Abstract
Purpose
Since the first description, the use of polypropylene mesh in hernia repair has gained wide acceptance. The aim of this study was to assess whether polypropylene mesh implantation has any effects on femoral blood vessels.
Methods
A 0.5 × 1.0 cm polypropylene mesh was inserted into the rat femoral artery and vein on the right side. After 14, 28 and 90 days, the rats were reoperated. The meshes were excised for histological processing. Blood flow in the dorsum of the foot skin, femoral artery and vein were measured in all groups before mesh implantation and at 14, 28, and 90 days after mesh implantation.
Results
Following placement of mesh graft on vascular structures, inflammation and fibrosis developed to a varying degree depending on the time elapsed. On the other hand, fibrosis did not change the histological structure of vessels. There was a decrease in both arterial and venous circulation due to the pressure of the graft.
Conclusions
These data suggest that fibrosis due to mesh graft can negatively affect blood flow in vessels due to mechanical pressure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inguinal herniorrhaphy is one of the most common operations performed in general surgery clinics [1]. Herniorrhaphy can be performed using several different open or laparascopic methods. Since the introduction of the use of prosthetic mesh, preperitoneal or on-lay implantation of polypropylene mesh in hernia repair has gained wide acceptance. The tension-free mesh repairs are associated with lower recurrence rates than non-mesh methods [2]. Prosthetic mesh induces an acute inflammatory response followed by chronic foreign-body reaction. This reaction creates scar tissue and increases the strength of the implant area [3].
Depending on the surgical technique, polypropylene mesh is in contact with the surrounding structures. Previous studies have demonstrated the effects of polypropylene mesh on surrounding tissue, leading to symptoms such as chronic pain (mesh inguinodynia), organ erosion and urological complications due to contact between the mesh and the spermatic cord [4–6]. In posterior repairs of inguinal hernias, the polypropylene mesh is placed preperitoneally to the posterior wall of the inguinal canal. This procedure can be done both laparoscopically and openly. Preperitoneal mesh plug femoral hernioplasty also effects reliable repair of femoral hernias [7]. In both posterior repairs of inguinal hernias with mesh and preperitoneal mesh plug femoral hernioplasty, the mesh is in close contact with the major vessels of this area. However, there is little information on the effects of polypropylene mesh these major vessels.
This study was designed to assess whether polypropylene mesh implantation has any effects on femoral blood vessels.
Materials and methods
Animal model
The study was approved by the Faculty Animal Ethics Committee at our institution.
Thirty male Wistar albino rats weighing 250–300 g were housed under diurnal lighting conditions (12 h darkness and 12 h light) and fasted overnight; free access to water was allowed before the experiment. Animal housing, care, and application of experimental procedures were all done in accordance with the Guidelines for Care and Use of Laboratory Animals, published by the National society for Medical Research and the National Institutes of Health.
Study protocol
Blood flow of femoral artery, femoral vein and dorsum of the foot skin were monitored by laser Doppler flowmetry (Laser Doppler flowmeter, MP100 Biopac Systems, Santa Barbara, CA). Data was analysed with the programme AcqKnowledge for Windows V.3.5.7 for MP 100 system (Biopac Systems) and minimum values of blood flow measured as beam per unit (BPU) were taken as blood flow value.
The animals were fixed in the supine position. The inguinal area was shaved and the skin disinfected using 10% povidone-iodine solution. The operating area was covered by sterile cloths. All operations were carried out under heat lamps in order to maintain body temperature constant at 35–36°C, and were all carried out by the same surgeon using the same aseptic and sterile technique.
Anaesthesia was attained by intraperitoneal injection of 80 mg/kg body weight ketamine (Ketalar®, Parke Devis, Eczacibasi, Istanbul) and 8 mg/kg body weight xylazine (Rompun®, Bayer Turk Kimya San, Sti., Istanbul). 50 mg/kg cefazoline (Cefamezin, Eczacıbaşı) as prophylactic antibiotherapy was administered intraperitoneally before surgery.
Rats were divided in three groups: Group A (n = 10), Group B (n = 10), Group C (n = 10). Before the operation, blood flow of the dorsum of the foot skin was measured in all groups. In all animals, the inguinal areas were explored bilaterally through inguinal incision. The femoral artery, femoral vein and femoral nerve were identified, and blood flow of the femoral artery and femoral vein were measured for 1 min in both sides. After measurement of blood flow, a 0.5 × 1.0 cm polypropylene mesh (Prolen®, Ethicon, Somerville, NJ) was laid on only one side and fixed to the quadriceps femoris fascia covering the femoral artery, femoral vein and nerve by means of two sutures (5/0 polypropylene, Prolene®, Ethicon). The contra-lateral side of each animal was dissected and the femoral artery, femoral vein and femoral nerve identified, but no mesh was placed on this side.
After 14 days (Group A), 28 days (Group B) or 90 days (Group C), the rats were reoperated. Before the operation, blood flow of the dorsum of the foot skin was measured again in all groups bilaterally. Femoral artery, femoral vein and femoral nerve were identified again on both sides. Blood flow of the femoral artery was measured 5 mm distal to the mesh and blood flow of the femoral vein was measured 5 mm proximal to the mesh in the right side. The same measurements were performed on the other side. Blood flow in arteries, veins and skin was compared, both in terms of postoperative versus preoperative values, and also mesh implanted versus sham implantation. After the measurements, the subjects were sacrificed with high-dose sodium thiopental. The meshes including femoral artery, femoral vein and femoral nerve in the right side, and only the femoral artery, femoral vein and femoral nerve in the left side, were excised for histological processing.
Histological tissue processing
Samples were fixed in 10% formaldehyde. Samples were dehydrated by immersion in a series of alcohol concentrations and embedded in paraffin. The 3–5 μm sections were stained with haematoxylon and eosin (H&E). Representative cross-sections were examined under a light microscope.
Statistical analysis
SPSS for Windows version 16.0 (SPSS, Chicago, IL) was used for statistical evaluation. Data were compared by chi-square and Kruskall–Wallis tests, and one way ANOVA. If the P-value from these latter tests was statistically significant, Wilcoxon signed ranks test was used for further analysis. A P value ≤0.05 was regarded as statistically significant.
Results
During the study, no mortality or infective complications were seen in the subjects.
Macroscopic aspects
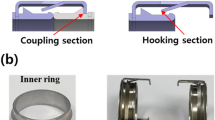
At re-operation, there was a marked adherence of the mesh to the surrounding structures in all subjects in which mesh was implanted. On the contra-lateral side (without mesh) of these animals no adherence was noted. The degree of fibrosis in group C was greater than groups A and B (Fig. 1).
Microscopic evaluation
Chronic inflammatory and foreign body reactions were seen on the mesh implanted side in all subjects. Fourteen days after mesh implantation (Group A), a low grade inflammation associated with an increase in cell count and oedema developed around the artery, vein and peripheric nerves (Fig. 2a). During this period no effect of mesh on vascular structures was observed. There was no development of connective tissue that might cause fibrosis. No histological change was seen on the sham side.
Interface mesh-recipient tissue. N Nerve, A arteria, V vein, M polypropylene mesh graft, CT connective tissue. a 14 days after the mesh implantation (Group A): note low grade inflammation around the vascular structure and nerve (original magnification ×5, H&E staining), b 28 days after mesh implantation (Group B): a thin connective tissue septum appeared between the vessels and mesh along with organised thin collagen fibres (original magnification ×10, H&E staining), c 90 days after mesh implantation (Group C): more intense fibrous tissue with increased and more organised collagen fibres (original magnification ×5, H&E staining)
Twenty-eight days after mesh implantation (Group B), a thin connective tissue septum developed between the vessels and mesh, and in this area cell count increased and thin collagen fibers were more organised (Fig. 2b). There was no effect of mesh on the vascular structures. No histological change was seen in the sham side.
Ninety days after mesh implantation (Group C), fibrosis was more intense in the mesh implanted group when compared with the other groups, but no histological change was seen in the vessel wall and intima (Fig. 2c). No histological change was seen in the sham side.
Arterial and venous blood flow evaluation
Postoperative venous blood flow was significantly lower in the mesh implanted side when compared with preoperative values in group A (P < 0.05) but no statistically significant change was seen in the flow of arteries, veins and skin when comparing the mesh implanted versus sham group.
Postoperative arterial blood flow was reduced in the mesh implanted side compared with the sham group in group B (P < 0.05) but no change in venous and skin blood flow was observed due to mesh.
Postoperative arterial blood flow was significantly lower in the mesh implanted side when compared not only with preoperative values but also with the sham group in group C (P = 0.005, P < 0.05, respectively) and there was no change in the venous and skin blood flow. When the total data of the 30 subjects was assessed, postoperative blood flows of both arteries and veins were significantly lower in the mesh implanted side (P = 0.012, P = 0.009, respectively).
The results of arterial, venous and skin blood flow are shown in Table 1.
Discussion
After the first anatomical repair of an inguinal hernia by the German surgeon Vinzenz von Czerny [8], different kinds of procedures for the management of inguinal hernias have been defined. Although prosthetic polypropylene mesh implantation has become the preferred surgical treatment for inguinal hernia, there are an increasing number of reports concerning complications after prosthetic polypropylene mesh implantation. Meshes should strengthen the abdominal wall without the reduction in mobility that is associated with scar formation as a result of the inflammatory reaction due to a chronic foreign-body reaction [3, 9, 10]. Mesh repairs are associated with low recurrence rates; on the other hand, complications such as wound infection, chronic pain (mesh inguinodyna), adhesion, organ erosion and testicular atrophy, spermatocel, painful ejaculation, and sensitivity of the testis can be seen in mesh repairs [4–6]. Despite the well known effects of mesh contraction-fibrotic reaction on the spermatic cord and peripheral nerves [11, 12], there are few data about the effects on femoral vessels [13, 14]. We aimed to evaluate the local effects of mesh on femoral vessels in our study.
Mesh inguinodyna is chronic pain developing after herniorraphy. It is possibly secondary to chronic scarring or neuroma formation. Demirer et al. demonstrated that inflammatory and fibrotic reaction may cause adhesions and mechanical compression of peripheral nerves, which is associated with myelin degeneration, endoneurinal and perineurial edema, thickening of collagen layers around axons and axonal loss that may cause chronic inflammatory demyelinative peripheral neuropathy [12]. Thus, placement of mesh in direct contact with inguinal nerves is not recommended in order to avoid groin pain [15].
Recent clinical and experimental evidence show the effects of mesh structures within the spermatic cord. Long-lasting pain during copulation, spermatoceles, spermatic granuloma, azospermia secondary to inguinal vasal obstruction and testicular venous congestion after polypropylene mesh herniorrhaphy have been reported [6, 16–19]. Morphological and functional changes are due to adhesions between the mesh and the structures of the spermatic cord as a result of the foreign body reaction [19]. On the other hand, Uzzo et al. observed no significant differences regarding testicular volume, temperature, blood flow, and vasograms between mesh and they did not detect erosion or stenosis of the cord structures due to the mesh [20].
The first study associated with the flow in femoral vessels after hernia repair with mesh published in this field was by Taylor et al. [13]. Patients underwent unilateral inguinal hernia repair with mesh by open or laparoscopic methods followed up a median of 3 years; afterwards, doppler ultrasonography was performed to determine the diameters and haemodynamic characteristics of the testis and femoral vessels. No difference was found in testicular blood flow, volume or echogenicity between open and laparascopic repair or the contralateral side. Also, the dimensions and blood flows of the femoral artery and vein were similar in all groups. A similar study by Özmen et al. demonstrated no significant change in femoral vessel diameter and blood flow after preperitoneal mesh replacement during open or laparoscopic hernia repair. Also, deep vein thrombosis was not observed in any of the patients [14].
In our study, a reduction in arterial blood flow was observed as 7.5% postoperatively on the 28th day and as 36.7% postoperatively on the 90th day of the placement of mesh on femoral vessels. A significant reduction in venous flow was observed in postoperative values compared with preoperative values in the mesh implanted side in group A, but no statistically significant change was seen in the flow of veins in mesh implanted compared to sham group in any of the groups. When the arterial flows were compared between the mesh implanted side and sham operated side, a significant reduction was found in arterial flow on the 28th day and 90th day in the mesh implanted group. No significant difference was found in venous and skin blood flows between mesh implanted and sham operated groups. The following question may arise: if a reduction in arterial flow was observed, why was a similar result not observed in venous flow?. The answer might be the small number of subjects in each group; when the total data was assessed (n = 30), the postoperative blood flow of both the artery and the vein was found to be decreased significantly compared to preoperative blood flow in the mesh implanted group (P = 0.012, P = 0.009, respectively).
We think that the reduction in blood flow observed in our study was due to mechanical pressure. Fibrosis was more intense microscopically and macroscopically on the 90th day of the placement of mesh as compared to the 14th day. But no change was observed in vessel wall structure, intima and diameters. The increase in fibrosis with time might explain the decrease in blood flow with time.
Conclusions
The results of this study add fibrosis due to mesh graft that can negatively effect the blood flow in vessels due to mechanical pressure to the negative effects of meshes reported in the surgical literature. Studies are being performed to develop new prosthetic materials because no prosthetic material that causes no reaction as an inside tissue has yet been found.
References
Rutkow IM, Robbins AW (1993) Demographic, classificatory, and socioeconomic aspects of hernia repair in the United States. Surg Clin North Am 73:413–426
Lichtenstein IL, Shulman AG, Amid PK (1989) The tension free hernioplasty. Am J Surg 157:188–193
Beets GL, Go PM, van Mameren H (1996) Foreign body reactions to monofilament and braided polypropylene mesh used as preperitoneal implants in pigs. Eur J Surg 162:823–825
Malekpour F, Mirhashemi SH, Hajinasrolah E, Salehi N, Khoshkar A, Kolahi AA (2008) Ilioinguinal nerve excision in open mesh repair of inguinal hernia—results of a randomized clinical trial: simple solution for a difficult problem? Am J Surg 195:735–740
Lo DJ, Bilimoria KY, Pugh CM (2008) Bowel complications after prolene hernia system (PHS) repair: a case report and review of the literature. Hernia 12:437–440
Langenbach M, Schmidt J, Lazika M, Zirngibl H (2003) Urological symptoms after laparoscopic hernia repair. Reduction with a variant of polypropylene mesh. Urologe 42:375–381
Robbins AW, Rutkow IM (1998) Repair of femoral hernias with ‘‘plug’’ technique. Hernia 2:73–75
Von Czerny V (1877) Studien zur radikalbehandlung der hernien. Wien Med Wochenschr 27:497 528,554,578
Klinge U, Klosterhalfen B, Conze J, Limberg W, Obolenski B, Ottinger AP, Schumpelick V (1998) Modified mesh for hernia repair that is adapted to the physiology of the abdominal wall. Eur J Surg 164:951–960
Klosterhalfen B, Klinge U, Schumpelick V (1998) Functional and morphological evaluation of different polypropylene-mesh modifications for abdominal wall repair. Biomaterials 19:2235–2246
Junge K, Binnebösel M, Rosch R, Ottinger A, Stumpf M, Mühlenbruch G, Schumpelick V, Klinge U (2008) Influence of mesh materials on the integrity of the vas deferens following Lichtenstein hernioplasty: an experimental model. Hernia 12:621–626
Demirer S, Kepenekci I, Evirgen O, Birsen O, Tuzuner A, Karahuseyinoglu S, Ozban M, Kuterdem E (2006) The effect of polypropylene mesh on ilioinguinal nerve in open mesh repair of groin hernia. J Surg Res 131:175–181
Taylor SG, Hair A, Baxter GM, O’Dwyer PJ (2001) Does contraction of mesh following tension free hernioplasty effect testicular or femoral vessel blood flow? Hernia 5:13–15
Ozmen MM, Ozalp N, Zulfikaroglu B, Soydinc P, Ziraman I, Hengirmen S (2004) The evaluation of the peak flow velocity and cross-sectional area of the femoral artery and vein following totally extraperitoneal vs preperitoneal open repair of inguinal hernias. Hernia 8:332–335
Callesen T, Bech K, Kehlet H (1999) Prospective study of chronic pain after groin hernia repair. Br J Surg 86:1528–1531
Silich RC, McSherry CK (1996) Spermatic granuloma. An uncommon complication of the tension-free repair. Surg Endosc 10:537–539
Shin D, Lipshultz LI, Goldstein M, Barmé GA, Fuchs EF, Nagler HM, McCallum SW, Niederberger CS, Schoor RA, Brugh VM III, Honig SC (2005) Herniorrhaphy with polypropylene mesh causing inguinal vassal obstruction: a preventable cause of obstructive azoospermia. Ann Surg 241:553–558
Peiper C, Junge K, Klinge U, Strehlau E, Ottinger A, Schumpelick V (2006) Is there a risk of infertility after inguinal mesh repair? Experimental studies in the pig and the rabbit. Hernia 10:7–12
Peiper C, Junge K, Klinge U, Strehlau E, Krones C, Ottinger A, Schumpelick V (2005) The influence of inguinal mesh repair on the spermatic cord: a pilot study in the rabbit. J Invest Surg 18:273–278
Uzzo RG, Lemack GE, Morrissey KP, Goldstein M (1999) The effects of mesh bioprosthesis on the spermatic cord structures: a preliminary report in a canine model. J Urol 161:1344–1349
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sulaimanov, M., Genc, V., Cakmak, A. et al. The effects of polypropylene mesh on femoral artery and femoral vein in mesh repair. Hernia 14, 629–634 (2010). https://doi.org/10.1007/s10029-010-0724-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-010-0724-6