Abstract
Inguinal hernia repair with mesh is one of the most common operations performed by general surgeons. Mesh infection is a rare complication that has detrimental effects on the patient and the healthcare system. The purpose of this systematic review was to determine an evidence-based management approach for patients with infected mesh following an open Lichtenstein inguinal hernia repair. The literature search was achieved using the Preferred Reporting Items for Systematic Reviews and Meta-analysis guidelines (PRISMA). The quality of the papers was assessed using Grading of Recommendations Assessment Development and Evaluation (GRADE) criteria. Studies were analysed by two independent reviewers. A total of 1532 abstracts and articles were reviewed. Fourteen met the inclusion criteria. In most, the mesh used was either monofilament or multifilament polypropylene. Most (86.8%) underwent mesh removal despite attempts at conservative management. Universally, in the presence of sinus formation (infected mesh to skin), mesh removal was required for definite resolution of infection. After a period of conservative management, removal of infected mesh following Lichtenstein inguinal hernia repair may be recommended. However, the quality of evidence is poor. Techniques such as partial removal or use of negative pressure dressings may need to be further explored.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inguinal hernias account for 75% of abdominal wall hernias [1]. The lifetime risk of developing an inguinal hernia is 27% for males and 3% for females [1]. Once inguinal hernias are symptomatic, elective surgical repair with mesh is recommended to relieve symptoms and to avoid obstruction or strangulation, which would require an emergency operation [2]. Inguinal hernia repair may be performed with an open (anterior) or laparoscopic approach. In the open mesh technique, the Lichtenstein tension-free repair with onlay mesh is the procedure of choice. It has been endorsed by the European Hernia Society as being the preferred method because it is associated with minimal perioperative morbidity, can be performed as a day-case procedure, is easy to learn and has an overall recurrence rate of less than 4% [3].
The use of mesh reduces the rate of hernia recurrence. Important characteristics of mesh are pore size, tensile strength, fibres (multifilament versus monofilament), chemical composition, weight, reactivity and constitution. Polypropylene (e.g. PROLENE) meshes are commonly used [4].
Inguinal hernia repair is classified as a clean surgical wound (class 1) and therefore should have a 2% or lower rate of infection. Surgical site infection (SSI) may be superficial surgical site infection (SSSI) or deep surgical site infection (DSSI) [5]. DSSI (i.e. mesh infections) are rare but generate significant morbidity. The rate of SSI with elective inguinal herniorrhaphy is reported at 2 to 4% in most studies with less than one quarter being mesh infections. Diagnosis of mesh infection is based on symptoms (pain, feeling unwell), signs (swelling, erythema, purulent discharge, sinus, fevers) and investigations (needle aspiration or swab with wound microbiology culture and sensitivity, blood test, ultrasound, CT scan, MRI, indium labelled white blood cell scan). However, in latent disease, the diagnosis may be difficult, especially as it can be a silent persisting infection with no clinical signs [4].
Many different approaches for the management of deep-seated mesh infection are documented: use of antibiotics alone, incision and drainage, use of negative pressure therapy and removal of mesh [4, 6]. There is no consensus or systematic review in the literature to guide the management of infected inguinal hernia mesh following open repair. A systematic review of the incidence and management of infected mesh after an open inguinal hernia repair (Lichtenstein approach) using Preferred Reporting Items for Systematic Reviews and Meta-analysis principles was undertaken to determine the current best management and level of evidence.
Material and Methods
Using the PRISMA method, a literature search was performed [7]. Studies published up to December 2017 with the MESH terms: “inguinal hernia”, “inguinal herniorrhaphy”, “infected mesh”, “mesh infection” were identified using the Boolean operators OR and AND in six databases: PubMed, Embase, Scopus, Cochrane, Ovid MEDLINE and Clinicaltrials.gov. The references of the studies found were manually searched for any potentially relevant article. No formal inquiry was made to the authors of selected papers.
To be included, the article needed to report on the outcomes of management of a Lichtenstein inguinal mesh repair with infected mesh. Articles featuring non-Lichtenstein repairs (e.g. plug/patch, preperitoneal repairs), laparoscopic inguinal hernia repair, incisional, ventral and other types of hernia repair were excluded. Articles with ambiguous results or inadequate clinical detail were also excluded. Other exclusion criteria were Lichtenstein inguinal mesh repair with SSSI only, non-English language articles and publication as abstract only. Case reports which did not have a trial of conservative management were excluded too.
Results were manually extracted by two independent reviewers. Primary outcome was resolution of infection as a function of different strategies of managing the infected mesh (i.e. conservative versus surgical). The risk of bias as well as the quality of individual studies will be assessed by Grading of Recommendations Assessment Development and Evaluation Criteria (GRADE) criteria [8]. A narrative review of the relevant studies describing outcomes of conservative versus operative management of mesh infection from RCT and Retrospective Studies will be presented. A formal meta-analysis was not possible.
Results
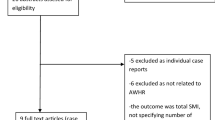
The identification process for eligible studies is summarised in Fig. 1. The search strategy initially produced 1532 studies, of which 1479 were excluded on the basis of the title, abstract or meeting exclusion criteria. Of the remaining 53 studies, 39 were excluded as indicated. Fourteen studies met all the inclusion criteria: five case reports, four retrospective case series, five RCT. For ease of presentation, the eligible studies will be grouped by type of study.
Case Studies
Ismail (2002), Chatzimavroudis (2014), Filippou (2017), Sohail (2004), Maheshwari (2016) reported case studies [9,10,11,12,13].
The studies included eight men and one woman. Eight out of nine meshes used were unspecified polypropylene mesh and the method of mesh fixation was usually not mentioned. Presentation of infection post Lichtenstein repair was a median of 34 months (ranging from 0.56 to 144 months). Eight out of nine patients presented with a discharging sinus at the incision site. Most pathogens causing the infection were identified: four Staphylococcus aureus, one Proteus, one Pseudomonas aeruginosas and one Mycoplasma gondii.
All nine patients received intravenous antibiotics with incision and drainage as needed.
The median length of conservative management was 4 months (ranging from 2 days—overwhelming sepsis—to 24 months). All patients needed readmission after failure of conservative management and underwent total mesh explantation and sinus excision. None needed more extensive surgery (e.g. bowel resection).
Post removal of mesh, patients were usually followed for 6 months. All had resolution of infection and none had hernia recurrence.
These case studies highlight mesh infection presenting more than 10 years after the primary surgery.
Retrospective Case Series
Celdrán (2007), Jezupors (2006), Akyol (2013), Chen (2016) met the inclusion criteria. [14,15,16,17].
A total of 6513 patients were included in these retrospective series and a total of 25 mesh infections were reported (0.4%). Twenty-two patients were male and three were female. Their median age was 57.7 years (ranging from 23 to 75 years old). All had insertion of polypropylene mesh (17 multifilament, 6 monofilament and 2 unspecified). The method of fixation was not specified. The use of prophylactic antibiotics at time of primary surgery was usually not reported. No complication at the time of primary surgery was mentioned.
The time between primary surgery and infection was a median of 7.5 months (ranging from 0.5 to 60 months), but one study did not provide the time frame. Twenty-one out of 25 patients presented with a chronic sinus at time of diagnosis. In nine cases, no pathogen was cultured whereas 11 had Staphylococcus aureus (including two Methicillin Resistant Staphylococcus aureus), three were other gram-positive pathogens (including two Acid-fast gram-positive bacteria) and four were gram-negative bacteria.
All 25 patients received antibiotics and required either incision and drainage or debridement of the wound. The median length of time for conservative management was 1.2 months (ranging from 0.5 to 2.5 months), with one study that did not report the duration.
All had resolution of the infection with mesh removal and only two developed hernia recurrence (8%). The timing of follow-up post removal of mesh was not always available, but the median was 29.2 months (ranging from 12 to 115 months).
RCT on Use of Prophylactic ABs at Time of Inguinal Hernia Repair
Aufenacker (2004), Perez (2005), Yerdel (2001), Shankar (2010), Othman (2001) are RCTs investigating the use of prophylactic antibiotics or a placebo at the time of induction for an open Lichtenstein hernia repair [18,19,20,21,22]. These published the incidence of SSSI and DSSI and discussed the benefits of giving prophylactic antibiotics. Only these five studies were retained as they reported DSSI. As management of DSSI was a by-product of the RCTs, we considered these studies to be observational studies only.
To begin with, 2228 patients were included but 2069 completed the trials and 13 had a DSSI (0.6%). The median age of all patients was 52.5 years old and more than 85% were male. Three studies used monofilament with PROLENE for suture fixation, and two studies used unspecified polypropylene mesh. Three studies reported the timing of the infection from the day of surgery, ranging from 0.13 to 2.6 months.
In nine cases, the culprit pathogen was Staphylococcus aureus, two were Streptococcus spp. and two were Pseudomonas aeruginosa. The rest were unspecified or undiagnosed. Five out of 13 had resolution of symptoms with conservative management and therefore their mesh was salvaged. Eight needed total mesh removal after failure of conservative management (Table 2).
All Studies
Out of 8741 Lichtenstein inguinal hernia repairs from case series and RCTs, there were 38 mesh infections (0.4%). Five were successfully managed without mesh removal (13.2%). But the majority (33) needed mesh removal (i.e. 86.8%).
Including the case studies, our study included 47 patients with infected mesh. Forty-two meshes needed explantation for resolution of infection (89.3%).
Grading of Recommendations Assessment Development and Evaluation Criteria
As the case series are retrospective without any control population or strict inclusion criteria, there are significant limitations in the study design. Hence, the risk of bias is non-negligible.
In the RCTs, there is also bias regarding the reporting as this outcome was a rare event and there may be inadequate accounting of patients and events due to incomplete follow-up. One study finished early due to perceived benefits of prophylactic antibiotics. Overall, there is incomplete reporting regarding the DSSI and their management. So, the risk of bias is present and downgrades the evidence.
The results regarding management of mesh infection seemed consistent throughout the nine studies and point towards removal of mesh. Nonetheless, this is based on a heterogeneous population across nine retrospective and prospective studies with a low rate of DSSI.
Therefore, the overall quality of the evidence is poor, which leads to weak conclusions regarding the recommendation towards mesh removal in patients affected with mesh infection post Lichtenstein inguinal hernia repair.
Discussion
This review shows failure of conservative management in 89.3% of reported mesh infections following a Lichtenstein inguinal hernia repair. This was obtained by combining all reported mesh infections in the studies reviewed. To date, there is no systematic review on management of infected mesh post Lichtenstein repair. This might be due to the rarity of the event, the lack of reporting or the paucity of relevant studies. While DSSI involving the mesh is rare, the number of patients affected is high given how frequently Lichtenstein hernia repair is performed.
Mesh infection can be difficult to diagnose. During the early stages, it is almost impossible to clinically differentiate a superficial wound infection from infected mesh. As the superficial wound infection is treated with antibiotics and usually resolves quickly, infection that lasts longer or does not respond to antibiotics should raise the suspicion of a deeper infection, most likely involving the mesh. The presence of a fistula or the development of an abscess at the area of mesh implantation also suggests a mesh infection. Occasionally, an abscess adjacent to a mesh may not cause any systemic features or any obvious local signs of infection.
The trial of conservative management after recognition of DSSI ranged from a few days to, in extreme cases, up to 49 months. The median for the whole group could not be calculated due to lack of reporting, especially in the RCTs. From this data, it may be reasonable to consider mesh explantation after 1 month of conservative management without resolution or reoccurring after multiple representations resolving with antibiotics.
One French study from 2011, the largest series of mesh infections after inguinal hernia repair, reported failure of conservative management and mesh removal in 86% of patients. The DSSI mostly occurred during the first month (50%), but 26% were diagnosed one year after the procedure. Thirty-three patients had resolution of infection with mesh removal. Nineteen had multiple attempts at conservative management prior to explantation. Their findings were similar to those reported in our study including the types of pathogen found—mainly Staphylococcus aureus, followed by Escherichia coli and Pseudomonas spp. [23]. However, this study was not included because it presented mixed laparoscopic and open approaches, making it unfeasible to isolate the results for Lichtenstein repair only.
The type of mesh used may play a role in the decision for mesh removal. ePTFE infected mesh is often explanted due to its hydrophobic properties and microporous structure [24, 25]. The European Hernia Society guidelines recommend the use of non-absorbable monofilament mesh for inguinal hernia repair in adults to reduce the risk of incurable chronic sinus formation or fistula [3]. In the case of DSSI with the presence of a multifilament mesh, the guidelines state that complete wound healing after adequate drainage alone is virtually impossible. This is linked to the fact that bacteria can hide from leucocytes because the structure of the mesh is closely woven with small pore diameter and therefore cannot be perfectly sterilised [3]. In this study, no ePTFE meshes were identified but mesh composition details were missing for one patient. Most infected meshes used were polypropylene (46/47). However, the proportion of mono versus multifilament polypropylene mesh is undetermined.
Recognised patient factors (age, gender, ASA, comorbidities, obesity, smoking or immunosuppression) were not systematically reported in these studies [26, 27]. The patients’ median age was 54.8 years old. Overall, more than three-quarters of mesh infections were in males; this is probably because inguinal hernia repair is most often carried out in the male population. The reported timing of infection ranged from 1 week to 144 months. The very late presentations with mesh infection were from case studies. Retrospective studies showed timing extending to 1.5 years. Commonly, the DSSI occurs within the first few months after surgery [4, 23]. Some suggest that infection presenting a long time after implantation when a fibrous capsule has already developed can only be resolved by mesh explantation. This is based on the observation that antibiotic penetration will be incomplete due to the presence of the fibrous capsule. The fibrous capsule may also minimise the signs and symptoms of infection [22, 28].
Explantation of mesh after a Lichtenstein repair has its inherent morbidity and technical challenges—injury to the vas deferens and testicular neurovascular bundle to the testis. Some authors have recommended performing the removal of mesh in two stages to allow for reduction of inflammation and better visualisation of tissue planes. The first stage starts with initial incision and drainage then removal of mesh after fistula formation [14]. Of the 33 patients who needed mesh removal, two patients developed hernia recurrence clinically. Fawole et al.’s (2006) retrospective study on 2139 open inguinal hernia repair over an 8-year period identified 14 DSSI who needed mesh removal. After follow-up post mesh explantation, only two patients had asymptomatic hernia recurrence (2/14). They extrapolated that strength of mesh repair rests in the fibrous reaction induced with the transversalis fascia by the prosthetic material rather than in the physical presence of the mesh [28]. This study was not included due to the presence of mesh plug repair mixed with the Lichtenstein approach and the inability to extract relevant data.
Five studies included in this review were RCTs on the use of prophylactic antibiotics for elective hernia repair. In low-risk patients and in hospitals where there is a low incidence of wound infection, there is not a specific benefit to prophylactic antibiotics as there is no obvious association between use of antibiotic prophylaxis and incidence of DSSI [3, 29, 30].
This study has several limitations. First, it incorporates case reports and retrospective studies, some of which had missing data. Results of case reports are subject to author bias as well as small sample sizes and were thus excluded from analysis. The multitude of case reports available in the literature suggests deep-seated mesh infection is not very common. As these reports are very heterogeneous and without blinding or randomisation, there is significant reporting and selecting biases. Some studies reported only on patients who had mesh removed due to DSSI, so DSSI that resolved with conservative management may have been unreported. Therefore, there would be a reporting bias towards removal of mesh in the event of DSSI. Patients successfully treated conservatively may be unreported. The primary outcome of the RCTs was detecting and reporting infection, so management of mesh infection was not the focus of the trials: reporting the management of DSSI was thus limited.
Secondly, because of insufficient data due to incomplete reporting, this study is unable to produce a timeline regarding removal of mesh once infected. Once a sinus has developed, infected mesh should be removed. As previously mentioned, if infection does not resolve with conservative management within a month, mesh infection should be considered as well as the requirement for mesh explantation.
Third, some newer options (e.g. negative pressure wound therapy or partial excision of mesh) were not included but may be a viable option to eradicate mesh infection [31,32,33].
Conclusion
In conclusion, the studies were heterogeneous so analysis is difficult. Mesh infection following a Lichtenstein inguinal hernia repair may not be a rare event and impacts patients significantly. While ultimately prevention of mesh infection is the goal [34], when mesh infection is diagnosed, and conservative management fails, mesh removal will be necessary. The hernia is unlikely to recur.
References
Jenkins JT, O’Dwyer PJ. Inguinal hernias. BMJ (Clin Res ed). 2008;336(7638):269–72.
Leblanc KE, Leblanc LL, Leblanc KA. Inguinal hernias: diagnosis and management. Am Fam Physician. 2013;87(12):844–8.
Simons MP, Aufenacker T, Bay-Nielsen M, Bouillot JL, Campanelli G, Conze J, et al. European hernia society guidelines on the treatment of inguinal hernia in adult patients. Hernia. 2009;13(4):343–403.
Deysine, M. (2013) Hernia infections: pathophysiology - diagnosis - treatment - prevention, S.l: CRC press.
Centres for Disease Control And Prevention. 2018. Surgical site infection (SSI) event. Procedure-associated Module. https://www.cdc.gov/nhsn/PDFs/pscManual/0pscSSIcurrent.pdf
Shubinets et al. (2018) Management of infected mesh after abdominal hernia repair: systematic review and single-institution experience. Ann Plast Surg, 80(2):145–153.
Liberati et al. (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol, 62(10):e1–e34.
Atkins, D.A., et al., (2004) Systems for grading the quality of evidence and the strength of recommendations I: critical appraisal of existing approaches The GRADE Working Group. , 4(1), p.38.
Ismail W, Agrawal A, Zia M. Fate of chronically infected onlay mesh in groin wound. Hernia. 2002;6(2):79–81.
Chatzimavroudis G, Papaziogas B, Atmatzidis S, Atmatzidis K. Obesity as a lifetime risk factor for mesh infection after groin hernia repair. Ann Surg. 2014;259(6):e89.
Filippou D. Late inguinal mesh infection 12 years after the initial operation: report of the case and short review of the literature. Case reports in surgery, 2017, p.4385913me risk factor for mesh infection after groin hernia repair. Ann Surg. 2017;259(6):e89.
Sohail MR, Smilack JD. Hernia repair mesh-associated Mycobacterium goodii infection. J Clin Microbiol. 2004;42(6):2858–60.
Maheshwari J, Garg K. Mesh infection after inguinal hernia mesh repair – experience of five mesh removal. IOSR J Dent Med Sci. 2016;V12(15(4)):78–80.
Jezupors A, Mihelsons M. The analysis of infection after polypropylene mesh repair of abdominal wall hernia. World J Surg. 2006;30(12):2270–8.
Akyol C, Kocaay F, Orozakunov E, Genc V, Kepenekci Bayram I, Cakmak A, et al. Outcome of the patients with chronic mesh infection following open inguinal hernia repair. J Korean Surg Soc. 2013;84(5):287–91.
Chen T, Zhang Y-H, Wang H-L, Chen W, Wang J. Late-onset deep mesh infection: a study of eight cases detected from 2666 consecutive patients with abdominal wall hernia repairs. Chin Med J. 2016;129(15):1870–2.
Celdrán A, Esteban J, Mañas J, Granizo JJ. Wound infections due to Mycobacterium fortuitum after polypropylene mesh inguinal hernia repair. J Hosp Infect. 2007;66(4):374–7.
Aufenacker et al. (2004) The role of antibiotic prophylaxis in prevention of wound infection after Lichtenstein open mesh repair of primary inguinal hernia: a multicenter double-blind randomized controlled trial. Ann Surg, 240(6):955–961.
Perez AR, Roxas MF, Hilvano SS. A randomized, double-blind, placebo-controlled trial to determine effectiveness of antibiotic prophylaxis for tension-free mesh herniorrhaphy. J Am Coll Surg. 2005;200(3):393–7.
Yerdel MA, Akin EB, Dolalan S, Turkcapar AG, Pehlivan M, Gecim IE, et al. Effect of single-dose prophylactic ampicillin and sulbactam on wound infection after tension-free inguinal hernia repair with polypropylene mesh: the randomized, double-blind, prospective trial. Ann Surg. 2001;233(1):26–33.
Shankar VG, Srinivasan K, Sistla SC, Jagdish S. Prophylactic antibiotics in open mesh repair of inguinal hernia – a randomized controlled trial. Int J Surg. 2010;8(6):444–7.
Othman I. Prospective randomized evaluation of prophylactic antibiotic usage in patients undergoing tension free inguinal hernioplasty. Hernia: J Hernias Abdominal Wall Surg. 2011;15(3):309–13.
Johanet H, Contival N. Mesh infection after inguinal hernia mesh repair. J Visc Surg. 2011;148(5):e392–4.
Brown CN, Finch JG. Which mesh for hernia repair? Ann R Coll Surg Engl. 2010;92(4):272–8.
Petersen S, Henke G, Freitag M, Faulhaber A, Ludwig K. Deep prosthesis infection in incisional hernia repair: predictive factors and clinical outcome. Eur J Surg= Acta Chirurgica. 2001;167(6):453–7.
Chiow AKH, Chong CK, Tan S-M. Inguinal hernias: a current review of an old problem. Proc Singapore Healthcare. 2010;19(3):202–11.
Oberg S, Andresen K, Rosenberg J. Etiology of inguinal hernias: a comprehensive review. Front Surg. 2017;4:52.
Fawole A, Chaparala S, Ambrose R. Fate of the inguinal hernia following removal of infected prosthetic mesh. Hernia. 2006;10(1):58–61.
Miserez M, et al. Update with level 1 studies of the European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia. 2014;18(2):151–63.
Mazaki T, et al. A randomized trial of antibiotic prophylaxis for the prevention of surgical site infection after open mesh-plug hernia repair. Am J Surg. 2014;207(4):476–84.
Meagher H, Clarke Moloney M, Grace PA. Conservative management of mesh-site infection in hernia repair surgery: a case series. Hernia. 2015;19(2):231.
Sabbagh C, et al. Partial removal of infected parietal meshes is a safe procedure. Hernia. 2012;16(4):445–9.
Bueno-Lledó J, et al. Partial versus complete removal of the infected mesh after abdominal wall hernia repair. Am J Surg. 2017;214(1):47–52.
Deysine M. Post mesh herniorrhaphy infection control: are we doing all we can? Hernia. 2004;8(2):90–1.
Acknowledgments
This research was undertaken as part of the third year of the MSc in Surgical Sciences or Edinburgh Surgical Sciences Qualification www.essq.rcsed.ac.uk
Author information
Authors and Affiliations
Contributions
Dr. Amelie Maurel: study conception and design, acquisition of data, analysis and interpretation of data, drafting of manuscript
Dr. Darren Karadimos: acquisition of data, analysis and interpretation of data
Dr. Arkadiusz Peter Wysocki: study conception and design, analysis and interpretation of data, critical revision of manuscript
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
For this type of study, formal consent was not required.
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent
Informed consent was not required to undertake this systematic review.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Surgery
Rights and permissions
About this article
Cite this article
Maurel, A., Karadimos, D. & Wysocki, A.P. Management of Infected Mesh After Lichtenstein Hernia Repair: a Systematic Review. SN Compr. Clin. Med. 1, 730–736 (2019). https://doi.org/10.1007/s42399-019-00114-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42399-019-00114-0