Abstract
Induction of preoperative progressive pneumoperitoneum is an elective procedure in patients with hernias with loss of domain. A prospective study was carried out from June 2003 to May 2005 at the Hospital de Especialidades, Instituto Mexicano del Seguro Social, Leon, Mexico. Preoperative progressive pneumoperitoneum was induced using a double-lumen intraabdominal catheter inserted through a Veress needle and daily insufflation of ambient air. Variables analyzed were age, sex, body mass index, type, location and size of defective hernia, number of previous repairs, number of days pneumoperitoneum was maintained, type of hernioplasty, and incidence of complications. Of 12 patients, 2 were excluded because it was technically impossible to induce pneumoperitoneum. Of the remaining 10 patients, 60% were female and 40% were male. The patients’ average age was 51.5 years, average body mass index was 34.7, and evolution time of their hernias ranged from 8 months to 23 years. Nine patients had ventral hernias and one had an inguinal hernia. Pneumoperitoneum was maintained for an average of 9.3 days and there were no serious complications relating to the puncture or the maintenance of the pneumoperitoneum. One patient who previously had undergone a mastectomy experienced minor complications. We were able to perform hernioplasty on all patients, eight with the Rives technique, one with supra-aponeurotic mesh, and one using the Lichtenstein method for inguinal hernia repair. One patient’s wound became infected postoperatively. Preoperative progressive pneumoperitoneum is a safe procedure that is easy to perform and that facilitates surgical hernia repair in patients with hernia with loss of domain. Complications are infrequent, patient tolerability is adequate, and the proposed modification to the puncture technique makes the procedure even safer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Induction of preoperative progressive pneumoperitoneum to treat very large hernias with loss of domain was introduced in l940 by Goñi Moreno [1]. Later, Herszage, Berlemont, Koontz, Gravez, and Martínez Munive [2] reported several interesting modifications of the original method. Preoperative progressive pneumoperitoneum is recommended for patients with giant hernias and a large amount of viscera in the hernial sac, when it would not otherwise be possible to perform the hernioplasty [3, 4] or when forced reduction of the hernia might cause the patient to develop abdominal compartmental syndrome postoperatively [5].
The function of the abdominal wall is to contain and protect the viscera, to help activate trunk movements and to assist with evacuation and urination. Equally important is the regulation of diaphragmatic movements for adequate pulmonary ventilation [3]. When a patient’s hernia has a large sac, holding large quantities of viscera, changes occur in the mesentery, the intestines, the subcutaneous cellular tissue, and the skin that enfolds the sac. Venous and lymphatic returns are reduced because of the compression caused by the fibrotic ring or hernial defect on the loops that protrude outside the cavity. This causes an edematous, thick intestine, and mesentery which makes its reduction difficult. Under pressure, the subcutaneous cellular tissue deviates laterally, leaving the skin excessively distended, with impaired circulation and a tendency to atrophy. In advanced cases, this can lead to ulcerated zones that will be difficult to regenerate and are a site for chronic infections. Because of humidity and continual friction, bacterial and mycotic infections occur in the folds that form in the normal abdomen and the hernial skin.
Hernias with loss of domain also cause progressive contractions of the abdominal muscles due to lack of viscera and reduces the pressure and capacity of the abdominal cavity. As more intestines leaves the sac, intraabdominal pressure lessens, decreasing the hemidiaphragm and altering ventilatory equilibrium, which causes both inspiratory and expiratory restriction [3].
In patients with hernias with loss of domain, induction of preoperative progressive pneumoperitoneum corrects some of these problems, principally by enlarging the abdominal cavity to contain the protruding intestinal contents so that hernioplasty can be performed [3, 4] without risk of posterior compartmental syndrome [5]. Larger series of patients have undergone this procedure with good results by insufflating oxygen, carbon dioxide [6], or, in the original method developed by Goñi, ambient air filtered through siphon bottles containing iodopovidone [1]. Martínez Munive [2] installed in the abdominal cavity the type of double-lumen catheter used for subclavian puncture, then insufflated with ambient air with a syringe. This procedure was performed without complications.
Objective
We report our experience with induction of preoperative progressive pneumoperitoneum via a double-lumen catheter. Inserting a reusable Veress needle in the peritoneal cavity as a guide for the initial puncture and a pathway for the metallic guide of the subclavian catheter increases safety by reducing the possibility of visceral lesions at the time of puncture.
Methods
A prospective study was carried out from June 2003 to May 2005 at the Specialty Hospital (UMAE) No. 1, Medical Center of León, Guanajuato, Mexico, which is a third-level medical facility of the Instituto Mexicano del Seguro Social. Patients with inguinal, ventral, and incisional abdominal-wall hernias were selected during outpatient surgical consultations with the three participating surgeons. All patients had hernias with loss of domain, in which the volume of the sac and visceral contents was greater than the capacity of the abdominal cavity. Patients received a preoperative electrocardiogram and underwent a spirometer test as well as routine preoperative laboratory tests. All patients of the study were advised and gave their informed consent for the pneumoperitoneum procedure and the hernioplasty.
Puncture technique
After each patient had fasted for 6 h, we determined where to make the puncture based on the locations of previous incisions and possible adhesion-free spaces (in some patients assisted by ultrasonography), preferably in the left hypochondrium under the edge of the ribs. Simple lidocaine was applied at 1 or 2%, and the abdominal puncture was made with a reusable Veress needle. After the insertion of the needle, a proof was made with aspiration and the free flow of the physiologic solution. Ambient air was insufflated through the needle toward the abdominal cavity. We used a 50-cc syringe in quantities of 100 cc to detach any adhesions or intestinal loops near to the Veress needle. Then, the internal part of the needle was disassembled to enable the passage of the flexible metallic guide of the central catheter. Once the metallic guide was inserted in the cavity, the needle was completely removed, and the catheter was inserted using the Seldinger technique. Once in the cavity, the catheter was affixed to the skin. A three-way key was placed in the distal lumen of the catheter, and insufflation of the cavity began with ambient air. Either 1,000 or 4,000 cc were insufflated, depending on when the patient confirmed the sensation of abdominal fullness. Monitoring was done with a sphygmomanometer connected to the other lumen of the catheter to ensure that intraabdominal pressure did not exceed 15 mm Hg. Once the initial insufflation was completed, we confirmed the success of the pneumoperitoneum by taking a teleradiograph of the thorax while the patient was in a supine or sitting position. Daily insufflations were administered in quantities of 1,000–2,000 cc, according to patient tolerance, for 7–10 days in patients with inguinal hernias or 9–15 days in patients with ventral hernias. At the end of this period, the patient underwent the surgical procedure and during the procedure the pneumoperitoneum catheter was removed. Oral antibiotic therapy with cephalosporins or third-generation quinolones was administered at induction of the pneumoperitoneum. Metoclopramide, 10 mg every 8 h was also given, as well as an analgesic, when necessary. The surgical technique of wall repair with polypropylene mesh was performed according to the criteria of the surgeon (Figs. 1, 2, 3, 4).
Study variables and statistical analysis
Study variables were age, sex, weight, body mass index (BMI), and type, location and size of hernia. Also, number of previous hernioplasties, the number of days the pneumoperitoneum was maintained, incidence of complications due to puncture or pneumoperitoneum, and hernia-repair technique were considered.
For statistical analysis, measures of central tendency were calculated. Dispersion was used for the numeric variables and frequency tables were used for the descriptive variables.
Results
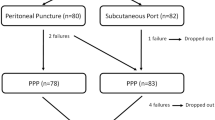
During a period of 23 months, 12 patients with large hernias with loss of domain were seen for consultation. Two patients were excluded from the study because it was not possible to induce pneumoperitoneum. Of the 10 remaining patients, 6 (60%) were female, and 4 (40%) were male. Average age was 51.5 years (range 41–66 years), and average BMI was 34.7. The longest time of evolution of the hernia was 23 years and the shortest time was 8 months (Table 1).
Two patients had pathological history of type 2 diabetes mellitus and arterial hypertension, one patient had atherosclerosis, one patient had a permanent colostomy due to Fournier’s syndrome, and another patient had a history of breast cancer, which had been treated with right mastectomy, chemotherapy, and radiotherapy 6 months previously.
Eight patients (80%) had incisional hernias, 1 patient (10%) had an inguinal hernia, and 1 patient (10%) had a primary umbilical hernia. Six patients (60%) had undergone previous hernia repairs. One patient had previously undergone 12 hernioplasties. Only one patient developed a deep infection of the abdominal wall after a previous hernioplasty.
All patients were hospitalized for induction of preoperative progressive pneumoperitoneum. The average time of pneumoperitoneum was 9.3 days (range 7–15 days). In the two patients who had undergone multiple laparotomies, the puncture was done without mishap, but, upon insufflation of air only partial distension of the abdomen was achieved because of adhesions. We attempted a puncture in two different locations at the abdominal site with the same results. Therefore, we decided to continue the surgery without inducing the pneumoperitoneum. These two patients were excluded from the study.
No patients, including the two excluded from the study, experienced complications related to the puncture or maintenance of the pneumoperitoneum. Discomfort related to the procedure included epigastric pain, a sensation of gastric fullness, and early satiation, which diminished with administration of analgesics and metoclopramide. One patient had moderate subcutaneous emphysema of the thorax and neck without systemic repercussions or discomfort. In no case was it necessary to terminate the pneumoperitoneum. The patient who had undergone right mastectomy had a dissection on the inferior cutaneous flap of the major pectoral and bleeding in the healing zone, but this did not require medical or surgical treatment.
The average size of the hernial ring in ventral and incisional hernias was 290.9 cm2 (range 176–490 cm2). In the case of the inguinal region, the size was comparatively much smaller (7 cm).
In eight patients, pneumoperitoneum was sufficient to reintroduce the loops into the cavity and perform an adequate hernioplasty. In one patient, the visceral reintroduction was incomplete, but it permitted hernioplasty with supra-aponeurotic mesh. In 8 patients (80%) with incisional hernias, the Rives technique with a transcutaneous fixing was used, and in 1 patient (10%), supra-aponeurotic mesh onlay was performed, because of the difficulty in reintroduction of the loops in complete form. In 1 patient (10%) with an inguinal hernia, the Lichtenstein method was used. Only two additional procedures were performed; in the patient with the permanent colostomy we dismantled the colostomy and reimplanted in another site distant from the hernial area and in a patient with a giant uterine fibroma we performed a hysterectomy. No other complications occurred during the procedures.
The postoperative hospital stay average was 2.3±0.9 days (range 1–4 days). There were no immediate postoperative complications. One patient developed a deep surgical wound infection 8 d after discharge. The infection was treated with antibiotic therapy and daily irrigation with saline solution, without removal of the mesh.
Discussion
Abdominal-wall hernias with large hernial sacs retaining a large quantity of intestinal loops for a long period of time are extremely difficult to repair. These hernias are said to have “loss of domain” because the contents of the hernia exceed the capacity of the abdominal cavity. The forced reduction of these hernias can lead to insufficient respiration, abdominal compartmental syndrome, or even inability to complete the hernioplasty.
To resolve this problem, induction of a progressive pneumoperitoneum has been carried out preoperatively for more than 60 years. As described by some authors [2–4], maintenance of the pneumoperitoneum increases the capacity of the retracted abdominal cavity, performs a pneumatic lysis of intestinal adhesions, and improves diaphragmatic function.
Created by Goñi Moreno [1–3] in the 1940s, this procedure has since been modified, making it simpler to apply. One of the first proposed modifications was to replace the laborious procedure of introducing ambient air with the siphon system, insufflation of oxygen, carbon dioxide (though it is rapidly reabsorbed), or natural ambient air. One of the most significant modifications was reported by Martínez Munive [2]. In place of a thick catheter, the authors used a thin-double-lumen catheter of the type used in subclavian punctures, thereby decreasing the incidence of infection. We propose to further modify this technique to avoid visceral injuries. In our modification, the initial puncture is made with a Veress needle and through it the Seldinger procedure is performed for the placement of the catheter. Caldironi [6] used the Veress needle to introduce carbon dioxide through a laparoscopic insufflator, then immediately removed the needle. Our technique eliminates the inconvenience of having to make daily punctures, which increase the risk to the patient and produce very rapid absorption of carbon dioxide, possibly resulting in a decrease of abdominal distention in less than 24 h.
As is common, our patients had long-term hernias, and 60% of patients had undergone multiple previous hernioplasties. BMI plays an important role, 75% of patients were classified as either overweight or morbidly obese. In our patients, most hernias were located in the midline, one patient had a parastomal hernia and another had an inguinal hernia. Although, it has been reported that this procedure can be performed on an outpatient basis, because they were our first patients to undergo induction of pneumoperitoneum, we preferred that they be admitted to inpatient care. The modification we suggested above facilitates the introduction of the needle and the catheter and we did not observe any complications during this stage or during the daily introduction of ambient air, like visceral puncture, peritonitis, or air embolism. In patients with inguinal hernias, pneumoperitoneum was maintained for 7 days; in patients with ventral or incisional hernias, the duration varied from 7 to 15 days, in accordance with the dimensions of the hernial sac in relation to the abdominal cavity. As has been shown in other studies [1–4, 6], patient discomfort during maintenance of the pneumoperitoneum was minimal to moderate and it was not necessary to terminate the procedure due to patients’ discomfort. Only two minor complications occurred. One patient developed subcutaneous emphysema in the chest and neck and the patient who had previously undergone mastectomy had overstretching of the skin and bleeding of the scar with no consequences other than pain. In neither of these cases was it necessary to suspend the insufflation.
In nine patients, induction of preoperative progressive pneumoperitoneum sufficiently reduced intestinal loops and the Rives procedure with preperitoneal mesh was performed [7]. In one case, the reduction was incomplete, but it was possible to place supra-aponeurotic mesh (onlay) without difficulty [8]. In the patient with an inguinal hernia, Lichtenstein-type hernioplasty [9] was performed. In the patient with the parastomal hernia, the permanent colostomy was removed and reinserted on the opposite side of the abdomen.
There was only one postoperative complication. A patient with diabetes mellitus developed an abscess on the abdominal wall that was treated with debridement and cleaning; it was not necessary to remove the mesh. The patient with the colostomy, whose surgical treatment was considered to be clean contaminated, had seropurulent material through a point of the suture without any noticeable manifestation of infection or abscess of the abdominal wall. The patient recovered satisfactorily without any special treatment.
Preparing a hernia for surgical treatment by inducing preoperative progressive pneumoperitoneum facilitates dissection of the hernial sac and its contents due to the preoperative lysis of adhesions by the insufflated air [4]. Herzage et al. also report a spontaneous dissection of the gallbladder from the hepatic bed during maintenance of pneumoperitoneum. In addition, preparing a hernia with progressive pneumoperitoneum allowed us to locate other hernias or weak zones that were not evident in the initial physical exploration of the abdominal wall. The increased facility of performing a tension-free repair was notable, in ease of reintroducing the contents from the sac to the abdominal cavity and of closing the skin flaps of the abdominal wall. Dissection of the retromuscular plane for the placement of the prosthesis was made easier. Adequate tolerance for the reintroduction of the viscera into the abdominal cavity was also observed during immediate postsurgical evolution of patients who did not present hemodynamic or ventilatory complications.
Finally, we report that some high-risk patients who have been advised in the past not to elect hernia repair are now able to undergo the procedure with the use of preoperative progressive pneumoperitoneum.
Conclusions
Progressive preoperative pneumoperitoneum is safe and easy to apply. It is indicated in patients with hernias with loss of domain to facilitate tension-free surgical repair. The incidence of complications is low, patient tolerance is adequate, and our proposed modification of the puncture technique makes the procedure even safer.
References
Goñi-Moreno I (1947) Chronic eventrations and large hernias: preoperative treatment by progressive pneumoperitoneum—original procedure. Surgery 22:945–953
Martínez MA, Quijano OF, Padilla LR, Hesiquio SR, Álvarez CO, Medina RO (2002) Catéter de doble luz para neumoperitoneo en hernias gigantes. Informe de cuatro pacientes. Cir Gen 24:313–318
Willis S, Schumpelick V (2000) Use of Pneumoperitoneum in the repair of giant hernias. Hernia 4:105–111
Herszage L (2003) Abordaje de las eventraciones de pared. In: Mayagoitia JC (ed) Hernias de la pared abdominal. Tratamiento actual, 1st. edn. McGraw-Hill, Mexico, pp 201–212
Munegato G, Grigoletto R, Brandolese R (2000) Respiratory mechanics in abdominal compartement syndrome and large incisional hernias of the abdominal wall. Hernia 4:282–285
Caldironi MW, Romano M, Bozza F (1990) Progresive pneumoperitoneum in the management of giant incisional hernias; a study of 41 patients. Br J Surg 77:306–308
Mayagoitia GJC, Cisneros MHA, Suarez FD (2003) Hernioplastia de pared abdominal con técnica de Rives. Cir Gral 25:19–24
Correa RA, Canals RPP, Mederos CON, Roselló FJR, Esperón NR, Mustafá GLR (2002) Reparación de Hernias incisionales grandes con malla supraaponeurótica. Rev Cubana Cir 41:156–163
Amid PK (1998) The Lichtenstein open tension-free hernioplasty. Cir Gen 20 (Supl 1):17–20
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mayagoitia, J.C., Suárez, D., Arenas, J.C. et al. Preoperative progressive pneumoperitoneum in patients with abdominal-wall hernias. Hernia 10, 213–217 (2006). https://doi.org/10.1007/s10029-005-0040-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-005-0040-8