Abstract
Background: The aim of this study was to investigate the outcome of preperitoneal repair using laparoscopic (TEP) and open (OPM) approach in recurrent inguinal hernia. Methods: We performed a prospective controlled nonrandomized clinical study in 188 patients with 207 recurrent inguinal hernias over a period of 5 years. TEP repair was employed for 86 repairs, and OPM was used in 121 procedures. The main outcome measurements were: recurrence rate, operating time, hospital stay, and postoperative complications. Results: There were three recurrences (1.7%). Two in the OPM group (1.8%) and one (1.3%) in the TEP group [P=NS (not significant)]. The TEP procedure was faster than OPM for unilateral repair (40.8 vs 46.3 min) (P<0.001). Postoperative complications were more frequent in the OPM group (23.9%) than the TEP group (13.9%) (P=NS). Hospital stay was significantly shorter in the TEP group (1.2 vs 3.9 days) (P<0.001). Conclusions: Preperitoneal approach (open or laparoscopic) seems to be a good option in recurrent inguinal hernia when these procedures are done by experienced surgeons.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The repair of recurrent inguinal hernia is usually a difficult operation, requiring surgical experience and an accurate knowledge of the inguinal anatomy. This type of repair does not always have successful results, and high recurrence and complications rates have been reported [1, 2, 3, 4, 5].
The anterior mesh approach is the most commonly performed technique, but it has the disadvantage of reoperating through scar tissue with the risk of testicular damage and a large number of local haematomas. However, a preperitoneal (posterior) approach, open or laparoscopic, reduces these problems [4].
The main advantages of the preperitoneal approach are mesh placement in the preperitoneal space where the hernia is produced and avoiding the disadvantage of reoperating through scar tissue.
Laparoscopic extraperitoneal repair (TEP) reproduces the same precepts of the open preperitoneal approach: extensive dissection and big mesh covering all the myopectineal area, avoiding the missed hernia syndrome, but with all the advantages of laparoscopic access, reducing their inconveniences with lower postoperative discomfort and faster return to normal activities [6, 7, 8, 9, 10, 11].
The aim of this prospective, controlled clinical study was to investigate the long-term outcomes of the laparoscopic TEP repair and the open preperitoneal mesh repair (OPM) for the recurrent inguinal hernia when both procedures are done by experienced groups.
Patients and methods
From January 1995–December 1999, 188 patients were operated on for recurrent inguinal hernia in two hospitals. To avoid bias from the learning curve, all the TEP repairs were performed in the center by surgeons with experience in laparoscopic extraperitoneal approach, while the open preperitoneal approach was done in the other center by surgeons experienced with this access.
All patients between 21 and 80 years of age with recurrent inguinal hernia were considered for this study. High-risk patients (American Society of Anesthesiologists (ASA) IV), with incarcerated or massive scrotal hernias and morbid obesity (Body Mass Index (BMI) >35 kg/m2) were excluded.
Detailed informed consent was obtained from all the patients.
General anaesthesia was indicated in ASA I-II patients in the laparoscopic group, while ASA III and ASA I-II patients who did not like this procedure underwent spinal anaesthesia. Open repair patients underwent spinal anaesthesia, except those who preferred general anaesthesia.
Surgical technique
Cefazolin (2 gr IV) was employed in antibiotic prophylaxis, replaced by Clindamicine (600 mg/IV) in case of allergy.
Open preperitoneal mesh repair (OPM)
Open preperitoneal mesh repair (OPM) was undertaken, as described by Nyhus. Through a lower abdominal transverse incision, the anterior rectus sheath was incised and the muscle reflected medially. The preperitoneal space was cleaved with blunt dissection, exposing the myopectineal orifice. The hernia was reduced and not repaired. A 15×15-cm polypropylene mesh, without slits, (Ethicon, USA) was inserted in the preperitoneal space, parietalizing the spermatic-cord elements, and fixed with nonabsorbable sutures [12].
Laparoscopic extraperitoneal repair (TEP)
A preperitoneal dissection was made with a balloon through a subumbilical incision. Two 5-mm trocars were inserted in the midline. Extensive lateral dissection, isolation of the cord structures, and hernia reduction were performed. A 13×15-cm anatomic polypropylene mesh (3DMAX, Bard, USA) was placed, covering all of the myopectineal orifice, and fixed [2].
Follow-up
All patients were visited and physically examined 7 days after the surgery and at 1, 3, and 12 months postoperatively and yearly thereafter.
Statistical analysis
Statistical analyses were performed with the SPSS 7.5-Windows program (SPSS, Chicago, Ill., USA). Percentages were compared by means of the chi-square test and continuous variables were compared with the Student’s t-test or variance analysis.
A P value of less than 0.05 indicated statistical difference.
Results
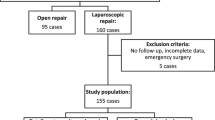
During this period, 188 patients with 207 recurrent inguinal hernias were repaired in both hospitals. One hundred and twenty-one repairs were performed using OPM and 86 using TEP. In 19 cases, the recurrence was bilateral.
There were 182 men and six women. The mean age of the patients was 57 years (range 21–80).
Patient characteristics and physical status are shown in Table 1. There were no statistical differences between the groups in terms of age, sex, ASA, previous repairs or follow-up.
Of the 207 inguinal repairs, 164 (79%) had been repaired once previously, 24 (12%) followed two previous repairs, 16 (8%) followed three, and three (1%) four previous repairs.
In 54 patients (28.7%), primary repair has been bilateral.
A contralateral primary hernia was also repaired in five patients in the laparoscopic group and two in the open group.
There were no major intraoperative complications.
There were 33 peritoneal tears (42.3%) in TEP repairs, but only four of these were extensive and needed conversion (5.1%), due to dissection difficulties or peritoneal tears. One case was converted to Lichtenstein repair, and the other three were switched to transabdominal laparoscopic repair (TAPP).
The TEP procedure was faster than OPM for unilateral repair (40.8±8.3 min vs 46.3±7.1 min) (P<0.001). Bilateral repair required 75.2±19.7 min for laparoscopic repair and 77.6±5.5 min for the open approach.
No statistically significant difference was observed in the incidence of postoperative complications, but they were more frequent in the open group than the laparoscopic group (Table 2). There were 29 (23.9%) postoperative complications in the OPM group and 12 (13.9%) in the TEP group (chi-square:4.16; P=NS). Most of them were minor (haematoma, seroma, or urinaries). Prolonged pain >1 month in the operative area was reported by five OPM patients and one TEP patient. There were no injuries to the bowel, large vessels, urinary bladder, or testicular atrophies. One TEP patient required reoperation for bleeding. There were no deaths.
Hospital stay was significantly shorter in the TEP group (1.2±1.2 days vs 3.9±1.3 days in the OPM group) (t=15.22; P<0.001). Only three TEP patients were treated as day cases.
One hundred seventy-six patients were examined between June 2002 and January 2003. All these patients completed a minimum of 3 years follow-up. Twelve could not attend for examination. The average follow-up period was 43.3 months in the TEP group and 48.7 months in the OPM group.
Three recurrent hernias were detected (1.7%). Two patients (1.8%) had a recurrence in the OPM group, and one patient (1.3%) had a recurrence in the TEP group. (P=NS)
All the recurrences occurred within 12 months of surgery.
Discussion
It is known that the preperitoneal approach is a good option for recurrent inguinal hernia. This access avoids reoperating through distorted anatomy and scar tissue, reducing the risk of testicular damage and permitting inspection of all potential groin hernia sites. An extensive dissection allows the use of a large mesh covering all the myopectineal area, avoiding the missed hernia syndrome [4, 10].
Despite the fact that open preperitoneal mesh repair offers clear benefits, this method has not been widely adopted, and the anterior tension-free repair (Lichtenstein) remains the most commonly performed technique in the treatment of recurrent inguinal hernia. Recently, Hair reports that only 15% of repairs for recurrent hernia were preperitoneal in Scotland (9% laparoscopic and 6% open preperitoneal) [13].
An unfamiliar anatomy, an uncomfortable approach with the use of large incisions, and difficult visualisation of the groin anatomy remain major reasons for this lack of surgeons’ interest.
TEP laparoscopic repair reproduces the precepts of the open preperitoneal approach, reducing their inconveniences, offering good vision of the preperitoneal space, and permitting an easier approach. This produces less postoperative discomfort and a faster return to normal activities [6, 7, 9, 14, 15, 16].
Only one trial has compared an open preperitoneal repair with a laparoscopic preperitoneal repair (TAPP) in recurrent inguinal hernia [17]. The results of this study reflect a recurrence rate of 1.9% for OPM and 12.5% for TAPP. This recurrence is more than expected, probably because of the surgeons’ inexperience, due to the fact that they hadn’t finalised their learning curve.
Excellent results have been reported with anterior mesh repair under local anaesthesia [18], laparoscopic techniques [2, 7, 9, 14, 19, 20], and the OPM approach [14, 21, 22] in recurrent hernia when these procedures are performed by experienced surgeons. Our prospective study is in accord with these studies and confirms the effectiveness of the preperitoneal approach for recurrent inguinal hernia with low recurrence and complication rates.
Postoperative complications, chronic neuralgia, and length of stay are less in the TEP group. In our opinion, this is because the laparoscopic approach makes it easier to avoid the large dissections of the open approach. Urinary complications in OPM are caused more by the spinal anaesthesia than the hernia repair.
Recurrences after preperitoneal repair are mainly due to technical errors and, therefore, occur early. The main causes are surgeon inexperience, incomplete dissection, missed hernia, insufficient mesh size, and inadequate position or migration when the mesh is not fixed [1, 2, 4, 10, 14, 23, 24, 25, 26]. All our recurrences occurred within 12 months of surgery.
This study confirms the previously reported favourable results of the preperitoneal approach (open or laparoscopic) in recurrent inguinal hernia when these procedures are done by experienced surgeons.
References
Bay-Nielsen M, Kehlet H, Strand L, Malmstrom J, Andersen FH, Wara P, Juul P, Callesen T (2001) Quality assessment of 26.304 herniorrhaphies in Denmark: a prospective nationwide study. Lancet 358:1124–1128
Feliu Palà X, Martín Gómez M, Morales Conde S, Fernández Sallent E (2001) The impact of the surgeon’s experience on the results of laparoscopic hernia repair. Surg Endosc 15:1467–1470
Haapaniemi S, Gunnarsson U, Nordin P, Nilsson E (2001) Reoperation after recurrent groin hernia repair. Ann Surg 234:122–126
Kurzer M, Belsham PA, Kark AE (2002) Prospective study of open preperitoneal mesh repair for recurrent inguinal hernia. Br J Surg 89:90–93
Nilsson E, Haapaniemi S, Gruber G, Sandblom G (1998) Methods of repair and risk for reoperation in Swedish hernia surgery from 1992 to 1996. Br J Surg 85:1686–1691
Feliu Palà X, Fernández Sallent E (1997) Tratamiento laparoscópico de la hernia inguinal recidivada (Laparoscopic repair of recurrent inguinal hernia). In: Porrero JL (ed) Cirugía de la pared abdominal (Abdominal wall surgery) Masson Ed. Barcelona. pp 180–187
Felix EL, Michas CA, McKnight RL (1995) Laparoscopic repair of recurrent hernias. Surg Endosc 9:135–138
Memon MA, Feliu X, Fernández Sallent E, Camps J, Fitzgibbons RJ (1999) Laparoscopic repair of recurrent hernias. Surg Endosc 13:807–810
Van Der Hem JA, Hamming JF, Meeuwis JD, Oostvogel HJ (2001) Totally extraperitoneal endoscopic repair of recurrent inguinal hernia. Br J Surg 88:884–886
Occelli G, Barrat C, Catheline JM, Voreux JP, Cueto-Rozon R, Champault G (2000) Laparoscopic treatment of inguinal hernias: prospective evaluation of 757 cases treated by a totally extraperitoneal route. Hernia 4:81–84
Sebbag H, Brunaud L, Collinet-Adler S, Ulmer M, Marchal F, Grosdidier G (2000) Long-term follow-up of totally extraperitoneal laparoscopic treatment of inguinal hernia at a single center. Hernia 4:292–295
Martínez-Ródenas F, Vila JM, Moreno J, Julián JF, Torres G, Badía JM, Pie J (1995) The preperitoneal approach in recurrent inguinal hernia. Posterior wall repair with a Marlex mesh. Video-review of Surgery 12:33–40
Hair A, Duffy K, McLean J, Taylor S, Smith H, Walker A, et al. (2000) Groin hernia repair in Scotland. Br J Surg 87:1722–1726
Keidar A, Kanitkar S, Szold A (2002) Laparoscopic repair of recurrent inguinal hernia. Surg Endosc 16:1708–1712
National Institute for Clinical Excellence (NICE) (2001) Guidance on the use of laparoscopic surgery for inguinal hernia. Technology Appraisal Guidance Nº 18. pp 1–103
Champault G, Rizk N, Catheline JM, Barrat C, Turner R, Boutelier P (1997) Inguinal hernia repair. Totally pre-peritoneal laparoscopic approach vs Stoppa operation. Randomized trial: 100 cases. Hernia 1:31–36
Beets GL, Dirksen CD, Go PMNYH, Geisler FEA, Baeten CGMI, Kootstra G (1999) Open or laparoscopic preperitoneal mesh repair for recurrent inguinal hernia? Surg Endosc 13:323–327
Gianetta E, Cuneo S, Vitale B, Camerini G, Marini P, Stella M (2000) Anterior tension-free repair of recurrent inguinal hernia under local anaesthesia: a 7-year experience in a teaching hospital. Ann Surg 231:132–6
Frankum CE, Ramshaw BJ, White J, Duncan TD, Wilson RA, Mason EM, Lucas G, Promes J (1999) Laparoscopic repair of bilateral and recurrent hernias. Am Surg 65:839–842
Sandbichler P, Draxl H, Gstir H, Fuchs H, Furtschegger A, Egender G, Steiner E (1996) Laparoscopic repair of recurrent inguinal hernias. Am J Surg 171:366–368
Janu PG, Sellers KD, Mangiante EC (1998) Recurrent inguinal hernia: preferred operative approach. Am Surg 64:569–574
Lobo E, Sanjuanbenito A, Fernandez-Merino J, Martínez-Molina E (1999) The preperitoneal (posterior) approach to the repair of recurrent inguinal hernia. Hernia 3:65–67
Crawford DL, Phillips EH (1998) Laparoscopic repair and groin hernia surgery. Surg Clin North Am 78:1047–1062
Felix E, Scott S, Crafton B, Geis P, Duncan T, Sewell R, McKernan B (1998) Causes of recurrence after laparoscopic hernioplasty. Surg Endosc 12:226–231
Knook MTT, Weidema WF, Stassen LPS, van Steensel CJ (1999) Endoscopic total extraperitoneal repair of primary and recurrent inguinal hernias. Surg Endosc 13:507–511
Lowham AS, Filipi CJ, Fitzgibbons RJ, Stoppa R, Wantz GE, Felix EL, Crafton WB (1997) Mechanisms of hernia recurrence after preperitoneal mesh repair: Traditional and laparoscopic. Ann Surg 225:422–431
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Feliu, X., Torres, G., Viñas, X. et al. Preperitoneal repair for recurrent inguinal hernia: Laparoscopic and open approach. Hernia 8, 113–116 (2004). https://doi.org/10.1007/s10029-003-0179-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-003-0179-0