Abstract
Purpose
This retrospective study aimed to analyze the relationship between tooth extraction and osteoradionecrosis (ORN) occurrence. The irradiation field, dose, and time interval between radiotherapy (RT) and ORN were reviewed. We also discuss appropriate guidelines for prophylactic tooth extraction.
Methods
A total of 33 patients treated for grade ≥2 (clinical) ORN in our department from 2002 to 2014 were enrolled. The following epidemiological data were retrospectively gathered: age, sex, histological diagnosis, primary tumor sites, radiation dose, chemotherapy, site of ORN, relationship between tooth extraction and ORN occurrence, and time interval between tooth extraction and the initiation or end of RT.
Results
Twenty-one percent of ORN cases resulted from tooth extraction. The most common site of ORN (82 %) was the mandibular molar region. About half of ORN cases (49 %) occurred within 2 years after RT. All patients who received tooth extraction after RT developed ORN (100 %) independently of time interval between tooth extraction and the end of RT (median interval, 37.5 months; range, 27–120 months). In contrast, only 50 % of patients who received tooth extraction before RT developed ORN. There may have been an association between the irradiation field and the site of ORN development
Conclusions
ORN occurrence due to tooth extraction was 21 %. Occurrence timing of ORN did not depend on time interval between tooth extraction and the end of RT. The irradiation field is certainly related to the site of ORN; therefore, prophylactic tooth extraction should be performed in consideration of the proposed radiation field and dose.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Radiotherapy (RT) plays an indispensable role in the current management of head and neck malignancies. Osteoradionecrosis (ORN) of the jaw, defined as exposed bone persisting for more than 6 months [1], is one of the serious late complications of RT for head and neck malignancies. When ORN of the jaw progresses, patients develop trismus, neuropathic pain, and chronic drainage, resulting in severely reduced quality of life. Although there are numerous reports on the medical management of ORN of the jaw, including surgical and conservative interventions [2–5], prevention of ORN is the most important issue for dental oncologists. A previous study by Ben-David et al. [6] reported that meticulous prophylactic dental care combined with the dosimetric advantages offered by intensity-modulated radiation therapy is likely an essential factor in reducing the incidence of ORN. That study found that the use of a strict prophylactic dental care policy and intensity-modulated radiation therapy resulted in no cases of clinical ORN.
A systematic review by Nabil et al. [7] reported that the incidence of ORN after dental extraction in irradiated patients was 7 %. A previous retrospective study of 830 cases between 1969 and 1999 reported that the time interval between RT and the occurrence of ORN was variable (median, 13 months; range, 2–122 months), indicating the time independence of ORN occurrence [8]. In prophylactic dental care and post-RT dental management, the following issues remain unresolved: (A) to what extent unrestorable teeth should be prophylactically removed and (B) how long regular dental follow-up should be performed. Although ORN can occur spontaneously as a result of odontogenic diseases [7], tooth extraction before or after RT is considered the most common initiating cause of ORN. However, prophylactic dental extraction remains a controversial issue, because a previous report revealed that pre-RT tooth extraction did not reduce the risk of ORN [9].
The objective of this study was to retrospectively review the cause of ORN, with a focus on the relationship between tooth extraction and ORN occurrence. The irradiation field, dose, and the occurrence timing of ORN were also assessed. Based on the results of this retrospective study, we discuss appropriate guidelines for prophylactic tooth extraction and the duration of post-RT dental follow-up.
Materials and methods
A total of 33 patients with ORN were treated in our department from 2002 to 2014. In the present study, ORN was defined according to the Common Terminology Criteria for Adverse Events v3.0 (CTCAE) (http://ctep.canchttp://ctep.cancer.gov/forms/CTCAEv3.pdf. http://ctep.cancer.gov/forms/CTCAEv3.pdf). ORN definition and grading according to CTCAE v3.0 includes grade 1: asymptomatic, radiographic findings only; grade 2: symptomatic and interfering with function, minimal bone removal indicated; grade 3: symptomatic and interfering with daily life activities, operative intervention or hyperbaric oxygen indicated; and grade 4: disabling. This study evaluated patients who had grade ≥2 ORN, defining grade 2 as the loss of mucosal coverage and bone exposure lasting 3–6 months. The following epidemiological data were retrospectively gathered from the medical charts: age, sex, comorbidity, histological diagnosis, primary tumor sites, radiation dose, chemotherapy, site of ORN, relation between tooth extraction and ORN, and time interval between RT and tooth extraction. This was a nonrandomized, retrospective study of patients and was thus granted exemption from institutional review board approval by our institution.
Results
Patient characteristics are shown in Table 1. All patients were treated conventional RT (i.e., there were no patients who received intensity-modulated radiation therapy [IMRT] and volumetric modulated arc therapy). None of the patients received antiresorptive medications, such as bisphosphonates and RANK ligand inhibitor. Five of 33 patients (15 %) with ORN had diabetes mellitus. Twenty-four of 33 patients (73 %) had periodontal disease. No trauma (e.g., trauma induced by prosthesis) caused ORN in this study.
In two patients, the irradiation dose recorded in the medical chart was less than 50 Gy (Table 1). One of these was an 82-year-old woman who received chemoradiotherapy (CRT) for maxillary carcinoma during the study period. She had undergone CRT and surgical intervention for maxillary sinus cancer at another hospital 32 years earlier. The second patient was a 71-year-old man who received RT for oral cancer during the study period. He had received brachytherapy for oral cancer at another hospital 26 years earlier. Therefore, the total irradiation dose in these patients was more than 50 Gy. Twenty-five of 33 patients (76 %) received chemotherapy in this study duration. Cisplatin alone was the most common in 15 patients (n = 25; 60 %).
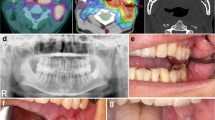
Figure 1a shows the site of ORN. Posterior mandible was the most common site of ORN (82 %). Figure 1b shows the time interval between RT and diagnosis of ORN. Forty-nine percent of ORN were diagnosed within 2 years after RT.
The relation of ORN and tooth extraction was assessed (Fig. 2). In 33 patients with ORN, 11 patients (33 %) received tooth extraction before (n = 4), during (n = 1), and after RT (n = 6). In 7 of 11 patients who received tooth extraction and do not achieve socket healing, ORN developed in the extraction site; therefore, the incidence of ORN due to tooth extraction was 21 % (7/33). In four patients who received tooth extraction, ORN developed independently of tooth extraction (extraction socket healed, but ORN occurred apart from the extraction socket). Two out of 4 patients who received tooth extraction before RT developed ORN (50 %), and their time intervals between tooth extraction and the initiation of RT were 13 and 19 days. In all patients who received tooth extraction after RT, ORN developed (100 %), and their time intervals between tooth extraction and the end of RT were 27, 28, 36, 39, 42, and 120 months (median interval 37.5 months).
Table 2 shows the relationship between the site of primary tumor and ORN. ORN occurred in both the maxilla and mandible in patients who received RT of the oral cavity and hypopharynx. In two patients with major salivary gland carcinoma (submandibular gland in both), ORN developed in the mandibular region. In three patients with paranasal sinus cancer, ORN developed only in the maxillary molar region. ORN occurred on the side contralateral to the primary lesion in patients with oral, nasopharyngeal, oropharyngeal, hypopharyngeal, and major salivary gland cancer (Table 2). In 5 of 33 patients (15 %), ORN developed in the bilateral mandibular molar region. Three of 5 bilateral cases of ORN developed without an obvious cause, such as tooth extraction.
Discussion
In this retrospective study, we aimed to analyze the cause and occurrence timing of ORN of the jaw, focusing on prophylactic dental extraction and duration of post-RT dental follow-up, in patients with head and neck cancer who received RT.
First of all, although a systematic review reported no ORN in any patients who received a radiation dose of less than 60 Gy [7], we found ORN in two patients who received a radiation dose of less than 50 Gy. These patients had received previous treatments including CRT or brachytherapy at other hospitals long before RT during this study period. A previous study mentioned that particular attention should be paid to teeth in parts of the jaw expected to receive a radiation dose greater than 50 Gy [6]. Other previous study reported that 50 and 60 Gy saw the most significant differences between the ORN group and the comparison group [10]. Our study indicates that primary RT less than 50 Gy has a low risk of causing ORN. In this study, 75 % of ORN patients received chemotherapy; nevertheless, chemotherapy did not significantly increase the incidence of ORN in some previous studies [9, 11]. There are no studies and literature reviews that indicate the correlation between chemotherapy and ORN as far as we know.
Second, the relation between primary lesion and ORN site was assessed, and we found that ORN can occur in both the maxilla and mandible after RT of the oral cavity and hypopharynx (Table 2). Although ORN did not occur in the maxilla in patients with oropharyngeal cancer in this study, the irradiation field for oropharyngeal cancer often involves both the maxilla and mandible. For the treatment of nasopharyngeal cancer, the irradiation field often involves both the upper and lower jaw, too. Severe radiation-induced salivary gland damage frequently occurs in these patients. Therefore, particular attention, including prophylactic extraction of teeth with severe caries and periodontitis, is needed in patients who are scheduled for RT of oral, nasopharyngeal, oropharyngeal, and hypopharyngeal cancer. This study also indicated that ORN occurred independently of the laterality in these patients, because ORN occurred on both the diseased and undiseased sides except in patients with nasal cavity (paranasal cavity) cancer (Table 2). In two patients who had submandibular gland cancer, ORN developed only in the mandibular region. We propose that prophylactic tooth extraction, especially in the mandible, should be performed before RT of the submandibular glands. This is because the irradiation field for submandibular gland cancer often involves only the lower jaw. None of the patients in this study received RT for parotid gland cancer. Parotid gland cancer is generally treated with rectangular irradiation; therefore, the irradiation dose is considered low in the maxilla and mandible of the contralateral side. In this study, three patients received RT for cancer of the paranasal sinus (one received carbon-ion therapy alone and the other received concomitant superselective intra-arterial chemotherapy) and subsequently developed ORN in the maxillary molar region. Prophylactic maxillary tooth extraction should be performed in patients scheduled for RT for nasal and paranasal cavity cancer. However, extraction of maxillary teeth near the tumor should be avoided before RT to prevent neoplasm spread and unexpected bleeding. It must also be noted that the necrotic bone is often exposed as a result of tumor necrosis after superselective intra-arterial chemotherapy and concomitant RT; therefore, careful oral care should be performed in these patients. Our study did not include patients who received RT for larynx and thyroid gland cancer. This was probably due to low risk of ORN in these patients, because the irradiation field for larynx and thyroid gland cancer did not involve the jaw and salivary glands. Patients who received only neck irradiation probably had low risk of ORN.
Prophylactic tooth extraction remains controversial. Some studies have reported a low prevalence of ORN associated with tooth extraction after RT (2.14 % [12] and 1.7 % [13]). A recent large retrospective cohort study reported that tooth extraction after RT was not an independent risk factor for ORN [11]. Some studies have found no apparent benefit of pre-RT extractions to reduce the risk of ORN and have indicated that pre-RT extractions can cause ORN [1, 11]. However, in one of these reports, the authors noted that a complete dental evaluation by an experienced practitioner is strongly recommended before RT and that it is important to discuss with patients the implications of extraction versus retaining teeth in the proposed high-dose RT field [11]. All unrestorable teeth and/or teeth with periodontal problems must be extracted to reduce the post-RT extractions that contribute to ORN [14]. Socket healing after tooth extraction usually requires 14 days, but in this study, two patients received tooth extraction 13 and 19 days before the start of RT. The timing of prophylactic tooth extraction is one of unresolved issues. To solve this issue, careful information sharing between dental oncologist and radiation oncologist is essential.
We regard strict criteria for prophylactic tooth extraction, such as those proposed by Ben-David et al. [6], as important in preventing ORN. Based on the results of this study and numerous previous reports, we propose that prophylactic tooth extraction should be performed with consideration of the proposed radiation field and dose, as shown in Table 3. Healthy dentition should be maintained in irradiated patients [1]; therefore, careful long-term follow-up by trained dental oncologists is essential after RT. However, the appropriate duration of follow-up is questionable because the occurrence of ORN is not time dependent [8]. The large majority of ORN events have been reported to occur within 2 years after RT [8]. It has been recommended that tooth extraction be avoided within 2 years after RT to reduce the risk of ORN [10]. On the other hand, a systematic review notes that the period 2–5 years after RT had the highest incidence of ORN after post-radiation extraction [7]. In our study, all patients who underwent tooth extraction after RT developed ORN (Fig. 2). In a previous report, patients were followed up by a dental oncologist and a radiation oncologist and/or head and neck surgeon to assess dental condition and the need for post-RT extractions at 6- to 8-week intervals for the first year, 2- to 4-month intervals for the second and third years, 6-month intervals for the fourth and fifth years, and annually thereafter [9]. We agree with their argument and propose that patients who received RT for the head and neck malignancies should be followed up by dental oncologists as long as possible.
Finally, we must mention the limitations of this study. The main limitation is the retrospective nature of the data with a small sample size. Second, this study did not include the developing alternatives to conventional RT, such as IMRT. A recent review noted that every patient treated with various types of RT should get enrolled on a clinical study and data collated meticulously to document and learn from experiences, because clinical data are currently sparse [15]. Moreover, the exact IMRT advantage on ORN remains to be elucidated [16]. Third, this study evaluated only diabetes mellitus as comorbidity. A recent study reported that the rate of patients with diabetes mellitus and ORN was 5.6 % [11]. Fourth, this study did not include the patient who received tooth extraction after RT and did not develop ORN. We must note that tooth extraction after RT does not cause absolutely ORN in all cases. Causal tooth of severe infection should be eliminated even in patients who received RT. To overcome these problems, a prospective study including a large sample size, cases receiving IMRT, and evaluation of comorbidities (such as smoking and alcohol) should be conducted in the near future.
As conclusions, about half of ORN cases (49 %) occurred within 2 years after RT. Only 21 % of ORN cases in this study were caused by tooth extraction. Occurrence of ORN did not depend on time interval between tooth extraction and the end of RT. The irradiation field is certainly related to the site of ORN; therefore, prophylactic tooth extraction should be performed in consideration of the proposed radiation field and dose.
References
Wahl MJ (2006) Osteoradionecrosis prevention myths. Int J Radiat Oncol Biol Phys 64:661–669
Lyons A, Ghazali N (2008) Osteoradionecrosis of the jaws: current understanding of its pathophysiology and treatment. Br J Oral Maxillofac Surg 46:653–660
Jacobson AS, Buchbinder D, Hu K, Urken ML (2010) Paradigm shifts in the management of osteoradionecrosis of the mandible. Oral Oncol 46:795–801
Baumann DP, Yu P, Hanasono MM, Skoracki RJ (2011) Free flap reconstruction of osteoradionecrosis of the mandible: a 10-year review and defect classification. Head Neck 33:800–807
D’Souza J, Lowe D, Rogers SN (2014) Changing trends and the role of medical management on the outcome of patients treated for osteoradionecrosis of the mandible: experience from a regional head and neck unit. Br J Oral Maxillofac Surg 52:356–362
Ben-David MA, Diamante M, Radawski JD, Vineberg KA, Stroup C, Murdoch-Kinch CA, et al. (2007) Lack of osteoradionecrosis of the mandible after intensity-modulated radiotherapy for head and neck cancer: likely contributions of both dental care and improved dose distributions. Int J Radiat Oncol Biol Phys 68:396–402
Nabil S, Samman N (2011) Incidence and prevention of osteoradionecrosis after dental extraction in irradiated patients: a systematic review. Int J Oral Maxillofac Surg 40:229–243
Reuther T, Schuster T, Mende U, Kübler A (2003) Osteoradionecrosis of the jaws as a side effect of radiotherapy of head and neck tumour patients—a report of a thirty year retrospective review. Int J Oral Maxillofac Surg 32:289–295
Chang DT, Sandow PR, Morris CG, Hollander R, Scarborough L, Amdur RJ, et al. (2007) Do pre-irradiation dental extractions reduce the risk of osteoradionecrosis of the mandible? Head Neck 29:528–536
Tsai CJ, Hofstede TM, Sturgis EM, Garden AS, Lindberg ME, Wei Q, et al. (2013) Osteoradionecrosis and radiation dose to the mandible in patients with oropharyngeal cancer. Int J Radiat Oncol Biol Phys 85:415–420
Chen J, Wang C, Wong Y, Wang C, Jiang R, Lin J, et al. (2014) Osteoradionecrosis of mandible bone in oral cancer patients—associated factors and treatment outcomes. Head Neck. doi:10.1002/hed.23949
Sulaiman F, Huryn JM, Zlotolow IM (2003) Dental extractions in the irradiated head and neck patient: a retrospective analysis of Memorial Sloan-Kettering Cancer Center protocols, criteria, and end results. J Oral Maxillofac Surg 61:1123–1131
Koga DH, Salvajoli JV, Kowalski LP, Nishimoto IN, Alves FA (2008) Dental extractions related to head and neck radiotherapy: ten-year experience of a single institution. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 105:e1–e6
Koga DH, Salvajoli JV, Alves FA (2008) Dental extractions and radiotherapy in head and neck oncology: review of the literature. Oral Dis 14:40–44
Parvathaneni U, Laramore GE, Liao JJ (2012) Technical advances and pitfalls in head and neck radiotherapy. J Oncol 2012:597467
De Felice F, Musio D, Tombolini V (2015) Osteoradionecrosis: an old toxicity in the IMRT era? Oral Oncol 51:e60–e61
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
Not required.
Conflict of interest
The authors indicate full freedom of investigation and no potential gconflicts of interest.
Financial disclosure
There was no grant support for this study.
Rights and permissions
About this article
Cite this article
Wanifuchi, S., Akashi, M., Ejima, Y. et al. Cause and occurrence timing of osteoradionecrosis of the jaw: a retrospective study focusing on prophylactic tooth extraction. Oral Maxillofac Surg 20, 337–342 (2016). https://doi.org/10.1007/s10006-016-0570-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10006-016-0570-5