Abstract
Purpose
We assessed treatment duration with selective serotonin reuptake inhibitors (SSRIs) among children and adolescents and investigated the association between treatment duration, age, sex, active ingredient, season of initiation, and reimbursement rate.
Method
Data on reimbursed SSRIs dispensed to children and adolescents aged <18 years in noninstitutional settings in Finland from 1999 to 2005 were extracted from the National Prescription Register. The association between treatment duration and explanatory factors was analyzed using Cox proportional hazards models.
Results
SSRIs were reimbursed for 3,710 (35.8%) male and 6,666 female (64.2%) patients from 1999 to 2004, of whom 3,853 (37.1%) received ≤100 days’ supply. Age ≤11 years [adjusted hazard ratio (HR) 0.87; 95% confidence interval (CI), 0.80–0.94] and 12–15 years (HR 0.89; 95% CI 0.84–0.93) was associated with longer treatment duration compared with adolescents aged 16–17 years. Shorter treatment duration was associated with initiating treatment from September to November compared with the other seasons. Recipients of a higher reimbursement rate had longer treatment duration (HR 0.46, 95% CI 0.39–0.55) compared with those who received a lower reimbursement rate. Shorter treatment duration was weakly associated with use of fluvoxamine (HR 1.16; 95% CI 1.03–1.30) compared with fluoxetine.
Conclusions
Shorter treatment duration was less common among younger children, when initiated from September to November and among recipients of a higher reimbursement rate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The World Health Organization and European Medicines Agency have highlighted the importance of conducting research, including pharmacoepidemiological studies, specifically for children and adolescents [1, 2]. The safety and efficacy of psychotropic drug use among children and adolescents has attracted recent attention [3, 4]. Research into the role of pharmacotherapy in the treatment of child and adolescent depression has been identified as a particular priority. This is due to drug safety concerns and the possible association between untreated depression and impaired social skills, poor academic performance, and developmental disorders [5].
Selective serotonin reuptake inhibitors (SSRI) are the most widely used antidepressants among children and adolescents [6–8]. They are prescribed for indications of depressive disorders, anxiety, bulimia nervosa, obsessive compulsive disorder, panic disorder, posttraumatic stress disorder, and social phobias. However, few studies have assessed treatment duration with SSRIs among children and adolescents. In Ireland, 58% of children and adolescents aged <16 years were dispensed only one antidepressant prescription in 2003 [9]. In the UK, >60% of children and adolescents discontinued taking antidepressants within 2 months between 1992 and 2001 [10]. Older age, female gender, and tricyclic antidepressant (TCA) use were associated with early discontinuation. In younger children, TCAs are often used for indications other than depression, such as nocturnal enuresis. In a US Medicaid population, 51% of 5- to 17-year-olds used <80% of their prescribed antidepressants, with higher rates of adherence in the first 3 months being associated with younger age, non-Hispanic white ethnicity, use of other psychotropic drugs, optimal provider contact, and adequate antidepressant dose [11]. In Finland, 31% of children and adolescents aged <20 years who received a reimbursed SSRI from 1999 to 2005 received only one prescription [12]. Among people <26 years in Finland in 2007, 26% of males and 21% overall collected only one antidepressant prescription [6].
Treatment guidelines provide varying or minimal advice regarding optimum treatment duration with SSRIs among children and adolescents. However, United States, UK, and Finnish guidelines recommend that pharmacological treatment of adolescent depression should continue for 6–12 months [13–15]. This recommendation is supported by evidence from observational studies conducted among adults, suggesting patients who discontinue treatment early have higher rates of relapse or recurrence [16–18]. However, more recent studies conducted among adults have not reported an association between initial treatment duration and the time to a second treatment episode [19, 20]. Nevertheless, rapid discontinuation of antidepressants has been associated with earlier recurrence of depression and panic disorder [21].
Few studies have assessed factors associated with treatment duration with SSRIs among children and adolescents. This knowledge is important for clinicians, drug regulatory bodies, and policymakers alike. The objectives of this study were to assess treatment duration with SSRIs among all children and adolescents in Finland who initiated treatment between 1999 and 2004 and to investigate the association between treatment duration and age, sex, active ingredient, season of initiation, and reimbursement rate.
Materials and methods
Data sources
This was a national study using data from the Finnish National Prescription Register [22], which keeps records of all drugs reimbursed by the Social Insurance Institution of Finland (SII). All 5.3-million Finnish residents living in noninstitutional settings are covered by National Health Insurance, which includes reimbursement for pharmaceuticals. Antidepressants are eligible for either basic reimbursement (42% of patient costs) or special reimbursement (100% of the patient costs exceeding 1.50 euro) [23]. The register includes records for between 91% and 99% of SSRI use in noninstitutional settings in Finland from 1999 to 2005 [24] (personal information from Hanna Koskinen and Tinna Voipio). Data recorded in the register include each patient’s birth date, gender, dispensing date of each prescription, and number of dispensed packages. In Finland, up to 3-months’ supply of a drug can be reimbursed in a single dispensing. There is a high concordance between self-reported psychotropic use and psychotropic use among adolescents recorded in a national prescription register [25]. Finnish Prescription Register has been used previously to study nationwide psychotropic drug use [12, 24, 26, 27]. All drugs in the register are coded using the Anatomical Therapeutic Chemical (ATC) classification system that is recommended by the World Health Organization [28]. Antidepressant drugs included in this study were all SSRIs with the ATC code N06AB (escitalopram, citalopram, fluoxetine, sertraline, paroxetine, and fluvoxamine). In Finland, SSRIs had largely replaced the use of TCAs by 1999, with an overall annual consumption of 21.4 defined daily doses (DDDs)/1,000 inhabitants per day for SSRIs compared with 4.5 DDDs/1,000 inhabitants/day for TCAs. Mianserin was the only other antidepressant used in 1999, and it was used at a rate of 1.4 DDDs/1,000 inhabitants per day [29].
Study population
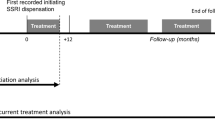
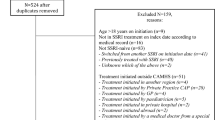
The study population comprised all new users of SSRIs aged <18 years between 1 January 1999 and 31 December 2004 and who were followed until 31 December 2005.
Measures and definitions
A new user was defined as a person dispensed an SSRI who had not collected a prescription for any SSRI in the previous 365 days. The date of initial purchase was defined as the index date. The length of treatment was defined as the total number of dispensed tablets, assuming a dose of one tablet per day. The DDD was assumed to be the dose for liquid dose forms. The basis of this assumption was that there is a range of different drug strengths available in Finland, thereby negating the need for dividing tablets or capsules, and that the recommended daily dose of SSRI treatment is similar for children, adolescents, and adults [13, 30]. The discontinuation date was based on the period covered by the last prescription. Treatment was considered discontinued if there was a treatment-free gap of 210 days. SSRI antidepressants were analyzed as a group (ATC code N06AB), and switches between different SSRIs were considered as continuing therapy. Children and adolescents were categorized into three groups based on their age at the index date: 0–11, 12–15, and 16–17 years old. These categories were selected because the Finnish Current Care Guidelines for Depression recognize children aged ≥12 years as youths [15]. Antidepressant use among children and adolescents in Finland also starts to increase among children aged 12–15 years [6]. The final group was selected because it was assumed that adolescents aged ≥16 years were postpuberty, and use of antidepressants in Finland increases considerably among adolescents aged ≥16 years [6]. The season of initiation was categorized as summer (June–August), autumn (September–November), winter (December–February), or spring (March–May) based on the index date. We analysed the number of children and adolescents who had treatment durations ≤100 days. This was because reimbursed pack sizes of SSRIs in Finland range from 10 to 100 tablets/capsules, with approximately 13% of children and adolescents initiating treatment with a pack size of 98 or 100 tablets/capsules (unpublished data, the Social Insurance Institution of Finland). The reimbursement rate was divided in two categories: <50%, which covers all recipients in the Basic Refund Category, and >50%, which covers all recipients in the Special Refund Category, who experience psychoses and depressive disorders with psychosis or mania.
Ethical considerations
Under Finnish law, ethics committee approval was not required because only deidentified patient data were used.
Data analysis
Factors associated with treatment duration, studied as a continuous variable, were investigated using Cox regression models adjusted for baseline covariates. The association of time-specific potential explanatory factors with discontinuation was modeled separately for all successive periods from the time of initiation, formed separately for each individual based on the timing of discontinuation since initiation. When studying treatment duration according to year of initiation, the year 2003 was used as the reference. This was because of the safety warnings and health advisories about the use of SSRIs that were issued from that year onward. Observations were censored when a child or adolescent taking an SSRI turned 18 years or when the end of the study period was reached, whichever came first. Sensitivity analyses for different treatment-free gaps of 60–270 days were performed.
Results
In total, 10,376 children and adolescents initiated an SSRI from 1999 to 2004, 35.8% of whom were boys. There were between 1,200 and 1,974 new users each year (Table 1); 53.5% of users were aged 16–17 years. The overall annual proportion of Finnish children and adolescents <18 years who initiated an SSRI in 1999 was 0.10%. The overall annual proportion of Finnish children and adolescents who initiated an SSRI from 2000 to 2004 ranged from 0.15% to 0.18%.
Of all the users who initiated an SSRI during the study period, 37.1% had treatment durations of ≤100 days (Table 1). The mean length of treatment was 267 days and median 161 days in all children and adolescents. In children and adolescents who continued treatment >100 days, mean length was 394 and median 300 days. Citalopram or fluoxetine were the two most frequently initiated SSRIs over the study period (36.8% and 24.5%, respectively). However, initiation of citalopram decreased and of escitalopram increased over the study period (Table 2). The initiation of SSRI treatment with fluoxetine increased rapidly in 2004, whereas the opposite was true for paroxetine. Autumn was the period of greatest initiating activity, with 29.6% of SSRIs initiated from September through November.
During the study period 2,023 (19.5%) children or adolescents restarted their treatment after discontinuing for at least 7 months. During the first drug treatment episode, 1,078 (10.4%) children or adolescents switched SSRIs. In adjusted analyses, age ≤11 years [hazard ratio (HR) 0.87; 95% confidence interval (CI), 0.80–0.94] and age 12–15 years (HR 0.89; 95% CI 0.84–0.93) was associated with longer treatment duration compared with age 16–17 years (Table 3). Treatment duration was shorter among children and adolescents who initiated treatment from September to November compared with the other seasons. Users of fluvoxamine (HR 1.16; 95% CI 1.03–1.30) were associated with shorter treatment duration compared with users of fluoxetine. Treatment discontinuation was inversely associated with receipt of special reimbursement of 100% (HR 0.46, 95% CI 0.39–0.55) compared with nonreceipt of special reimbursement. Gender was not associated with treatment duration.
Discussion
This is the first national study to investigate treatment duration among children and adolescents dispensed SSRIs. The main finding was that more than one third of children and adolescents had treatment durations of ≤ 100 days. Longer treatment duration was observed among younger children, when treatment was initiated in seasons other than September through November and among recipients of a higher reimbursement rate. There may be several reasons why younger children had longer treatment durations. First, a greater proportion of younger children may have been prescribed SSRIs for disorders other than depression. These other disorders may have required shorter durations of SSRI treatment than depression does. Second, physicians may have had a higher threshold for prescribing SSRIs to younger children and, therefore, these children may have been experiencing more severe disorders than older children and adolescents. Third, shorter treatment periods may have been associated with nonadherence; younger children’s parents may have been more involved in administration and supervision of their child’s drug therapy. Previous research suggests that parental involvement in drug taking predicts better adherence and disease control among children and adolescents [31–33]. Younger children may have been monitored and followed up more closely, which has been shown to increase adherence [11]. More than 70% of psychopharmaceutical treatment for Finnish children aged <16 years is initiated by specialist physicians, whereas 59% is initiated by specialist physicians for adolescents aged 16–20 years [6]. In Finland, recipients of specialist secondary health care are routinely prompted to attend follow-up visits. However, adolescents receiving treatment in the primary care system may have been less likely to receive unsolicited follow-up.
Children and adolescents who were recipients of a higher reimbursement rate had longer treatment durations. There are several possible reasons for this finding. First, the Finnish reimbursement system provides higher reimbursement to children and adolescents with psychoses and depressive disorders with psychosis or mania. Thus, eligibility for higher reimbursement indicates more severe illness. A meta-analysis has demonstrated a positive association between adherence to drug therapy and physician-rated but not parent-rated illness severity [34]. However, nonadherence to drug therapy is often considered poor among adults with lack of symptom relief and due to the nature of depression [35]. Second, SSRIs may have been discontinued due to the high cost of ongoing treatment. Cost-related nonadherence is common among adults with depression or poor mental health [36–38]. However, all Finnish residents are entitled to receive at least 42% basic reimbursement for the costs of prescription drugs, including antidepressants, from the SII. The extent of cost-related nonadherence has not been widely studied in Finland. Further research is needed to investigate the generalizability of these findings, including to countries with income-related rather than disease-related provision of drug subsidies.
Children and adolescents who commenced treatment during the autumn months (September to November) exhibited shorter treatment durations. In central Finland, the length of day varies from 5 h in December to 19 h in June [39]. The winter months are characterized by long periods of darkness and cold temperatures. Previous research has identified a high prevalence of transient seasonal affective disorder during October–February in Nordic countries both in adults and in adolescents [40–43]. It is possible that children and adolescents who initiated treatment during September to November had a milder form of depressive symptoms than those who initiated during the other seasons. Further research is required to investigate the generalizability of these findings.
There was a weak association between shorter treatment duration and initiation of fluvoxamine compared with fluoxetine. This may reflect the use of this active ingredient for indications other than depression, including anxiety disorders. However, there were <100 children and adolescents who initiated fluvoxamine and, hence, this finding should be interpreted cautiously. The possible differences in adherence and persistence between active ingredients remain an important topic for future research.
Whereas research into SSRI treatment duration and discontinuation among children and adolescents is scarce, research suggests that more than half of adults who discontinue taking SSRIs in The Netherlands do not inform their physician about stopping drug use [44]. More than 60% of adults in Japan who discontinued taking an SSRI did not inform their physician [45]. Nonpersistence may be linked to both adverse reactions and fear of adverse reactions [44]. It is important that clinicians are aware of the risk of discontinuation so that they can implement strategies to minimize premature discontinuation. A positive intent to continue treatment before initiating an antidepressant drug is associated with greater symptom improvement in adults [46].
Study strengths and limitations
The Finnish National Prescription Register provided a complete record of all SSRI prescriptions reimbursed for all children and adolescents in noninstitutional settings in Finland. However, a corresponding limitation was that the register did not include records of SSRIs supplied or dispensed to children and adolescents in institutional care. In 2004, 7% of all wholesale consumption of SSRIs in Finland was in institutional settings [47]. A small percentage of children and adolescents may have entered institutional care during the follow-up period, resulting in apparent treatment discontinuation. Another reason for apparent treatment discontinuation may be switching to nonpharmacological therapies or serotonin and noradrenaline reuptake inhibitors (SNRIs), which were not included in this study. SNRIs are not indicated for children and adolescents in Finland, but they are occasionally used nevertheless [6]. The register did not include antidepressants that were purchased without reimbursement. However, all Finnish residents were eligible to receive drug subsidies and so dispensing without reimbursement was likely to be rare. Another limitation is that we had no access to information about diagnosis, dose, or disease severity. Thus, we were not able to adjust the results according to these parameters. Data used in our study was for the period 1999–2005. The use of antidepressants among people aged 14–26 years increased during and following our study period [6]. This increase has been partly due to the increased prescription of newer antidepressants, although SSRIs remain the most widely used. Unlike in many other countries, overall prescribing of SSRIs did not decline in Finland following the safety warnings and health advisories issued in 2003 [12]. The fundamental reimbursement system for antidepressants has not changed since our study was conducted.
An advantage of using register-based data was that it was not subject to recall bias [48]. However, not all reimbursed drugs were necessarily taken by the children and adolescents. Our definition of treatment duration was based on the number of dispensed tablets/capsules, and this may have resulted in treatment duration being overestimated in our analyses. Similarly, treatment duration may have been underestimated if children or adolescents halved tablets or overestimated if the prescribed daily dose was two or more tablets/capsules per day.
We investigated the treatment duration by varying the treatment-free gaps from 60 to 270 days to define treatment discontinuation (Tables 4 and 5). The number of discontinuations and mean and median duration varied, as expected, with duration being longer when using longer gaps. However, factors associated with treatment duration in the Cox proportional hazards model remained largely the same when conducting these sensitivity analyses. Both winter and autumn treatment initiations were associated with shorter treatment duration when using shorter treatment gaps to define discontinuation. The associations between lower age and longer treatment duration were weaker when using shorter gaps to define treatment discontinuation. When using the shortest gap to define treatment discontinuation (60 days), there was no longer a significant association between age 0 and 11 years and longer treatment duration. Additional studies are needed to explore factors associated with treatment duration in subsamples of SSRI users with diagnoses that may require shorter-term treatment (for example, specific phobias). An interesting topic for further research would be to explore whether provision of nonpharmacological therapy is associated with duration of pharmacological treatment. In order to include information about diagnoses and disease severity, further qualitative research or research using health administration databases that include clinical data are required. Given that studies about the clinical significance of treatment duration are rare, the clinical significance of the statistically significant associations identified in our study remain uncertain. Nevertheless, the associations identified in our study emphasize important areas for future research.
Conclusion
More than one third of children and adolescents had SSRI treatment episodes ≤100 days. Longer treatment duration was observed among younger children, when treatment was initiated in other seasons than September through November, and among recipients of a higher reimbursement rate. Clinicians should be aware of the high rates of possible premature treatment discontinuation.
References
WHO (2010) Medicines: medicines for children. (referred 17 January 2012) http://www.who.int/mediacentre/factsheets/fs341/en/index.html
Verhamme K, Sturkenboom M (2010) Study designs in paediatric pharmacoepidemiology. Eur J Pharmacol 67(S1):67–74. doi:10.1007/s00228-010-0930-2
Nor Aripin KN, Choonara I, Sammons HM (2011) Systematic review of safety in paediatric drug trials published in 2007. Eur J Clin Pharmacol. Aug 20. [Epub ahead of print]
Correll CU, Kratochvil CJ, March JS (2011) Developments in pediatric psychopharmacology: focus on stimulants, antidepressants and antipsychotics. Journal of Clinical Psychiatry 72(5):655–70. doi:10.4088/JCP.11r07064
Seidel L, Walkup JT (2006) Selective Serotonin Reuptake Inhibitor Use in the Treatment of the Pediatric Non-Obsessive-Compulsive Disorder Anxiety Disorders. Journal of Child and Adolescent Psychopharmacology 16(1/2):171–179. doi:10.1089/cap.2006.16.171
Autti-Rämö I, Sourander A, Seppänen J, Martikainen J (2011) Use of antidepressants among 0–26 year olds in Finland during 1997–2007. European Journal of Psychiatry 25(3):164–172. doi:10.4321/S0213-61632011000300006
Bonati M, Clavenna A (2005) The epidemiology of psychotropic use in children and adolescents. International Review of Psychiatry 17(3):181–188. doi:10.1080/09540260500093768
Volkers A, Heerdink ER, van Dijk L (2007) Antidepressant use and off-label prescribing in children and adolescents in Dutch general practice. Pharmacoepidemiology and Drug Safety 16:1054–1062. doi:10.1002/pds.1430
Bennett K, Teeling M, Feely J (2005) Overprescribing of antidepressants to children: pharmacoepidemiological study in primary care. British Medical Journal 331:1451–1452. doi:10.1136/bmj.331.7530.1451
Murray ML, de Vries CS, Wong ICK (2004) A drug utilization study of antidepressants in children and adolescents using the General Practice Research Database. Arch Dis Child 89:1098–1102. doi:10.1136/adc.2004.064956
Fontanella CA, Bridge JA, Marcus SC, Campo JV (2011) Factors associated with antidepressant adherence for Medicaid-enrolled children and adolescents. Ann Pharmacother 45(7–8):898–909 [Epub ahead of print]
Foulon V, Svala A, Koskinen H, Chen TF, Saastamoinen LK, Bell JS (2010) Impact of regulatory safety warnings on the use of antidepressants among children and adolescents in Finland. Journal of Child and Adolescent Psychopharmacology 20:145–150 doi: http://dx.doi.org/10.1089/cap.2009.0040
Practice Parameter for the Assessment and Treatment of Children and Adolescents With Depressive Disorders. Journal of American Academy of Child and Adolescent Psychiatry, 46(11):1503–1526, 2007 (referred 18 March 2011). http://www.aacap.org/galleries/PracticeParameters/Vol%2046%20Nov%202007.pdf
NICE Guideline. Depression in children and young people. 2005. (referred 18 March 2011). http://www.nice.org.uk/nicemedia/live/10970/29856/29856.pdf
Depression (online). Current Care guideline. Working group set up by the Finnish Medical Society Duodecim and the Finnish Respiratory Society. Helsinki: Finnish Medical Society Duodecim, 2010 (referred 18 March 2011) [in Finnish]. www.kaypahoito.fi
Melfi CA, Chawla AJ, Croghan TW, Hanna MP, Kennedy S, Sredl K (1998) The effects of adherence to antidepressant treatment guidelines on relapse and recurrence of depression. Arch Gen Psychiatry 55:1128–1132. doi:10.1001/archpsyc.55.12.1128
Claxton AJ, Li Z, McKendrick J (2000) Selective serotonin reuptake inhibitor treatment in the UK: risk of relapse or recurrence of depression. Br J Psychiatry 177:163–168. doi:10.1192/bjp.177.2.163
Sood N, Treglia M, Obenchain RL, Dulisse B, Melfi CA, Croghan TW (2000) Determinants of antidepressant treatment outcome. American Journal of Managed Care 6:1327–1336
Gardarsdottir H, van Geffen EC, Stolker JJ, Egberts TC, Heerdink ER (2009) Does the length of the first antidepressant treatment episode influence risk and time to a second episode? J Clin Psychopharmacol 29:69–72. doi:10.1097/JCP.0b013e31819302b1
Gardarsdottir H, Egberts TC, Stolker JJ, Heerdink ER (2009) Duration of antidepressant drug treatment and its influence on risk of relapse/recurrence: immortal and neglected time bias. Am J Epidemiol 170:280–285. doi:10.1093/aje/kwp142
Baldessarini RJ, Tondo L, Ghiani C, Lepri B (2010) Illness risk following rapid versus gradual discontinuation of antidepressants. Am J Psychiatry 167:934–941. doi:10.1176/appi.ajp. 2010.09060880
Furu K, Wettermark B, Andersen M, Martikainen JE, Almarsdottir AB, Sørensen HT (2010) The Nordic Countries as a Cohort for Pharmacoepidemiological Research. Basic & Clinical Pharmacology & Toxicology 106:86–94. doi:10.1111/j.1742-7843.2009.00494.x
Finnish Statistics on Medicines 2010 (2011). Finnish Medicines Agency Fimea and The Social Insurance Institution, Helsinki, Finland. (referred 16 January 2012) http://www.fimea.fi/instancedata/prime_product_julkaisu/fimea/embeds/fimeawwwstructure/20681_Suomen_laaketilasto_2010_netti.PDF
Koskinen H, Maljanen T, Martikainen J (2009) Antipsychotics and antidepressants: An analysis of cost growth in Finland from 1999 to 2005. Clin Ther 31:1469–1477. doi:10.1016/j.clinthera.2009.07.003
Skurtveit S, Selmer R, Tverdal A, Furu K (2008) The validity of self-reported prescription medication use among adolescents varied by therapeutic class. Journal of Clinical Epidemiology 61:714–717. doi:10.1016/j.jclinepi.2007.11.013
Tiihonen J, Lönnqvist J, Wahlbeck K, Klaukka T, Tanskanen A, Haukka J (2006) Antidepressants and the risk of suicide, attempted suicide, and overall mortality in a nationwide cohort. Arch Gen Psychiatry 63:1358–1367. doi:10.1001/archpsyc.63.12.1358
Tiihonen J, Lönnqvist J, Wahlbeck K, Klaukka T, Niskanen L, Tanskanen A, Haukka J (2009) 11-year follow-up of mortality in patients with schizophrenia: a population-based cohort study (FIN11 study). Lancet 374:620–627. doi:10.1016/S0140-6736(09)60742-X
WHO collaborating centre for drug statistics methodology. (referred 18 March 2011). http://www.whocc.no/atc_ddd_index/
Finnish Statistics on Medicines 1999 (2000). Finnish Medicines Agency and The Social Insurance Institution, Helsinki, Finland
Hetrick S, Merry S, McKenzie J, Sindahl P, Proctor M: Selective serotonin reuptake inhibitors (SSRIs) for depressive disorders in children and adolescents. The Cochrane Library, CD004851: 2009. (referred 18 March 2011). http://onlinelibrary.wiley.com/o/cochrane/clsysrev/articles/CD004851/pdf_standard_fs.html
Anderson B, Ho J, Brackett J, Finkelstein D, Laffel L (1997) Parental involvement in diabetes management tasks: Relationships to blood glucose monitoring adherence and metabolic control in young adolescents with insulin-dependent diabetes mellitus. J Pediatr 130(2):257–265. doi:10.1016/S0022-3476(97)70352-4
van Dellen QM, Stronks K, Bindels PJE, Öry FG, van Aalderen WMC (2008) Adherence to inhaled corticosteroids in children with asthma and their parents. Respiratory Medicine 102:755–763. doi:10.1016/j.rmed.2007.12.005
Berg CA, King PS, Butler JM, Pham P, Palmer D, Wiebe D (2010) Parental involvement and adolescents diabetes management: the mediating role of self-efficacy and externalizing and internalizing behaviors. Journal of Pediatric Psychology 1–11 (referred 18 March 2011) http://jpepsy.oxfordjournals.org/content/early/2010/10/04/jpepsy.jsq088.full.pdf+html
DiMatteo RM, Haskard KB, Williams SL (2007) Health beliefs, disease severity, and patient adherence. A meta-analysis. Medical Care 45:521–528. doi:10.1097/MLR.0b013e318032937e
Masand PS (2003) Tolerability and adherence issues in antidepressant therapy. Clin Ther 25(8):2289–2304. doi:10.1016/S0149-2918(03)80220-5 DOI:dx.doi.org
Briesacher BA, Gurwitz JH, Soumerai SB (2007) Patients at-risk for cost-related medication nonadherence: a review of the literature. Journal of General Internal Medicine 22(6):864–871. doi:10.1007/s11606-007-0180-x
Kemp A, Roughead E, Preen D, Glover J, Semmens J (2010) Determinants of self-reported medicine underuse due to cost: a comparison of seven countries. Journal of Health Services Research & Policy 15(2):106–114. doi:10.1258/jhsrp.2009.009059
Zivin K, Ratliff S, Heisler MM, Langa KM, Piette JD (2010) Factors influencing cost-related nonadherence to medication in older adults: a conceptually based approach. Value in Health 13(4):338–345. doi:10.1111/j.1524-4733.2009.00679.x
Finnish Meteorological Institute. Length of day. (referred 18 March 2011) Available online at http://www.fmi.fi/weather/climate_7.html
Sourander A, Koskelainen M, Helenius H (1999) Mood, latitude and seasonality among adolescents. Journal of American Academy of Child and Adolescent Psychiatry 38(10):1271–1276. doi:10.1097/00004583-199910000-00016
Saarijärvi S, Lauerma H, Helenius H, Saarilehto S (1999) Seasonal affective disorders among rural Finns and Lapps. Acta Psychiatr Scand 99:95–101. doi:10.1111/j.1600-0447.1999.tb07206.x
Magnusson A (2000) An overview of epidemiological studies on seasonal affective disorder. Acta Psychiatr Scand 101:176–184. doi:10.1034/j.1600-0447.2000.101003176.x
Rastad C, Sjöden P-O, Ulfberg J (2005) High prevalence of self-reported winter depression in a Swedish county. Psychiatry and Clinical Neurosciences 59:666–675. doi:10.1111/j.1440-1819.2005.01435.x
van Geffen E, van Hulten R, Bouvy M, Egberts A, Heerdink E (2008) Characteristics and reasons associated with nonacceptance of selective serotonin-reuptake inhibitor treatment. Ann Pharmacother 42:218–225. doi:10.1345/aph.1K516
Sawada N, Uchida H, Suzuki T, Watanabe K, Kikuchi T, Handa T, Kashima H (2009) Persistence and compliance to antidepressant treatment in patients with depression: A chart review. BMC Psychiatry 9:38–47. doi:10.1186/1471-244X-9-38
Warden D, Trivedi M, Wisniewski S, Lesser I, Mitchell J, Balasubramani G, Fava M, Shores-Wilson K, Stegman D, Rush AJ (2009) Identifying risk for attrition during treatment for depression. Psychother Psychosom 78:372–379. doi:10.1159/000235977
National Agency for Medicines and Social Insurance Institution of Finland: Finnish Statistics on Medicines 2004. Helsinki 2005
Lau HS, de Boer A, Beuning KS, Porsius A (1997) Validation of pharmacy records in drug exposure assessment. Journal of Clinical Epidemiology 50:619–625. doi:10.1016/S0895-4356(97)00040-1
Acknowledgements
We thank Ms. Hilkka Ruuska of the Social Insurance Institution for assistance with data management.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Saastamoinen, L.K., Wallin, M., Lavikainen, P. et al. Treatment duration with selective serotonin reuptake inhibitors among children and adolescents in Finland: a nationwide register study. Eur J Clin Pharmacol 68, 1109–1117 (2012). https://doi.org/10.1007/s00228-012-1233-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-012-1233-6