Abstract
The reported incidence of trocar site hernias in bariatric surgery ranges between 0.5 and 3%. The best available evidence derives from retrospective studies analysing prospective databases, thus including only patients who presented with symptoms or received surgical treatment due to trocar site hernias after a laparoscopic bariatric procedure. A systematic literature research was conducted up until September 2017. Search strategies included proper combinations of the MeSH terms ‘laparoscopy’ and ‘bariatric surgery’, ‘trocar/port’ and ‘hernia’. Searches were not limited by publication type or language. The review was registered in PROSPERO (ID 85102) and performed according to the PRISMA guidelines. Sixty-eight publications were included. Pooled hernia incidence was 3.22 (range 0–39.3%). Thirteen trials reported systematic closure of the fascia; 12 trials reported no closure. Data availability did not allow for pooling to calculate relative risk. Higher BMI and specific hernia examination using imaging modalities were associated with a significantly higher incidence of trocar site hernias. Studies dedicated to detection of TsH reported a pooled incidence of 24.5%. Trocar site hernias are an underestimated complication of minimally invasive multiportal bariatric surgery. While high-quality trials are not available allowing for a precise calculation of the incidence, existing data are indicative of very high incidence rates. Risk factors for developing a trocar site hernia in bariatric surgery have not yet been systematically analysed. Prospective studies in this field are necessary.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Obesity has become the new pandemic with more than 37% of the American population affected, according to the United States Ministry of Health [1]. Since the introduction of surgical treatment, bariatric procedures have become one of the most popular types of surgery, with more than 47.000 procedures performed in the UK between 2013 and 2015 [2].
With consideration for the standardisation and reproducibility of bariatric procedures, efforts are being made to reduce surgical morbidities. Apart from the classic complications of bariatric surgery, trocar site hernias (TsH) are clearly an underrepresented problem, particularly as they usually develop months or years after surgery and are often at first asymptomatic. Most of the studies that report long-term results after bariatric surgery present various emergency cases of strangulated trocar site hernias while the actual prevalence remains unknown [3, 4] and asymptomatic or oligosymptomatic patients rarely present.
A further concern is the closure of the fascia and its potential effect on the development of trocar site hernias. Evidence in non-bariatric populations supports the approach of closing the fascia in incisions larger than 10 mm [5]; however, there are case presentations describing incisional hernia risk even with trocars smaller than 5 mm [6].
Clinical examination of trocar wounds has proven to be unreliable for the evaluation of trocar site hernias in obese patients [7]. Recent prospective trials assessed sonography and CT scans for the detection of abdominal wall defects after surgery in obese patients [7, 8]. The results considering the incidence of incisional hernias are concerning and highlight the urgency of further investigations.
We conducted a systematic review and pooled analysis to evaluate the actual incidence of trocar site hernias after bariatric procedures and in order to understand the role of fascia closure in the development of trocar site hernias.
Materials and Methods
The systematic review and pooled analysis was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. The objective of the analysis was to estimate the prevalence of trocar site hernias (TsH) in the bariatric population and assess the role of fascia closure and its possible impact on the development of TsH.
All studies reporting on the incidence of TsH in bariatric patients were included. Since the actual prevalence of the TsH in the bariatric population remains unknown, studies were included regardless of the number of patients. Case reports, reviews and technical trials, studies in paediatric patients and conference abstracts of unpublished data were excluded. Studies evaluating uniportal surgical approaches, single-incision laparoscopies and natural orifice techniques were also not included.
Systematic Literature Research
The following databases were searched by a specialised clinical librarian (MG) up through 22 September 2017: Current Contents Medicine, The Cochrane Library, Cinahl, ClinicalTrial.gov, WHO ICTRP and the Web of Science Core Collection Index. Search strategies included proper combinations of the MeSH terms and text words related to three aspects: ‘laparoscopy’ and ‘bariatric surgery’ and ‘trocar/port’ and ‘hernia’. The search was not limited by publication type and there were no restrictions on language. The exact search terms can be provided on reasonable request. The review was registered in the PROSPERO registry for systematic reviews and meta-analyses (ID 85102).
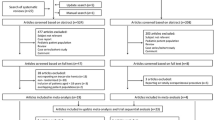
The database search provided 2718 references. After removing duplicates, 1669 references were available for reviewing. Two independent reviewers (authors 1 and 2) hand-searched the references to assess the publications for eligibility. The citations of the initially included references were hand-screened as well in order to further identify relevant publications, through which 83 additional references were found. One hundred ninety-five full-text articles were assessed for eligibility, and 68 articles were ultimately included in the qualitative analysis (Fig. 1). The abstracts of articles in languages other than English were translated accordingly and assessed for eligibility. The table of the included references can be found in the appendix (Table 1).
The same reviewers independently performed the extraction of the data from the included studies. The findings of the two independent reviewers were controlled for concordance. Disagreements were resolved with discussion and intense analysis of the trials and the data. In order to provide and analyse as much data as possible, original authors were contacted via e-mail. In case no valid e-mail address was available, a thorough web-based search and contact through social media was attempted.
The incidence of TsH was estimated as the proportion of patients who developed a trocar site hernia relative to the total number of patients included in the trial. We did not perform a quality assessment of the data, since all the included studies are of low or very low quality.
Statistics
The weighting of the various trials was based on four factors: study design, targeted hernia examination during the follow-up, mean follow-up and number of patients included in the trial. The scoring and allocation of points for the study design was as follows: four for randomised controlled trials, three for prospective, non-randomised studies, two for retrospective studies with prospective database and one for retrospective studies. Considering the routine performance of a targeted hernia examination during the follow-up visits, studies in which patients were routinely examined for hernia-associated symptoms with the use of an imaging modality (CT, MRI or ultrasound scans) were given three points. Studies where only a targeted clinical examination was performed were scored two points, and studies where no specific hernia examination was performed with one point. In case no data was available, the study was rated with a score of zero. Relative frequency was calculated for each factor. The relative frequencies were additionally weighted with percentages of 40, 30, 20 or 10. The study design was weighted with 40%, targeted hernia examination with 30%, follow-up with 20% and number of patients with 10%.
Usual validated weighting algorithms could not be used because of the notable heterogeneity of the included trials and the numerous parameters that were included in the weighting process. An additional factor restricting the implementation of validated weighting tools was the retrospective character of most trials included in the present analysis. The abovementioned algorithm was developed at the Institute of Medical Statistic and Biomathematics of our University in order to allow for the analysis of multiple weighted factors using the SAS software and to minimise the risk of bias.
All statistical calculations were performed using SAS software, version 9.3 (SAS Institute Inc., Cary, NC, USA). Quantitative, approximately normally distributed parameters are presented using mean values and standard deviations; for skewed data, median and range are provided. The median values of two subgroups were compared using the Mann-Whitney U test. Statistical significance has been assumed for p values less than 0.05.
Results
Sixty-eight studies were included in the qualitative analysis. One study was a randomised control trial, nine studies were prospective, 21 studies retrospectively analysed prospectively collected data and 37 studies were retrospective series. Study exclusion was performed according to the aforementioned criteria.
The final analysis included 31.516 patients. The mean follow-up was 18.56 months (range 0–96 months). The pooled hernia incidence was 3.22% (range 0–39.3%, SD 8.19). In order to better assess the influence of fascia closure on the development of trocar site hernias, all corresponding authors were contacted by e-mail. The response rate leading to additional data was 25% (17/68).
The role of the body mass index (BMI) in the development of TsH was available for analysis. Studies with a mean patient BMI > 45 kg/m2 reported significantly higher pooled incidence of TsH compared to studies with a mean patient BMI < 45 kg/m2 (5.26 vs 0.50%, p = 0.015, Fig. 2).
Furthermore, we performed an analysis of methods for trocar site hernias diagnosis and how various studies approached the follow-up for trocar site hernias. In 42 studies, data concerning how follow-up was performed were not available. In 10 studies, no specific follow-up concerning trocar site hernias was performed. In 11 studies, patients were clinically examined for the presence of TsH and 5 studies systematically used imaging modalities (CT or sonography scans) during follow-up evaluation for trocar site hernias.
Studies where clinical examination was used to detect TsH did not demonstrate a higher pooled TsH incidence compared to studies where no examination was performed. However, the use of an imaging modality was associated with a significantly higher pooled incidence of TsH compared to no examination at all (16.22 vs 1.28%, p = 0.04). A comparison of studies that used imaging and studies that used only clinical examination revealed a higher pooled incidence in the imaging group, without reaching statistical significance (16.22 vs 1.37%, p = 0.06, Fig. 3).
We also evaluated the aspect of the follow-up interval. The included studies were divided into two groups: a group where mean follow-up was longer than 12 months and a second group where follow-up was shorter than 12 months (34 studies were included in each group). Studies with a follow-up interval after 12 months had significantly higher pooled TsH incidence compared to studies reporting a follow-up of less than 12 months (4.59 vs 0.8%, p = 0.023, Fig. 4).
Fascia Closure
In the present analysis, we considered the role of fascia closure in the development of trocar site hernias. The primary hypothesis was that a lack of fascia closure would be associated with a higher incidence of trocar site hernias.
Before weighting the studies, we compared TsH incidence in trials that reported not closing the fascia and trials where the fascia was routinely closed. Interestingly, trials reporting systematic closure of the fascia were associated with a significantly higher incidence of TsH compared to studies where the fascia was not closed (1.26 vs 0.76%, p = 0.02). After weighting of the included studies, the trend of higher incidence rates associated with fascia closure persisted, but this difference was no longer significant (fascia closure 1.13% versus no fascia closure 0.77%, Figs. 5 and 6).
Furthermore, we evaluated specific trocar characteristics in order to identify particular risk factors for the development of trocar site hernias. The only factor where sufficient data for analysis were available was the size of the trocar. Data from 25 trocar hernias could be analysed. No hernias could be detected in the 5-mm trocars, one hernia developed in a 10-mm trocar, 14 hernias in the 11- or 12-mm trocars, one hernia in a 13-mm trocar and nine hernias in the 15-mm extraction trocars after sleeve gastrectomies. As for the hernia associated with the 10-mm trocar, the fascia had not been closed during the operation. In 12 of 14 cases of TsH in the 11-/12-mm trocars, the fascia had not been sutured and in two cases, closure had been performed. Fascia suturing was also performed during the case associated with the 13-mm TsH. As for the hernias reported following the use of the 15-mm trocars, in four cases, fascia closure had been performed and in three cases, the fascia was not closed. In two cases, data concerning the fascia closure were not available. Data regarding the placement of the trocar and the anatomical position (transrectal vs. lateral pararectal placement, cutting vs. non-cutting trocars) were not available for analysis.
Discussion
We performed a systematic literature research in order to identify the actual incidence of trocar site hernias after laparoscopic multiportal bariatric procedures. The literature research provided 1752 references, of which 68 were included based on the aforementioned inclusion and exclusion criteria.
One of the main objectives of this analysis was to clarify the role of fascia closure in the bariatric patient and its possible influence on the development of TsH. Before weighting the studies, we found—contrary to our expectations—a higher incidence of TsH in studies where the fascia had been routinely closed. After weighting and sorting the trials based on quality, the tendency for a higher incidence in trials where the fascia was closed persisted; however, it was no longer significant.
Furthermore, we considered hernia development and fascia closure with regard to trocar size. Data from 25 hernias were available. No hernias were detected with the 5-mm trocars and only one hernia arose when using a 10-mm trocar, so no recommendations can be provided for the 5-mm and 10-mm trocars concerning fascia closure. Analysis of larger trocar sites indicated 14 hernias associated with the use of the 11-/12-mm trocars, with 12 cases where the fascia was not closed. Consequently, fascia closure when using the 11-/12-mm trocars can be considered. This finding contradicts the initial frequency distribution, which pointed to a higher incidence of hernias in cases where the fascia had been closed. Data for trocars larger than 12 mm remain controversial and therefore do not allow for any recommendations concerning intraoperative fascia closure.
After implementing the aforementioned scoring for the included studies, we calculated a pooled incidence of 3.2%. A particularly interesting factor we further assessed was the intention to detect trocar site hernias. Unfortunately, data regarding how the follow-up was performed could only be acquired in 26 studies, so the present analysis clearly underestimates the actual incidence of trocar site hernias. In 10 of the remaining 26 studies, no specific hernia examination during the follow-up period was performed, resulting in a pooled hernia incidence of 6.9% in the studies where the authors ‘searched for a hernia’. Taking our results as well as earlier evidence into account [7], it can be safely postulated that clinical examination is not suitable for detecting an asymptomatic or oligosymptomatic trocar hernia in the obese patient. Furthermore, a careful analysis of the five included studies where an imaging modality was primarily used for hernia detection proved to be frustrating [7, 8, 64, 71, 72]. Arru et al. analysed the incidence of TsH in a prospective feasibility three-port sleeve gastrectomy study in 25 patients without finding any cases of TsH [71]. However, imaging was performed only 3 months after surgery. In another study, Rossi et al. reviewed all patients after laparoscopic Roux-en-Y gastric bypass (LRYGB) who received a CT scan for any reason and reported an incidence of 0.81% [64].
In contrast, there are three studies where the authors intentionally looked for TsH using imaging. Rebibo et al. reviewed 228 patients who received a CT scan in order to evaluate for TsH after sleeve gastrectomy, with a mean follow-up of 27 months. The authors reported an incidence of 18.8% [72]. Ahlqvist et al. examined the trocar insertion sites in 26 asymptomatic patients after LRYGB using CT scans and found hernias in 15.4% of cases after a mean follow-up of 33 months [7]. In a further study, Scozzari et al. used sonography scans to examine 150 patients after LRYGB with a mean follow-up of 30 months and described a TsH incidence of 39.3%, which is also the highest rate reported thus far [8]. A calculation of TsH incidence in the only three studies where a hernia was the primary outcome results in a rate of 24.5%.
Conclusion
Long-term follow-up data from non-bariatric population define obesity as a major risk factor for developing trocar site hernias [73]. The results of the current analysis clearly indicate that trocar site hernias are a massively underestimated problem in bariatric surgery. The pooled incidence was 3.2%; however, the actual rate probably lies closer to the 24.5% calculated above. Patients with a higher BMI seem to be at greater risk for developing a hernia. Coexisting morbidities and operation-associated factors cannot be adequately analysed in a multivariate setting because of insufficient data. The role of fascia closure remains complicated, but closure when using trocars larger than 10 mm can be considered.
A major limiting factor in this analysis is that the majority of the trials included are heterogeneous, retrospective studies reporting either short- or long-term results of bariatric surgery that focus primarily on weight loss or other surgical complications. Trocar hernias are mostly reported as emergency operations during the follow-up period that occurred in the same setting where the bariatric procedure was performed. Therefore, the incidence provided in the vast majority of the included studies heavily underestimates the actual numbers. Prospective studies are urgently needed. Our group is currently planning a prospective randomised trials hoping to clarify the role of fascia closure in the development of trocar site hernias.
Limitations
As previously noted, most studies included in this analysis were not dedicated to detecting hernias after bariatric procedures and only three included studies have TsH as their primary outcome. The reason for including all studies was moreover to highlight the underrepresentation of this major issue in the bariatric literature. A further limitation is the implementation of a self-made scoring system in the present review, possibly increasing the risk of bias in this study. The reason for its use was the lack (to the best of our knowledge) of an alternative validated scoring system that could incorporate all assessed parameters.
Change history
21 April 2020
The review was not registered for systematic reviews and meta-analyses, and should be disregarded.
References
Flegal KM, Kruszon-Moran D, Carroll MD, et al. Trends in obesity among adults in the United States, 2005 to 2014. JAMA. 2016;315(21):2284–91.
Welbourn R, Pournaras DJ, Dixon J, et al. Bariatric surgery worldwide: baseline demographic description and one-year outcomes from the second IFSO global registry report 2013–2015. Obes Surg. 2018;28(2):313–22.
Anwar M, Collins J, Kow L, et al. Long-term efficacy of a low-pressure adjustable gastric band in the treatment of morbid obesity. Ann Surg. 2008;247(5):771–8.
Zehetner J, Holzinger F, Triaca H, et al. A 6-year experience with the Swedish adjustable gastric band prospective long-term audit of laparoscopic gastric banding. Surg Endosc. 2005;19(1):21–8.
Kadar N, Reich H, Liu CY, et al. Incisional hernias after major laparoscopic gynecologic procedures. Am J Obstet Gynecol. 1993;168(5):1493–5.
Bergemann JL, Hibbert ML, Harkins G, et al. Omental herniation through a 3-mm umbilical trocar site: unmasking a hidden umbilical hernia. J Laparoendosc Adv Surg Tech A. 2001;11(3):171–3.
Ahlqvist S, Bjork D, Weisby L, et al. Trocar site hernia after gastric bypass. Surg Technol Int. 2017;30:170–4.
Scozzari G, Zanini M, Cravero F, et al. High incidence of trocar site hernia after laparoscopic or robotic Roux-en-Y gastric bypass. Surg Endosc. 2014;28(10):2890–8.
Mendoza D, Newman RC, Albala D, et al. Laparoscopic complications in markedly obese urologic patients (a multi-institutional review). Urology. 1996;48(4):562–7.
Maietta P, Milone M, Coretti G, et al. Retrieval of the gastric specimen following laparoscopic sleeve gastrectomy. Experience on 275 cases. Int J Surg. 2016;28(Suppl 1):S124–7.
Weiner R, Wagner D, Bockhorn H. Laparoscopic gastric banding for morbid obesity. J Laparoendosc Adv Surg Tech A. 1999;9(1):23–30.
Corcelles R, Boules M, Froylich D, et al. Laparoscopic three-port sleeve gastrectomy: a single institution case series. J Laparoendosc Adv Surg Tech A. 2016;26(5):361–5.
Ternamian AM, Deitel M. Endoscopic threaded imaging port (EndoTIP) for laparoscopy: experience with different body weights. Obes Surg. 1999;9(1):44–7.
Chakhtoura G, Zinzindohoue F, Ghanem Y, et al. Primary results of laparoscopic mini-gastric bypass in a French obesity-surgery specialized university hospital. Obes Surg. 2008;18(9):1130–3.
Bonatti H, Hoeller E, Kirchmayr W, et al. Ventral hernia repair in bariatric surgery. Obes Surg. 2004;14(5):655–8.
Scopinaro N, Marinari GM, Camerini G. Laparoscopic standard biliopancreatic diversion: technique and preliminary results. Obes Surg. 2002;12(3):362–5.
Susmallian S, Ezri T, Charuzi I. Laparoscopic repair of access port site hernia after lap-band (R) system implantation. Obes Surg. 2002;12(5):682–4.
Shoar S, Aboutaleb S, Karem M, et al. Comparison of two specimen retrieval techniques in laparoscopic sleeve gastrectomy: what is the role of endobag? Surg Endosc. 2017;31:4883–7.
DeMaria EJ, Sugerman HJ, Kellum JM, et al. Results of 281 consecutive total laparoscopic Roux-en-Y gastric bypasses to treat morbid obesity. Ann Surg. 2002;235(5):640–5. discussion 645–647
Mizrahi I, Alkurd A, Ghanem M, et al. Outcomes of laparoscopic sleeve gastrectomy in patients older than 60 years. Obes Surg. 2014;24(6):855–60.
Chevallier JM, Zinzindohoue F, Douard R, et al. Complications after laparoscopic adjustable gastric banding for morbid obesity: experience with 1,000 patients over 7 years. Obes Surg. 2004;14(3):407–14.
Zinzindohoue F, Chevallier JM, Douard R, et al. Laparoscopic gastric banding: a minimally invasive surgical treatment for morbid obesity: prospective study of 500 consecutive patients. Ann Surg. 2003;237(1):1–9.
Triantafyllidis G, Lazoura O, Sioka E, et al. Anatomy and complications following laparoscopic sleeve gastrectomy: radiological evaluation and imaging pitfalls. Obes Surg. 2011;21(4):473–8.
Antanavicius G, Sucandy I. Robotically-assisted laparoscopic biliopancreatic diversion with duodenal switch: the utility of the robotic system in bariatric surgery. J Robot Surg. 2013;7(3):261–6.
Loy JJ, Youn HA, Schwack B, et al. Safety and efficacy of laparoscopic adjustable gastric banding in patients aged seventy and older. Surg Obes Relat Dis. 2014;10(2):284–9.
Rubin M, Benchetrit S, Lustigman H, et al. Laparoscopic gastric banding with Lap-Band for morbid obesity: two-step technique may improve outcome. Obes Surg. 2001;11(3):315–7.
Wang W, Wei PL, Lee YC, et al. Short-term results of laparoscopic mini-gastric bypass. Obes Surg. 2005;15(5):648–54.
Marema RT, Perez M, Buffington CK. Comparison of the benefits and complications between laparoscopic and open Roux-en-Y gastric bypass surgeries. Surg Endosc. 2005;19(4):525–30.
Wiesner W, Schob O, Hauser RS, et al. Adjustable laparoscopic gastric banding in patients with morbid obesity: radiographic management, results, and postoperative complications. Radiology. 2000;216(2):389–94.
Derici S, Atila K, Bora S, et al. Simple, safe, and cost-effective technique for resected stomach extraction in laparoscopic sleeve gastrectomy. Gastroenterol Res Pract. 2016; Article ID 7090128, 4 pages, 2016.
Schauer PR, Ikramuddin S, Gourash W, et al. Outcomes after laparoscopic Roux-en-Y gastric bypass for morbid obesity. Ann Surg. 2000;232(4):515–29.
Casella G, Soricelli E, Fantini A, et al. A time-saving technique for specimen extraction in sleeve gastrectomy. World J Surg. 2010;34(4):765–7.
Regan JP, Inabnet WB, Gagner M, et al. Early experience with two-stage laparoscopic Roux-en-Y gastric bypass as an alternative in the super-super obese patient. Obes Surg. 2003;13(6):861–4.
Gibson SC, Le Page PA, Taylor CJ. Laparoscopic sleeve gastrectomy: review of 500 cases in single surgeon Australian practice. ANZ J Surg. 2015;85(9):673–7.
Chiu CC, Lee WJ, Wang W, et al. Prevention of trocar-wound hernia in laparoscopic bariatric operations. Obes Surg. 2006;16(7):913–8.
Bou Nassif G, Scetbun E, Lecurieux-Lafayette C, et al. “Hand-over-hand grasping technique”: a fast and safe procedure for specimen extraction in laparoscopic sleeve gastrectomy. Obes Surg. 2017;27(5):1391.
Sanchez-Pernaute A, Perez-Aguirre E, Botella AG, et al. Prophylactic closure of trocar orifices with an intraperitoneal mesh (ventralex((R))) in laparoscopic bariatric surgery. Obes Surg. 2008;18(11):1489–91.
Arias E, Martinez PR, Ka Ming Li V, et al. Mid-term follow-up after sleeve gastrectomy as a final approach for morbid obesity. Obes Surg. 2009;19(5):544–8.
Szold A, Abu-Abeid S. Laparoscopic adjustable silicone gastric banding for morbid obesity: results and complications in 715 patients. Surg Endosc. 2002;16(2):230–3.
Coskun H, Bozbora A, Ogunc G, et al. Adjustable gastric banding in a multicenter study in Turkey. Obes Surg. 2003;13(2):294–6.
Keidar A, Carmon E, Szold A, et al. Port complications following laparoscopic adjustable gastric banding for morbid obesity. Obes Surg. 2005;15(3):361–5.
Hans PK, Guan W, Lin S, et al. Long-term outcome of laparoscopic sleeve gastrectomy from a single center in mainland China. Asian J Surg. 2017 April 17; [Epub ahead of print]. Accessed on 07/06/2017. Available at: https://doi.org/10.1016/j.asjsur.2017.04.003.
Belachew M, Belva PH, Desaive C. Long-term results of laparoscopic adjustable gastric banding for the treatment of morbid obesity. Obes Surg. 2002;12(4):564–8.
Patel S, Szomstein S, Rosenthal RJ. Reasons and outcomes of reoperative bariatric surgery for failed and complicated procedures (excluding adjustable gastric banding). Obes Surg. 2011;21(8):1209–19.
Higa KD, Boone KB, Ho T. Complications of the laparoscopic Roux-en-Y gastric bypass: 1,040 patients--what have we learned? Obes Surg. 2000;10(6):509–13.
Armstrong J, O'Malley SP. Outcomes of sleeve gastrectomy for morbid obesity: a safe and effective procedure? Int J Surg. 2010;8(1):69–71.
Nocca D, Krawczykowsky D, Bomans B, et al. A prospective multicenter study of 163 sleeve gastrectomies: results at 1 and 2 years. Obes Surg. 2008;18(5):560–5.
Parikh MS, Fielding GA, Ren CJ. U.S. experience with 749 laparoscopic adjustable gastric bands: intermediate outcomes. Surg Endosc. 2005;19(12):1631–5.
Lakdawala M, Agarwal A, Dhar S, et al. Single-incision sleeve gastrectomy versus laparoscopic sleeve gastrectomy. A 2-year comparative analysis of 600 patients. Obes Surg. 2015;25(4):607–14.
Sakran N, Raziel A, Goitein O, et al. Laparoscopic sleeve gastrectomy for morbid obesity in 3003 patients: results at a high-volume bariatric center. Obes Surg. 2016;26(9):2045–50.
Major P, Janik MR, Wysocki M, et al. Comparison of circular- and linear-stapled gastrojejunostomy in laparoscopic Roux-en-Y gastric bypass: a multicenter study. Wideochir Inne Tech Maloinwazyjne. 2017;12(2):140–6.
Balsiger BM, Ernst D, Giachino D, et al. Prospective evaluation and 7-year follow-up of Swedish adjustable gastric banding in adults with extreme obesity. J Gastrointest Surg. 2007;11(11):1470–6. discussion 1446–1447
Lattuada E, Zappa MA, Mozzi E, et al. Injection port and connecting tube complications after laparoscopic adjustable gastric banding. Obes Surg. 2010;20(4):410–4.
van Dielen FM, Soeters PB, de Brauw LM, et al. Laparoscopic adjustable gastric banding versus open vertical banded gastroplasty: a prospective randomized trial. Obes Surg. 2005;15(9):1292–8.
Himpens J, Dobbeleir J, Peeters G. Long-term results of laparoscopic sleeve gastrectomy for obesity. Ann Surg. 2010;252(2):319–24.
Frezza EE, Reddy S, Gee LL, et al. Complications after sleeve gastrectomy for morbid obesity. Obes Surg. 2009;19(6):684–7.
Aly MYF, Lee WJ. Letter to the editor: trocar site hernia prevention in laparoscopic bariatric surgery. Obes Surg. 2016;26(9):2227–8.
Michalik M, Lech P, Bobowicz M, et al. A 5-year experience with laparoscopic adjustable gastric banding--focus on outcomes, complications, and their management. Obes Surg. 2011;21(11):1682–6.
Coblijn UK, de Raaff CA, van Wagensveld BA, et al. Trocar port hernias after bariatric surgery. Obes Surg. 2016;26(3):546–51.
Rosenthal RJ, Szomstein S, Kennedy CI, et al. Direct visual insertion of primary trocar and avoidance of fascial closure with laparoscopic Roux-en-Y gastric bypass. Surg Endosc. 2007;21(1):124–8.
Higa KD, Ho T, Boone KB. Laparoscopic Roux-en-Y gastric bypass: technique and 3-year follow-up. J Laparoendosc Adv Surg Tech A. 2001;11(6):377–82.
Sucher R, Resch T, Mohr E, et al. Single-incision laparoscopic sleeve gastrectomy versus multiport laparoscopic sleeve gastrectomy: analysis of 80 cases in a single center. J Laparoendosc Adv Surg Tech A. 2014;24(2):83–8.
Lee M, Nam EJ, Kim S, et al. Two-port access laparoscopic surgery in gynecologic oncology. Int J Gynecol Cancer. 2013;23(5):935–42.
Rossi A, McLaughlin D, Witte S, et al. An expanded retrospective review of trocar site hernias in laparoscopic gastric bypass patients. J Laparoendosc Adv Surg Tech A. 2017;27(6):633–5.
Dresel A, Kuhn JA, Westmoreland MV, et al. Establishing a laparoscopic gastric bypass program. Am J Surg. 2002;184(6):617–20. discussion 620
Johnson WH, Fecher AM, McMahon RL, et al. VersaStep trocar hernia rate in unclosed fascial defects in bariatric patients. Surg Endosc. 2006;20(10):1584–6.
Toouli J, Kow L, Collins J, et al. Efficacy of a low-pressure laparoscopic adjustable gastric band for morbid obesity: patients at long term in a multidisciplinary center. Surg Obes Relat Dis. 2008;4(3 Suppl):S31–8.
Catheline JM, Fysekidis M, Bachner I, et al. Five-year results of sleeve gastrectomy. J Visc Surg. 2013;150(5):307–12.
Pilone V, Di Micco R, Hasani A, et al. Trocar site hernia after bariatric surgery: our experience without fascial closure. Int J Surg. 2014;12(Suppl 1):S83–6.
Puzziferri N, Austrheim-Smith IT, Wolfe BM, et al. Three-year follow-up of a prospective randomized trial comparing laparoscopic versus open gastric bypass. Ann Surg. 2006;243(2):181–8.
Arru L, Azagra JS, Goergen M, et al. Three-port laparoscopic sleeve gastrectomy: feasibility and short outcomes in 25 consecutives super-obese patients. Cir Esp. 2013;91(5):294–300.
Rebibo L, Dhahri A, Chivot C, et al. Trocar site hernia after laparoscopic sleeve gastrectomy using a specific open laparoscopy technique. Surg Obes Relat Dis. 2015;11(4):791–6.
Erdas E, Dazzi C, Secchi F, et al. Incidence and risk factors for trocar site hernia following laparoscopic cholecystectomy: a long-term follow-up study. Hernia. 2012;16(4):431–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
All authors declare that they have no conflict of interest.
Ethical Approval Statement
For this type of study, formal consent is not required.
Informed Consent Statement
Does not apply.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Karampinis, I., Lion, E., Grilli, M. et al. Trocar Site Hernias in Bariatric Surgery—an Underestimated Issue: a Qualitative Systematic Review and Meta-Analysis. OBES SURG 29, 1049–1057 (2019). https://doi.org/10.1007/s11695-018-03687-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-018-03687-2