Abstract
Introduction
Spigelian Hernia (SH) is a rare ventral hernia with a high incarceration and obstruction risk. The purpose of this study is to present our experience in diagnosis and treatment of this rare hernia entity.
Materials and Method
Sixteen patients underwent surgery for SH between 2000 and 2010. Analysis parameters included demographic data, location of defect, diagnostic methods, mode of surgery, mode of anesthesia and postoperative outcome.
Results
Mean follow-up was 98 months. The gender bias was 37.5 %: 62.5 % (man: woman) with mean age of 56 years. The SH was right-sided in 56.25 %, left-sided in 37.5 % and bilateral in 6.25 % of the cases. The preoperative diagnosis was correct in 25 % of the cases. Eight patients (50 %) underwent elective surgery, and the other 8 patients (50 %) underwent surgical treatment on emergency basis. Two patients underwent open hernia repair by primary suture, 13 patients underwent open mesh repair and one patient underwent a laparoscopic mesh repair. Neither a major hernia repair-related complication nor mortality could be registered.
Conclusion
SH is a rare entity with a wide clinical spectrum and difficulties in preoperative diagnosis. Once the diagnosis of SH is established, a surgical treatment is indicated because of the high complication risk.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
SH was named after Adrian van der Spieghel, who first described the semilunar line. SH is defined as a hernia occurring through the spigelian aponeurosis [1]. The spigelian aponeurosis is formed by the fusion of the aponeurosis of internal oblique muscle and of transversus abdominis muscle. The margins of spigelian aponeurosis are formed by the linea semilunaris and the lateral edge of the rectus muscle. It extends from the costal cartilage of the 8th rib to symphysis pubis [1–3]. In the upper abdominal wall, the spigelian aponeurosis is posterior to the rectus muscle, making the clinical diagnosis of fascia defects extremely difficult. Beneath the umbilical region, the aponeurosis forms a weak barrier that is susceptible to protruding peritoneal sacs or extraperitoneal fat [1, 3–5]. SH is a rare entity with a reported incidence of 0.12–2 % of all abdominal wall hernias and was first described by Klinklosch in 1764. More than half of all spigelian hernias are located in a 6 cm wide region distal to the umbilicus and above the inferior epigastric vessels. This region is referred as “spigelian hernia belt” [1, 2]. The most common symptom of spigelian hernia is pain due to contraction of the abdominal musculature. A further symptom is a palpable mass in 35 % of cases [6–16].
Predisposing factors are collagen disorders, age, obesity, rapid weight loss, multiple pregnancies, chronic pulmonary diseases, trauma, iatrogenic causes and congenital disorders [3, 10, 17]. Ultrasonography (US) of the abdomen and computed tomography (CT) are the most sensitive diagnostic tools for characterizing a SH [11, 13]. Once SH is diagnosed, there is the need for surgical treatment, because of the high risk for serious complications, such as incarceration, obstruction and strangulation of the protruding structures [11, 15]. Emergency surgery is estimated to be performed in 21–33 % of the cases, due to incarceration and strangulation of hernia content [2, 9–11, 15].
Here we report our single center experience in the surgical treatment of SH, including patients who underwent elective surgical treatment or emergency surgery. Our aim was to review the long-term outcome of these patients, mode of surgery, morbidity, mortality and the sensitivity of diagnostic methods.
Patients and methods
Study population
Between January 2000 and December 2010, 16 patients with 17 SH referred to the Surgical Department of the General Hospital of Western Attica. These patients were identified from a prospective database and were retrospectively analyzed. We analyzed the demographic data, site of the defect, diagnostic methods, mode of surgical treatment, long-term outcome and postoperative complications.
Demographic parameters and diagnostic imaging
Mean patient age was 56 years (range: 28–83). Of 16 patients, 10 (62.5 %) were women. The diagnostic workup included US and in 1 case contrast-enhanced CT. In 9 patients, the SH was right-sided (56.25 %), in 6 patients (37.5 %) left-sided and in 1 patient bilateral (Table 1). In all patients “real” spigelian hernias have been diagnosed, and in none of them there was the possibility to confuse it with an incisional hernia.
Surgical procedures and mode of anesthesia
In all patients, the indication for surgical treatment was given. Either an open or laparoscopic hernia repair was performed. Fifty percent of the patients (n = 8) underwent elective surgical treatment and 8 patients emergency surgery (Table 2).
Six patients (37.5 %) underwent surgery under spinal anesthesia and 10 patients (62.5 %) under general anesthesia (Table 2).
The parameters assessed were blood loss in the perioperative phase, early postoperative course, surgical and non-surgical complications, mortality, length of stay in the hospital and the relief of symptoms after surgical treatment. Postoperative mortality and morbidity were assessed up to 3 months post-surgery.
Results
We recorded two main clinical symptoms: abdominal discomfort or pain in 9 patients (56.25 %), a palpable mass in 4 patients (25 %) and a combination of both (abdominal pain, palpable mass) in 3 patients (18.75 %) (Tables 1, 2).
Preoperative diagnosis was established correctly in 4 patients (25 %): in 3 patients by physical examination and US and in one patient by physical examination and CT scan (Figs 1, 2), while in 12 patients the diagnosis of SH was established during surgery (75 %). These patients presented with acute abdominal pain, nausea and the clinical situation of an obstruction with ileus (n = 8) and/or a palpable mass (n = 4). The low sensitivity of the US examination was mostly dependent on the clinical situation of the patients, which could not be sufficiently examined because of pain (n = 8). Due to the clinical symptoms of the patients, we had to abandon a laparoscopic procedure, and we preferred a conventional operative treatment.
Sixteen patients with 17 SH underwent surgical treatment in our department, eight patients with 9 SH (50 %) underwent elective surgery, and 8 patients (50 %) were operated on emergency basis. All patients underwent emergency surgery had an incarcerated SH, and in one patient, a strangulation of colon was diagnosed additionally (Fig. 3). This patient was referred to our department with large bowel ileus and a painful mass in the right lower abdominal quadrant. During surgery, strangulation with necrosis of cecum, terminal ileum and ascending colon was diagnosed. Except for hernia repair, we performed an extended right colectomy.
Open primary suture repair was performed in 2 patients (12.5 %), open preperitoneal mesh repair in 13 patients (81.25 %) according to our technique using PHS (Prolene Hernia system) [18] (Fig. 4) and laparoscopic mesh repair in 1 patient (6.25 %) (Table 2).
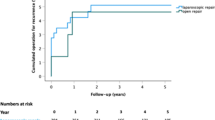
Patient follow-up as of December 2010 or till time of death ranged from 0 to 120 months, with a median follow-up of 102 months (mean = 98 months). None of the patients was lost from follow-up, which included a clinical examination. We abandoned an US control examination because all patients underwent surgery (n = 16) reported symptom relief after treatment.
There was no peri- or postoperative mortality in our study. Postoperative complications were recorded in 2 (12.5 %) patients. Two patients had seroma, and in one patient, pneumonia was registered additionally. Both patients had an open hernia repair (open primary suture repair in 1 patient and open mesh repair in 1 patient) and underwent a successful conservative treatment. Neither a blood loss over 200 ml nor a recurrence was registered.
Mean hospital stay was 3.5 days (range 1–9 days). Five (31.5 %) patients died during follow-up due to a concomitant malignant disease (n = 2) or cardiovascular disease (n = 3). No hernia-repair-related major complication was recorded in any patient (Table 2).
Discussion
SH is defined as the protrusion of preperitoneal fat or a peritoneal sac, with or without an organ, across a congenital or acquired defect in the spigelian line. It is also known as “lateral ventral hernia,” “anterolateral hernia” or “hernia through the conjoint tendon” [2–4]. It is an acquired type of hernia in most cases and occurs mainly in adults between 40 and 70 years, affecting both men and women and sides (left, right) equally. In infants and children, the defect is congenital. Previous studies presented a total number of approximately 900 reported cases worldwide [8]. A review study reported 159 articles, 479 cases and 19 series with more than 5 patients [13].
The most common symptoms of SH are abdominal pain and the occurrence of a painful mass [9]. Diagnosis of SH is difficult because of: the nonspecific variety of symptoms, their small size, the intramural location between different muscle layers and the low sensitivity of clinical examination and common diagnostic tools [5]. Physical examination alone fails to establish the diagnosis in more than 50 % of cases [10]. However, Larson et al. [11] reported that history and physical examination alone could establish the diagnosis of SH in 74 % of cases. In differential, diagnosis must be mainly concern of rectus sheath hematoma, abdominal abscess and seroma. Less common are other entities as fibroma, lipoma, sarcoma and hemangioma of abdominal wall. Many authors reported that SH may remain undiagnosed until emergency surgery is performed. Weiss et al. reported in a series of 178 patients that the diagnosis was established correctly in the preoperative phase in 92 cases (51.7 %) [5, 12]. In our series 50 % of patients underwent emergency surgery and the preoperative diagnosis was established correctly in only 4 patients (25 %).
The diameter of the hernia neck is usually approximately 0.5–2 cm, and this leads to an obstruction and incarceration of the hernia content in 21 % of the cases [3, 13].The hernia sac usually contains the greater omentum [14] and in rare cases segments of the small bowel [15–17], of the colon [19, 20], the appendix [21–23], bladder [24], stomach, gallbladder, Meckel diverticulum, ovaries and testes [5]. Some authors reported patients having SH on both sides. [25–28]. According to our series, 1 patient had a bilateral SH diagnosed and underwent an open preperitoneal mesh repair. Furthermore, 9 patients (56 %) showed an incarceration of greater omentum; an incarceration of small bowel or other organs was registered in 4 patients (25 %).
Plain abdominal X-ray examinations may show signs of an ileus in cases, where an incarceration of bowel is present. High resolution US, combined with Valsalva maneuver, especially in obese patients may help in diagnosis of SH [5, 29–31]. CT is the diagnostic tool with the highest sensitivity [32, 33].
Once the diagnosis SH is established, there is the need for surgical treatment because of the high risk of complications [34–38].The percentage of emergency operation is estimated to be 21–33 % due to incarceration and strangulation [3, 5, 12, 13, 36]. The surgical options for repair of SH vary from the open hernia repair (primary suture repair, mesh repair preperitoneal or intraperitoneal) to the laparoscopic hernia repair. Open procedures are still widely used due to the high rate of emergency surgery [11, 17].
Generally, repair of SH consists of open anterior herniorrhaphy using direct muscle approximation or mesh placement [1]. As far as the open mesh repair is concerned, there is the possibility of either intraperitoneal or extraperitoneal technique, where the intraperitoneal mesh repair has the risk of formation of adhesions and/or fistulas [38]. Recently several authors reported their experience in SH repair through preperitoneal placement of PHS (Prolene Hernia System) mesh in 1 day cases [18, 39, 40]. During the last years, the laparoscopic intraperitoneal mesh repair of SH has improved considerably and has become a major alternative to conventional methods [13, 35, 41–43]. The main problem remains the formation of adhesions and fistulas that mainly depends on the nature of the mesh being placed. The laparoscopic transabdominal suture repair of SH has been also reported [44]. An alternative to this procedure is the totally extraperitoneal laparoscopic mesh repair.
The hospital stay for patients underwent open surgical treatment is estimated to be 5 days, while the average length of hospital stay in patients underwent laparoscopic repair is reported to be 1 day. Best results seem to be offered after totally extraperitoneal laparoscopic approach [41]. In our series, we were not able to examine these parameters, as we performed a laparoscopic procedure in one patient. This patient had a hospital stay of 1 day and underwent a laparoscopic transabdominal mesh repair.
Furthermore, we marked a very low complication rate (11.8 %), although many patients underwent emergency surgery, in comparison to other studies, which reported a complication rate of 30 % [28]. This fact supports the opinion that elective and emergency surgery for rare and complicated hernia entities is safe and results in good long-term quality of life in experienced, high volume centers. Furthermore, the mean hospital stay was 3.5 days and was comparable to other studies. On the other side, we have to mark the very low sensitivity of US examination in our series, which has been the result of two parameters: very difficult conditions during examination (abdominal pain in emergency patients and obesity) in the most cases and low experienced radiologist.
One limitation of the present study is its retrospective nature. Nevertheless, the data reported included all patients that underwent elective and emergency surgery with no exclusions and underline the importance in favor of immediate surgery. Another limitation is that this study was performed in a single institution, and the results obtained might not be comparable to those in other centers. Unicentral studies, however, have the advantage of reducing the number of possible differences in surgical technique.
Conclusions
SH is a rare entity with difficulties in diagnosis, high risk of life threatening complications such as bowel incarceration or strangulation and a very wide clinical spectrum. Of great importance is the early establishment of diagnosis. Once the diagnosis established, the indication for immediate surgical treatment must be given. We believe that even in patients with an asymptomatic spigelian hernia, the indication for surgery should be given, because of the high risk of incarceration. Furthermore, advanced diagnostics are needed, in order to exclude the presence of bilateral SH.
Abbreviations
- SH:
-
Spigelian hernia
- CT:
-
Computed tomography
- U/S:
-
Ultrasound sonography
- ml:
-
Milliliter
- cm:
-
Centimeter
- PHS:
-
Prolene hernia system
References
Skandalakis PN, Zoras O, Skandalakis JE, Mirilas P (2006) Spigelian hernia: surgical anatomy, embryology and technique of repair. Am Surg 72(1):42–48
Spangen L (1976) Spigelian hernia. Acta Chir Scand Suppl 462:1–47
Montes IS, Deysine M (2003) Spigelian and other uncommon hernia repair. Surg Clin N Am 83:1235–1253
Olson RO, Davis WC (1968) Spigelian hernia: rare or obscure? Am J Surg 116:842–846
Spangen L (1989) Spigelian hernia. World J Surg 13:573–586
Broughton G, Alvarez JD (1997) Repair of a spigelian hernia. Am Coll Surg 185:508–509
Houlihan TJ (1976) A review of spigelian hernia. Am J Surg 131:734–735
Spangen L (1994) Spigelian hernia. In: Bendavid R (ed) Prostheses and abdominal wall hernias. R G Landes, Austin, p 563
Jain KM, Hestings OM, Kunz VP (1977) Spigelian hernia. Am Surg 43:569–600
Stirnemann H (1982) The Spigelian hernia: missed? Rare? Puzzling diagnosis? Chirurg 53:314–317
Larson DW, Farley DR (2002) Spigelian hernias: repair and outcome for 81 patients. World J Surg 26:1277–1281
Weiss Y, Lernau OZ, Nissen S (1974) Spigelian hernia. Ann Surg 180:567–572
Moreno-Egea A, Flores B, Girela E, Martin JG, Aguayo JL, Canteras M (2002) Spigelian hernia: Bibliographical study and presentation of a series of 28 patients. Hernia 6:167–170
Zacharakis E, Papadopoulos V, Ganidou M, Zacharakis E (2006) Incarcerated Spigelian hernia: a case report. Med Sci Mon 12(7):CS 64–CS 66
Baucom C, Nguyen QD, Hidalgo M, Slakey D (2009) Minimally invasive Spigelian hernia repair. JSLS 13:263–268
Tsalis K, Zacharakis E, Lambrou I, Betsis D (2004) Incarcerated small bowel in spigelian hernia. Hernia 8:384–386
Vos DI, Scheltinga MRM (2004) Incidence and outcome of surgical repair of spigelian hernia. Br J Surg 91:640–644
Perrakis E, Velimezis G, Vezakis A, Antoniades J, Savanis G, Patrikakos V (2003) A new tension-free technique for the repair of umbilical hernia, using the Prolene Hernia System–early results from 48 cases. Hernia 7(4):178–180
Topal E, Kaya E, Topal NB, Sahin I (2007) Giant spigelian hernia due to abdominal wall injury. Hernia 11:67–69
Miller R, Lifschitz O, Mavor E (2008) Incarcerated spigelian hernia mimicking colon carcinoma. Hernia 12(1):87–89
Thomasset SC, Villatoro E, Wood S, Martin A, Finlay K, Patterson JE (2010) An unusual Spigelian hernia involving the appendix: a case report. Cases J 3:22
Lin PH, Koffron AJ, Heilitzer TJ, Lujan HJ (2000) Right lower quadrant abdominal pain due to appendicitis and incarcerated spigelian hernia. Am Surg 66(8):725–727
Onal A, Sokmen S, Atila K (2003) Spigelian hernia associated with strangulation of the small bowel and appendix. Hernia 7:156–157
Scotte M, Majerus B, Sibert L, Teniere P (1991) Bladder incarceration in a Spigel hernia. J Chir (Paris) 128(2):74–75
Klimopoulos S, Kounoudes C, Vaidakis A, Galanis G (2001) Low spigelian hernias: experience of 26 consecutive cases in 24 patients. Eur J Surg 167:631–633
Safioleas M, Stamatakos M, Moustakakis K, Safioleas P, Skandalakis P (2007) Spigelian hernia. A rare case of bilateral hernia and presentation of our experience. Chirurgia (Bucur) 102(4):429–432
Ng JW (2004) A case of small spigelian hernias succesfully treated by a simple laparoscopy-assisted technique. Surg Laparosc Endosc Percutan Tech 14(5):300–303
Malazgirt Z, Topgul K, Sokmen S, Ersin S, Turkcapar AG, Gok H, Gonullu N, Paksoy M, Ertem M (2006) Spigelian hernias: a prospective analysis of baseline parameters and surgical outcome of 34 consecutive patients. Hernia 10:326–330
Torzilli G, Carmana G, Lumachi V (1995) The usefulness of ultrasonography in the diagnosis of the spigelian hernia. Int Surg 80:280–282
Fried AM, Meeker WR (1979) Incarcerated Spigelian hernia: ultrasonic differential diagnosis. Am J Roentgenol 133(1):107–110
Muffid MM, Abu-Yousef MM, Kakish ME, Urbaneta LF, Al-Jurf AS (1997) Spigelian hernia: diagnosis by high-resolution real-time sonography. J Ultrasound Med 16:183–187
Bennett D (2002) Incidence and management of primary abdominal wall hernias: unbilical, epigastric and spigelian. In: Fitzgibbons RJ, Greenburg AG (eds) Nyhous and Condon s hernia, 5th edn. Lippincot Williams and Wilkins, Philadelphia, pp 389–413
Balthazar EJ, Subramanyam BR (1983) Radiographic diagnosis of spigelian hernia. Am J Gastroenterol 78:525–528
Spangen L (1995) Spigelian hernia. In: Nyhous LM, Condon RE (eds) Nyhous and Condon s hernia, 4th edn. Lippincot, Phladelphia, pp 381–392
Nursal TZ, Kologlu M, Aran O (1997) Spigelian hernia presenting as an incarcerated incisional hernia. Hernia 1:149–150
Rogers FB, Camp PC (2001) A strangulated spigelian hernia mimicking diverticulitis. Hernia 5:51–52
Artioukh DY, Walker SJ (1996) Spigelian hernia: presentation, diagnosis and treatment. J R Coll Surg Edinb 441:241–243
Malazgirt Z, Dervisoglu A, Polat C, Guneren H, Akpolat T (2003) Preperitoneal mesh repair of spigelian hernias under local anesthesia: description and clinical evaluation of a new technique. Hernia 7:202–205
Licheri S, Pisano G, Pintus M, Erdas E, Martinasco L, Pomata M, Daniele GM (2004) The treatment of Spigelian hernia with the Prolene Hernia System: notes on techniques. Chir Ital 56(2):265270
Campanelli G, Pettinari D, Nicolosi FM, Avesani EC (2005) Spigelian hernia. Hernia 9(1):3–5
Moreno-Egea A, Carrasco L, Girela E, Martin JG, Aguayo JL, Canteras M (2002) Open vs laparoscopic repair of spigelian hernia. Arch Surg 137:1266–1268
Palavinelu C, Vijaykumar M, Jani KV, Rajan PS, Maheshkmaar GS, Rajapandian S (2006) Laparoscopic transabdominal preperitoneal repair of spigelian hernia. JSLS 10:193–198
Louring-Andersen M, Hjiorne FP, Skovdal J, Bisgaard T (2009) Diagnosis and treatment of Spigelian hernia. Ugeskr Laeger 23:171(48):3518–3522.
Bittner JG 4th, Edwards MA, Shah MB, MacFadyen BV, Mellinger JD (2008) Mesh-free laparoscopic spigelian hernia repair. Am Surg 74(8):713–720
Conflict of interests
All authors declare no conflict of interests.
Author information
Authors and Affiliations
Corresponding author
Additional information
A. Perrakis and G. Velimezis contributed equally to this work.
Rights and permissions
About this article
Cite this article
Perrakis, A., Velimezis, G., Kapogiannatos, G. et al. Spigel hernia: a single center experience in a rare hernia entity. Hernia 16, 439–444 (2012). https://doi.org/10.1007/s10029-012-0925-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-012-0925-2