Abstract
Purpose
Late-onset mesh infection, occurring months to years following hernia repair, is a rare complication of hernia surgery. Its management usually requires removal of the mesh. The aim of this paper was to assess the rate of recurrence of inguinal herniae following removal of the mesh for late onset deep mesh infection.
Methods
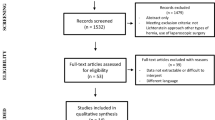
We performed a literature review to assess the rate of recurrence of herniae following the removal of a delayed onset infected mesh. Relevant studies from January 1966 to June 2010 were identified from a Medline, Pub Med, Embase, Scopus and Cochrane database search. Studies that reported recurrence of the hernia following removal of delayed onset infected meshes were included. Results were tabulated and analysed to derive conclusions.
Results
Some 153 abstracts were reviewed and 12 potential studies initially identified; of these, only 7 were finally included in this review. The included studies were six case series and one case report and comprised a total of 40 patients in whom delayed-onset infected mesh was removed. The median follow-up period after the removal of the infected mesh was 26 months. Of these 40 patients, only 2 (<5%) developed a recurrent hernia. Removal of the mesh resulted in resolution of symptoms in the majority of the patients.
Conclusion
Based on this review, removal of a late-onset infected mesh results in resolution of symptoms in the majority of cases, whereas recurrence of hernia is not common. However, further research is required as the number of patients in our review is relatively small.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tension free hernia repair using prosthetic meshes is the commonest procedure performed for inguinal hernias these days. This is because of its relative ease and low recurrence rates [1]. It has been endorsed by constituted bodies such as the European Hernia Society (EHS) as being the method of choice for open adult hernia repair because it is associated with minimal peri-operative morbidity, can be performed as a day-case procedure and has an overall recurrence rate of less than 4% [2]. Postoperative complications include superficial wound infection with an incidence between 2.88% and 4.37% [3]. This is usually not related to the prosthetic material [1, 3] and can be resolved by using appropriate antibiotics although in some cases incision and drainage of any collections may be required [4]. Early post operative mesh infection, defined as infection of the mesh occurring within a few days to weeks postoperatively, may occur despite the judicious use of prophylactic antibiotics [3, 4] in up to 1.7% of cases [5]. However, rarely, the mesh may become infected months or even years after the original surgery.
Late-onset deep seated prosthetic mesh infection is deleterious and requires removal of mesh in most cases [1, 3, 6]. The reported incidence of deep infection varies in different case series and ranges from 0.03% to 1.4% [1, 3]. Whereas early postoperative mesh infection is considered to be caused by contamination, the reasons behind delayed onset mesh infection are not clear [4]. Meshes incite a foreign body reaction and cause TNF-α induced inflammation and leukocyte chemotaxis [7]. Inflammatory cells are gradually replaced by fibroblasts and giant cells [8], which are prone to attachment by surrounding bacteria [7, 8]. However, commonly used prolene meshes incite only a mild leukocyte-endothelial reaction and hence mesh-induced bacterial adherence to the implantation site is not thought to be the likely reason behind late-onset mesh infection [7]. Moreover, prevention of late-onset deep infection of the mesh with bacteriostatic agents such as cyanoacylates has not shown any beneficial effects in in vitro studies [8]. Late-onset deep seated prosthetic mesh infection presents as chronic groin pain, swelling, low grade sepsis and, in extreme cases, a discharging sinus [3, 6]. Initial management with antibiotics may not resolve the symptoms and removal of the infected mesh is usually necessary to alleviate chronic sepsis [9].
The aim of this study was to determine the incidence of inguinal hernia recurrence following removal of mesh in patients with late-onset deep seated mesh infection. In addition, long-term symptom resolution following removal of mesh was studied.
Methods
We performed a literature review to assess the rate of recurrence of hernia following removal of a late onset infected mesh. Relevant studies from January 1966 to June 2010 were identified from a Medline, PubMed, Embase and Cochrane database search. Studies that reported recurrence of the hernia following the removal of a delayed onset infected mesh were included. Publications that did not report on the rates of hernia recurrence, or did not include patients with late onset mesh infection were excluded. All the abstracts were identified by the first author (S.R.) and were then reviewed by a second author (S.K.). Any differences in the opinion about selection and interpretation of data were discussed with the senior author (E.P.P.) whose decision was deemed final. The main outcome measure was incidence of inguinal hernia recurrence following removal of the infected prosthetic mesh. In addition, various long-term symptoms associated with removal of the mesh, such as chronic pain and chronic groin sepsis, were assessed. Although the data were reviewed systematically and results were tabulated and analysed to derive conclusions, a meta-analysis was not possible as none of the studies included had a comparison group and the number of patients included in the publications was small.
Results
Some 153 abstracts were reviewed and although 12 potential studies were initially identified, only 7 were included in the final review [1, 3, 6, 9, 12–14]. The included studies were six case series and one case report and these comprised a total of 40 patients in whom delayed onset infected mesh was removed. A second published case report on the topic of late-onset deep seated mesh infection [4] was identified; however, this did not specifically address the issue of recurrence following the removal of infected prosthetic mesh and was therefore excluded. The gender of included patients was traced in three case series and the case report—there were 27 male and 4 female patients [1, 6, 9, 13]; the gender of the patients was not known in the three remaining case series [3, 12, 14]. The follow-up period after removal of the infected mesh ranged from 12 to 48 months. The follow up period was not mentioned in two case series and the case report [9, 13, 14]. Of the 40 patients in whom the delayed onset infected mesh was removed, only 2 (less than 5%) developed a recurrent hernia (12 and 44 months after removal of the mesh). The primary procedure was laparoscopic hernia repair in one case, while the second patient underwent open mesh repair of inguinal hernia. Removal of the mesh resulted in resolution of symptoms in up to 95% of patients. The studies included in the review as well their main outcomes are summarized in Table 1.
Discussion
Chronic groin sepsis caused by late-onset deep seated mesh infection is a rare (reported incidence of 0.7%; range, 0.03–1.4%) complication of inguinal hernia repair that often necessitates removal of the mesh to resolve symptoms [1]. The purpose of this review was to identify whether or not this removal of mesh leads to recurrence of the hernia, and also whether or not it results in resolution of symptoms. The results showed that recurrence of herniae following removal of the infected prosthetic mesh is not common (2 out of 40 cases, or less than 5%). Moreover, removal of the mesh led to complete resolution of the symptoms in approximately 95% of cases. However, due to the paucity of available studies, their retrospective nature and the small number of patients included in them, more research is required to further validate these results.
Open tension-free hernia repair using prosthetic meshes is an operation frequently performed for inguinal herniae. It has a low recurrence rate of between 0.14 and 4% [1, 2, 10], and a recent meta-analysis has shown that there is sufficient evidence to support its use in comparison to other techniques of herniorhaphy [3, 5, 11]. Post operative infections, including late-onset deep seated mesh infection, is one of the complications of the hernia repair. Previous studies have demonstrated that approximately 2.88–4.37% of patients suffer from postoperative mesh infection [3]. Deep seated and delayed onset mesh infections on the other hand are less common and present complex treatment challenges. Conservative management can potentially salvage the mesh although it is not successful on all occasions. EHS guidelines deem it necessary to remove the mesh where a poly-filament mesh has been used although they suggest that it may be possible to salvage the mesh in cases of mono-filament materials [2]. Greenberg et al. [16] demonstrated success in salvaging meshes in 7 out of 11 patients treated conservatively for deep seated mesh infection. Their management included intravenous antibiotics, dressing change with normal saline, and drainage of any abscesses along with the use of wound vacuum assist devices [16]. Patients were followed up for a minimum of 3 years and there were no recurrences. The four remaining patients had their meshes removed, as conservative management was unsuccessful; however, no further follow up data was available for these patients and therefore they were not included in our results [16]. This again points out that removal of the mesh will be necessary in a proportion of patients who fail conservative management [5], and that this results in complete resolution of the symptoms [4–6].
Our review included six case series and a case report. All of these were retrospective studies and included 40 patients in total. Only two (less than 5%) patients who had their meshes removed following infection had recurrence of hernia. The median follow up period of all the published papers was 26 months. Taylor et al. reported both the recurrences in their 12 cases (16%) in whom the mesh was removed for chronic groin sepsis, and these occurred 12 and 44 months after the removal of the mesh. One of these patients had undergone laparoscopic hernia repair. Their results were based on a survey of surgeons in the West of Scotland performing inguinal hernia repair, who were asked whether or not they had encountered chronic groin sepsis. On the other hand, Fawole et al. identified 14 cases of chronic groin sepsis requiring mesh removal over a period of 8 years, but found no recurrences at a median follow-up period of 44 months (range 5–91 months) [1]. Similar results were reported by Yerdel et al. [12] and Kucuk et al. [14] in their respective case series; however, the follow up period was not mentioned in either of these studies.
Chronic groin sepsis has also been reported following laparoscopic hernia repair. Avtan et al. [9]found three cases of mesh infection—two with delayed infection after laparoscopic repair of their herniae. All of them underwent mesh removal, as antibiotics failed to resolve the sepsis; there were no recurrences although the follow up period was not mentioned. In our review, of the 40 patients with chronic groin sepsis, operative details were available for 38 cases. Out of these 38 patients, 4 had undergone laparoscopic repair of their primary hernia and, of these, 1 developed a recurrence.
Our review has some limitations. Firstly, all the studies included in this review are retrospective case series with relatively small sample sizes. The lack of randomised trials on the management of chronic groin sepsis following hernia repairs is probably a reflection of the very low rates of occurrence of late onset mesh involvement, which would make conducting any randomised trial difficult. Secondly, the studies included in the review do not have an adequate period of follow up after removal of the mesh. The longest follow up period is only 4 years, whereas evidence suggests that only half of the recurrences occur in first 5 years; and that a follow up of at least 10 years is required to rule out any recurrence [15]. The paper by Taylor et al. [6] included in our review is actually a questionnaire survey, which may therefore underestimate the rates of late onset groin sepsis. Lastly, as a consequence of publication bias, unreported cases of chronic groin sepsis and its subsequent management cannot be ruled out.
Our results suggest that removal of the mesh should be offered to patients with late onset mesh infection. Based on the results of this review, this would result in resolution of sepsis and not lead to recurrence of the hernia. Due to the relatively short follow-up period of the studies included in this review, it may be argued that more recurrences may occur over time, and that the true incidence of hernia recurrence may be much higher. However, even if this were true, managing a hernia recurrence after resolution of sepsis should not pose major problems.
In conclusion, based on this review, recurrence of hernia following removal of an infected mesh after late onset mesh infection is not common and results in resolution of the sepsis in the majority of cases. However, further research is required as the number of patients in our review is relatively small.
References
Fawole AS, Chaparala RP, Ambrose NS (2006) Fate of the inguinal hernia following removal of infected prosthetic mesh. Hernia 10(1):58–61
Simons MP, Aufenacker T, Bay-Neilsen M et al (2009) European hernia society guidelines on the treatment of inguinal hernia in adult patients. Hernia 13:343–403
Delikoukos S, Tzovaras G, Laikou P, Matzos F (2007) Late-onset deep mesh infection after inguinal hernia repair. Hernia 11:15–17
Ismail W, Agrawal A, Zia MI (2002) Fate of chronically infected onlay mesh in groin wound. Hernia 6:79–81
Aufenacker T, Geldere D, Mesdag T et al (2004) The role of antibiotic prophylaxis in prevention of wound infection after Lichtenstein open mesh repair of primary inguinal hernia. Ann Surg 240(6):955–960
Taylor SG, O’Dwyer PJ (1999) (1999) Chronic groin sepsis following tension-free hernioplasty. Br J Surg 86(4):562–565
Roller Jonas, Matthias W, Langenbecks L (2008) Prolene–Monocryl-composite meshes do no increase micro vascular Staphylococcus aureus adherence and do not sensitize for leukocytic inflammation. Arch Surg 393:349–357
Karatepe O, Ozturk A, Koculu S (2008) To what extent is cyanoacrylate useful to prevent early wound infections in hernia surgery? Hernia 12:603–607
Avtan L, Avci C, Bulut T, Fouranier G (1997) Mesh infections after laparoscopic inguinal hernia repair. Surg Laparosc Endosc 7:192–195
Rodríguez-Cuéllar E, Villeta R, Ruiz PT et al (2005) National project for the management of clinical processes (in Spanish). Surgical treatment of inguinal hernia. Cir Esp 77(4):194–202
Scott NW, McCormack K, Graham P, Go PM, Ross SJ, Grant AM (2002) Open mesh versus non-mesh for repair of femoral and inguinal hernia. Cochrane Database Syst Rev 4, CD002197
Yerdel M, Akin E, Dolalan S, Turkcapar A, Pehlivan M (2001) Effect of single-dose prophylactic antibiotic on wound infection after tension-free inguinal hernia repair with polypropylene mesh: the randomised, double blind, prospective trial. Ann Surg 233:26–33
Foschi D, Corsi F, Cellerino P, Trabucchi A, Trabucchi E (1998) Late rejection of the mesh after laparoscopic hernia repair. Surg Endosc 12(5):455–457
Kucuk HF, Sikar HE, Kurt N, Uzun H, Eser M (2010) Lichtenstein or darn procedure in inguinal hernia repair: a prospective randomised comparative study. Hernia 14(4):357–360
Leibl BJ, Daubler P, Schmidt CG, Kraft K, Biitner R (2000) Long term results of a randomized clinical trial between laparoscopic hernioplasty and shouldice repair. Br J Surg 87:780–783
Greenberg JJ (2010) Can composite infected mesh be salvaged? Hernia 14:589–592
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rehman, S., Khan, S., Pervaiz, A. et al. Recurrence of inguinal herniae following removal of infected prosthetic meshes: a review of the literature. Hernia 16, 123–126 (2012). https://doi.org/10.1007/s10029-011-0873-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-011-0873-2