Abstract
Purpose
This retrospective study was conducted to compare the long-term outcomes of single-incision totally extraperitoneal (S-TEP) inguinal hernia repair and conventional multiport totally extraperitoneal (M-TEP) inguinal hernia repair.
Methods
The study population included 186 consecutive patients (S-TEP, n = 149; M-TEP, n = 37) who underwent elective surgery for inguinal hernia at Osaka Police Hospital between 2011 and 2013.
Results
No significant between-group difference was found in patient or hernia characteristics or in perioperative outcomes, with the exception of age (S-TEP group vs. M-TEP group: median 69 [IQR 60–75] years vs. 64 [55–69] years, respectively; P = 0.019). Furthermore, no significant between-group difference was found in follow-up time (5.5 [3.0–5.8] vs. 5.4 [3.1–5.7] years, P = 0.839), recurrence rate (0.6 vs. 2.4%, P = 0.358), chronic pain (1.2 vs. 0%, P = 1.000), feeling the mesh (2.3 vs. 7.1%, P = 0.142), or movement limitation (0.6 vs. 0%, P = 1.000). All chronic symptoms were “mild but not bothersome.” A metachronous contralateral inguinal hernia developed in 8.1% of patients.
Conclusion
The long-term outcomes of S-TEP repair were comparable to those of M-TEP, with rates of recurrence, chronic pain, feeling the mesh, and movement limitation falling within acceptable limits.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Totally extra-peritoneal (TEP) inguinal hernia repair is considered a standard inguinal hernia repair procedure, alongside trans-peritoneal hernioplasty (TAPP) and the Lichtenstein procedure [1]. Single-incision laparoscopic surgery (SILS) is a minimally invasive procedure that is performed through a single, small incision, and is considered a feasible alternative to conventional multiport laparoscopic surgery (MPS). At Osaka Police Hospital, we now perform TEP inguinal hernia repair by means of SILS in patients who qualify for such surgery [2,3,4]. Osaka Police Hospital is a high-volume multidisciplinary acute care hospital in Japan with a long tradition in SILS as well as MPS. At this hospital cholecystectomy, colectomy, gastrectomy, and adhesiolysis for small bowel obstruction are performed mainly by means of SILS.
Five randomized controlled trials comparing the perioperative and short- and/or mid-term outcomes of single-incision laparoscopic TEP (S-TEP) inguinal hernia repair and conventional multiport TEP (M-TEP) inguinal hernia repair have been reported [5,6,7,8,9,10], and the outcomes among large groups of patients who have undergone S-TEP hernia have also been reported [11,12,13,14]; however, data on the long-term outcomes (5 years or longer) are limited. Thus, we conducted a retrospective study in which we compared the long-term outcomes of S-TEP inguinal hernia repair to those of M-TEP inguinal hernia repair, particularly in terms of recurrence, chronic pain, feeling the mesh, and movement limitation. In addition, we investigated the occurrence of contralateral inguinal hernia for future reference.
Methods
Study patients
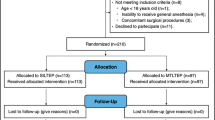
To identify patients to be included in the study, we reviewed the records of patients who underwent S-TEP or M-TEP inguinal hernia repair at Osaka Police Hospital between January 2011 and December 2013. Patients who had undergone emergency TEP repair (n = 2), those who had undergone TEP repair along with another surgery (n = 4; 3 along with incisional hernia repair and 1 along with cholecystectomy), and those who required conversion to open anterior-approach surgery (n = 4) were excluded, leaving 186 patients (S-TEP: n = 149 [170 hernias]; M-TEP: n = 37 [42 hernias]) who met the inclusion criteria (Fig. 1).
The study was conducted under approval by the institutional review board of Osaka Police Hospital (approval number: 741).
Treatment strategy
In treating inguinal hernia surgically, we generally perform TEP repair. Exceptions are made when general anesthesia is contraindicated or the patient has undergone radical prostatectomy, lateral lymph node dissection for low rectal cancer [15], or preperitoneal hernia repair, such as Prolene Hernia System repair [16,17,18] or Kugel repair [19, 20]. We performed M-TEP repair routinely until September 2011, when we began performing S-TEP repair for any patient deemed to be a suitable candidate.
Surgical technique
S-TEP repair and M-TEP repair were performed according to standard protocols, as previously described [14]. A single 25-mm subumbilical incision was made, and a vertical incision was made in the anterior rectus fascia on the affected side(s) to enter and develop the preperitoneal space. Pneumopreperitoneum was then established by insufflation of 8 mmHg CO2. For M-TEP repair, one 10-mm port was placed in the subumbilical incision, and two 5-mm ports were placed in the midline (one 5-cm from the pubic tubercle and the other between the subumbilical and suprapubic ports), and a 10-mm flexible-tip Olympus EndoEye videoscope (Olympus Medical Systems, Tokyo, Japan) was used. For S-TEP repair, single port access devices (Lap Protector mini and EZ Access; Hakko Co., Ltd. Nagano, Japan) were placed in the subumbilical incision. A 10-mm flexible-tip Olympus EndoEye videoscope was used for patients treated before April 2013. Thereafter, a 5-mm flexible-tip Olympus EndoEye videoscope was used. A polypropylene mesh (3D Max Light®; CR BARD Inc., Murray Hill, NJ, USA) was placed in the dissected preperitoneal space, covering the inguinal floor, and then fixed to the pubic bone, Cooper’s ligament, and above the iliopubic tract with AbsorbaTack™ (Covidien, Mansfield, MA, USA). After deflation of the preperitoneal space, the rectus sheath was closed with 2-0 Vicryl (Ethicon, Somerville, NJ, USA), and the skin was closed with 3-0 PDS (Ethicon). The repair procedure did not include intraoperative exploration for a contralateral hernia. Both types of repair (S-TEP or M-TEP) were usually performed by an experienced staff surgeon (i.e., a surgeon with experience in 20 or more TEP cases) and a resident. In some cases, the operation was performed by a less experienced staff surgeon and a resident, with an experienced staff surgeon supervising the procedure. During the 3-year period noted above, a total of 5 staff surgeons performed such repairs.
Data collection and follow-up
For the purpose of the study, the following data were obtained from patients’ clinical records: clinical characteristics, including age, sex, body mass index, and American Society of Anesthesiologists (ASA) physical status at the time of presentation; operative and postoperative variables, including operation time, estimated blood loss volume, and postoperative length of stay; and postoperative complications. Further, we assessed whether patients experienced recurrence or the development of a metachronous contralateral inguinal hernia, which was defined as an inguinal hernia occurring at a hernia-naïve site on the side opposite the S-TEP or M-TEP repair; this did not include any contralateral hernia that developed at a site of previous hernia repair. Patients were seen in the outpatient setting 1 to 2 weeks after the surgery, 1 month later, and then 3 months later. For the purpose of the study, patients were contacted by telephone approximately 5 years after the operation and asked questions according to the Japanese version of the Carolinas Comfort Scale™ (CCS) [21, 22], a quality-of-life survey pertaining specifically to hernia patients undergoing hernia repair with mesh, with 0 being the best possible score and 115 being the worst possible score. For patients who were not available by telephone, the latest outpatient follow-up information was used for the analysis. All interviews were conducted by a single nurse who was trained in using the Japanese version of the CCS. Patients who reported any symptoms at the time of the interview were scheduled for a clinic visit. Axial computed tomography (CT) images acquired for any reason within 3 months after the latest contact were referred to for evaluation of recurrence.
Study endpoints
The primary study endpoint was the rate of hernia recurrence within 5 years after the operation. The secondary endpoints were chronic pain, feeling the mesh, movement limitation, and the development of a contralateral hernia within 5 years after surgery.
Statistical analyses
Variables are shown as the number (and percentage) of patients or of hernias or as the median (and interquartile range) value. Between-group differences in continuous variables categorical variables were analyzed by the Wilcoxon rank-sum test and Fisher’s exact test, respectively. All statistical analyses were performed with JMP 15.1.0 (SAS Institute Inc., Cary, NC, USA). P values of < 0.05 were considered to indicate statistical significance.
Results
The clinical characteristics of the patients in each group are shown in Table 1. There was a significant difference in the age of the two groups, with patients in the S-TEP group being significantly older than those in the M-TEP group (P = 0.019). Ten (5.9%) hernias in the S-TEP group were recurrent hernias, five had previously been repaired without surgical mesh, four had previously been repaired using a mesh-plug, and one had previously been repaired using a PROLENE® hernia system. The operative variables and perioperative complications of the two groups are shown in Table 2 and did not differ to a statistically significant extent between the two groups.
The long-term outcomes of TEP repair in the two groups are shown in Table 3. The follow-up time was 5.5 (3.0–5.8) years for patients in the S-TEP group and 5.4 (3.1–5.7) years for patients in the M-TEP group, and did not differ to a statistically significant extent (P = 0.839). All 149 patients (170 hernias) in the S-TEP group underwent follow-up at 2 weeks, 146 (166 hernias) underwent follow-up at 1 month, 145 (165 hernias) underwent follow-up at 3 months, and 99 (116 hernias) were contacted at 5 years. Thirty-six (41 hernias) of the 37 patients in the M-TEP group underwent follow-up at 2 weeks, 36 (41 hernias) underwent follow-up at 1 month, and 36 (41 hernias) underwent follow-up at 3 months; 29 patients (31 hernias) were contacted at 5 years. CT images were available for 28 hernias (16.4%) in the S-TEP group and 10 hernias (23.8%) in the M-TEP group, without a significant difference (P = 0.268). One hernia recurred at 4 years after repair in the S-TEP group (0.6% recurrence rate), and 1 hernia recurred at 2 years after repair in the M-TEP group (2.4% recurrence rate). A metachronous contralateral inguinal hernia developed in a total of 15 patients (8.1%), 12 in the S-TEP group and three in the M-TEP group. The sites at which the 12 metachronous contralateral hernias developed in the S-TEP group patients accounted for 10.5% of the 114 (total) contralateral hernia-naïve sites in this group, and the sites at which the three metachronous contralateral hernias developed in the M-TEP group patients accounted for 10.3% of the 29 (total) contralateral hernia-naïve sites in this group, without a significant between-group difference (P = 1.000). Chronic pain was noted in two patients (1.2%) in the S-TEP group. Both of these patients had a total CCS pain score of 4. No patients in the M-TEP group experienced chronic pain (P = 1.000). Feeling the mesh was noted by four patients (2.3%) in the S-TEP group, with the total CCS score for feeling the mesh being 8 in one patient, 6 in two patients, and 4 in one patient, whereas feeling the mesh was noted by three patients (7.1%) in the M-TEP group, with the total CCS score for feeling the mesh being 8 in one patient, 6 in one. and 2 in one (P = 0.142). Movement limitation was noted in one patient (0.6%) in the S-TEP group, with the total CCS score for movement limitation being 6, whereas no movement limitation was noted in the M-TEP group (P = 1.000). All reported symptoms were “mild but not bothersome,” according to the CCS.
Discussion
Although S-TEP inguinal hernia repair and conventional M-TEP inguinal hernia repair are reported to be comparable in terms of safety, feasibility, and at least the short- and mid-term outcomes [5,6,7,8,9,10, 14], most of the data analyzed were obtained within 2 years after surgery [5,6,7,8,9], and some only represent the results of male patients with a primary inguinal hernia [7, 10]; thus, much remains to be clarified regarding the role of S-TEP in real-world practice. In the present study, we minimized the patient exclusion criteria so that we could evaluate the outcomes of M-TEP and S-TEP inguinal hernia repair in patients who are typically encountered in clinical practice. We found that the rate at which hernia recurred within 5 years after S-TEP repair and M-TEP repair did not differ to a statistically significant extent. We also found that the recurrence rate of 0.6% among patients who underwent S-TEP repair and 2.4% among those who underwent M-TEP repair was comparable to previously reported recurrence rates (1.1–4.0%) [23, 24]. In addition, in the present study, the rate of overall metachronous contralateral occurrence was 8.1%, and did not differ to a statistically significant extent between the S-TEP and M-TEP groups, which was consistent with previously reported contralateral occurrence rates of 6.7–10.5% (with some of the contralateral hernias having been detected during intraoperative exploration) [25, 26]. We also found that the prevalence of chronic pain (1.2% in the S-TEP group and 0% in the M-TEP group), prevalence of feeling the mesh (2.3% in the S-TEP group and 7.1% in the M-TEP group), and prevalence of movement limitation (0.6% in the S-TEP group and 0% in the M-TEP group) were comparable to the previously reported prevalence of 1–6% [27,28,29,30], 2–18% [29,30,31], and 3% [29, 30], respectively.
Although patients in our S-TEP group were significantly older than those in our M-TEP group, age has not been associated with a difference in the perioperative outcomes of TEP [3, 32], and this may mean that age has little or no effect on long-term outcomes.
The present study was associated with some limitations, including its retrospective observational study design, which means that it was susceptible to selection bias. In addition, because some patients were lost to follow-up and thus recurrence could not be evaluated either by physical examination or on CT images, the possibility of a type II error cannot be ruled out. Further, patient satisfaction, in terms of body image [33], for example, was not evaluated. Furthermore, variables such as perioperative care were not factored into the analysis in detail. Nonetheless, because reports comparing the long-term outcomes, including recurrence, chronic pain, and feeling the mesh, between M-TEP repair and S-TEP repair performed for patients with inguinal hernia are limited, we believe our data will help surgeons and other specialists in considering whether to perform S-TEP repair for patients with inguinal hernia.
On the basis of our study data, which reflect our clinical experience thus far, we conclude that the S-TEP approach is a feasible option for inguinal hernia repair. We caution that the procedure should be performed by surgeons with expertise in SILS.
References
HerniaSurge Group. International guidelines for groin hernia management. Hernia. 2018;22:1–165.
Wakasugi M, Akamatsu H, Tori M, Ueshima S, Omori T, Tei M, et al. Short-term outcome of single-incision laparoscopic totally extra-peritoneal inguinal hernia repair. Asian J Endosc Surg. 2013;6:143–6.
Wakasugi M, Tei M, Anno K, Mikami T, Tsukada R, Koh M, et al. Single-incision totally extraperitoneal inguinal hernia repair is safe and feasible in elderly patients: a single-center experience of 365 procedures. Asian J Endosc Surg. 2016;9:281–4.
Wakasugi M, Suzuki Y, Tei M, Anno K, Mikami T, Tsukada R, et al. The feasibility and safety of single-incision totally extraperitoneal inguinal hernia repair after previous lower abdominal surgery: 350 procedures at a single center. Surg Today. 2017;47:307–12.
Cardinali L, Mazzetti CH, Cadenas Febres A, Repullo D, Bruyns J, Dapri G. Prospective randomized study comparing single-incision laparoscopic versus multi-trocar laparoscopic totally extraperitoneal (TEP) inguinal hernia repair at 2 years. Surg Endosc. 2018;32:3262–72.
Tsai YC, Ho CH, Tai HC, Chung SD, Chueh SC. Laparoendoscopic single-site versus conventional laparoscopic total extraperitoneal hernia repair: a prospective randomized clinical trial. Surg Endosc. 2013;27:4684–92.
Wijerathne S, Agarwal N, Ramzi A, Liem DH, Tan WB, Lomanto D. Single-port versus conventional laparoscopic total extra-peritoneal inguinal hernia repair: a prospective, randomized, controlled clinical trial. Surg Endosc. 2016;30:1356–63.
Choi BJ, Jeong WJ, Lee IK, Lee SC. Single-port versus conventional three-port laparoscopic totally extraperitoneal inguinal hernia repair: a randomized controlled trial. Hernia. 2016;20:789–95.
Tran H, Turingan I, Tran K, Zajkowska M, Lam V, Hawthorne W. Potential benefits of single-port compared to multiport laparoscopic inguinal herniorraphy: a prospective randomized controlled study. Hernia. 2014;18:731–44.
Chia DKA, Lomanto D, Wijerathne S. Patient-reported outcomes and long-term results of a randomized controlled trial comparing single-port versus conventional laparoscopic inguinal hernia repair. World J Surg. 2020;44:2191–8.
Kim JH, An CH, Lee YS, Kim HY, Lee JI. Single incision laparoscopic totally extraperitoneal hernioplasty (SIL-TEP): experience of 512 procedures. Hernia. 2015;19:417–22.
Dapri G, Gerard L, Paesmans M, Cadière GB, Saussez S. First 200 consecutive transumbilical single-incision laparoscopic TEPs. Hernia. 2017;21:29–35.
Wakasugi M, Hasegawa J, Ikeda Y. Single-incision laparoscopic totally extraperitoneal inguinal hernia repair with tumescent local anesthesia: report of more than 2000 procedures at a day-surgery clinic. Surg Today. 2020. https://doi.org/10.1007/s00595-020-02141-0.
Wakasugi M, Masuzawa T, Tei M, Omori T, Ueshima S, Tori M, et al. Single-incision totally extraperitoneal inguinal hernia repair: our initial 100 cases and comparison with conventional three-port laparoscopic totally extraperitoneal inguinal hernia repair. Surg Today. 2015;45:606–10.
Fujita S, Mizusawa J, Kanemitsu Y, Ito M, Kinugasa Y, Komori K, et al. Mesorectal excision with or without lateral lymph node dissection for clinical stage II/III lower rectal cancer (JCOG0212): a multicenter, randomized controlled, noninferiority trial. Ann Surg. 2017;266:201–7.
Nakagawa M, Nagase T, Akatsu T, Imai S, Fujimura N, Asagoe T, et al. Randomized prospective trial comparing clinical outcomes 3 years after surgery by Marcy repair and Prolene Hernia System repair for adult indirect inguinal hernia. Surg Today. 2013;43:1109–15.
Hayashi Y, Miyata K, Yuasa N, Takeuchi E, Goto Y, Miyake H, et al. Short- and long-term outcomes of open inguinal hernia repair: comparison of the Prolene Hernia System and the Mesh Plug method. Surg Today. 2014;44:2255–62.
Magnusson J, Nygren J, Gustafsson UO, Thorell A. UltraPro Hernia System, Prolene Hernia System and Lichtenstein for primary inguinal hernia repair: 3-year outcomes of a prospective randomized controlled trial. Hernia. 2016;20:641–8.
Okinaga K, Hori T, Inaba T, Yamaoka K. A randomized clinical study on postoperative pain comparing the Polysoft patch to the modified Kugel patch for transinguinal preperitoneal inguinal hernia repair. Surg Today. 2016;46:691–8.
Nienhuijs S, Staal E, Keemers-Gels M, Rosman C, Strobbe L. Pain after open preperitoneal repair versus Lichtenstein repair: a randomized trial. World J Surg. 2007;31:1751–7 (discussion 8–9).
Heniford BT, Lincourt AE, Walters AL, Colavita PD, Belyansky I, Kercher KW, et al. Carolinas Comfort Scale as a measure of hernia repair quality of life: a reappraisal utilizing 3788 international patients. Ann Surg. 2018;267:171–6.
Heniford BT, Walters AL, Lincourt AE, Novitsky YW, Hope WW, Kercher KW. Comparison of generic versus specific quality-of-life scales for mesh hernia repairs. J Am Coll Surg. 2008;206:638–44.
Roos MM, Bakker WJ, Schouten N, Voorbrood CEH, Clevers GJ, Verleisdonk EJ, et al. Higher recurrence rate after endoscopic totally extraperitoneal (TEP) inguinal hernia repair with ultrapro lightweight mesh: 5-year results of a randomized controlled trial (TULP-trial). Ann Surg. 2018;268:241–6.
Melkemichel M, Bringman S, Widhe B. Lower recurrence rate with heavyweight mesh compared to lightweight mesh in laparoscopic totally extra-peritoneal (TEP) repair of groin hernia: a nationwide population-based register study. Hernia. 2018;22:989–97.
Zheng R, Altieri MS, Yang J, Chen H, Pryor AD, Bates A, et al. Long-term incidence of contralateral primary hernia repair following unilateral inguinal hernia repair in a cohort of 32,834 patients. Surg Endosc. 2017;31:817–22.
Lee CH, Chiu YT, Cheng CF, Wu JC, Yin WY, Chen JH. Risk factors for contralateral inguinal hernia repair after unilateral inguinal hernia repair in male adult patients: analysis from a nationwide population based cohort study. BMC Surg. 2017;21(17):106.
van der Pool AE, Harlaar JJ, den Hoed PT, Weidema WF, van Veen RN. Long-term follow-up evaluation of chronic pain after endoscopic total extraperitoneal repair of primary and recurrent inguinal hernia. Surg Endosc. 2010;24:1707–11.
Golani S, Middleton P. Long-term follow-up of laparoscopic total extraperitoneal (TEP) repair in inguinal hernia without mesh fixation. Hernia. 2017;21:37–43.
Gitelis ME, Patel L, Deasis F, Joehl R, Lapin B, Linn J, et al. Laparoscopic totally extraperitoneal groin hernia repair and quality of life at 2-year follow-up. J Am Coll Surg. 2016;223:153–61.
Ali SM, Zendejas B, Yadav S, Hernandez-Irizarry RC, Lohse CM, Farley DR. Predictors of chronic groin discomfort after laparoscopic totally extraperitoneal inguinal hernia repair. J Am Coll Surg. 2013;217:72–8 (discussion 8–80).
Matikainen M, Vironen J, Kössi J, Hulmi T, Hertsi M, Rantanen T, et al. Impact of mesh and fixation on chronic inguinal pain in Lichtenstein hernia repair: 5-year outcomes from the Finn Mesh Study. World J Surg. 2021;45:459–64.
Chung Y, Choi JW, Kim HC, Kim SH, Choi SI. Feasibility of totally extraperitoneal (TEP) laparoscopic hernia repair in elderly patients. Hernia. 2019;23:299–303.
Dunker MS, Stiggelbout AM, van Hogezand RA, Ringers J, Griffioen G, Bemelman WA. Cosmesis and body image after laparoscopic-assisted and open ileocolic resection for Crohn’s disease. Surg Endosc. 1998;12:1334–40.
Acknowledgements
The authors thank Hitomi Kanie for her management of the data collection and Tomoko Kawanishi for conducting the telephone interviews of the patients. We also thank Prof. Tina Tajima of St. Marianna University School of Medicine for her meticulous English editing.
Funding
The work described herein was supported by departmental resources only.
Author information
Authors and Affiliations
Contributions
YS conceived and designed the study; YS, MW, MM, and KT acquired the data; YS and MW analyzed and interpreted the data; YS drafted the manuscript; MW, MM, KT, YN, MT, KF, MO, TM, and HA critically revised the manuscript; and MW, MM, KT, YN, MT, KF, MO, TM, and HA approved submission of the manuscript in its current form.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest in association with the present study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Suzuki, Y., Wakasugi, M., Mikamori, M. et al. Long-term outcomes of single-incision versus multiport laparoscopic totally extra-peritoneal inguinal hernia repair: a single-institution experience of 186 consecutive cases. Surg Today 52, 114–119 (2022). https://doi.org/10.1007/s00595-021-02323-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-021-02323-4