Abstract
Introduction
Progressive preoperative pneumoperitoneum (PPP) is used to prepare incisional hernias with loss of domain (IHLD) operations. The aim of the present study was to analyze the effect of PPP on peritoneal volume [measured using a new computed tomography (CT)-based method] and respiratory function.
Methods
From July 2004 to July 2008, 19 patients were included in a prospective, observational study. The volumes of the incisional hernia (VIH), the abdominal cavity (VAC), the total peritoneal content (VP) and the VIH/VP ratio were measured before and after PPP using abdominal CT scan data. Spirometric parameters were measured before and after PPP, and postoperative clinical data were evaluated.
Results
Before and after PPP, the mean VIH was 1,420 cc and 2,110 cc (P < 0.01), and the mean VAC was 9,083 cc and 11,104 cc (P < 0.01). The VAC increased by 2,021 cc (P < 0.01) and was greater than the mean VIH before PPP. After PPP, the spirometric measurements revealed a restrictive syndrome. The overall postoperative morbidity rate was 37%.
Conclusions
PPP increased the hernia and abdominal volumes. PPP induced a progressive, restrictive syndrome.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Some incisional hernias are considered to be complex and dangerous to treat (regardless of the hernia site and any co-morbidities). These are large incisional hernias (defined as having a diameter greater than 10 cm) [1] and incisional hernias with loss of domain (IHLD). In the latter case, the hernia contents are held in place by adhesions and cannot be reintegrated into the abdominal cavity (i.e., the herniated organs have lost their “right of domain” in the abdomen) [2]. The incidence of incisional hernia has increased over recent years, and a report published in 1999 revealed that large median incisional hernias accounted for nearly 21% of all incisional hernias treated in our department [3, 4]. Treatment of large incisional hernias and IHLD is considered to be dangerous because fascia closure under tension not only constitutes a risk factor for recurrence [5] but is also life threatening (due to intra-abdominal hypertension, also known as abdominal compartment syndrome) [6, 7] with the risk of respiratory compliance disorders and intestinal ischemia [6–9].
To prevent this postoperative risk, progressive preoperative pneumoperitoneum (PPP) (also known as the Goni Moreno protocol) [10, 11] has been suggested as a preparatory procedure for the treatment of IHLD [12, 13] and other hernias [14]. In our department, Stoppa et al. [15] reported the use of PPP in 18.5% of 247 cases. To the best of our knowledge, there are no literature data on the volumetric and respiratory effects of PPP. Kingsnorth et al. [16] considered that a hernia sac (or second abdomen) volume >15–20% of the natural abdominal compartment volume would require respiratory adaptation. However, this figure was based on anecdotal experience, rather than a quantitative analysis. We recently reported that in the management of IHLD, PPP increased the length of the muscles in the anterolateral abdominal wall but that the corresponding gain in width also prevented “coverage” of the incisional hernia [10].
Since the 1980s, hepatobiliary surgeons and radiologists have developed the concept of hepatic volume measurements [17]. Liver volumes are calculated from a computed tomography (CT) scan [18, 19] and the results are used in practice as a guide to the optimal therapeutic indication (e.g., immediate resection or prior portal embolization). A method for calculating the abdominal hernia volume has recently been described [20]. In collaboration with radiologists, we have also developed a reproducible method for calculating the intraperitoneal volume and content of the hernia sac before and after PPP. In parallel, we assessed the impact of PPP on volumetric lung function by studying respiratory function test (RFT) results before and after the procedure.
The purpose of the present study was to investigate the impact of PPP on peritoneal volume, respiratory function and clinical outcomes.
Patients and methods
Population
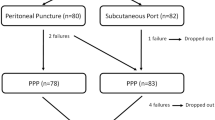
Since 2004, we have performed a prospective study on incisional hernias prepared by Goni Moreno PPP. Of the 227 patients operated on for incisional hernia between July 2004 and July 2008, 24 patients were prepared by PPP for IHLD (n = 22) or hernia with loss of domain (n = 2) operations. A large incisional hernia is defined by a hernia defect width of over 10 cm and a medium-sized incisional hernia is defined by a hernia defect width between 5 and 10 cm [1]. There is loss of domain when the hernia contents are fixed in place by adhesions and cannot be reintegrated into the abdominal cavity [2]. Five patients were excluded: in one case, mental retardation made spirometry unfeasible and four patients were excluded because CT volume measurements were not feasible (because some of the IHLD fell outside the CT scan’s field of view). Hence, 19 patients were included in the study. A non-contrast, low-dose abdominal CT scan and lung function tests were performed before and after PPP. The protocol was approved by the independent ethics committee at Amiens University Hospital (reference: 2010–2014).
Therapeutic technique: progressive preoperative pneumoperitoneum
For patients with large incisional hernia or IHLD, our department has always applied a strategy including PPP. Since July 1987, a total of 115 patients (including the 24 patients in the present study) have been prepared by PPP. After analyzing the CT scan and, notably, checking for the absence of bowel at Palmer’s point (i.e., at the intersection of the linea alba and the linea semi lunaris, at the intersection of the left hypochondriac region and the left lumbar region), ambient air was introduced at this point under local anesthesia via a Palmer needle (with an atraumatic end) and a 50 ml syringe connected to a 3-way valve. The valve itself was plugged into the Palmer needle (Fig. 1). The initial procedure was performed in an operating theatre but subsequent sessions took place in the patient’s hospital room. One morbidly obese patient [body mass index (BMI = 57.8)] and one patient having undergone a primary abdominal aesthetic surgery procedure received PPP through a subcutaneous port (implanted under general anesthesia). The PPP procedure consisted in intraperitoneal injection of ambient air every 2 days for around 2 weeks. During each session, air injection was continued as long as the patient remained clinically free of scapular pain, dyspnea or subcutaneous emphysema. When these signs appeared, air injection was stopped and a further session was initiated 2 days later. Between each injection and until surgery, patients wore an abdominal belt to avoid gas accumulating within the hernia. Intra-abdominal pressure monitoring was attempted during the insufflation sessions (using a laparoscopic pressure sensor) but the measurements were neither reliable nor reproducible.
Data analyzed
Demographic data
Age, gender, BMI, American Society of Anaesthesiologists (ASA) status and a history of active smoking, chronic obstructive pulmonary disease (COPD) and/or asthma were analyzed.
Criteria related to disease
The incisional hernias and other hernias were classified according to the international consensus classification [1].
Quantitative analysis (size, volume) of incisional hernias
Intraperitoneal volumes were calculated from non-contrast 16-and 32-slice multi-detector CT data (GE Healthcare) using Myrian Expert® software. Unlike liver volume measurements, the tissue density prevents the automatic recognition of intra-peritoneal contents. Hence, volumes were calculated by the application of 12–17 operator-defined sections. The boundaries were defined (using a double-blind method) by a surgeon and a radiologist (TY). The software then determined the volume after extrusion. The retroperitoneal space was outside the boundaries and was thus calculated separately. The volume of the incisional hernia (VIH), the abdominal cavity volume (VAC, excluding the incisional hernia), the total peritoneal volume (VP, including the incisional hernia, i.e., VIH+VAC) and the VIH/VP ratio were calculated (Table 1) (Fig. 2). The length and the width of the hernia were measured from the CT data using specific software, as described previously [10]. The CT scans were performed in the absence of an abdominal belt.
Respiratory function tests
The following respiratory function parameters were studied: functional residual capacity (FRC, defined as the volume of air present in the lungs at the end of passive expiration), thoracic gas volume (TGV), residual volume (RV, defined as the volume remaining after maximal expiration), total lung capacity (TLC, defined as the volume of air in the lung after maximal inspiration) and the RV/TLC ratio. An obstructive syndrome was defined as an increase in this ratio.
Dynamic lung volumes were also studied. The forced vital capacity (FVC) is defined as the maximum volume of air that can be exhaled or inspired during a forced maneuver. The forced expiratory volume in 1 s (FEV1) is defined as the volume exhaled during the first second of a forced expiratory maneuver (starting from the total lung capacity). FEF75, FEF50 and FEF25 are the expiratory flow values at 75%, 50% and 25% of TLC, respectively. The FEF75-25 difference is defined as the average air flow during the middle portion of expiration. The peak expiratory flow (PEF, in liters per second) is defined as the peak flow achieved during a maximally forced expiration initiated at full inspiration. The inspired volume in 1 s (VIMS) is defined as the inspired volume during the first second of a forced inspiration. An obstructive syndrome was defined as an FEV1/VC ratio below 70%.
Peroperative and postoperative clinical data
The mean operating time, the position of the prosthesis and postoperative data (morbidity, mortality, length of hospitalization and length of stay in the intensive care unit) were recorded.
Study design
The incisional hernia patients’ volume and spirometric parameters were recorded before and after PPP. The patients’ age and BMI and the height and width of the incisional hernia and post-operative clinical data were also evaluated.
Statistical analysis
The objective of the present study was to analyze the impact of PPP on the volume of the hernia, the abdominal volume, the VIH/VP ratio and the spirometric parameters. Each patient served as his/her own control. All studied criteria were quantitative variables. A univariate analysis was performed using a Wilcoxon test and a P value <0.05 was considered to be statistically significant. All statistical analyses were performed with Statview® software (SAS Institute, Cary NC).
Results
Descriptive analysis of the patient population
Nineteen consecutive patients (15 women and 4 men) with a mean age of 62 years (range: 41–82) underwent PPP. The mean BMI was 39 (range: 22–58). Eleven patents (61%) had an ASA score = 3. Thirteen patients (68%) were non-smokers, four patients (21%) had COPD and one patient (5%) had asthma. There were 17 incisional hernias and two other hernias. Sixteen patients had a median incisional hernia, one had a lateral incisional hernia, one had an umbilical hernia and one had an inguinal hernia. This was a primary incisional hernia or other hernia in 15 cases and recurrence of an incisional hernia in 4 cases. There was cutaneous ulceration in three cases. The mean time since occurrence of the incisional hernia or other hernia was 136.9 months (range: 8–600). The mean number of previous laparotomies per patient was 1.57 (range: 0–6) and five patients had a history of abdominal sepsis. The incisional hernias were large (64%) or medium-sized (36%) with respiratory failure. Seven of the incisional hernias (46.6%) had a length of over 15 cm. Twelve patients (64.7%) had a primary incisional hernia. The mean time since the diagnosis of incisional hernia was 145 ± 151 months (range: 8–600). The hernia was on the midline in 14 (82.3%) cases. Three patients (17.6%) had a combined incisional hernia. The two patients presenting with hernia had a medium-size umbilical hernia with severe respiratory failure and a bilateral, inguinoscrotal hernia with loss of domain (Table 1).
Description of the PPP
The mean insufflated air volume was 14.7 ± 4.4 l (4.5–19.2), with an average of 2.3 ± 0.8 l (0.9–4.5) introduced during each session over a period of 16.5 ± 6.4 days (4–28). Six patients (31.5%) developed subcutaneous emphysema (n = 5) or dyspnea (n = 1) after the procedures. One patient (5%) developed respiratory intolerance that required peritoneal exsufflation. There were no other complications of PPP. Two patients failed to undergo surgery because of acute kidney failure related to obstructive urinary tract lithiasis (n = 1) and anaphylactic shock on induction of anesthesia (n = 1). One procedure was postponed because of phlebitis (n = 1). However, these patients were not excluded from our analysis because they had undergone pre-and post-PPP volume measurements and RFTs. The mean duration of preoperative hospitalization was 24 ± 6.3 days (range 15–40).
Analysis of the volume of the incisional hernia, the abdominal cavity volume and the VIH/VP ratio
Before and after PPP, respectively, the volume of the incisional hernia was 1,420 ± 1,110 cc (165–3,481) and 2,110 ± 1,464 cc (517–4,802) (P < 0.01), the abdominal cavity volume was 9,083 ± 2,549 cc (3,741–12,202) and 11,104 ± 3,893 cc (6,593–21,782) (P < 0.01) and the VIH/VP ratio was 13.9 ± 11.1% (1.5–4) and 14.9 ± 10.5% (4.4–34.3) (NS) (Table 2). The mean volume of intra-peritoneal air before surgery could be estimated as the VP before PPP plus the volume of air insufflated (i.e., 10,503 + 14,700 = 25,203 cc). The post-PPP volume measurement revealed a VP of 13,214 cc. The rate of intraperitoneal air loss over 16.5 days was about 47%.
Respiratory function tests
Relative to pre-PPP values, post-PPP dynamic lung volumes fell by 25.3% for FVC (P < 0.01), 29.6% for FEV1 (P < 0.05), 24.7% for FEV0.5 (P < 0.01), 7.5% for PEF (P < 0.01), 25.4% for FEF50 (P < 0.01), 17.3% for FEF25 (P < 0.05) and 30.6% for FEF75-25 (P < 0.01) (Tables 3, 4). The changes in FEF75 and VIMS were borderline-significant, with decreases of 13.7% and 17.8%, respectively. The Tiffeneau ratio (FEV1/VC) and pulmonary gas measurements were not affected significantly by the procedure. There was a borderline-significant change in static lung volumes (TGV, RV and RV/TLC). The TLC fell by 15.4% but this change was not statistically significant. There were no significant pre- vs post-PPP changes in PaO2 and PaCO2.
Per- and post-operative clinical data
The mean operating time was 150 min (range: 45–240). Fascia closure was possible in 94.8% of cases (n = 18). The prosthesis was an inlay in 38.8% of cases (n = 7), a sublay in 33.3% of cases (n = 6), preperitoneal in 16.6% of cases (n = 3) and an onlay in 11.1% of cases. No prosthesis was implanted in 5.2% of cases (n = 1) (Cloteau-Premont fascioplasty was performed instead). The overall postoperative morbidity rate was 36.8% (Table 5). Two patients developed postoperative compartment syndrome with a bladder pressure of 27 mmHg and 30 mmHg, respectively. Curarization was enough to resolve the compartment syndrome in one case but the other patient required reoperation. Three patients were reoperated (mesenteric infarct due to compartment syndrome; cutaneous necrosis; clinical suspicion of recurrence, respectively). The mean length of stay in the intensive care unit was 3.33 days (range: 0–29). The mean overall length of stay in hospital was 34.4 days (range: 20–68). The mortality rate was 10.5% (n = 2). In the patient reoperated on for compartment syndrome at postoperative day 1, a mesenteric infarct was found during laparotomy and the patient died 24 h later (despite bowel resection). In this patient, post-PPP CT scan and respiratory function tests were performed but the PPP was deflated 48 h before surgery because of cutaneous ulceration; hence, the compartment syndrome could not be considered to be a post-PPP complication. The second patient had a history of COPD and died of postoperative pneumonia.
Discussion
To the best of our knowledge, this is the first prospective study to have evaluated the impact of PPP on peritoneal volumes and respiratory function prior to the treatment of incisional hernias. The PPP is known to have parietal and respiratory effects [10, 21, 22]. The PPP lengthens the muscles but also lengthens the incisional hernia [12] and does not alter the VIH/VP ratio. The procedure does not spontaneously reinstate the herniated volume but increases the likelihood of being able to return the volume to the abdominal cavity. In our series, the VIH increased by 690 cc after PPP (P < 0.01). The VAC increased by 2,021 cc (P < 0.01) and was superior to the mean VIH before PPP (1,420 cc), and roughly equal to the mean volume (2,110 cc) of the VIH after PPP. Before and after PPP, the VIH/VP ratio was 13.9% and 14.9%, respectively (NS). Hence, PPP increases VIH and VAC to the same extent. Although the VIH/VP ratio did not change, the PPP-induced gain in abdominal volume (2,021 cc) was greater than the volume of the incisional hernia (1,420 cc).
PPP decreased most of the dynamic lung volumes but did not change the Tiffeneau ratio. The TLC was not lowered significantly. PPP induced a restrictive syndrome that lacked clinical impact in 95% of cases. Indeed, PPP appears to have the same respiratory effects as surgical treatment of incisional hernias [23]. The progressive nature of the PPP causes respiratory adaptation, whereas there is no adaptation in reinstatement of an incisional hernia. One patient (5%) presented respiratory intolerance; exsufflation was performed and surgical repair was contraindicated. PPP can also be a therapeutic measure. A 25% decrease in vital capacity was reported by Johnson et al. [22]. Several authors have stated that the volume effect of PPP facilitates the reintegration of the herniated volume [21, 24, 25]. The adhesiolytic effect of PPP [24–26] may explain the distribution of air throughout the peritoneal cavity. This result justifies the use of a belt between each PPP session to restrict the spread of air through the hernia, whereas elongation of the incisional hernia by air has been used to facilitate dissection [21, 25]. The operation of IHLD decreases thoracic compliance [6, 7] without changing lung compliance [7]. Surgery can also cause abdominal, four-stroke breathing [27]. PPP alone is not able to restore the thoracoabdominal synergy mentioned by some authors [21] because it increases the VAC and the VIH to the same extent. The addition of a restraining belt is required to limit the abdominal breathing. However, by increasing the intra-abdominal pressure [26], PPP decreases thoracic compliance and progressively prepares the abdominal cavity for reintroduction of the herniated volume. The post-surgery vital capacity is less impaired after preparation by PPP [22]. Trivellini has shown that, to avoid respiratory complications, any increase in intra-abdominal pressure during surgery should be compensated by fasciotomy [6]. There are no surgical techniques for decreasing tension along the suture line [27] but PPP prepares the respiratory function. This pulmonary preparation seems to be vital in patients with IHLD. In addition to having respiratory problems specifically related to the repair of an incisional hernia, the majority of patients are obese [9]. General anesthesia in obese patients causes a greater decrease in chest and lung compliance than in healthy subjects [28]. The respiratory preparation before repair of incisional hernia with loss of domain therefore requires smoking cessation, preparation for PPP with an abdominal belt and respiratory physiotherapy. Tanaka et al. [20] evaluated the peritoneal volume as a predictor of the need to use PPP. They recommended performing a PPP when the VIH/VAC ratio was >25% but did not state the criteria on which this cut-off value was based. Their approach differed from ours, since we used the VIH/VP ratio. Furthermore, their PPP was performed through an indwelling catheter placed in the left hypochondrium. In our study, we introduced a Palmer needle into the abdominal cavity for each session. There were no hollow organ injuries. Possible explanations for the absence of perforation are (1) the loss of domain of bowel loops (leaving a gap in the abdominal cavity and thus reducing the risk of hollow organ injury), and (2) our careful analysis of the pre-PPP CT scan results in general and the position of the bowel in particular. Tanaka et al. injected CO2, whereas we preferred to injected air in view of the volatile nature of CO2 known in laparoscopy and the resulting loss of gas (Table 6). Intraperitoneal reabsorption, dissemination and compression caused an intraperitoneal air loss rate of 47% over 16.5 days with 2,021 cc of air remaining in the abdominal cavity immediately before surgery. The peritoneum has a high reabsorption capacity. The daily peritoneal fluid reabsorption rate varies from 1.5 to 2.5 L/day, whereas gas reabsorption increases to 38–42 L/min with CO2 [29] and decreases in cases of high intraperitoneal pressure [29]. This result prompted us to insufflate air rather than CO2 and to insufflate a larger volume of air, in order to increase the efficiency of the PPP. In the series using air, mean volumes of 7–23 L [24, 25] were insufflated over 6–21 days [13, 25, 26, 30]. Nitrogen oxide can be used to insufflate greater volumes (23–35 L) [30] but the gas has a high reabsorption rate.
In the present prospective study, we found a cutaneous complication rate of 15.8%. There was only one case of compartment syndrome—the major problem in IHLD repair. Kingsnorth et al. [16] found a cutaneous complications rate of 34.6% but did not analyze pulmonary complications. In a prospective evaluation of the postoperative complications of open versus laparoscopic ventral repair, Kaafarani et al. [31] found a complication rate at 8 weeks of 47.9% in the open repair group. The latter study included patients with small, medium-sized and large incisional hernia. These results underline the underestimation of postoperative morbidities caused by retrospective evaluation. Moreover, only two sets of postoperative clinical data are available for IHLD repair. In the 23-patient series reported by Tanaka et al. [32] (using PPP), there were two deaths (8.7%) and 6 wound infections (26%) but no complications related to PPP catheter implantation. In the 19-patient series described by Agnew et al. [33] (using the components separation technique), one patient (5.3%) died of an ischemic stroke, one patient developed pneumonia (5.3%), three patients developed wound infections (15.8%) and two patients developed seroma (10.5%). We are not aware of any prospective study having compared PPP and the components separation technique. PPP increased the abdominal volume and the incisional hernia volume to the same extent. Although the VIH/VP ratio did not change, the PPP-induced gain in abdominal volume (2,021 cc) was greater than the volume of incisional hernia (1,420 cc). PPP leads to a generally well-tolerated, progressive restrictive syndrome. In terms of volumes and respiratory parameters, PPP is a preparation for reintegration of an IHLD. The goal of peritoneal volume determination is to anticipate intra and post-operative problems for IHLD and could be considered as a stress test before IHLD repair. Recent publications on the subject attest to the growing interest in this preparation [9, 19]. In conclusion, PPP increases the volume of the abdomen, and thus facilitates reintegration of the bowel into the abdomen. By inducing a progressive, restrictive syndrome, PPP prepares the lung for bowel reintegration. Prolongation of hospitalization is the major limitation of this approach. The next step in studying the PPP could be the use of volume criteria to predict tension-free fascia closure.
References
Korenkov M, Paul A, Sauerland S, Neugebauer E, Arndt M, Chevrel JP, Corcione F, Fingerhut A, Flament JB, Kux M, Matzinger A, Myrvold HE, Rath AM, Simmermacher RK (2001) Classification and surgical treatment of incisional hernia. Results of an experts’ meeting. Langenbecks Arch Surg 386:65–73
Rives J, Chevrel JP, Caix M (1987) Surgery of the abdominal wall. In: Rives J, Chevrel JP, Caix M (eds) Hernias and surgery of the abdominal wall. Springer, Berlin, pp 116–143
Dabbas N, Adams K, Pearson K, Royle G (2011) Frequency of abdominal wall hernias: is classical teaching out of date? JRSM Short Rep 2:5
Stoppa R, Ralaimiaramanana F, Henry X, Verhaeghe P (1999) Evolution of large ventral incisional hernia repair. The French contribution to a difficult problem. Hernia 3:1–3
Lowe JB 3rd, Lowe JB, Baty JD, Garza JR (2003) Risks associated with “components separation” for closure of complex abdominal wall defects. Plast Reconstr Surg 111:1276–1283
Trivellini G, Zanella G, Danelli PG, Pratolongo D, Ferri O (1984) Surgical treatment of large eventrations. Study of a technic adapted to disorders of respiratory compliance. Chirurgie 110:116–122
Munegato G, Grigoletto R, Brandolese R (2000) Respiratory mechanics in abdominal compartment syndrome and large incisional hernias; a study of 41 patients. Hernia 4:282–285
Cady B, Brooke-Cowden GL (1976) Repair of massive abdominal wall defects. Combined use of pneumoperitoneum and Marlex mesh. Surg Clin North Am 56:559–570
Paajanen H, Laine H (2005) Operative treatment of massive ventral hernia using polypropylene mesh: a challenge for surgeon and anesthesiologist. Hernia 9:62–67
Dumont F, Fuks D, Verhaeghe P, Brehant O, Sabbagh C, Riboulot M, Yzet T, Regimbeau JM (2009) Progressive pneumoperitoneum increases the length of abdominal muscles. Hernia 13:183–187
Goni Moreno I (1971) Pneumoperitoneum applied to the surgical preparation of large chronic eventrations. Prensa Med Argent 58:1037–1041
Koontz AR, Graves JW (1954) Preoperative pneumoperitoneum as an aid in the handling of gigantic hernias. Ann Surg 140:759–762
Mayagoitia JC, Suarez D, Arenas JC, Diaz de Leon V (2006) Preoperative progressive pneumoperitoneum in patients with abdominal-wall hernias. Hernia 10:213–217
Forrest J (1979) Repair of massive inguinal hernia: with pneumoperitoneum and without using prosthetic mesh. Arch Surg 114:1087–1088
Stoppa R, Louis D, Verhaeghe P, Henry X, Plachot JP (1987) Current surgical treatment of post-operative eventrations. Int Surg 72:42–44
Kingsnorth AN, Sivarajasingham N, Wong S, Butler M (2004) Open mesh repair of incisional hernias with significant loss of domain. Ann R Coll Surg Engl 86:363–366
Okamoto E, Kyo A, Yamanaka N, Tanaka N, Kuwata K (1984) Prediction of the safe limits of hepatectomy by combined volumetric and functional measurements in patients with impaired hepatic function. Surgery 95:586–592
Dello SA, van Dam RM, Slangen JJ, van de Poll MC, Bemelmans MH, Greve JW et al (2007) Liver volumetry plug and play: do it yourself with ImageJ. World J Surg 31:2215–2221
Wigmore SJ, Redhead DN, Yan XJ, Casey J, Madhavan K, Dejong CH et al (2001) Virtual hepatic resection using three-dimensional reconstruction of helical computed tomography angioportograms. Ann Surg 233:221–226
Tanaka EY, Yoo JH, Rodrigues AJ Jr, Utiyama EM, Birolini D, Rasslan S (2010) A computerized tomography scan method for calculating the hernia sac and abdominal cavity volume in complex large incisional hernia with loss of domain. Hernia 14:63–69
Goni Moreno I (1978) The rational treatment of hernias and voluminous chronic eventrations: Preparation with progressive pneumoperitoneum. Lippincott, Philadelphia
Johnson WC (1972) Preoperative progressive pneumoperitoneum in preparation for repair of large hernias of the abdominal wall. Am J Surg 124:63–68
De Santis L, Frigo F, Bruttocao A, Terranova O (2003) Pathophysiology of giant incisional hernias with loss of abdominal wall substance. Acta Biomed 74:34–37
Astudillo R, Merrell R, Sanchez J, Olmedo S (1986) Ventral herniorrhaphy aided by pneumoperitoneum. Arch Surg 121:935–936
Barst HH (1972) Pneumoperitoneum as an aid in the surgical treatment of giant herniae. Br J Surg 59:360–364
Coelho JC, Brenner AS, Freitas AT, Campos AC, Wiederkehr JC (1993) Progressive preoperative pneumoperitoneum in the repair of large abdominal hernias. Eur J Surg 159:339–341
Rives J, Pires JC, Flament JB, Palot JP (1987) Major incisional hernia. In: Chevrel JP (ed) Surgery of the abdominal wall. Springer, Berlin, pp 116–144
Pelosi P, Croci M, Ravagnan I, Tredici S, Pedoto A, Lissoni A et al (1998) The effects of body mass on lung volumes, respiratory mechanics, and gas exchange during general anesthesia. Anesth Analg 87:654–660
Tan PL, Lee TL, Tweed WA (1992) Carbon dioxide absorption and gas exchange during pelvic laparoscopy. Can J Anaesth 39:677–681
Connolly DP, Perri FR (1969) Giant hernias managed by pneumoperitoneum. JAMA 209:71–74
Kaafarani H, Hur K, Campasano M, Reda D, Itani K (2009) Classification and valuation of postoperative complications in a randomized trial of open versus laparoscopic ventral herniorraphy [abstract 221]. Hernia 13(Suppl 1):S69
Tanaka EY, Yoo JH, Rodrigues AJ Jr, Utiyama EM, Birolini D, Rasslan S (2010) A computerized tomography scan method for calculating the hernia sac and abdominal cavity volume in complex large incisional hernia with loss of domain. Hernia 14:63–69
Agnew SP, Small W Jr, Wang E, Smith LJ, Hadad I, Dumanian GA (2010) Prospective measurements of intra-abdominal volume and pulmonary function after repair of massive ventral hernias with the components separation technique. Ann Surg 251:981–988
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sabbagh, C., Dumont, F., Fuks, D. et al. Progressive preoperative pneumoperitoneum preparation (the Goni Moreno protocol) prior to large incisional hernia surgery: volumetric, respiratory and clinical impacts. A prospective study. Hernia 16, 33–40 (2012). https://doi.org/10.1007/s10029-011-0849-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-011-0849-2