Abstract
Background
In Edinburgh a group of surgeons agreed to convert to a lightweight, composite mesh (Ultrapro—Ethicon) for totally extraperitoneal (TEP) inguinal hernia surgery. The aim of this study was to compare the outcome following the use of a new lightweight vs a standard heavyweight mesh during TEP hernia repair.
Methods
Patients undergoing TEP using lightweight (LWM) or heavyweight meshes (HWM) between March 2004 and March 2006 were identified from the Lothian Surgical Audit database. The patients who re-presented with recurrence of hernia were studied in greater detail. Date of re-attendance at a clinic with recurrence was used as a surrogate for date of recurrence.
Results
Two hundred and fifty one patients had 371 hernia repairs with LWM. A total of 16 (4.3%) recurred with a median follow-up of 14.5 months. A concurrent group of 326 patients had 425 repairs with standard mesh and have had 12 (2.82%) recurrences with a median follow-up of 22.4 months. A group of patients operated immediately prior to the introduction of LWM consisted of 328 patients who had 436 repairs using HWM, of whom 13 (2.98%) have recurred with a median follow-up of 43 months. Whilst there are no statistically significant differences in recurrence rates between these groups, we are concerned that the LWM group has the highest recurrence rate despite the shortest follow-up.
Conclusion
In view of increased patient comfort, we continue to recommend LWM for laparoscopic inguinal hernia surgery but would recommend that, in larger hernias and possibly for all, the surgeon should improve mesh adhesion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There is growing interest in the use of lighter weight meshes (LWM) for all types of hernia repair based upon predicted benefits when compared with heavyweight mesh (HWM). These include accelerated recovery with less post-operative pain [1] and earlier return to normal activity [2], increased patient comfort with reduced mesh awareness [3] and less chronic pain [4–6] with improved quality of life [3, 7, 8]. Claims are also made for a decreased tendency to shrink due to reduced intensity of collagenisation with a possible reduction in late recurrence and increased resistance to infection [9]. Use of lightweight mesh to avoid parastomal hernia in the presence of severe peritoneal contamination has been reported [10]. However, surgeons may be wary of using a material of reduced strength with a perceived risk of increased recurrence but may be reassured by the knowledge that even the lightest of meshes available are still three times stronger than a human abdominal wall. However, this concern can only be heightened by early reports suggesting that increased recurrence has occurred with LWM although suggesting this may be due to technical errors in fixation [6, 11].
A group of surgeons in Edinburgh were sufficiently impressed by the predicted benefits of lightweight mesh to agree to change to the use of lightweight, composite, polypropylene, monocryl-coated mesh (Ultrapro—Ethicon) for routine inguinal hernia surgery by both laparoscopic and open repair. Other surgeons did not wish to change current practice and remained with HWM as we have shown previously that we have a low incidence of chronic pain after totally extraperitoneal (TEP) repair [12]. Surgeons also agreed to audit their results in terms of patient comfort and recurrence rates. Initially, LWM was not always available and therefore HWM was used. We have published an early study of chronic pain, mesh awareness and activity levels, which confirms many benefits of LWM over standard mesh. This study is continuing and the advantages of LWM are increasing with time. The present report is only concerned with recurrence after laparoscopic (TEP) repair.
Materials and methods
Totally extraperitoneal repair has been performed in Edinburgh since 1992, and our surgical technique has been described [13]. By using the prospective, computerised audit of the Lothian Surgical Audit (LSA), we have identified recurrence in our patients throughout this period and published data on our learning curves. Most consultant surgeons have completed their learning curve and reached a plateau in terms of recurrence. Our standard TEP technique has been described, and surgeons use a 15 × 10 cm polypropylene mesh (Prolene Ethicon) which is placed over the inguino/femoral region and employ no fixation. We have continued to use a mesh of this size after conversion to Ultrapro and do not routinely fix the mesh.
Using the LSA database, we identified all patients undergoing TEP surgery between January 2002 and June 2006. LWM was first used in April 2004. We have therefore divided the patients into three groups: group 1 being all patients operated between 2002 and March 2004, prior to the introduction of LMW and who received HWM; group 2 being operated between April 2004 and June 2006 using LWM; and group 3 being patients operated between April 2004 and June 2006 with HWM. In most cases, the mesh type was recorded prospectively by the surgeon but in others we could identify the mesh type from nursing operating theatre records where all implants are identified in the theatre manuals. We also used the prospective operation record and clinic letters to identify the consultant team, the surgeon and the type, unilateral vs bilateral, size of hernia and technical difficulties. During this study the surgeons did not record size of the hernia according to any standard classification. However, they recorded the presence of a large defect based on their experience, which from our experience suggests a defect of 3 cm or more.
Using LSA we identified all patients referred back for surgical review with a recurrent hernia. Previous studies using telephone contact have shown that most recurrent hernias are quickly re-referred by general practitioners and are therefore identified by LSA.
Statistical analysis was performed using SPSS version 12.0. Kaplan–Meier analysis was used to assess differences in time to recurrence between the three groups of meshes.
P-value of <0.05 was considered as statistically significant.
Patients were operated either at the Royal Infirmary within the NHS or at BUPA Murrayfield Hospital in the private sector.
Results
Group 1 (all HWM: pre LWM) consisted of 328 patients with 436 repaired herniae of whom 13 (2.98%) are known to have recurred with a median follow-up of 43 months (32–60 months). Group 2 (LWM) consisted of 251 patients with 371 repairs of whom 16 (4.3%) have recurred with a median follow-up of 14.5 months (6–32 months). Group 3 (HWM concurrent with LWM) consisted of 326 patients with 425 hernia of whom 12 (2.82%) have recurred with a median follow-up of 22.4 months (6–32 months) (Table 1).
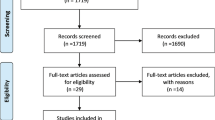
As shown in Fig. 1, no statistical difference was noted in time to recurrence in the three groups of meshes (log-rank test, P = 0.2).
Twelve consultant teams contributed to the data set overall, 11 to group 1, 11 to group 2 and 11 to group 3. Ten consultants teams contributed to all three groups and there is no reason to believe that any differences found may be due to individual consultant contributions.
Of the 11 consultants that used LWM, 5 performed only nine repairs in total with one recurrence. The remaining six surgeons performed between 30 and 97 repairs with recurrence rates between 1.5 and 6.5% (median 4%). There was no statistically significant difference in recurrence rates among any of these individual surgeons.
Consultants either performed or were present at most operations. In group 2 (LWM), trainees performed 76 operations (30%) with consultant supervision, whilst in group 3 (HWM), 48 (14%) were performed by trainees. This difference is due to one high-activity surgeon who continued to use HWM and has no teaching responsibility. In the LWM group, 6 of the 17 recurrences were operated by a trainee (35%), indicating no significant tendency for trainee operations to be associated with recurrence.
In group 2 (LWM), the operation recorded that the surgeon used a tacker in 10 (4%) of the 251 patients, usually following an expressed concern that the hernial defect was large. None of these patients recurred. Similarly, in group 3 (HWM), tackers were used in 4 (1.2%) of the 326 patients. The difference in the use of a tacker just fails to reach statistical significance (P = 0.052) but suggests a tendency for surgeons to be less prepared to rely on adherence alone with LWM and thus resort to tacking more often.
In group 2 (LWM), recurrence occurred in 15 patients, including one bilateral repair recurring on both sides. Overall of the 15 patients who developed recurrence, 11 had undergone a bilateral operation and 4 unilateral. Overall in this group, 120 patients had bilateral repair and 131 unilateral. The high incidence of bilateral repair in the recurring patients was not significantly different from the whole group (P = 0.065). A bilateral repair has double the chance of recurring and when analysed by hernia, the recurrence rate in bilateral repairs was 5% compared with 3% after unilateral repair. This difference is not statistically significant. In group 3 (HWM), of the 12 patients who recurred, 7 had undergone bilateral repair and 5 unilateral. Overall, there were 99 bilateral repairs and 227 unilateral repairs in this group. Although again there was a tendency for bilateral repairs to recur more frequently, this was not statistically significant, and when analysed by hernia, the recurrence rates were very similar at 3.5 and 2.2%.
In the 16 recurrences after LWM repair, the initial repair was for an indirect hernia in 11 and direct hernia in 5. In eight cases the surgeon commented on the large size of the hernia and had some technical problems in four. In the 11 HWM recurrences, the initial hernia was direct in 6 and indirect in 5. Ten of the 11 operations described a large hernia, and in 2 there were technical difficulties described. These distributions were not significantly different but do support the expected view that larger hernias are more likely to recur.
Additional historic data were not available for most consultants but one consultant had performed over 500 HWM repairs during the previous 7 years with only 4 identified recurrences to date. This consultant had 4 recurrences after 65 repairs with LWM, statistically significantly worse than the previous 7 years experience (P < 0.05) despite the less than 2-year follow-up in the LWM group.
Discussion
In its detailed meta-analysis, NICE [14] reports a typical recurrence rate after TEP of 2.3% within 2 years. This is abstracted from published randomised trials where it might be expected that results are better than in routine clinical practice. A large American randomised trial [15] reported a 10% recurrence rate within 2 years after TEP. By contrast, individual centres of excellence have reported recurrence rates well below 1% [16, 17], but these are almost certainly not representative of normal practice. Many regional and national audits together with large trials report that about 10% of all inguinal hernia repairs are undertaken for recurrence and, perhaps surprisingly, there is little if any evidence of improvement over the recent past despite the widespread introduction of prosthetic mesh [18]. Based on these data, we have to conclude that at least 10% of present day inguinal hernia repairs will ultimately fail. It might be reasonable therefore to conclude that a recurrence rate of 1% per year during the initial post-operative years indicates an acceptable, if not state of the art, level of performance in inguinal hernia repair. Against this background, our 2002–2004 recurrence rate of 2.98% with a median follow-up of 43 months would suggest that our surgeons are performing to an acceptable standard, at least equivalent to those RCTs included by NICE and well above that reported from the USA Veterans trial [15]. Our recurrence rate of 2.8% using HWM meshes with a median follow-up of 22 months is also similar to that reported by NICE.
By contrast a recurrence rate of 4.3% with a median follow-up of 14 months in the LWM group is suggestive of poorer practice than might be expected from a reasonable centre. We have also suggested in a previous detailed analysis of our own recurrence that early failure after TEP is due to technical operative issues [19]. In an attempt to extrapolate what the recurrence rate might rise to in group 2 (LWM), we find that the recurrence rate is presently 6.6% in the first 30 hernia operations with a minimum 2-year follow-up and 5.5% recurrence in the first 126 hernia operations with a minimum follow-up of 18 months. It therefore seems likely that recurrence with a minimum follow-up of 2 years will be in the region of 5% or even greater. Based on the estimate that 2-year recurrence rates may rise to this level, it can be extrapolated that for every 100 hernia repairs performed, three to four additional patients will recur using 15 × 10 cm LWM compared to standard mesh.
Lightweight mesh is exceptionally strong, and any increase in recurrence is not likely to be due to an intrinsic lack of strength. When staples are not used, the surgeon depends on the adhesion between the mesh and abdominal wall to prevent retraction of the mesh into the abdominal wall defect. Also the intrinsic mesh stiffness plays a part in holding the mesh in place. The adhesion strength must relate to the relative area of adhesion in comparison to the area of the defect. Theoretically, using a mesh of 15 × 10 cm with an area of 150 cm2, the ratio of adhesion to defect will be 191:1 for a defect with a diameter of 1 cm. This ratio falls to 48:1 as the hernial defect increases to 2 cm, 21:1 for 3 cm, 12:1 for 4 cm and 8:1 for 5 cm. As a result, a hernia with a 5-cm diameter will have less than one-twentieth of the mesh adhesion strength of a 1-cm defect.
From our work it seems likely that a critical point may be reached where, as the hernia defect increases in diameter, the adhesion strength between mesh and abdominal wall is insufficient to prevent the displacement of the mesh into the defect. This effect could be counteracted by using a larger LWM, thus increasing the adhesion area relative to the defect area. Alternatively, the surgeon could use glue to increase the adhesive bond between mesh and muscle. Use of a heavier and stiffer mesh would have the same beneficial effect. Finally, the use of staple fixation may help, but it is not possible to staple all around an inguinal hernia defect without risk to major vessels and nerves.
At the present time, our own research and that of others has demonstrated that LWM significantly increases patient comfort and reduces long-term chronic pain. However, in patients with larger hernial defects, simple placement of 15 × 10 cm LWM without additional measures to prevent early mesh displacement has resulted in an increased risk of recurrence in keeping with earlier reports [6, 11]. Whilst a randomised trial would be ideal, based on our work and that of others, it seems logical that surgeons wishing to derive the benefits of LWM for their patients may have to modify their technique in order to reduce the risk of recurrence. Of the present available methods to achieve increased adhesion between mesh and abdominal wall, we currently prefer to use LWM, increasing its size for larger hernias as is standard practice for ventral hernia repair. We will continue to audit our results.
Our experience suggests that ultra-lightweight meshes may have even greater problems of adhesion and fixation and should be introduced with some caution.
References
Khan LR, Kumar S, Nixon SJ (2006) Early results for new lightweight mesh in laparoscopic totally extra-peritoneal inguinal hernia repair. Hernia 10:303–308
Bringman S, Wollert S, Ostgerberg J, Heikkinen T (2005) Early results of a randomized multicenter trial comparing Prolene and VyproII mesh in bilateral endoscopic extraperitoneal hernioplasty (TEP). Surg Endosc 19:536–540
Post S, Weiss B, Willer M, Neufang T, Lorenz D (2004) Randomized clinical trial of lightweight composite mesh for Lichtenstein inguinal hernia repair. Br J Surg 91:44–48
Bringman S, Wollert S, Osterberg J, Smedberg S, Granlund H, Heikkinen TJ (2006) Three-year results of a randomized clinical trial of lightweight or standard polypropylene mesh in Lichtenstein repair of primary inguinal hernia. Br J Surg 93:1056–1059
Puccio F, Solazzo M, Marciano P (2005) Comparison of three different mesh materials in tension-free inguinal hernia repair: prolene versus Vypro versus surgisis. Int Surg 90(3 Suppl):S21–S23
O’Dwyer PJ, Kingsnorth AN, Molloy RG, Small PK (2005) Randomized clinical trial assessing impact of a lightweight or heavyweight mesh on chronic pain after inguinal hernia repair. Br J Surg 92:166–170
Horstmann R, Hellwig M, Classen C, Rottgermann S, Palmes D (2006) Impact of polypropylene amount on functional outcome and quality of life after inguinal hernia repair by the TAPP procedure using pure, mixed, and titanium-coated meshes. World J Surg 30:1742–1749
Heikkinen T, Wollert S, Osterberg J, Smedberg S, Bringman S (2006) Early results of a randomised trial comparing Prolene and VyproII-mesh in endoscopic extraperitoneal inguinal hernia repair (TEP) of recurrent unilateral hernias. Hernia 10:34–40
Cobb WS, Kercher KW, Heniford BT (2005) The argument for lightweight polypropylene mesh in hernia repair. Surg Innov 12:63–69
Israelsson LA (2005) Preventing and treating parastomal hernia. World J Surg 29:1086–1089
Conze J, Kingsnorth AN, Flament JB, Simmermacher R, Arlt G, Langer C, Schippers E, Hartley M, Schumpelick V (2005) Randomized clinical trial comparing lightweight composite mesh with polyester or polypropylene mesh for incisional hernia repair. Br J Surg 92:1488–1493
Kumar S, Wilson RG, Nixon SJ, Macintyre IM (2002) Chronic pain after laparoscopic and open mesh repair of groin hernia. Br J Surg 89:1476–1479
Nixon SJ, Kumar S (2005) The totally extraperitoneal approach (TEP) to inguinal hernia repair. Surgeon 3:281–287, 305
National Institute for Clinical Excellence (NICE) (2004) Laparoscopic surgery for inguinal hernia repair. Technology appraisal no. 83. http://www.nice.org.uk/pdf/TA083guidance.pdf
Neumayer L, Giobbie-Hurder A, Jonasson O, Fitzgibbons R, Dunlop D, Gibbs J, Reda D, Henderson W (2004) Open mesh versus laparoscopic mesh repair of inguinal hernia. N Engl J Med 350:1819–1827
Tamme C, Scheidbach H, Hampe C, Schneider C, Kockerling F (2003) Totally extraperitoneal endoscopic inguinal hernia repair (TEP). Surg Endosc 17:190–195
Kapiris SA, Brough WA, Royston CM, O’Boyle C, Sedman PC (2001) Laparoscopic transabdominal preperitoneal (TAPP) hernia repair. A 7-year two-center experience in 3017 patients. Surg Endosc 15:972–975
Schumplick V, Klinge U (2003) Prosthetic implants for hernia repair. Br J Surg 90:1457–1458
Lamb AD, Robson AJ, Nixon SJ (2006) Recurrence after totally extraperitoneal laparoscopic repair: implications for operative technique and surgical training. Surgeon 4:299–307
Acknowledgements
We wish to thank our surgical colleagues for allowing analysis and publication of their data.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Akolekar, D., Kumar, S., Khan, L.R. et al. Comparison of recurrence with lightweight composite polypropylene mesh and heavyweight mesh in laparoscopic totally extraperitoneal inguinal hernia repair: an audit of 1,232 repairs. Hernia 12, 39–43 (2008). https://doi.org/10.1007/s10029-007-0275-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-007-0275-7