Abstract
Pediatric bipolar disorder (BD) and unipolar disorder (UD) share common symptomatic and functional impairments. Various brain imaging techniques have been used to investigate the integrity of brain white matter (WM) and gray matter (GM) in these disorders. Despite promising preliminary findings, it is still unclear whether these alterations may be considered as common trait markers or may be used to distinguish BD from UD. A systematic literature search of studies between 1980 and September 2013 which reported WM/GM changes in pediatric and adolescent BD/UD, as detected by diffusion tensor imaging and voxel-based analysis was conducted. Of the 34 articles judged as eligible, 17 fulfilled our inclusion criteria and were finally retained in this review. More abnormalities have been documented in the brains of children and adolescents with BD than UD. Reductions in the volume of basal ganglia and the hippocampus appeared more specific for pediatric UD, whereas reduced corpus callosum volume and increased rates of deep WM hyperintensities were more specific for pediatric BD. Seminal papers failed to address the possibility that the differences between unipolar and bipolar samples might be related to illness severity, medication status, comorbidity or diagnosis. UD and BD present both shared and distinctive impairments in the WM and GM compartments. More WM abnormalities have been reported in children and adolescents with bipolar disease than in those with unipolar disease, maybe as a result of a low number of DTI studies in pediatric UD. Future longitudinal studies should investigate whether neurodevelopmental changes are diagnosis-specific.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bipolar disorder (BD) is a chronic and disabling disorder characterized by relevant impairments in social, emotional, and academic functioning in childhood and early adolescence [1, 2]. The prevalence rate of bipolar spectrum disorder has been estimated to be 2 % among children and adolescents in the community [3]. Early-onset BD is usually associated with poorer performance, comorbidity with substance abuse, suicide attempts, hospitalization, and legal difficulties [4–7]. Similarly, major depressive disorder (MDD) in children and adolescents is associated with a fourfold increased risk of recurrence in adulthood, long-term functional impairment and adult disability [8, 9].This poor outcome in children and adolescents with unipolar disorder (UD) or BD emphasizes the need for adequate understanding of the mechanisms underlying these affective conditions [10–14].
Although many studies attempted to elucidate the neurobiological basis of affective disorders in children and adolescents, their pathogenesis remains unclear. During the last decades, brain imaging techniques provided new approaches to detect in vivo structural and functional brain changes. Magnetic resonance imaging studies reported a wide range of morphometric alterations in both pediatric BD [15–20] and UD [21–27].
Diffused GM abnormalities have been found in patients with pediatric BD, specifically volumetric changes in the anterior limbic network (ALN), including the prefrontal regions, thalamus, striatum, amygdala, hippocampal complex, and the midline cerebellum [28].
In their meta-analysis, Arnone et al. [29] found that reduced prefrontal cortex and increased globus pallidus volumes are some of the most consistent findings in children and young adults with BD. There is also evidence that adolescents with a recent single manic episode exhibited smaller subgenual cingulate cortex volumes than healthy controls (HC) [30], whereas drug-naïve adult individuals with a first-episode depression showed reduced GM volume in the right pre-supplementary motor area [31]. Reduced GM has also been reported in the prefrontal cortex, amygdala, and hippocampi of depressed children. However, these results were inconsistent, due to heterogeneous samples and differences in terms of gender, illness duration, severity of symptoms, medication, or episode states [32–34].
A second line of studies explored white matter (WM) integrity in these disorders using diffusion tensor imaging (DTI) [35]. Studies using a region-of-interest (ROI) approach reported abnormalities in prefrontal–limbic circuits that have been associated with affective dysregulation in BD [33]. Specifically, lower fractional anisotropy (FA) has been found in the anterior corona radiata (ACR) [36] and superior frontal WM in pediatric BD [37]. Recently, studies using either voxel-based morphometry (VBM) analysis or tract-based spatial statistics (TBSS) reported WM abnormalities and lower FA in several brain regions [38–40].
Similarly, DTI studies conducted in pediatric UD reported microstructural WM abnormalities during the first episode of depression in both depressed young adults [41] and adolescents [42].
There are also some neuroimaging studies that were conducted among unaffected but high risk of BD/MDD individuals aimed to reveal WM changes [43–45].
Few studies in the current literature examined whether some VBM/DTI abnormalities may help in distinguishing individuals with UD or BD. For example, Cardoso de Almeida and Phillips [46] suggested more widespread abnormalities in WM connectivity and more WM hyperintensities in BD than UD, more habenula volume reductions in BD but not UD, and differential patterns of functional abnormalities in emotion regulation and attentional control neural circuitry in both BD and UD. There is, however, the pressing need for more neuroimaging studies using larger samples sizes, and comparing BD and UD depressed subjects.
In this context, we aimed to systematically review the current literature to determine whether pediatric/adolescent BD is associated with greater or more consistent WM or GM alterations than pediatric/adolescent UD.
Methods
Information sources, search strategy, and study selection
A detailed search strategy was used to identify relevant studies. In order to provide a new and timely critical review of VBM/DTI abnormalities and their possible involvement in children/adolescents with UD or BD, we performed a systematic PubMed/Medline, Scopus, and Science Direct search to identify all papers and book chapters in the English language during the period between 1980 and January 2014.
The search used first the following terms: “Voxel-based morphometry analysis”, OR “VBM analysis”, AND “Diffusion tensor imaging” OR “DTI” AND “White matter hyperintensities” OR “White matter lesions” OR “White matter abnormalities” OR “White matter changes signals” AND “Grey matter hyperintensities” OR “Grey matter lesions” OR “Grey matter abnormalities” to investigate “pediatric and adolescent samples with bipolar disorder” OR “PBD” OR “Bipolar disorder in children and adolescents” AND subsequently the same terms to investigate “Pediatric and adolescent samples of unipolar disorders” OR “Unipolar disorders in children and adolescents”. When a title or abstract seemed to describe a study eligible for inclusion, the full article was examined to assess its relevance based on the inclusion criteria. Two blinded, independent researchers (GS and MP) conducted a two-step literature search. Any discrepancies between the two reviewers were resolved by consultations with the senior authors (JH, MA, RJ, PG). The reference lists of the articles were also manually checked for relevant studies while other publications were cross-referenced for any additional published articles. Only English language full-text articles reporting original data about the main topic were included.
Study design and eligibility criteria
We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses’ (PRISMA) guidelines [47]. Studies were included according to the following criteria: (a) being an original paper in a peer-reviewed journal and (b) containing an analysis of VBM/DTI abnormalities in samples of bipolar/unipolar disorders. Figure 1 summarizes the search strategy used for selecting studies (identification, screening, eligibility, inclusion process) in the present review. We excluded studies explicitly conducted on high-risk subjects. Papers that were not written in English, book chapters, conference abstracts, and case studies were not reviewed.
Recorded variables
We retained the following variables for each article about VBM/DTI abnormalities and their possible involvement in bipolar/unipolar disorders of children and adolescents: sample characteristics, study design, treatment-resistant definition, location of WM/GM abnormalities, main findings, limitations, and conclusions (Table 1).
Results
Number of selected studies
The combined search strategy yielded a total of 68 articles, of which 34 full-text articles were screened and 34 excluded. Articles not published in peer-reviewed journals and not in English, papers without abstracts, abstracts that did not explicitly mention the link between WM/GM abnormalities and bipolar/unipolar disorders in children and adolescents, articles published before 1980, and those with unclear data concerning materials and methods or number of patients analyzed, were excluded. Of the initial 45 papers, 34 were considered of relevance and 27 were judged eligible. However, seven full-text articles were also excluded due to their low relevance (two studies were conducted on FEP patients) for the main theme, and three articles were excluded as they included high-risk subjects. This left 17 papers that fulfilled inclusion criteria, including 326 patients and 360 controls.
Types of studies selected
Several studies documented the association between WM/GM abnormalities and bipolar/unipolar disorders in children and adolescents. Table 1 summarizes the most relevant studies about DTI neuroimaging abnormalities in children and adolescents with unipolar disorder whereas Table 2 includes the nine most relevant studies about DTI neuroimaging abnormalities in children and adolescents with bipolar disorder. Table 3 summarizes the two most relevant studies about VBM neuroimaging abnormalities in children and adolescents with UD, whereas Table 4 includes the five most relevant studies about VBM neuroimaging abnormalities in children and adolescents with bipolar disorder. These studies were all cross-sectional in nature with the exception of the study of Adleman et al. [54], including an initial cross-sectional phase and a subsequent 2-year follow-up period.
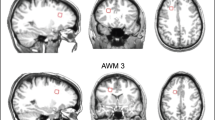
DTI studies in samples of children and adolescents with BD
Nine DTI studies showed neuroimaging abnormalities in samples of children/adolescents with BD. Significantly lower FA was found by Lu et al. [33] in the anterior limb of the internal capsule (ALIC) of 35 pediatric subjects presenting with first-episode type I BD compared with 46 controls. Gao et al. [35] reported significantly lower FA values in the right anterior cingulate of pediatric bipolar children in comparison with healthy volunteers. Lower FA values were reported by Saxena et al. [49] in the callosal genu and anterior commissure of 10 bipolar adolescents than with 10 age-matched HC. James et al. [50] reported reduced GM density in the left orbito-frontal cortex, left pars triangularis, right premotor cortex, occipital cortex, right occipital fusiform gyrus, and right crus of the cerebellum of 15 bipolar subjects with psychosis, compared to 20 euthymic age- and gender-matched controls. Reduced FA values were also shown in the anterior corpus callosum associated with the prefrontal cortices. Voxel-based morphometry, tract-based spatial statistics, and probabilistic tractography were all used to analyze the DTI data.
Gönenç et al. [51] suggested that FA was reduced and radial diffusivity increased on the left side, whereas on the right side, trace was increased and T2 values were decreased in subjects with BD compared with control subjects. Significantly lower FA was found in the ACR of 13 children/adolescents with BD compared to 15 controls. Also, FA and regional fiber coherence index (r-FCI) values were significantly lower in ADHD than BD and controls in both the ALIC and superior region of the internal capsule (SRI) [36]. The authors suggested that apparent diffusion coefficient was significantly increased in specific brain areas of subjects with ADHD compared to both bipolar subjects and controls.
Kafantaris et al. [40] found that 26 adolescents with BD type I showed alterations in WM regions, including lower FA in the right orbital frontal lobe and higher apparent diffusion coefficient in the right and left subgenual region. Patients with BD manifested a significant correlation between lower FA across regions and lower visuomotor speed. Lower FA values compared to 18 age- and IQ-matched controls in the fornix, left mid-posterior cingulate gyrus, throughout the corpus callosum, in fibers extending from the fornix to the thalamus, and in parietal and occipital corona radiata bilaterally have also been reported in 21 bipolar adolescents by Barnea-Goraly et al. [39].
Finally, Frazier et al. [38] found that 10 bipolar children exhibited reduced FA in the bilateral superior frontal tracts, including the SLF I and CG-PACWM relative to eight HC and seven children at risk for BD. Furthermore, bipolar children showed reduced FA in left orbital frontal WM and the right corpus callosum body. Bipolar children also exhibited lower FA in the right and left CG-PACWM than for children at risk for BD (AR-BPD). In addition, lower FA relative to HC was found in bilateral SLF I in both the BD and AR-BPD groups.
DTI studies in samples of children and adolescents with UD
Only one DTI study reported brain imaging abnormalities in samples of children and adolescents with UD. Cullen et al. [42] found that 14 adolescents with MDD exhibited lower FA in the WM tract connecting the subgenual ACC to amygdala in the right hemisphere when compared with 14 healthy volunteers.
VBM studies in samples of children and adolescents with BD
Five VBM studies reported neuroimaging abnormalities in samples of children and adolescents with BD. Adleman et al. [54] reported that the GM volumes of the pre-SMA, dorsolateral prefrontal cortex (DLPFC) and insula were increased in 68 HC compared with 55 with BD and 78 with severe mood dysregulation. Regarding globus pallidus, increased GM volume in BD compared with healthy volunteers and severe mood dysregulation patients have been reported. After 2 years of follow-up, an abnormal increase in the volume of the superior/inferior parietal lobule as well as in the precuneus of 34 BD patients was found. Hajek et al. [55] also reported that 19 patients with BD who had a substantial burden of illness and a <3 months of lifetime exposure to lithium exhibited smaller right inferior frontal gyrus (rIFG) volumes when compared with 29 control subjects (having a substantial burden of long-lasting BD). This negative association was not replicated in lithium-treated BD patients.
As suggested by Jarvis et al. [56], cannabis use disorder was associated with structural differences in frontal and temporal cortical regions, as well as subcortical regions such as the caudate (hypothesized to be involved in emotional and motivational regulation); this study was performed in 14 adolescents with BD, of which seven were cannabis consumers.
Dickstein et al. [57] found that 20 bipolar subjects had reduced GM volume in the left DLPFC (Brodmann area 9) and, using a less conservative statistical threshold, in the left accumbens and left amygdala, when compared to 20 controls. Significantly greater GM volume has been also found in 10 bipolar subjects in the basal ganglia, thalamus and left temporal lobe bilaterally by Wilke et al. [58] when compared to 52 age- and gender-matched controls. In addition, localized GM deficits in bipolar subjects were also reported in the medial temporal lobe, orbito-frontal cortex and anterior cingulate.
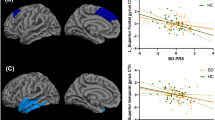
VBM studies in samples of children and adolescents with UD
Only two VBM studies reported brain imaging abnormalities in samples of children and adolescents with UD. Shad et al. [52] found significantly lower GM volume in the frontolimbic regions and caudate of 22 MDD adolescents when compared with 22 age- and gender-matched normal controls. Also, Frodl et al. [53] suggested that the left prefrontal cortex was smaller in 24 patients with MDD than in 27 controls. Childhood stress predicted hippocampal WM abnormalities.
Conclusions and discussion
Summary of main results
The present review is, to our knowledge, the first study examining whether pediatric/adolescent BD is associated with greater or more consistent WM/GM alterations than pediatric/adolescent UD. We aimed to investigate whether some VBM/DTI abnormalities can distinguish samples of children/adolescents with BD or UD from HC.
Only three VBM/DTI studies [42, 52, 53] investigated the existence of brain imaging abnormalities in samples of children/adolescents with UD versus fourteen VBM/DTI studies [35, 36, 38–40, 48–51, 54–58] showing neuroimaging abnormalities in pediatric/adolescent samples with BD.
Based on the main findings, more WM abnormalities have been reported in BD children/adolescents compared to those with UD. In particular, bilateral abnormalities in WM connectivity of brain regions and neural circuitry critically involved in emotion regulation and sensory processing have been reported in BD, but not UD. The bilateral findings in BD, but not UD, indicated more widespread WM connectivity alterations in BD compared to UD. WM tracts abnormalities may be related to both axonal disorganization and demyelization or apoptosis; future studies should directly investigate this important issue using recent techniques such as Magnetization Transfer Ratio or axonal calibration [59].
Main neuroimaging abnormalities in children/adolescents with BD
Several studies have suggested the existence of WM/GM abnormalities in samples of children/adolescents with BD. In their meta-analytic study on adults, Kempton and colleagues [60] suggested that basal ganglia and hippocampal volume reductions seem to be more specific for MDD than BD, whereas reduced corpus callosum cross-sectional area and increased rates of deep WM hyperintensities seem to be more common in BD than MDD. As argued below, these findings have only partially been confirmed in samples of children and adolescents. However, alterations throughout the amygdala and basal ganglia appear poorly specific, since they have also been documented in BD [42, 54, 58] and many other neuropsychiatric disorders [42]. The presence of subcortical alterations within the amygdala and basal ganglia in childhood [61] could subsequently extend to prefrontal cortical regions continuing to develop into adulthood. These frontolimbic abnormalities occurring during childhood and early adolescence would suggest the existence of neurodevelopmental conditions [62]. Abnormalities throughout the anterior limbic system and associated prefrontal regions have been hypothesized to be involved in affective, cognitive and vegetative symptoms in BD [63–65]. In line with results in adult samples, one of the most common brain region in which abnormalities have been documented in pediatric/adolescent bipolar samples is the corpus callosum [38, 39, 50]. The corpus callosum represents the major interhemispheric commissure connecting most of the neocortical brain regions and including fundamental brain networks related to attention, memory, language and emotional states [66–72]. The corpus callosum develops during childhood/adolescence as demonstrated by the increased size [73], reduced signal intensity [72] and increased FA values [74].
Some authors [75, 76] suggested that, although the signal intensity of the corpus callosum is reduced and its shape altered in pediatric/adolescent bipolar samples, no differences in size have been reported between bipolar children/adolescents and healthy volunteers.
Barnea-Goraly et al. [39] suggested an abnormal maturation process in the corpus callosum of bipolar subjects, as reflected by the lower FA in adolescence—representing reduced coherence or aberrant myelination and increasing FA with age. This might be due to changes in the extracellular compartment related to abnormal perivascular structures [73], but might also be related to the different measurements of FA in the corpus callosum of adults and adolescents [77].
Abnormalities in the CC3-motor area of the corpus callosum interconnecting right and left paracingulate, anterior cingulate, supplementary motor areas and lateral premotor regions in the frontal lobes could be related to alterations in activity and motivation—that are frequently observed in children with BD [38].
As hypothesized, WM integrity in prefrontal limbic network has been found to be significantly altered as demonstrated by the lower FA in children with BD. Two studies suggested that there are changes in the WM of the ALIC [33, 36]. Greater alterations have been reported in the WM microstructure of the left ALIC with pediatric bipolar onset compared to adult bipolar onset [36].
Disorganized integration of prefrontal–limbic circuitry associated with affective dysregulation has been hypothesized in BD [33, 78]. The prefrontal structures appear to show dysfunctions in modulating subcortical structures. The alterations in the WM microstructure of the ALIC have also been demonstrated in another DTI tractography study [79]. This may increase the vulnerability to develop bipolar illness, by altering the processing of emotional information throughout the limbic system.
Main neuroimaging abnormalities in children/adolescents with UD
Only three VBM/DTI studies [42, 52, 53] showed the existence of brain imaging abnormalities in samples of children and adolescents with UD. Shad et al. [52] showed lower GM volumes in the frontolimbic areas and caudate of depressed adolescents than in healthy volunteers. These authors also suggested that GM changes in the striatum, especially in the caudate nucleus, may relate to the initial presentation of MDD. The involvement of frontolimbic regions in the pathogenesis of adult MDD has been extensively reported [79–83]. Dorsolateral and orbito-frontal regions of the prefrontal cortex (PFC) play a critical role in self-monitoring and executive control of the medial PFC and limbic system [84, 85].
As suggested by Frodl et al. [53], even subtle changes of the hippocampal WM may be relevant in the pathogenesis of adolescent depression. Hippocampal abnormalities have been reported in both unipolar depressed children and adolescents [53], whereas other authors suggested the existence of alterations in the WM tract connecting subgenual ACC to amygdala in the right hemisphere [42]. Consistent evidence [86–88] suggested that the subgenual ACC is a critical brain structure functionally connected with the activity of frontolimbic regions. An alteration in the ACC, including disorganized integrity of WM microstructure of the uncinate fasciculus would provide an abnormal regulatory input to the amygdala [89]. These WM changes may reflect a critical axonal reduction or cell loss in the outgoing fibers of the fimbria to the structures of the limbic system and may be responsible for the cognitive/emotional disturbances of depression. There is evidence that childhood trauma (e.g., physical or sexual abuse) may be associated with reduced hippocampal volume in subjects who subsequently develop depressive disorders in adulthood [90–92].
Cullen et al. [42] also suggested that there are lower mean FA values (reflecting reduced WM integrity) in right WM tracts connecting subgenual ACC to the amygdala in adolescents with UD. These authors stated that alterations of this connection may be involved in many neuropsychiatric disorders (e.g., bipolar disorder and schizophrenia).
Methodological differences between VBM analyses and ROI-based approaches could be fundamental in explaining some conflicting findings. This is, for example, the case of the ROI-based study of Chen et al. [23] that failed to demonstrate significant differences in OFC volume between depressed adolescents and controls.
Taken together, these few studies supported the hypothesis that dysfunctions in the microstructure of WM pathways within frontolimbic neural networks are involved in the pathophysiology of UD in children and adolescents.
Tables 5 and 6 summarize the main GM and WM abnormalities and the different brain regions that have been reported as dysfunctional in children and adolescents with BD versus UD, respectively.
Psychotic features in children and adolescents with bipolar/unipolar disorders
Whether data from first-episode psychosis (FEP) samples or BD/UD samples with psychotic features at their first presentation may help clinicians to distinguish between the subsequent (unipolar/bipolar) trajectories of affective illness is currently a matter of debate. Adolescence is an interesting period to compare the phenotypic expressions of BD with psychosis and schizophrenia.
Janssen et al. [93] analyzed data from 70 FEP adolescents and found that smaller right and left thalamus volume was positively correlated with increased severity of sensory integration neurological soft signs. In addition, smaller right caudate volume was effectively associated with increased impairment in sequencing complex motor acts. Extensive abnormalities in the left medial frontal GM volume have been also reported in bipolar patients with psychotic features at their FEP [94] when compared to bipolar patients without psychosis. Specifically, patients with GM volume abnormalities in the left medial frontal gyrus were more likely to be diagnosed with BD type I than subjects with schizophrenia.
Conversely to early-onset schizophrenia, pediatric BD with psychosis has commonly been associated with fewer cognitive deficits [95], although abnormalities in executive functioning and working memory are quite common in both these disorders. Remarkably, larger GM changes and altered WM integrity in motor control regions have been identified in patients with early-onset schizophrenia compared to those with adult-onset disease [96].
Hatton et al. [97] reported that young people with emerging anxiety, affective or psychotic disorders, had reduced left anterior insula GM volume associated with a poorer neurocognitive performance and more severe clinical symptoms compared to controls. However, no significant differences have been suggested between diagnostic groups.
A correlation between altered fornix connectivity (FA values in the right fornix), volumetric reductions in the hippocampus and self-certainty (measuring the confidence in beliefs and judgments) has been reported by Buchy et al. [98]. In their DTI study conducted on either affective or non-affective psychotic individuals, the authors suggested no significant differences between affective or non-affective psychotic subjects.
Also, de Azevedo-Marques Périco et al. [99], aiming to investigate structural brain differences between BD-I subjects and MDD subjects with psychotic features, found more pronounced GM reduction in the right-sided dorsolateral prefrontal cortex and a trend toward left-sided GM deficits in the dorsolateral prefrontal cortex of MDD patients (also after repeating the analysis with scanner site as a confounding covariate) when compared to BD subjects. However, the study did not focus exclusively on pediatric/adolescent samples. There are also studies that did not support the existence of differences between patients with pediatric BD with psychotic features and those with early-onset schizophrenia. Scherk et al. [100] found no significant differences in GM/WM volumes between thirty-five patients with BD who had experienced psychotic symptoms during their illness and thirty-two control subjects. Significant correlations have been observed between GM/WM volumes with number of manic or depressive episodes, duration of illness, existence of psychotic symptoms, and treatment with lithium or antipsychotics.
Also, Zanetti et al. [101] reported no statistically significant differences in the frequencies and severity scores of WM alterations when comparing the affective psychosis (psychotic BD and UD) with non-affective psychosis (schizophrenia/schizophreniform disorder) and control subgroups.
Findings are usually limited by the controversy concerning whether pediatric BD with psychosis and early-onset schizophrenia should be considered as two different diagnostic entities [102]. Also, the interpretation of differences between first-episode BD and MDD subjects may be complicated by the fact that, based on epidemiological studies, approximately 1–5 % of unipolar depressed subjects will develop a bipolar illness beyond one year after their initial identification [103, 104].
Main limitations
Findings must be interpreted in light of the following limitations. The present review allowed to identify a wider array of DTI abnormalities with BD versus UD, but this does not necessarily reflect the actual neurobiology of these disorders. To definitely disentangle this point, a meta-analysis is now required, including a search for unpublished negative findings, or using methods to evaluate whether there was a publication bias. Such a meta-analysis was judged not possible at the time of the review, due to limited and heterogeneous available data.
Also, the low number of studies, especially in UD, and the limited sample size of most studies did not allow the generalization of findings. In particular, studies may be underpowered to detect modest differences within samples. Furthermore, most studies were cross-sectional in nature and did not control for multiple comparisons. Prospective studies appear necessary to distinguish between those with trait markers of BD/UD and those at risk of conversion from MDD to BD. Indeed, follow-up studies have found that 20 to 40 % of adolescents with MDD develop BD within a period of 5 years after the onset of depression [105]. One of the most helpful future direction is to identify biomarkers underlying pathophysiological processes together with the development of symptom dimensions related to BD. Examination of the development of neural abnormalities occurring before the behavioral changes associated with BD, or other mood disorders, is crucial for clinicians.
Moreover, most of the patients included in these studies were under medication at the time of scanning, and this must be considered a confounding factor. Although lithium has been demonstrated to increase GM volume compared to placebo, MRI changes in the brain differ before and after lithium [106], and the effects of antipsychotics and mood stabilizers on WM integrity and GM volumes are still quite unclear [107]. Also, samples were often mixed, including both adolescents with varying mood states. The effects of both mood states and psychiatric comorbidities on VBM/DTI findings have been not adequately evaluated in most studies. The presence of ADHD comorbidity in bipolar children may be interpreted as a potential confounding factor. ADHD symptoms are very frequent in samples of bipolar children—ranging to 80 % [38]; this high comorbidity induced some authors [108] to suggest that ADHD may represent a phenotypic manifestation of early-onset BD.
Also, psychosis occurs in 16 % of BD cases and is usually a marker of severity and poorer prognosis [105]; some studies analyzed bipolar subjects with psychotic features, so that the findings may not be generalized to BD as a whole.
Importantly, interpretation of WM abnormalities explored with DTI and anatomical measurement are not straightforward. Voxelwise analysis is subject to type I errors, whereas the spatial resolution of the studies using DTI acquisition may be excessively low.
As suggested by Frazier et al. [38], most DTI studies suffer from low sensitivity and could be quite sensitive only to FA differences in subsections of the most densely packed fibers.
The observation of lower FA measurement in specific brain areas could be erroneously interpreted as lower connectivity [42], leading to imprecise anatomical measurement of WM. Recent advancements in this field using meta-analytic and multimodal neuroimaging approaches should help to clarify how FA differences may reflect connectivity dysfunctions. Moreover, processing pipelines of DTI data are diverse and no clear consensus exists on how to handle DTI data.
Although ROI studies provide relevant information on regional differences, they should be similarly considered cautiously, especially in the identification of more global changes in the brain. Reliable tractography studies are also missing.
Considering that the main findings derived by the included studies are highly heterogeneous, it has not been possible to analyze some relevant issues (e.g., differences in the instruments/criteria used to diagnose BD in children; BD subtypes and bipolar polarity; duration of the illness; childhood versus adolescent onset; effects of psychoactive medications; eventual comorbidity; family history of BD; socio-demographic factors; sample size; different scans; methods to evaluate the used scans and statistics) that could have influenced the main results of the present review. All these issues may explain, at least partially, the large disparity and disorganization of the main results.
Finally, most of the correlations that were reported should be interpreted as exploratory (see Tables), since no correction for multiple comparisons has been performed or because post hoc behavioral analyses included only a subset of the entire samples. Future neuroimaging studies should be useful in elucidating pathophysiological processes underlying the differential development of BD from UD supporting to clarify the relationship between structural and functional neuroimaging findings. They will require large multicentric samples.
Implications and future directions
Overall, based on the limited studies available, more WM abnormalities have been reported in BD children/adolescents than in those with UD suggesting the possible existence of vulnerability markers for BD. More studies about WM abnormalities in youths with UD are necessary.
Future longitudinal studies should: (1) directly compare groups of children with UD and BD; (2) use multimodal imaging for cross-validation of the results and easier interpretation; and (3) combine follow-up imaging assessments to investigate whether neurodevelopmental changes may be considered specifically related to diagnostic categories. In addition, future studies should focus on dimensional approaches able to redefine “bipolarity” in terms of underlying pathophysiological processes in genetically and symptomatically at risk subjects. These studies should also be conducted using more reliable neuroimaging techniques such as tractography to provide biomarkers as well as biological targets for more selective personalized treatments. Longitudinal follow-up studies should also allow identifying differential developmental trajectories between bipolar and unipolar subjects. Finally, the combination of different neuroimaging techniques and the development of novel algorithms based on machine learning, a branch of artificial intelligence, should warrant a more detailed understanding of neural circuitry abnormalities underlying major affective disorders [109].
References
Washburn JJ, West AE, Heil JA (2011) Treatment of pediatric bipolar disorder: a review. Minerva Psichiatr 52:21–35
Faedda GL, Baldessarini RJ, Suppes T, Tondo L, Becker I, Lipschitz DS (1995) Pediatric-onset bipolar disorder: a neglected clinical and public health problem. Harv Rev Psychiatry 3:171–195
Van Meter AR, Moreira AL, Youngstrom EA (2011) Meta-analysis of epidemiologic studies of pediatric bipolar disorder. J Clin Psychiatry 72:1250–1256
Geoffroy PA, Etain B, Scott J, Henry C, Jamain S, Leboyer M, Bellivier F (2013) Reconsideration of bipolar disorder as a developmental disorder: importance of the time of onset. J Physiol Paris 107:278–285
Lewinsohn PM, Klein DN, Seeley JR (1995) Bipolar disorders in a community sample of older adolescents: prevalence, phenomenology, comorbidity, and course. J Am Acad Child Adolesc Psychiatry 34:454–463
Lewinsohn PM, Klein DN, Seeley JR (2000) Bipolar disorder during adolescence and young adulthood in a community sample. Bipolar Disord 2:281–293
[No authors listed] (2001) National Institute of Mental Health Research roundtable on prepubertal bipolar disorder. J Am Acad Child Adolesc Psychiatry 40:871–878
Williams SB, O’Connor EA, Eder M, Whitlock EP (2009) Screening for child and adolescent depression in primary care settings: a systematic evidence review for the US Preventive Services Task Force. Pediatrics 123:e716–e735
Pine DS, Cohen P, Gurley D, Brook J, Ma Y (1998) The risk for early-adulthood anxiety and depressive disorders in adolescents with anxiety and depressive disorders. Arch Gen Psychiatry 55:56–64
Pompili M, Rihmer Z, Akiskal H, Amore M, Gonda X, Innamorati M, Lester D, Perugi G, Serafini G, Telesforo L, Tatarelli R, Girardi P (2012) Temperaments mediate suicide risk and psychopathology among patients with bipolar disorders. Compr Psychiatry 53:280–285
Serafini G, Pompili M, Innamorati M, Dwivedi Y, Brahmachari G, Girardi P (2013) Pharmacological properties of glutamatergic drugs targeting NMDA receptors and their application in major depression. Curr Pharm Des 19:1898–1922
Serafini G, Pompili M, Innamorati M, Giordano G, Montebovi F, Sher L, Dwivedi Y, Girardi P (2012) The role of microRNAs in synaptic plasticity, major affective disorders and suicidal behavior. Neurosci Res 73:179–190
Goldstein BI, Bukstein OG (2010) Comorbid substance use disorders among youth with bipolar disorder: opportunities for early identification and prevention. J Clin Psychiatry 71:348–358
Yoon YH, Chen CM, Yi HY, Moss HB (2011) Effect of comorbid alcohol and drug use disorders on premature death among unipolar and bipolar disorder decedents in the United States, 1999 to 2006. Compr Psychiatry 52:453–464
Mitsunaga MM, Garrett A, Howe M, Karchemskiy A, Reiss A, Chang K (2011) Increased subgenual cingulate cortex volume in pediatric bipolar disorder associated with mood stabilizer exposure. J Child Adolesc Psychopharmacol 21:149–155
Mahon K, Burdick KE, Szeszko PR (2010) A role for white matter abnormalities in the pathophysiology of bipolar disorder. Neurosci Biobehav Rev 34:533–554
Biederman J, Makris N, Valera EM, Monuteaux MC, Goldstein JM, Buka S, Boriel DL, Bandyopadhyay S, Kennedy DN, Caviness VS, Bush G, Aleardi M, Hammerness P, Faraone SV, Seidman LJ (2008) Towards further understanding of the co-morbidity between attention deficit hyperactivity disorder and bipolar disorder: a MRI study of brain volumes. Psychol Med 38:1045–1056
Adleman NE, Barnea-Goraly N, Chang KD (2004) Review of magnetic resonance imaging and spectroscopy studies in children with bipolar disorder. Exp Rev Neurother 4:69–77
Frazier JA, Ahn MS, DeJong S, Bent EK, Breeze JL, Giuliano AJ (2005) Magnetic resonance imaging studies in early-onset bipolar disorder: a critical review. Harv Rev Psychiatry 13:125–140
Fusar-Poli P, Howes O, Bechdolf A, Borgwardt S (2012) Mapping vulnerability to bipolar disorder: a systematic review and meta-analysis of neuroimaging studies. J Psychiatry Neurosci 37:170–184
Chantiluke K, Halari R, Simic M, Pariante CM, Papadopoulos A, Giampietro V, Rubia K (2012) Fronto-striato-cerebellar dysregulation in adolescents with depression during motivated attention. Biol Psychiatry 71:59–67
Halari R, Simic M, Pariante CM, Papadopoulos A, Cleare A, Brammer M, Fombonne E, Rubia K (2009) Reduced activation in lateral prefrontal cortex and anterior cingulate during attention and cognitive control functions in medication-naïve adolescents with depression compared to controls. J Child Psychol Psychiatry 50:307–316
Chen HH, Rosenberg DR, MacMaster FP, Easter PC, Caetano SC, Nicoletti M, Hatch JP, Nery FG, Soares JC (2008) Orbitofrontal cortex volumes in medication naïve children with major depressive disorder: a magnetic resonance imaging study. J Child Adolesc Psychopharmacol 18:551–556
Matsuo K, Rosenberg DR, Easter PC, MacMaster FP, Chen HH, Nicoletti M, Caetano SC, Hatch JP, Soares JC (2008) Striatal volume abnormalities in treatment-naïve patients diagnosed with pediatric major depressive disorder. J Child Adolesc Psychopharmacol 18:121–131
Caetano SC, Fonseca M, Hatch JP, Olvera RL, Nicoletti M, Hunter K, Lafer B, Pliszka SR, Soares JC (2007) Medial temporal lobe abnormalities in pediatric unipolar depression. Neurosci Lett 427:142–147
Rosso IM, Cintron CM, Steingard RJ, Renshaw PF, Young AD, Yurgelun-Todd DA (2005) Amygdala and hippocampus volumes in pediatric major depression. Biol Psychiatry 57:21–26
Nolan CL, Moore GJ, Madden R, Farchione T, Bartoi M, Lorch E, Stewart CM, Rosenberg DR (2002) Prefrontal cortical volume in childhood-onset major depression: preliminary findings. Arch Gen Psychiatry 59:173–179
Adler CM, DelBello MP, Strakowski SM (2006a) Brain network dysfunction in bipolar disorder. CNS Spectr 11:312–320, quiz 323–324
Arnone D, Cavanagh J, Gerber D, Lawrie SM, Ebmeier KP, McIntosh AM (2009) Magnetic resonance imaging studies in bipolar disorder and schizophrenia: meta-analysis. Br J Psychiatry 195:194–201
Singh MK, Chang KD, Chen MC, Kelley RG, Garrett A, Mitsunaga MM, Bararpour L, Howe M, Reiss AL, Gotlib IH (2012) Volumetric reductions in the subgenual anterior cingulate cortex in adolescents with bipolar I disorder. Bipolar Disord 14:585–596
Cheng YQ, Xu J, Chai P, Li HJ, Luo CR, Yang T, Li L, Shan BC, Xu XF, Xu L (2010) Brain volume alteration and the correlations with the clinical characteristics in drug-naïve first-episode MDD patients: a voxel-based morphometry study. Neurosci Lett 480:30–34
Foland-Ross LC, Brooks JO 3rd, Mintz J, Bartzokis G, Townsend J, Thompson PM, Altshuler LL (2012) Mood-state effects on amygdala volume in bipolar disorder. J Affect Disord 139:298–301
Lu LH, Zhou XJ, Fitzgerald J, Keedy SK, Reilly JL, Passarotti AM, Sweeney JA, Pavuluri M (2012) Microstructural abnormalities of white matter differentiate pediatric and adult-onset bipolar disorder. Bipol Disord 14:597–606
Najt P, Nicoletti M, Chen HH, Hatch JP, Caetano SC, Sassi RB, Axelson D, Brambilla P, Keshavan MS, Ryan ND, Birmaher B, Soares JC (2007) Anatomical measurements of the orbitofrontal cortex in child and adolescent patients with bipolar disorder. Neurosci Lett 413:183–186
Gao W, Jiao Q, Qi R, Zhong Y, Lu D, Xiao Q, Lu S, Xu C, Zhang Y, Liu X, Yang F, Lu G, Su L (2013) Combined analyses of gray matter voxel-based morphometry and white matter tract-based spatial statistics in pediatric bipolar mania. J Affect Disord 150:70–76
Pavuluri MN, Yang S, Kamineni K, Passarotti AM, Srinivasan G, Harral EM, Sweeney JA, Zhou XJ (2009) Diffusion tensor imaging study of white matter fiber tracts in pediatric bipolar disorder and attention-deficit/hyperactivity disorder. Biol Psychiatry 65:586–593
Adler CM, Adams J, DelBello MP, Holland SK, Schmithorst V, Levine A, Jarvis K, Strakowski SM (2006) Evidence of white matter pathology in bipolar disorder adolescents experiencing their first episode of mania: a diffusion tensor imaging study. Am J Psychiatry 163:322–324
Frazier JA, Breeze JL, Papadimitriou G, Kennedy DN, Hodge SM, Moore CM, Howard JD, Rohan MP, Caviness VS, Makris N (2007) White matter abnormalities in children with and at risk for bipolar disorder. Bipolar Disord 9:799–809
Barnea-Goraly N, Chang KD, Karchemskiy A, Howe ME, Reiss AL (2009) Limbic and corpus callosum aberrations in adolescents with bipolar disorder: a tract-based spatial statistics analysis. Biol Psychiatry 66:238–244
Kafantaris V, Kingsley P, Ardekani B, Saito E, Lencz T, Lim K, Szeszko P (2009) Lower orbital frontal white matter integrity in adolescents with bipolar I disorder. J Am Acad Child Adolesc Psychiatry 48:79–86
Ma N, Li L, Shu N, Liu J, Gong G, He Z, Li Z, Tan L, Stone WS, Zhang Z, Xu L, Jiang T (2007) White matter abnormalities in first-episode, treatment-naive young adults with major depressive disorder. Am J Psychiatry 164:823–826
Cullen KR, Klimes-Dougan B, Muetzel R, Mueller BA, Camchong J, Houri A, Kurma S, Lim KO (2010) Altered white matter microstructure in adolescents with major depression: a preliminary study. J Am Acad Child Adolesc Psychiatry 49:173–183
Whalley HC, Sprooten E, Hackett S, Hall L, Blackwood DH, Glahn DC, Bastin M, Hall J, Lawrie SM, Sussmann JE, McIntosh AM (2013) Polygenic risk and white matter integrity in individuals at high risk of mood disorder. Biol Psychiatry 74:280–286
Sprooten E, Sussmann JE, Clugston A, Peel A, McKirdy J, Moorhead TW, Anderson S, Shand AJ, Giles S, Bastin ME, Hall J, Johnstone EC, Lawrie SM, McIntosh AM (2011) White matter integrity in individuals at high genetic risk of bipolar disorder. Biol Psychiatry 70:350–356
Linke J, King AV, Poupon C, Hennerici MG, Gass A, Wessa M (2013) Impaired anatomical connectivity and related executive functions: differentiating vulnerability and disease marker in bipolar disorder. Biol Psychiatry 74:908–916
Cardoso de Almeida JR, Phillips ML (2013) Distinguishing between unipolar depression and bipolar depression: current and future clinical and neuroimaging perspectives. Biol Psychiatry 73:111–118
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339:b2535
Lu LH, Zhou XJ, Keedy SK, Reilly JL, Sweeney JA (2011) White matter microstructure in untreated first episode bipolar disorder with psychosis: comparison with schizophrenia. Bipol Disord 13:604–613
Saxena K, Tamm L, Walley A, Simmons A, Rollins N, Chia J, Soares JC, Emslie GJ, Fan X, Huang H (2012) A preliminary investigation of corpus callosum and anterior commissure aberrations in aggressive youth with bipolar disorders. J Child Adolesc Psychopharmacol 22:112–119
James A, Hough M, James S, Winmill L, Burge L, Nijhawan S, Matthews PM, Zarei M (2011) Greater white and grey matter changes associated with early cannabis use in adolescent-onset schizophrenia (AOS). Schizophr Res 128:91–97
Gönenç A, Frazier JA, Crowley DJ, Moore CM (2010) Combined diffusion tensor imaging and transverse relaxometry in early-onset bipolar disorder. J Am Acad Child Adolesc Psychiatry 49:1260–1268
Shad MU, Muddasani S, Rao U (2012) Gray matter differences between healthy and depressed adolescents: a voxel-based morphometry study. J Child Adolesc Psychopharmacol 22:190–197
Frodl T, Reinhold E, Koutsouleris N, Donohoe G, Bondy B, Reiser M, Möller HJ, Meisenzahl EM (2010) Childhood stress, serotonin transporter gene and brain structures in major depression. Neuropsychopharmacology 35:1383–1390
Adleman NE, Fromm SJ, Razdan V, Kayser R, Dickstein DP, Brotman MA, Pine DS, Leibenluft E (2012) Cross-sectional and longitudinal abnormalities in brain structure in children with severe mood dysregulation or bipolar disorder. J Child Psychol Psychiatry 53:1149–1156
Hajek T, Cullis J, Novak T, Kopecek M, Blagdon R, Propper L, Stopkova P, Duffy A, Hoschl C, Uher R, Paus T, Young LT, Alda M (2013) Brain structural signature of familial predisposition for bipolar disorder: replicable evidence for involvement of the right inferior frontal gyrus. Biol Psychiatry 73:144–152
Jarvis K, DelBello MP, Mills N, Elman I, Strakowski SM, Adler CM (2008) Neuroanatomic comparison of bipolar adolescents with and without cannabis use disorders. J Child Adolesc Psychopharmacol 18:557–563
Dickstein DP, Milham MP, Nugent AC, Drevets WC, Charney DS, Pine DS, Leibenluft E (2005) Frontotemporal alterations in pediatric bipolar disorder: results of a voxel-based morphometry study. Arch Gen Psychiatry 62:734–741
Wilke M, Kowatch RA, DelBello MP, Mills NP, Holland SK (2004) Voxel-based morphometry in adolescents with bipolar disorder: first results. Psychiatry Res 131:57–69
Alexander DC, Hubbard PL, Hall MG, Moore EA, Ptito M, Parker GJ, Dyrby TB (2010) Orientationally invariant indices of axon diameter and density from diffusion MRI. Neuroimage 52:1374–1389
Kempton MJ, Salvador Z, Munafò MR, Geddes JR, Simmons A, Frangou S, Williams SC (2011) Structural neuroimaging studies in major depressive disorder. Meta-analysis and comparison with bipolar disorder. Arch Gen Psychiatry 68:675–690
Caetano SC, Olvera RL, Glahn D, Fonseca M, Pliszka S, Soares JC (2005) Fronto-limbic brain abnormalities in juvenile onset bipolar disorder. Biol Psychiatry 58:525–531
Blumberg HP, Kaufman J, Martin A, Charney DS, Krystal JH, Peterson BS (2004) Significance of adolescent neurodevelopment for the neural circuitry of bipolar disorder. Ann N Y Acad Sci 1021:376–383
Strakowski SM, Delbello MP, Adler CM (2005) The functional neuroanatomy of bipolar disorder: a review of neuroimaging findings. Mol Psychiatry 10:105–116
Chang K, Adleman NE, Dienes K, Simeonova DI, Menon V, Reiss A (2004) Anomalous prefrontal-subcortical activation in familial pediatric bipolar disorder: a functional magnetic resonance imaging investigation. Arch Gen Psychiatry 61:781–792
Yurgelun-Todd DA, Gruber SA, Kanayama G, Killgore WD, Baird AA, Young AD (2000) fMRI during affect discrimination in bipolar affective disorder. Bipol Disord 2:237–248
Plas J, Brion F, Jeanneau A, Chevalier JF, Dussaux P, Brion S (1999) Contradictions in an original case. Contradictory psychiatric behavior after traumatic injury of the anterior part of the corpus callosum. Rev Neurol (Paris) 155:569–574
Paul LK, Lautzenhiser A, Brown WS, Hart A, Neumann D, Spezio M, Adolphs R (2006) Emotional arousal in agenesis of the corpus callosum. Int J Psychophysiol 61:47–56
Tamietto M, Adenzato M, Geminiani G, de Gelder B (2007) Fast recognition of social emotions takes the whole brain: interhemispheric cooperation in the absence of cerebral asymmetry. Neuropsychologia 45:836–843
Gazzaniga MS (2000) Cerebral specialization and interhemispheric communication: does the corpus callosum enable the human condition? Brain 123:1293–1326
Giedd JN, Rumsey JM, Castellanos FX, Rajapakse JC, Kaysen D, Vaituzis AC, Vauss YC, Hamburger SD, Rapoport JL (1996) A quantitative MRI study of the corpus callosum in children and adolescents. Brain Res Dev Brain Res 91:274–280
Giedd JN, Blumenthal J, Jeffries NO, Rajapakse JC, Vaituzis AC, Liu H, Berry YC, Tobin M, Nelson J, Castellanos FX (1999) Development of the human corpus callosum during childhood and adolescence: a longitudinal MRI study. Prog Neuropsychopharmacol Biol Psychiatry 23:571–588
Keshavan MS, Diwadkar VA, DeBellis M, Dick E, Kotwal R, Rosenberg DR, Sweeney JA, Minshew N, Pettegrew JW (2002) Development of the corpus callosum in childhood, adolescence and early adulthood. Life Sci 70:1909–1922
Chepuri NB, Yen YF, Burdette JH, Li H, Moody DM, Maldjian JA (2002) Diffusion anisotropy in the corpus callosum. AJNRAmJ Neuroradiol 23:803–808
Barnea-Goraly N, Menon V, Eckert M, Tamm L, Bammer R, Karchemskiy A, Dant CC, Reiss AL (2005) White matter development during childhood and adolescence: A cross sectional diffusion tensor imaging study. Cereb Cortex 15:1848–1854
Caetano SC, Silveira CM, Kaur S, Nicoletti M, Hatch JP, Brambilla P, Sassi R, Axelson D, Keshavan MS, Ryan ND, Birmaher B, Soares JC (2008) Abnormal corpus callosum myelination in pediatric bipolar patients. J Affect Disord 108:297–301
Yasar AS, Monkul ES, Sassi RB, Axelson D, Brambilla P, Nicoletti MA, Hatch JP, Keshavan M, Ryan N, Birmaher B, Soares JC (2006) MRI study of corpus callosum in children and adolescents with bipolar disorder. Psychiatry Res 146:83–85
Yurgelun-Todd DA, Silveri MM, Gruber SA, Rohan ML, Pimentel PJ (2007) White matter abnormalities observed in bipolar disorder: a diffusion tensor imaging study. Bipolar Disord 9:504–512
Phillips ML, Ladouceur CD, Drevets WC (2008) A neural model of voluntary and automatic emotion regulation: implications for understanding the pathophysiology and neurodevelopment of bipolar disorder. Mol Psychiatry 13:833–857
Lin F, Weng S, Xie B, Wu G, Lei H (2011) Abnormal frontal cortex white matter connections in bipolar disorder: a DTI tractography study. J Affect Disord 131:299–306
Merriam EP, Thase ME, Haas GL, Keshavan MS, Sweeney JA (1999) Prefrontal Cortical Dysfunction in Depression Determined by Wisconsin Card Sorting Test Performance. Am J Psychiatry 156:780–782
Drevets WC, Price JL, Furey ML (2008) Brain structural and functional abnormalities in mood disorders: Implications for neurocircuitry models of depression. Brain Struct Funct 213:93–118
Steele JD, Currie J, Lawrie SM, Reid I (2007) Prefrontal cortical functional abnormality in major depressive disorder: a stereotactic metaanalysis. J Affect Disord 101:1–11
Peng J, Liu J, Nie B, Li Y, Shan B, Wang G, Li K (2011) Cerebral and cerebellar gray matter reduction in first-episode patients with major depressive disorder: a voxel-based morphometry study. Eur J Radiol 80:395–399
Zou K, Deng W, Li T, Zhang B, Jiang L, Huang C, Sun X, Sun X (2010) Changes of brain morphometry in first-episode, drug-naϊve, non-late-life adult patients with major depression: An optimized voxel-based morphometry study. Biol Psychiatry 67:186–188
Ridderinkhof KR, Ullsperger M, Crone EA, Nieuwenhuis S (2004) The role of the medial frontal cortex in cognitive control. Science 306:443–447
Johansen-Berg H, Gutman DA, Behrens TE, Matthews PM, Rushworth MF, Katz E, Lozano AM, Mayberg HS (2008) Anatomical connectivity of the subgenual cingulate region targeted with deep brain stimulation for treatment-resistant depression. Cereb Cortex 18:1374–1383
Mayberg HS, Lozano AM, Voon V, McNeely HE, Seminowicz D, Hamani C, Schwalb JM, Kennedy SH (2005) Deep brain stimulation for treatment-resistant depression. Neuron 45:651–660
Drevets WC, Bogers W, Raichle ME (2002) Functional anatomical correlates of antidepressant drug treatment assessed using PET measures of regional glucose metabolism. Eur Neuropsychopharmacol 12:527–544
Drevets WC (1999) Prefrontal cortical-amygdalar metabolism in major depression. Ann N Y Acad Sci 877:614–637
Bremner JD, Randall P, Vermetten E, Staib L, Bronen RA, Mazure C, Capelli S, McCarthy G, Innis RB, Charney DS (1997) Magnetic resonance imaging-based measurement of hippocampal volume in posttraumatic stress disorder related to childhood physical and sexual abuse—A preliminary report. Biol Psychiatry 41:23–32
Stein MB, Koverola C, Hanna C, Torchia MG, McClarty B (1997) Hippocampal volume in women victimized by childhood sexual abuse. Psychol Med 27:951–959
Vythilingam M, Heim C, Newport J, Miller AH, Anderson E, Bronen R, Brummer M, Staib L, Vermetten E, Charney DS, Nemeroff CB, Bremner JD (2002) Childhood trauma associated with smaller hippocampal volume in women with major depression. Am J Psychiatry 159:2072–2080
Janssen J, Diaz-Caneja A, Reig S, Bombín I, Mayoral M, Parellada M, Graell M, Moreno D, Zabala A, Vazquez VG, Desco M, Arango C (2009) Brain morphology and neurological soft signs in adolescents with first-episode psychosis. Br J Psychiatry 195:227–233
Janssen J, Reig S, Parellada M, Moreno D, Graell M, Fraguas D, Zabala A, Garcia Vazquez V, Desco M, Arango C (2008) Regional gray matter volume deficits in adolescents with first-episode psychosis. J Am Acad Child Adolesc Psychiatry 47:1311–1320
White T, Ho BC, Ward J, O’Leary D, Andreasen NC (2006) Neuropsychological performance in first-episode adolescents with schizophrenia: a comparison with first-episode adults and adolescent control subjects. Biol Psychiatry 60:463–471
Douaud G, Smith S, Jenkinson M, Behrens T, Johansen-Berg H, Vickers J, James S, Voets N, Watkins K, Matthews PM, James A (2007) Anatomically related grey and white matter abnormalities in adolescent onset schizophrenia. Brain 130:2375–2386
Hatton SN, Lagopoulos J, Hermens DF, Naismith SL, Bennett MR, Hickie IB (2012) Correlating anterior insula gray matter volume changes in young people with clinical and neurocognitive outcomes: an MRI study. BMC Psychiatry 12:4
Buchy L, Luck D, Czechowska Y, Malla A, Joober R, Lepage M (2012) Diffusion tensor imaging tractography of the fornix and belief confidence in first-episode psychosis. Schizophr Res 137:80–84
de Azevedo-Marques Périco C, Duran FL, Zanetti MV, Santos LC, Murray RM, Scazufca M, Menezes PR, Busatto GF, Schaufelberger MS (2011) A population-based morphometric MRI study in patients with first-episode psychotic bipolar disorder: comparison with geographically matched healthy controls and major depressive disorder subjects. Bipolar Disord 13:28–40
Scherk H, Kemmer C, Usher J, Reith W, Falkai P, Gruber O (2008) No change to grey and white matter volumes in bipolar I disorder patients. Eur Arch Psychiatry Clin Neurosci 258:345–349
Zanetti MV, Schaufelberger MS, de Castro CC, Menezes PR, Scazufca M, McGuire PK, Murray RM, Busatto GF (2008) White-matter hyperintensities in first-episode psychosis. Br J Psychiatry 193:25–30
Craddock N, Owen MJ (2010) The Kraepelinian dichotomy– going, going… but still not gone. Br J Psychiatry 196:92–95
Schaffer A, Cairney J, Veldhuizen S, Kurdyak P, Cheung A, Levitt A (2010) A population-based analysis of distinguishers of bipolar disorder from major depressive disorder. J Affect Disord 125:350–354
Strakowski SM, Tsai SY, Delbello MP, Chen CC, Fleck DE, Adler CM, Arndt S, Amicone J (2007) Outcome following a first manic episode: cross-national US and Taiwan comparison. Bipolar Disord 9:820–827
Birmaher B, Axelson D, Strober M, Gill MK, Yang M, Ryan N, Goldstein B, Hunt J, Esposito-Smythers C, Iyengar S, Goldstein T, Chiapetta L, Keller M, Leonard H (2009) Comparison of manic and depressive symptoms between children and adolescents with bipolar spectrum disorders. Bipol Disord 11:52–62
Cousins DA, Aribisala B, Nicol Ferrier I, Blamire AM (2013) Lithium, gray matter, and magnetic resonance imaging signal. Biol Psychiatry 73:652–657
Hafeman DM, Chang KD, Garrett AS, Sanders EM, Phillips ML (2012) Effects of medication on neuroimaging findings in bipolar disorder: an updated review. Bipolar Disord 14:375–410
Singh MK, DelBello MP, Kowatch RA, Strakowski SM (2006) Co-occurrence of bipolar and attention-deficit hyperactivity disorders in children. Bipol Disord 8:710–720
Phillips ML, Swartz HA (2014) A critical appraisal of neuroimaging studies of bipolar disorder: toward a new conceptualization of underlying neural circuitry and a road map for future research. Am J Psychiatry 171:829–843
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Serafini, G., Pompili, M., Borgwardt, S. et al. Brain changes in early-onset bipolar and unipolar depressive disorders: a systematic review in children and adolescents. Eur Child Adolesc Psychiatry 23, 1023–1041 (2014). https://doi.org/10.1007/s00787-014-0614-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-014-0614-z