. Br J Surg 91:1570–1574
Wellwood J, Sculpher M, Stoker D et al (1998) Randomised controlled trial of laparoscopic versus open inguinal hernia mesh repair: outcome and cost. BMJ 317:103–110
Lawrence K, McWhinnie D, Jenkinson C et al (1997) Quality of life in patients undergoing inguinal hernia repair. Ann R Coll Surg Engl 79(1):40–45
Srsen D, Druzijanic N, Pogorelic Z, Perko Z, Juricic J, Kraljevic D, Krnic D, Bilan K, Mimica Z (2008) Quality of life analysis after open and laparoscopic inguinal hernia repair—retrospective study. Hepatogastroenterology 55:2112–2115
Myers E, Browne K, Kavanagh D, Hurley M (2010) Laparoscopic (TEP) versus Lichtenstein inguinal hernia repair: a comparison of quality-of-life outcomes. World J Surg 34:3059–3064
Conflict of interest
Drs. Bignell, Partridge, Mahon and Rhodes have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bignell, M., Partridge, G., Mahon, D. et al. Prospective randomized trial of laparoscopic (transabdominal preperitoneal-TAPP) versus open (mesh) repair for bilateral and recurrent inguinal hernia: incidence of chronic groin pain and impact on quality of life: results of 10 year follow-up. Hernia 16, 635–640 (2012). https://doi.org/10.1007/s10029-012-0940-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-012-0940-3