Abstract
Our objective was to describe the use of selective serotonin reuptake inhibitors (SSRIs) in the entire Danish population of children and adolescents from 1995 to 2011. Data on filled SSRIs were obtained for all children in Denmark aged 5–17 during 1995–2011. The amount and type of SSRIs filled were calculated as well as incidence rates and prevalence proportions. Furthermore, we looked at concurrent use of other psychotropic drug treatment duration. A total of 23,547 children aged 5–17 used SSRIs during the study period, most commonly sertraline followed by citalopram. Overall, the incidence rate increased from 0.57 per 1,000 person years in 1997 to 3.30 in 2010 and fell to 2.55 in 2011, while the prevalence proportion rose from 0.1 per 1,000 children at the end of 1995 to 3.3 at the end of 2011. However, these findings were driven entirely by an increase among adolescents (12–17 years), where the prevalence proportion rose from 0.11 and 0.36 to 4.64 and 8.52 per 1,000 boys and girls, respectively. A significant proportion of SSRI users used other psychotropic drugs concurrently, most notably antipsychotics (12–28 %) and psychostimulants (10–33 %). About 50 % of adolescents and 40 % of children discontinued treatment within 12 months of initiation. We found a marked increase in the use of SSRI drugs among adolescents in Denmark between 1995 and 2011. Whether this increase reflects a true increase in disorder occurrence, an increase in diagnostic intensity or more aggressive treatment remains uncertain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The use of selective serotonin reuptake inhibitors (SSRIs) in children has been subject to debate and controversy. Issues on efficacy and adverse reactions, especially reported cases of suicide-related behavior [1, 2], have in the past decade sparked warnings and guidelines from several regulatory authorities [3, 4]. Among the currently marketed SSRIs in Denmark, only fluoxetine holds an indication for major depression in children, while sertraline and fluvoxamine are indicated in cases of obsessive–compulsive disorder in children [5].
The current knowledge on SSRI drug utilization in children is fragmentary. There are very little adequate data for entire populations, and data on crucial drug utilization parameters such as regional differences, time-trends, co-medication or duration of therapy are virtually absent. The Danish Ministry of Health and Prevention reported cross-sectional data on the utilization of SSRIs among children and adolescents in 2010 [6], identifying 2,802 new users of SSRIs below the age of 18 from among a total of 5,677 users in that year.
Using the powerful and validated nationwide Danish prescription database [7–9], we aimed at providing a detailed study of prescription patterns of SSRIs among the entire pediatric population in Denmark in 1995–2011.
Methods
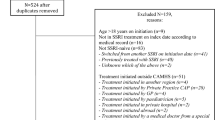
In this study, we described the use of SSRIs among children in Denmark, using descriptive statistics. We obtained prescription data for all children in Denmark aged 5–17 years during the period January 1, 1995 to December 31, 2011. On average, 838,000 children of this age resided in Denmark during the study years. We excluded children <5 years old as a preliminary analysis based on publicly available prescription data [10], showed negligible use of SSRIs in this age group.
Data source
National data on drug use in Denmark was extracted from the Danish National Prescription Database [8]. The registry contains complete information, from 1 January 1995 and onwards, on all prescriptions filled by Danish residents at outpatient pharmacies. For each filled prescription, the registry contains information on the following variables relevant for this study: drug type, quantity, date of purchase, person age, gender and region of residence. Registered drugs are categorized according to the Anatomic Therapeutic Chemical (ATC) index, a hierarchical classification system developed by the World Health Organization (WHO) for purposes of drug use statistics, and the quantity dispensed for each prescription is expressed by the defined daily dose (DDD) measure, also developed by the WHO [11]. In addition, the registry contains several other variables not used in this study. As described elsewhere, the registry is reported to have a high completeness and validity [8]. Population statistics were obtained from Statistics Denmark, a governmental institution that collects and maintains electronic records for a broad spectrum of statistical and scientific purposes.
Study drugs
SSRIs were defined as all drugs within ATC-group N06AB (selective serotonin reuptake inhibitors). The pediatric indication, ATC code and DDD-definition for each SSRI marketed in Demark are shown in Table 1.
Analysis
To structure the description of the analysis and the presentation of the results, we divided the analysis into five research questions collectively describing the use of SSRIs among children in Denmark. All analyses were performed stratified by age and gender. We used age categories as defined by EMA [12], young children 2–11 years (while excluding those below 5 years of age) and adolescent 12–17 years.
To investigate which SSRIs were used, we calculated the total amount of dispensed DDDs, specified by type of SSRI and study year (1995–2011).
To estimate the incidence rate of SSRI use, we defined incident use as the children’s first filled prescription for an SSRI in the registry. As data were not available prior to 1995, only data from 1997 onwards are shown. Using 1995 and 1996 as a run in period ensured that we did not misclassify previous users as incident users. We calculated incidence rates by dividing the number of children who in a given year filled their first ever SSRI prescription by the total number of children within each age and gender category living in Denmark on January 1 of the relevant year. The incidence rate was given per 1,000 person years.
To estimate the point prevalence proportion of SSRI drug use, we defined the point prevalence of SSRI use as the number of children, who on any given day either filled an SSRI prescription or had previously filled a prescription with enough SSRI doses to cover that day. When deciding whether SSRI doses covered a given day, we assumed one dispensed tablet to be the daily dose and then added 25 % to the dispensed amount to account for non-compliance and irregular prescription refills. Point prevalence proportions were calculated by dividing the number of current SSRI users by the total number of children within each age and gender category living in Denmark on January 1 of the relevant year. We further illustrated the age distribution of SSRI use by estimating the point prevalence proportion of use for each age year (as of December 31, 2011) among boys and girls. As the point prevalence estimate was based on refill patterns of prescriptions that occurred during late 2011 and not on actual drug intake, this date simply represents extent of use by the end of 2011. Lastly, to investigate regional differences in the use of SSRIs, we estimated the prevalence proportion (as of December 31, 2011) in each of the five Danish regions (North, Mid, South, Zealand and Capitol) and compared it with the national average.
We assessed concurrent psychotropic drug (ATC-groups N05 and N06) use by calculating the percentage of prevalent SSRI users in 2011, who in the same year also filled a prescription for another psychotropic drug, aggregated at the third ATC-level (e.g., N06B, psychostimulants). We further calculated standardized morbidity ratios (SMRs), i.e., the ratio between concurrent psychotropic drug use in the SSRI cohort and the expected psychotropic drug use in these children if they had the same use pattern as the total background pediatric population, standardized by gender and age in 1-year intervals.
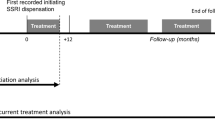
We produced a Kaplan–Meier curve to estimate the duration of SSRI drug use among children in Denmark. For each SSRI user, the duration of treatment was calculated from the day the first prescription was filled and until treatment was terminated. Treatment was defined as terminated when 180 days had passed since the individual had filled a prescription for any SSRI drug. The long interval allowed between prescriptions was chosen to avoid false termination of use among children who had long pauses between prescriptions. Children were excluded from this analysis if their first treatment episode was initiated in the first half of 1995 (i.e., the first 180 days of our dataset) to ensure that the correct start date was assigned. In this analysis, children were censored upon death or at the end of the study period (31 December 2011). Only the first treatment episode of each child was included in the survival analysis. When specifying by age category we used the age at the time of the first prescription. We further conducted a sensitivity analysis to test whether extending the interval allowed between SSRI prescription fills from 180 to 365 days would alter our results on treatment duration.
Other
All calculations were performed using STATA Release 12.0 (StataCorp, College Station, TX, USA). The study was approved by the Danish Data Protection Agency and Statistics Denmark’s Scientific Board. Approval from the Ethics Committee was not required according to Danish law.
Results
We identified 23,547 children aged 5–17 who used SSRIs during the study period (1995–2011), filling 170,356 prescriptions. The most commonly used SSRI substance over the entire period was sertraline (64,595 fillings), followed by citalopram (63,892 fillings), with sertraline being the dominant SSRI by the end of the study period (Fig. 1).
The overall incidence rate of SSRI use among children in Denmark increased from 0.57 per 1,000 person years in 1997 to its highest value 3.30 per 1,000 person years in 2010 and then fell slightly to 2.55 per 1,000 person years in 2011. Further analyses revealed that the increasing number of new users was confined to adolescent (12–17 years) children (Fig. 2a). Citalopram was the dominant first-line treatment throughout the study period, but since 2008 first-line treatment shifted towards sertraline and fluoxetine, especially at the expense of citalopram (data not shown).
The prevalence proportion of SSRI use among children in Denmark followed a similar pattern as the incidence rate (Fig. 2b). The overall prevalence proportion (5–17 years) rose from 0.1 per 1,000 children at the end of 1995 to 3.3 per 1,000 children at the end of 2011. Again, the increase was only observed among adolescents, with the most pronounced increase occurring among adolescent girls (Fig. 2b). Figure 3 shows the full age and gender spectrum of prevalent SSRI users in 2011. Until age 13, boys used SSRIs more commonly than girls, but thereafter the prevalence proportion ratio between genders was reversed. At age 14, girls were 1.3-fold more likely than boys to use SSRIs (5.0 per 1,000 girls vs. 3.8 per 1,000 boys) and at age 17, they were 2.4-fold more likely (20.1 per 1,000 girls vs. 8.4 per 1,000 boys).
We found only modest differences in prevalence proportions by region of residence, e.g., ranging from 3.98 to 6.13 per 1,000 children among boys aged 12–17 (in South and Zealand region, respectively) and 7.99–9.87 per 1,000 children among girls aged 12–17 (in North and Zealand region, respectively) (data not shown in full).
Psychostimulants and antipsychotics were the psychotropic drugs most frequently used concurrently with SSRIs among children in Denmark in 2011; 27–33 % of young (5–11 years) SSRI users received psychostimulants and 16–23 % of adolescent (12–17 years) SSRI users received antipsychotics in that same year (Table 2). The standardized morbidity ratios (SMR) in Table 2 show that SSRI users were many-fold more likely to use psychotropic drugs as compared with children of the background population of the same age.
Prevalence proportion (prevalence proportion is expressed as number of individuals per 1,000 in the population who on December 31, 2011 either filled an SSRI prescription or had previously filled a prescription with enough SSRI doses to cover that day) of SSRI use among children in Denmark in 2011 (December 31), according to age and gender
Our estimation of SSRI treatment duration, as depicted with a Kaplan–Meier plot (Fig. 4), shows that adolescents generally discontinued treatment earlier than younger children did. Almost 50 % of adolescents discontinued within 12 months of treatment, while over 60 % of young children (5–11 years) were still being treated with SSRIs at that time. At 24 months, over 35 % of the young users and approximately one-fourth of adolescents were still on SSRI drugs. Allowing 365 days between SSRI prescriptions, instead of 180 days, did not significantly alter these results.
Discussion
With this study we present to date the most comprehensive and largest longitudinal nationwide analysis of SSRI use among children and adolescents.
Our study has several important strengths. First, it is based on a comprehensive registering of drug use for a well-defined, unselected population [8]. There is no reason to suspect selection bias in our account. Second, all of the drugs included in our analysis are fully covered by the database. None of the drugs are available over the counter. Finally, there is very little loss to follow-up, and we are able to account for, e.g., migrations in or out of our population. The main limitation is that we do not have data on the indication for using SSRIs and the clinical information is fairly crude. A second limitation is that we do not have data on when the drugs are actually taken in relation to the timing of prescriptions. For example, we do not know whether the children cease their SSRI use shortly after their first prescriptions, unless a new prescription occurs. Finally, in this study we did not describe trends in use of other antidepressants, such as tricyclics. However, our data show that the use of tricyclic antidepressants was low and stable throughout the study period (approximately 200 children per year; data not shown) and would, as such, not have added much value to the study to include these into the analysis.
Use of specific SSRIs
The most frequently prescribed SSRIs to children in Denmark are currently (2011) sertraline, citalopram and fluoxetine. The choice of drugs and changes thereof has to some extent mirrored changes in marketing authorizations and regulatory recommendations. After receiving a pediatric marketing authorization in 2009, the share of sertraline prescriptions among all filled SSRI prescriptions in the pediatric population rose from 47 % (2008) to 58 % (2011). Similarly, once a pediatric indication was authorized for fluoxetine in 2006, its share of all filled SSRI prescriptions increased from 5 % (2005) to 14 % (2011). These changes were mostly at the cost of citalopram prescriptions, which were reduced from 45 % (2005) to 20 % (2011) of all filled SSRI prescriptions (Fig. 1).
Our results of the specific SSRI type used are also in line with a recent survey among specialists of all child and adolescent psychiatric outpatient departments and private psychiatric practices in Denmark [13]. When asked about medical treatment of obsessive–compulsive disorder (OCD), specialists named sertraline as the preferred first-line drug (63–81 %) and citalopram as the preferred second-line drug (47–53 %). Further, in 2008 the Danish Health and Medicines Authority issued guidelines for the prescription of SSRIs in children recommending fluoxetine as the first-line drug for depression and fluoxetine and sertraline for OCD [3]. Similarly, recent regulatory actions elsewhere, e.g., FDA “Black Box” warnings and the Paroxetine Public Health Warning, have resulted in altered prescription patterns of SSRIs in the United States and Canada [14–17], and may also be reflected in UK data [18, 19].
Incidence and prevalence of SSRI use
Compared with other Nordic, UK and North American data, the current incidence rates in Denmark are low-to-modest. In an Icelandic population-based study a slight decrease in prevalence proportion of SSRI use was found between the years 2003 and 2007, falling from 14.3 to 13.9 per 1,000 children (0–17 years). Incidence rates for SSRI use was not reported in that study, but the overall antidepressant incidence followed a statistically significant decreasing linear trend. About 42 % of all antidepressants used among Icelandic children in 2007 were off-label prescriptions with respect to age [20]. Finnish data from 1999–2005 demonstrated a stable incidence rate of SSRI use between 1.5 and 1.8 per 1,000, with a decreasing use of citalopram [21]. A nationwide Norwegian study of prescription patterns among 15–16-year-old adolescents revealed small increases in the prevalence proportion of SSRI use in 2006–2010, from 5.0 to 6.0 per 1,000 adolescent boys and 6.5–7.5 per 1,000 adolescent girls [22]. Further, data from the UK primary care database revealed a change in incidence rate from 3.2 per 1,000 person years in 2002 down to 1.7 in 2005 and up to 2.7 in 2007. This decrease in the UK may be a reflection of the Committee of Medicines (CSM) safety advice issued in 2003 against the use of SSRIs other than fluoxetine [19]. Subsequent changes in national treatment guidelines could also contribute to these observations in the UK, along with a declining rate of depression diagnoses, which may in some cases be due to GPs’ inclination to report symptoms rather than assign a full diagnosis following the warning [19].
Other recently reported European incidence rates of SSRI use are 3.7 and 4.0 per 1,000 person years in Germany and France, respectively [23–25]. There are no solid nationwide data from the United States on pediatric use of SSRIs, but the reported prevalence proportion, depending on geographical region and data source, appears to have been between 3 and 18 per 1,000 children in the past decade [16, 26–28]. The differences in the use of SSRIs in children between various countries may to some extent also reflect differences in the quality of available data sources and differences in methodological approaches.
In Denmark, the initiation of antidepressant treatment in children and adolescents has, since January 2008, exclusively been delegated to specialists in child- and adolescent psychiatry [3]. According to data on final diagnoses made by specialist departments and registered into the Danish Child and Adolescent Psychiatric Database (estimated national completeness about 80 %) [29], the incidence rate of affective and anxiety/obsessive compulsive disorders in children appears to have been relatively stable during 2005–2010. Incidence rates were 0.27 and 0.25 per 1,000 person years (0–17 years) in 2005, respectively, for affective and anxiety/obsessive disorders; and 0.25 and 0.23 per 1,000 person years in 2010 [29]. The Danish Health and Medicines Authority reported a slightly increasing prevalence proportion of these conditions in children in 2000, 2005 and 2010; 0.39, 0.77 and 1.18 per 1,000 children for affective disorders, and 1.13, 1.18, 2.03 per 1,000 children for anxiety/obsessive compulsive disorders [30]. As a comparison, the prevalence proportion of diagnosed attention-deficit hyperactivity (ADHD) and related disorders was 2.16, 3.66 and 8.10 per 1,000 children during these same years. The marked rise in use of SSRI drugs we found among adolescents in Denmark is, thus, unlikely to be fully explained by increasing incidence rates for diagnoses of affective or anxiety/obsessive compulsive disorders. We doubt that the substantial increase in sertraline use be primarily related to the authorized indication for this drug. We do, however, not have any reliable data on the incidence rates for OCD and major depression, the only conditions with licensed indications for SSRI use in children [5]. A substantial off-label use of antidepressants has been documented; in a recent US study, only 9.2 % of visits in ambulatory care settings prescribing antidepressants to children and adolescents were in accordance with FDA approved indications [31]. Additionally, an estimated 5 % of children and adolescents in Denmark with ADHD as a primary diagnosis are treated with SSRIs [32], which, given the high prevalence proportion of ADHD, could account for a large proportion of the SSRI users, and subsequently contribute to the increase in the use of SSRIs we found in the current study [32, 33]. Whether or not the observed increase in the use of SSRI’s reflects a true increase in disorder incidence/prevalence, an increase in diagnostic intensity, or a more aggressive treatment pattern remains uncertain and should be subject to future research.
Concurrent use of other psychotropic medications
Psychostimulants and antipsychotics were the psychotropic drugs most frequently used concurrently with SSRIs among children in Denmark in 2011. The standardized morbidity ratios we found demonstrate that SSRI users were several-fold more likely to use psychotropic drugs as compared with the background population of similar age. These data are in accordance with reported literature on frequencies of concurrent use of psychotropic drugs in children and adolescents [34]. Polypharmacy in affective disorders in children and adolescents has been reported with proportions between 16 and 45 % [35–38], with higher rates specifically reported for bipolar disorder [39, 40]. Concurrent use of antidepressants and antipsychotics was 16.7 % among patients with a diagnosis of bipolar disorder among 962 bipolar patients in the US National Ambulatory Medical Care Survey [40]. Concurrent use of psychostimulants and antidepressants appears to be very common with reported proportions between 5 and 33 % among pediatric patients in Denmark and the US [32, 41, 42]. Comorbidity between OCD/anxiety, affective disorders, ADHD and other psychiatric diagnoses are common, yet subject to controversy with respect to validity of the specific diagnoses implied [43–46].
Duration of SSRI therapy
Our data showed that about 50 % of adolescents discontinued SSRI use within 12 months of treatment, while over 60 % of younger children were still being treated at that time. At 24 months upon initiation of SSRI treatment, these proportions were about 35 and 25 %, respectively, while at 5 years, 15 % of children and 8 % adolescent users were still being treated with SSRIs. These differences are small to modest especially given the small number of children between 5 and 11 years of age included. There were no substantial differences in treatment duration with respect to gender. These observations may to some extent reflect differences in the threshold for initiation of SSRI therapy. Such a threshold may be higher in younger children, thus indirectly reflect a more solid treatment indication and/or severity of symptoms, which in turn may be associated with duration of therapy. More intense parental supervision and clinical follow-up, shown to be associated with better treatment adherence [47], could also explain the longer treatment durations we found for young children versus adolescents. However, as we do not have specific data on diagnoses, treatment effects or outcomes, these considerations remain speculative. Recent data on duration of SSRI therapy in children and adolescents are sparse. In a Finnish study covering data from 1999 to 2004, the median duration of SSRI therapy was 161 days (mean 267 days) for children and adolescents, with 79 % discontinuing treatment before day 400. In Finland young age was, likewise, associated with increased durations of SSRI treatment [21]. UK data for 1992–2001 demonstrated even shorter durations of SSRI treatment among children and adolescents, with a median of about 58 days and fewer than 10 % of users in treatment after 12 months [18].
Conclusion
We have demonstrated a marked increase in the incidence rate and prevalence proportion of SSRI drug use among adolescents in Denmark between 1995 and 2011. The reasons for increasing use are unclear, especially with respect to true occurrences of disorder versus increased awareness and diagnostic approaches and attitudes toward drug treatment. The distribution pattern between the specific SSRIs seems to some extent to reflect changes in SSRI labeling, as well as regulatory guidance and warnings on treatment decisions.
References
Gibbons RD, Brown CH, Hur K, Marcus SM, Bhaumik DK, Erkens JA et al (2007) Early evidence on the effects of regulators’ suicidality warnings on SSRI prescriptions and suicide in children and adolescents. Am J Psychiatry 164:1356–1363
Vitiello B, Swedo S (2004) Antidepressant medications in children. N Engl J Med 350:1489–1491
The Danish Ministry of Health and Prevention. (Guide to medicamental treatment of children and adolescents with psychiatric disorders, VEJ no 10332); Cited 11 Dec 2012. Available from www.retsinformation.dk/
European Medicines Agency (EMA). European Medicines Agency finalizes review of antidepressants in children and adolescents. EMEA/CHMP/128918/2005; Cited 11 Dec 2012. Available from: www.ema.europa.eu
Summary of Product Characteristics.; Cited 11 Dec 2012. Available from: www.produktresume.dk
Danish Medicines Agency. (Drugs against depression for children and adolescents); Cited 11/12/2012. Available from: www.laegemiddelstyrelsen.dk
Frank L (2000) Epidemiology. When an entire country is a cohort. Science 287:2398–2399
Kildemoes HW, Sorensen HT, Hallas J (2011) The Danish national prescription registry. Scand J Public Health 39:38–41
Thygesen LC, Ersboll AK (2011) Danish population-based registers for public health and health-related welfare research: introduction to the supplement. Scand J Public Health 39:8–10
National Institute for Health Data and Disease Control. Medstat.dk; Cited 4 April 2013. Available from: www.medstat.dk/en
WHO Collaborating Centre for Drug Statistics Methodology. Guidelines for ATC classification and DDD assignment 2013. 2012 Oslo
European Medicines Agency (EMA). ICH Topic E 11: Clinical Investigation of Medicinal Products in the Paediatric Population. Note for guidance on clinical investigation of medicinal products in the paediatric population (CPMP/ICH/2711/99). 2001
Nissen JB, Thomsen PH (2008) Clinicians’ views on clinical examination and treatment of children and adolescents with obsessive-compulsive disorder (OCD). A Danish national survey study. Nord J Psychiatry 62:309–314
Bhatia SK, Rezac AJ, Vitiello B, Sitorius MA, Buehler BA, Kratochvil CJ (2008) Antidepressant prescribing practices for the treatment of children and adolescents. J Child Adolesc Psychopharmacol 18:70–80
Katz LY, Kozyrskyj AL, Prior HJ, Enns MW, Cox BJ, Sareen J (2008) Effect of regulatory warnings on antidepressant prescription rates, use of health services and outcomes among children, adolescents and young adults. CMAJ 178:1005–1011
Pamer CA, Hammad TA, Wu YT, Kaplan S, Rochester G, Governale L et al (2010) Changes in US antidepressant and antipsychotic prescription patterns during a period of FDA actions. Pharmacoepidemiol Drug Saf 19:158–174
Valluri S, Zito JM, Safer DJ, Zuckerman IH, Mullins CD, Korelitz JJ (2010) Impact of the 2004 food and drug administration pediatric suicidality warning on antidepressant and psychotherapy treatment for new-onset depression. Med Care 48:947–954
Murray ML, de Vries CS, Wong IC (2004) A drug utilisation study of antidepressants in children and adolescents using the general practice research database. Arch Dis Child 89:1098–1102
Wijlaars LP, Nazareth I, Petersen I (2012) Trends in depression and antidepressant prescribing in children and adolescents: a cohort study in The Health Improvement Network (THIN). PLoS One 7:e33181
Zoega H, Baldursson G, Hrafnkelsson B, Almarsdottir AB, Valdimarsdottir U, Halldorsson M (2009) Psychotropic drug use among Icelandic children: a nationwide population-based study. J Child Adolesc Psychopharmacol 19:757–764
Saastamoinen LK, Wallin M, Lavikainen P, Airaksinen MS, Sourander A, Bell JS (2012) Treatment duration with selective serotonin reuptake inhibitors among children and adolescents in Finland: a nationwide register study. Eur J Clin Pharmacol 68:1109–1117
Steffenak AK, Wilde-Larsson B, Nordstrom G, Skurtveit S, Hartz I (2012) Increase in psychotropic drug use between 2006 and 2010 among adolescents in Norway: a nationwide prescription database study. Clin Epidemiol 4:225–231
Fegert JM, Kolch M, Zito JM, Glaeske G, Janhsen K (2006) Antidepressant use in children and adolescents in Germany. J Child Adolesc Psychopharmacol 16:197–206
Koelch M, Prestel A, Singer H, Keller F, Fegert JM, Schlack R et al (2009) Psychotropic medication in children and adolescents in Germany: prevalence, indications, and psychopathological patterns. J Child Adolesc Psychopharmacol 19:765–770
Sevilla-Dedieu C, Kovess-Masfety V (2008) Psychotropic medication use in children and adolescents: a study from France. J Child Adolesc Psychopharmacol 18:281–289
Merikangas KR, He JP, Rapoport J, Vitiello B, Olfson M (2013) Medication use in US youth with mental disorders. JAMA Pediatr 167:141–148
Vitiello B, Zuvekas SH, Norquist GS (2006) National estimates of antidepressant medication use among US children, 1997–2002. J Am Acad Child Adolesc Psychiatry 45:271–279
Zito JM, Tobi H, de Jong-van den Berg LT, Fegert JM, Safer DJ, Janhsen K et al (2006) Antidepressant prevalence for youths: a multi-national comparison. Pharmacoepidemiol Drug Saf 15:793–798
The Danish BupBase. (The Danish Database for Child and Adolescent Psychiatry 2005–2010 Annual Reports); Cited 5 March 2013. Available from: www.bupnet.dk
The Danish Health and Medicines Authority. (Development in Child and Adolescent Psychiatry Activity 2007–2010); Cited 12 March 2013. Available from: www.sst.dk
Lee E, Teschemaker AR, Johann-Liang R, Bazemore G, Yoon M, Shim KS et al (2012) Off-label prescribing patterns of antidepressants in children and adolescents. Pharmacoepidemiol Drug Saf 21:137–144
Pottegard A, Bjerregaard BK, Glintborg D, Kortegaard LS, Hallas J, Moreno SI (2013) The use of medication against attention deficit/hyperactivity disorder in Denmark: a drug use study from a patient perspective. Eur J Clin Pharmacol 69:589–598
Pottegard A, Bjerregaard BK, Glintborg D, Hallas J, Moreno SI (2012) The use of medication against attention deficit hyperactivity disorder in Denmark: a drug use study from a national perspective. Eur J Clin Pharmacol 68:1443–1450
Diaz-Caneja CM, Espliego A, Parellada M, Arango C, Moreno C (2012) Polypharmacy with antidepressants in children and adolescents. Int J Neuropsychopharmacol 1–20 [Epub ahead of print]
Comer JS, Olfson M, Mojtabai R (2010) National trends in child and adolescent psychotropic polypharmacy in office-based practice, 1996–2007. J Am Acad Child Adolesc Psychiatry 49:1001–1010
Dean AJ, McDermott BM, Marshall RT (2006) Psychotropic medication utilization in a child and adolescent mental health service. J Child Adolesc Psychopharmacol 16:273–285
McIntyre RS, Jerrell JM (2009) Polypharmacy in children and adolescents treated for major depressive disorder: a claims database study. J Clin Psychiatry 70:240–246
Schirm E, Tobi H, Zito JM, de Jong-van den Berg LT (2001) Psychotropic medication in children: a study from the Netherlands. Pediatrics 108:E25
Geller B, Tillman R, Bolhofner K, Zimerman B (2010) Pharmacological and non-drug treatment of child bipolar I disorder during prospective eight-year follow-up. Bipolar Disord 12:164–171
Moreno C, Laje G, Blanco C, Jiang H, Schmidt AB, Olfson M (2007) National trends in the outpatient diagnosis and treatment of bipolar disorder in youth. Arch Gen Psychiatry 64:1032–1039
Duffy FF, Narrow WE, Rae DS, West JC, Zarin DA, Rubio-Stipec M et al (2005) Concomitant pharmacotherapy among youths treated in routine psychiatric practice. J Child Adolesc Psychopharmacol 15:12–25
Hunkeler EM, Fireman B, Lee J, Diamond R, Hamilton J, He CX et al (2005) Trends in use of antidepressants, lithium, and anticonvulsants in Kaiser Permanente-insured youths, 1994–2003. J Child Adolesc Psychopharmacol 15:26–37
Daviss WB (2008) A review of co-morbid depression in pediatric ADHD: etiology, phenomenology, and treatment. J Child Adolesc Psychopharmacol 18:565–571
Esbjorn BH, Hoeyer M, Dyrborg J, Leth I, Kendall PC (2010) Prevalence and co-morbidity among anxiety disorders in a national cohort of psychiatrically referred children and adolescents. J Anxiety Disord 24:866–872
Kunwar A, Dewan M, Faraone SV (2007) Treating common psychiatric disorders associated with attention-deficit/hyperactivity disorder. Expert Opin Pharmacother 8:555–562
Masi G, Perugi G, Toni C, Millepiedi S, Mucci M, Bertini N et al (2006) Attention-deficit hyperactivity disorder: bipolar comorbidity in children and adolescents. Bipolar Disord 8:373–381
Fontanella CA, Bridge JA, Marcus SC, Campo JV (2011) Factors associated with antidepressant adherence for Medicaid-enrolled children and adolescents. Ann Pharmacother 45:898–909
Conflict of interest
JH has participated in research projects funded by Pfizer with grants paid to the institution where he was employed. He has personally received fees for consultation from the Danish Association of Pharmaceutical Manufacturers and from Lundbeck. PD is a paid consultant for Fertin Pharma, Denmark. AP and HZ report no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pottegård, A., Zoëga, H., Hallas, J. et al. Use of SSRIs among Danish children: a nationwide study. Eur Child Adolesc Psychiatry 23, 1211–1218 (2014). https://doi.org/10.1007/s00787-014-0523-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-014-0523-1