Abstract
Emotional dysregulation in childhood has been associated with various forms of later psychopathology, although no studies have investigated the personality related adolescent outcomes associated with early emotional dysregulation. The present study uses a typological approach to examine how the child behavior checklist-dysregulation profile (CBCL-DP) predicts DSM-5 pathological personality traits (as measured with the personality inventory for the diagnostic and statistical manual of mental disorders 5 or PID-5 by Krueger et al. (Psychol Med 2012)) across a time span of 4 years in a sample of 243 children aged 8–14 years (57.2 % girls). The results showed that children assigned to the CBCL-DP class are at risk for elevated scores on a wide range of DSM-5 personality pathology features, including higher scores on hostility, risk taking, deceitfulness, callousness, grandiosity, irresponsibility, impulsivity and manipulativeness. These results are discussed in the context of identifying early manifestations of persistent regulation problems, because of their enduring impact on a child’s personality development.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although the fourth edition of the diagnostic and statistical manual of mental disorders (DSM-IV-TR [2]) provides explicit criteria for bipolar disorder in adults, there is no consensus on the applicability of these criteria in younger age groups [3–5]. From an alternative and age-specific perspective, Biederman et al. [6] were the first to demonstrate that children suffering from juvenile bipolar disorder (JBD) can be characterized along their elevated scores on three scales of the well-established child behavior checklist (CBCL [7, 8]), including the anxious/depressed (AD), attention problems (AP), and aggressive behavior (AGG) scales. This initial finding was subsequently replicated by independent research groups [9–13], and stimulated the use of a specific label for this CBCL profile, such as the CBCL-juvenile bipolar disorder profile (CBCL-JBD [14]), the CBCL-pediatric bipolar disorder profile [15] or the CBCL mania proxy [16]. These different labels all refer to children with co-occurring clinical symptoms of anxiety or depression, attention problems and aggressive behavior, and hence only differ in their naming of this behavioral profile.
The validity of the CBCL-JBD profile has been well documented, with empirical evidence supporting its heritability [14], stability across age [17], and consistency across countries, samples and methodologies [14, 18]. Specific predictive validity of the CBCL-JBD profile for juvenile bipolarity was initially demonstrated by Biederman et al. [6] and was further replicated in a range of studies [10, 11, 14, 19, 20], that all underscored the value of the CBCL-JBD profile as a screening tool for bipolarity at a young age. More recent evidence has, however, shown that the profile is less predictive of future bipolar disorder in children, and more predictive of outcomes that are characterized by a broader dysregulation component [21–25], resulting in a proposal of Ayer et al. [23] to consider this profile as a proxy for the assessment of early self-regulation disorders, including affective, cognitive and behavioral dysregulation. Corroborating this suggestion, Althoff et al. [18] changed the profile “CBCL-juvenile bipolar disorder” (CBCL-JBD) into the “CBCL-dysregulation profile” (CBCL-DP),Footnote 1 reflecting its distinctiveness from the narrow construct of bipolarity and referring to a broader dysregulation phenotype.
Current evidence on the validity of the CBCL-DP heavily relies on cross-sectional designs, with only a few studies assessing its longitudinal outcome. Among these, the majority explored outcomes in terms of impairment and DSM-IV Axis I disorders [15, 18, 25–27], all suggesting that children with the DP are at higher risk for a wide range of maladaptive Axis I related outcomes, an overall high level of psychosocial impairment, and psychiatric hospitalization.
However, some limitations of these designs, such as the use of high risk samples and varying cut-off points, hamper the generalizability of these findings. Althoff et al. [28] addressed these limitations and examined the longitudinal outcomes of the CBCL-DP in children of the general population, by applying latent class analysis (LCA) to empirically define the CBCL-DP instead of an arbitrarily chosen T-score as cut-point. LCA is a statistical technique that searches for discrete, homogeneous groups of individuals with a similar response pattern (e.g., children who score concurrently high on the AD, AP and AGG scales are assigned to the CBCL-DP class). This method of grouping persons differs from factor analysis, a variable-centered approach of data analyses grouping items based on their loading on specific factors [29]. The specific advantage of LCA compared to the cut-off point procedure, concerns its sensitivity to the overall response pattern and its ability to include children with response profiles that resemble a CBCL-DP, even when they demonstrate a subthreshold score on one of the scales. Furthermore, LCA optimizes the generalizability compared to the cut-point approach [22, 28].
The validity of LCA has also been underscored by evidence supporting the heritability of the CBCL-DP (i.e., when comparing monozygotic and dizygotic odd ratios, there is a much higher likelihood of monozygotic twins to be subsumed in the same CBCL-DP class compared to dizygotic twins) [22], as well as its relation with suicidality [22] and a strong cross-informant correspondence [18]. In addition, the CBCL-DP class proved to significantly predict adult anxiety, mood, and disruptive behavior, as well as drug abuse disorders, showing that it signifies an early vulnerability profile for a persisting deficit in the regulation of affect, cognition and behavior. Moreover, LCA was also used in a recent cross-sectional study comparing the temperament of CBCL-DP children with children having a different CBCL profile [30]. The results showed that CBCL-DP children were specifically characterized by high novelty seeking, high harm avoidance, low reward dependence and low persistence [30], representing a “disengaged profile”, associated with impaired functioning and more psychopathology [31].
Specific evidence on the significance of early dysregulation for later Axis II personality disorders (PDs) is scarce, with only two longitudinal studies demonstrating a link between childhood dysregulation and adolescent/adult DSM-IV cluster B [25] and cluster C PDs or any PD [32], and one conceptual analysis of Althoff et al. [30] suggesting that the temperamental profile of dysregulated children is comparable to the temperament of adults suffering from DSM-IV cluster B PDs. This paucity of research on PD outcome for childhood dysregulation may be understood from the overall exclusion of childhood PD antecedents in the DSM-tradition that has discouraged research on the relevance of childhood maladaptive traits for adult PDs [33]. However, this field is now in a fast moving status, with substantial evidence indicating that the current DSM-IV operationalization of PDs not only lacks a developmental perspective on personality pathology, but also shows a number of limitations that impede a reliable and valid description of personality symptomatology [34, 35].
Building upon these limitations, the past decade has witnessed a shift toward a more dimensionally oriented system that addresses the categorical problems such as arbitrary criteria cut-offs, high comorbidity, lack of comprehensiveness, and temporal instability [35]. This dimensional approach will be embedded in the upcoming fifth edition of the DSM (DSM-5; http://www.dsm5.org) and will propose a dimensional personality trait model with a corresponding inventory (i.e., personality inventory for DSM-5 or PID-5 [1]), including 25 facets of personality pathology that can be empirically structured in five broadband domains of maladaptive personality variation (i.e., negative affect, detachment, antagonism, disinhibition and psychoticism), in a replicable way [36]. Furthermore, the scores on these PID-5 traits can be used to decide upon the correspondence of an individual’s trait profile with the six PD prototypes that are proposed for DSM-5 (i.e., the antisocial, borderline, narcissistic, avoidant, schizotypal and obsessive–compulsive PD prototypes) [37]. This PID-5 shows promising results in terms of its reliability and validity in adults [1, 36]. Furthermore, De Clercq et al. (under review) have addressed the need for a developmental perspective on PDs in DSM-5 and found preliminary evidence for the applicability of the PID-5 in adolescents.
From this proposed DSM-5 perspective on personality pathology, the present study is the first to examine the significance of childhood dysregulation for understanding later personality difficulties. More specifically, we will explore in a combined sample of community and referred children whether a CBCL-DP class can be empirically identified and differentiated from other profiles based upon LCA. We will examine how this early CBCL-DP has predictive value in terms of pathological personality traits 4 years later, including a conceptual analysis of similarities between the childhood CBCL-DP and each of the DSM-5 PD prototypes. We hypothesized (1) that a CBCL-DP class would be identified, because of its replicability across countries, samples and methodologies [14, 18], and further assumed that there would be significant differences in personality pathology outcome between dysregulated and non-dysregulated children, (2) that the predictive validity of the CBCL-DP class for later personality difficulties would be supported, based upon previous evidence on the association between the CBCL-DP and early Axis I related problems [15, 18, 25–27] as well as later personality difficulties [25, 30, 32], and (3) that this predictive value would be most explicit for cluster B PDs because of the shared dysregulation features.
Method
Participants and procedure
To maximize the variability in pathology scores, a combined Flemish sample was used (N = 243; 57.2 % girls; 8–14 years old, M = 10.87, SD = 1.80), including both children from the general population (n = 97) and referred children (n = 146), recruited by third-year undergraduate psychology students of Ghent University in the course of the Personality and Affect Longitudinal Study (PALS, for detailed information see [38]). Two follow-up assessments have previously been organized, with the current fourth wave of this follow-up study (referred to as “Time 2” in this paper) 4 years after the initial assessment (N = 166; 62.7 % girls; mean age = 15.10 years, SD = 1.79). In this last follow-up, participants received an unannounced five Euro voucher as a return for their enduring participation. Data collection was approved by the Ethical Review Board of Ghent University. Participants were assured that the information would be treated confidential and only served research purposes. Written informed consent was obtained from all participants. Figure 1 provides a schematic flow-chart illustrating recruitment and attrition.
Population sample
Students were instructed to recruit a Dutch-speaking child between 8 and 14 years old. Children with a mental retardation or a physical disability were excluded. An adequate geographical distribution of the sample can be assumed, because hometowns of students who enroll in the Ghent University psychology program are well-spread across Flanders. All students visited the families at home and provided information about the study aims, the procedure and ethics of data collection. Mothers were requested to fill out a set of questionnaires. At Time 1, the sample included 97 children (64.9 % girls; mean age = 10.84 years, SD = 1.84). 4 years later, at Time 2, the sample consisted of 66 adolescents (74.2 % girls; mean age = 15.02 years, SD = 1.80).
Referred sample
The same inclusion and exclusion criteria were applied as described above. In addition, children of the PALS referred subsample were either actively enrolled in mental health services, or were assigned to a waiting list of a specific mental health service centre. There were no further restrictions in terms of reason for referral; hence children with a variety of behavioral or emotional problems were included in the study. All children were recruited by students via general mental health services that were listed on an online directory of registered mental health care providers in Flanders. To insure a full geographical coverage of Flanders, students were provided with the contact details of the services selected by one of the researchers. Students made an appointment by phone with the treating psychologists, in order to explain the study aims, procedures and ethics of data collection. Psychologists were requested to invite the first family on their appointment schedule for participation in the study. After participants were provided a consent form and guiding information letter, the psychologist handed out the questionnaires. At the next appointment, the completed questionnaires and signed consent forms were returned in a sealed envelope. At Time 1, the referred sample consisted of 146 children (52.1 % girls; mean age = 10.94, SD = 1.85). 75 % was enrolled in mental health services for the first time, with 71 % experiencing active treatment at the moment of assessment. The primary reason for counseling or referral included anxiety symptoms (20.7 %), depressive symptoms (14.5 %), grief or emotional problems due to parental divorce (11.3 %), behavioral problems (10.7 %), personality or identity problems (7.6 %), developmental disorders (6.9 %), psychosomatic symptoms (5.0 %), study problems (5.0 %), social problems (3.8 %), attention or concentration problems (2.5 %), sleeping problems (1.9 %), eating problems (1.3 %), incontinence problems (1.3 %), and automutilation/suicide attempts (0.6 %). The remaining 6.9 % were referred for other reasons or this information was unavailable. 4 years later, the sample comprised 100 adolescents (55 % girls; mean age = 15.14 years, SD = 1.79).
Attrition
In both the general population and referred sample, the drop-out rate was the same (i.e., 32 %). The adolescents of the participating families did not differ in age compared to the drop-outs (F = 0.19, p = 0.67) neither in terms of education level (F = 0.10, p = 0.76), although the mothers of the current follow-up moment were higher educated than the drop-outs (F = 15.78, p = 0.00).
Measures
Child behavior checklist (CBCL)
At Time 1, mothers filled out the Dutch CBCL [7, 8], a standardized assessment of behavior and emotional problems in children from 6 to 18 years old. These problems are measured by 113 items on a 3-point scale. The CBCL consists of eight psychopathology scales (withdrawn/depressed, somatic complaints, anxious/depressed, social problems, thought problems, attention problems, rule-breaking behavior, and aggressive behavior). The CBCL has excellent psychometric properties and many studies have supported its reliability and validity in both clinical and non-clinical populations [7, 8, 20]. Furthermore, three broad scales (internalizing, externalizing, and total problems) and four competency scales are included (activities, social, school, and total competency). The present study used the eight psychopathology scales and they demonstrated sufficient internal consistency with Cronbach’s α’s ranging from 0.65 (rule-breaking behavior) to 0.92 (aggressive behavior). The CBCL-DP includes elevated ratings on the anxious/depressed, attention problems, and aggressive behavior scales with high reliability coefficients of Cronbach’s α = 0.92, 0.81 and 0.92, respectively.
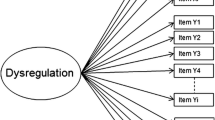
Personality inventory for DSM-5 (PID-5)
At Time 2, mothers completed the Dutch version of the PID-5 [1], developed by the DSM-5 personality and personality disorders workgroup, and translated into Dutch by De Clercq et al. (under review). The PID-5 maladaptive personality traits are measured by 220 items rated on a 4-point scale ranging from 0 to 3, with higher scores indicating more pathology. Initial findings on the hierarchical structure of the PID-5 [1, 36] suggest that the items can be hierarchically organized in 25 reliable facets ([1, 36], De Clercq et al. under review) of maladaptive personality that are further structured in five broad maladaptive trait domains, with proposed labels of negative affect, detachment, antagonism, disinhibition and psychoticism. In the present study, we only focused on the PID-5 facet-level because the DSM-5 trait proposal is currently only elaborated at this level. Cronbach α coefficients ranged from 0.77 (submissiveness) to 0.95 (eccentricity). Only one facet showed a rather low α coefficient of 0.53 (suspiciousness) attributable to the low item-total correlations of two items (r = 0.10 and −0.07), probably resulting from a reversed keying formulation. Therefore, these two reversed keyed items were omitted (resulting in a better coefficient of α = 0.76) and this adapted scale was used in all further analyses.
Analyses
LCA was conducted on the maternal rated CBCL at Time 1, to empirically explore the existence of a CBCL-DP class in the current data and to estimate class membership of all children. LCA is a person-centered data-analytic strategy and is able to assign persons to a statistically independent class when they respond in the same way to items (or scales) of a questionnaire. Thus, each class has a specific symptom (item or scale) endorsement profile [39]. Latent class models were fitted by a robust maximum likelihood algorithm using the program Mplus® 6.12 [40] and age, gender and clinical status were entered as covariates. Models estimating 1- through 7-class solutions were compared, relying on the CBCL T-scores of all scales. To calculate the best fitting model, a M class solution was compared to a M + 1 class solution. Changes in two goodness-of-fit indices were used as guidelines for model selection, i.e., the Akaike Information Criterion (AIC [41]) and the sample-size-adjusted Bayesian Information Criterion (ABIC [42]), with decreases in coefficients indicating a better fit. Class membership for all children was estimated based upon the highest class membership probability across classes. The latent class with the highest T-scores on the AD, AP, and AGG scales was labeled the CBCL-DP class, and was the focus of all further analyses. We specifically examined whether children assigned to the CBCL-DP class differed from those in other classes in terms of personality difficulties 4 years later by applying multivariate analysis of variance (MANOVA). The 25 DSM-5 personality pathology traits at Time 2 were entered as dependent factors and Time 1 DP class membership as a categorical independent variable, followed by a multiple comparison contrast procedure (five a priori paired contrasts) with Bonferroni correction (αPC = αPE/P = 0.05/5 = 0.01) using PASW Statistics 18.0.2 (SPSS). More precisely, we calculated the mean-level differences in the personality scores (T2) between the CBCL-DP class (class 6) and the five other classes, resulting in five contrasts (DP - class 1, DP - class 2, DP - class 3, DP - class 4 and DP - class 5). Given the mixed nature of the sample, we controlled for effects of clinical status in all analyses. To examine the predictive validity of the CBCL-DP, regression analyses were conducted using the CBCL-DP class membership probability as predictor and the 25 PID-5 traits as outcomes. Finally, the PID-5 personality traits predicted by the CBCL-DP were conceptually compared with the PID-5 traits of the PD prototypes as listed on the DSM-5 website.
Results
Exploring the presence of CBCL-DP
Table 1 demonstrates that a six-class solution represented the best fitting model and Table 2 reports the sociodemographic information for the six classes. A specific CBCL-DP class was identified (i.e., class 6) including 10.3 % of the children. These 25 children (13 boys and 12 girls) all belonged to the referred group (n = 146), and showed a mean T-score on the AD, AP and AGG CBCL scales of respectively 81, 76 and 74 (see Fig. 2).
The omnibus MANOVA after controlling for differences in clinical status was significant (F = 1.38, p = 0.007), as reflected in mean-level differences among classes for 18 out of 25 DSM-5 personality facets 4 years later (see Table 3). Five a priori contrasts were calculated with the CBCL-DP class as reference category.
The most significant differences (6 of the 25) were found between the CBCL-DP class and class 1 (no symptoms). More precisely, children in the CBCL-DP class scored significantly higher on hostility, impulsivity, emotional lability, deceitfulness, callousness, and grandiosity. The CBCL-DP class also showed significant differences with the mild internalizing class (class 3), demonstrating higher scores on impulsivity, deceitfulness, risk taking, and hostility. The contrast between the CBCL-DP class and class 2 (moderate attention problems with anxious-depressed and social problems) suggested two significant differences, with CBCL-DP children showing elevated scores on callousness and risk taking compared to class 2. Regarding the contrast between class 6 (CBCL-DP) and class 4 (severe anxious-depressed and thought problems), the children in the CBCL-DP class only scored significantly higher on risk taking compared to those in class 4. Finally, no significant differences were found between the CBCL-DP class and class 5 (moderate externalizing with anxious-depressed and social problems) on pathological personality trait outcome. This can be explained by the finding that there is only a difference in severity between those two classes.
Predictive validity of the CBCL-DP
The CBCL-DP class was a significant predictor of later hostility (β = 0.24, t = 3.22, p ≤ 0.01), risk taking (β = 0.25, t = 3.12, p ≤ 0.01), deceitfulness (β = 0.21, t = 2.63, p ≤ 0.01), and callousness (β = 0.20, t = 2.57, p ≤ 0.01), indicating that its predictive value is most significant for externalizing-related personality difficulties. Less substantial, but still significant associations were found with later grandiosity (β = 0.20, t = 2.46, p ≤ 0.05), irresponsibility (β = 0.17, t = 2.18, p ≤ 0.05), impulsivity (β = 0.17, t = 2.18, p ≤ 0.05) and manipulativeness (β = 0.16, t = 1.98, p ≤ 0.05) (Table 4), traits that are all sharing a disagreeable trait component.
CBCL-DP and DSM-5 personality disorder prototypes: a conceptual comparison
An overview of the eight maternal rated adolescent DSM-5 traits that are significantly associated with the CBCL-DP and the proposed DSM-5 PD prototypes (i.e., the antisocial, borderline, narcissistic, avoidant, schizotypal and obsessive–compulsive PD prototypes) is provided in Table 5. From a conceptual perspective, it can be suggested that the CBCL-DP is most similar to the adult antisocial PD prototype, with seven out of eight common traits (i.e., hostility, manipulativeness, deceitfulness, callousness, irresponsibility, impulsivity and risk taking). To a lesser extent, the CBCL-DP shows conceptual relations with the adult borderline PD prototype, sharing three of the eight CBCL-DP traits (hostility, impulsivity and risk taking). Regarding the narcissistic PD prototype, only grandiosity is a common factor with the CBCL-DP. The other prototypes do not show any conceptual similarity.
Discussion
The present study prospectively investigates the significance of the CBCL-DP for later personality difficulties in terms of scores on the proposed DSM-5 pathological personality traits. Consistent with our first hypothesis, we identified a CBCL-DP class by means of LCA, broadening the replicability of this profile across countries, samples and methodologies [14] toward the Flemish population. Compared to other CBCL profiles, the CBCL-DP showed, in general, a unique maladaptive personality profile. We also found evidence for our second hypothesis concerning the predictive validity of the CBCL-DP class for later personality difficulties. More specifically, children with a CBCL-DP are at risk for elevated scores on a wide range of DSM-5 maladaptive traits, including higher scores on hostility, risk taking, deceitfulness, callousness, grandiosity, irresponsibility, impulsivity and manipulativeness.
From a specific focus on the validity of the CBCL-DP, our findings are consistent with previous studies showing that the CBCL-DP is predictive of Axis II related pathology [25, 30, 32]. More specifically, the current longitudinal analysis suggests that the CBCL-DP class is conceptually most related to the proposed antisocial as well as to the borderline PD prototype for DSM-5. This is in line with our third hypothesis, assuming that the CBCL-DP class would especially be predictive for cluster B PDs.
This twofold antisocial and borderline outcome for CBCL dysregulated children may be understood from a number of shared characteristics, including impulsive aggression and shared environmental risk factors [43], further indicating that shared developmental aspects as reflected in the childhood CBCL-DP are plausible. More specifically, both the childhood antisocial and borderline construct are characterized by a symptomatic complexity of internalizing and externalizing problem behavior and neuropsychological abnormalities [44]. Each of these symptoms is well represented in the CBCL-DP, including high scores on the internalizing AD scale, the externalizing AGG scale, and the AP scale. Also the antisocial PD is characterized by internalizing pathology such as an increased suicide risk in youth suffering from this PD [45].
From this perspective, the current findings may contribute the developmental field of both the antisocial- and borderline-related pathology in several ways. First of all, the empirical identification of a CBCL-DP in childhood supports its universal character across countries, samples and methodologies [14], suggesting that childhood dysregulation may involve a significant endogenous etiological component. This biologically based perspective on dysregulation symptoms not necessarily implies that humans manifest similar symptoms across time [46]. This assumption refers to the principle of heterotypic continuity, suggesting that the observable level of dysregulation problems may shift over time [47]), although its underlying trait-level has a chronic nature [48]. In this respect, the various associations of the CBCL-DP with DSM-5 traits indicate that this symptomatic variation of dysregulation may also include long-term dysfunction in terms of personality symptoms, illustrating that early dysregulation reflects a temperamental vulnerability that gives rise to personality symptoms when children grow older. Further, our findings suggest that there is no clear one-to-one relation between childhood dysregulation and adult personality pathology, given that dysregulated children tend to develop a wide range of personality symptoms [49]. From these findings, rather than labeling the observed profile as “pediatric bipolar pathology” [14], or “pediatric antisocial or borderline pathology”, we support the suggestion of Althoff et al. [18] to label this profile as “dysregulated” because these children have problems with self-regulation that are broader than what a single PD diagnosis represents.
The present study demonstrates several strengths, such as using a personality outcome inventory (PID-5 [1]) developed from a newly proposed personality framework for DSM-5. We furthermore applied a recent statistical technique for deriving empirically based latent classes on the cross-culturally valid CBCL [7, 8], adopting a longitudinal design and including both referred and non-referred children.
Despite these strengths, our study is also characterized by several limitations. First of all, the number of children classified within the CBCL-DP class is rather small. Although this rate is comparable to other studies [25], prospective studies on outcome of childhood dysregulation would benefit from larger samples. Related to this, we can only draw conclusions upon personality pathology in the referred sample because the CBCL-DP was not identified in the population sample. This is probably due to the small sample size (n = 97) since previous studies did find a CBLC-DP class in population samples, e.g., [28]. Second, the present study is restricted to maternal reports at both Time 1 and 2, and should be broadened toward multiple raters at each assessment point to explore the replicability of findings across informants. Third, no information is available on the maladaptive personality traits in the drop-out group. However, in both the population and referred sample, the drop-out percentages were the same (i.e., 32 %) and even if systematic drop-out would have been the case, modeling within longitudinal datasets indicated that the effects on later regressions are negligible [50]. Fourth, the participants are recruited from a Flemish sample, which potentially limits the generalizability of the results to other countries. Fifth, it is now rather unclear how LCA can be used in an individual contact in clinical practice since it is a group-level analysis. However, in this study, we aimed to identify a CBCL-DP at a group-level and therefore, a large sample as well as a reliable statistical method, such as LCA, was needed. Finally, based upon the extensive literature on the development of antisocial- and borderline-related pathology, a future prospective study on the developmental pathway of early dysregulation should also represent a contextual perspective, including specific environmental risk factors that may be involved. Although the present study addresses at this point a more narrow perspective on dysregulation in terms of adolescent personality outcome, the current findings convincingly show the significance of early dysregulation in terms of its association with personality difficulties and hence empirically illustrate that a specific combination of scores on the various scales of the well-validated CBCL may contribute the diagnostic process of childhood psychopathology in terms of identifying children who are prone to more maladaptive pathways of personality development.
Notes
Throughout this study, we will use this broad CBCL-DP label as interchangeable with the other labels that have previously been proposed for this specific profile of psychopathology.
References
Krueger RF, Derringer J, Markon KE, Watson D, Skodol A (2012) Initial construction of a maladaptive personality trait model and inventory for DSM-5. Psychol Med. doi:10.1017/S0033291711002674
American Psychiatric Association (2000) Diagnostic and statistical manual of mental disorders (DSM-IV-TR), 4th edn, Text revision Author, Washington
Coyle JT, Pine DS, Charney DS, Lewis L, Nemeroff CB, Carlson GA, Joshi PT, Reiss D, Todd RD, Hellander M (2003) Depression and bipolar support alliance consensus statement on the unmet needs in diagnosis and treatment of mood disorders in children and adolescents. J Am Acad Child Adolesc Psychiatry 42(12):1494–1503. doi:10.1097/01.chi.0000091945.28938.8f
Geller B, Luby J (1997) Child and adolescent bipolar disorder: a review of the past 10 years. J Am Acad Child Psychiatry 36(9):1168–1176. doi:10.1097/00004583-199709000-00008
Leibenluft E, Charney DS, Towbin KE, Bhangoo RK, Pine DS (2003) Defining clinical phenotypes of juvenile mania. Am J Psychiatry 160(3):430–437. doi:10.1176/appi.ajp.160.3.430
Biederman J, Wozniak J, Kiely K, Ablon S, Faraone S, Mick E, Mundy E, Kraus I (1995) CBCL clinical-scales discriminate prepubertal children with structured interview-derived diagnosis of mania from those with ADHD. J Am Acad Child Psychiatry 34(4):464–471. doi:10.1097/00004583-199504000-00013
Achenbach TM, Rescorla LA (2001) Manual for ASEBA school-age forms and profiles. University of Vermont, Research Center for Children, Youth, & Families, Burlington
Verhulst FC, Van der Ende J (2001) Handleiding voor de CBCL/6-18, YSR en TRF (Dutch manual for CBCL/6-18, YSR, and TRF). Erasmus Universiteit Rotterdam, Sophia Kinderziekenhuis, Rotterdam
Carlson GA, Kelly KL (1998) Manic symptoms in psychiatrically hospitalized children—what do they mean? J Affect Disord 51(2):123–135. doi:10.1016/s0165-0327(98)00211-0
Dienes KA, Chang KD, Blasey CM, Adleman NE, Steiner H (2002) Characterization of children of bipolar parents by parent report CBCL. J Psychiatr Res 36(5):337–345. doi:s0022-3956(02)00019-510.1016/s0022-3956(02)00019-5
Geller B, Warner K, Williams M, Zimerman B (1998) Prepubertal and young adolescent bipolarity versus ADHD: assessment and validity using the WASH-U-KSADS, CBCL and TRF. J Affect Disord 51(2):93–100. doi:10.1016/s0165-0327(98)00176-1
Hazell PL, Lewin TJ, Carr VJ (1999) Confirmation that child behavior checklist clinical scales discriminate juvenile mania from attention deficit hyperactivity disorder. J Paediatr Child H 35(2):199–203
Wals M, Hillegers MHJ, Reichart CG, Ormel J, Nolen WA, Verhulst FC (2001) Prevalence of psychopathology in children of a bipolar parent. J Am Acad Child Psychiatry 40(9):1094–1102. doi:10.1097/00004583-200109000-00019
Hudziak JJ, Althoff RR, Derks EM, Faraone SV, Boomsma DI (2005) Prevalence and genetic architecture of child behavior checklist-juvenile bipolar disorder. Biol Psychiatry 58(7):562–568. doi:10.1016/j.biopsych.2005.03.024
Biederman J, Petty CR, Monuteaux MC, Evans M, Parcell T, Faraone SV, Wozniak J (2009) The child behavior checklist-pediatric bipolar disorder profile predicts a subsequent diagnosis of bipolar disorder and associated impairments in ADHD youth growing up: a longitudinal analysis. J Clin Psychiatry 70(5):732–740
Galanter CA, Carlson GA, Jensen PS, Greenhill LL, Davies M, Li W, Chuang SZ, Elliott GR, Arnold LE, March JS, Hechtman L, Pelham WE, Swanson JM (2003) Response to methylphenidate in children with attention deficit hyperactivity disorder and manic symptoms in the multimodal treatment study of children with attention deficit hyperactivity disorder titration trial. J Child Adol Psychop 13(2):123–136. doi:10.1089/104454603322163844
Boomsma DI, Rebollo I, Derks EM, van Beijsterveldt TCEM, Althoff RR, Rettew DC, Hudziak JJ (2006) Longitudinal stability of the CBCL-juvenile bipolar disorder phenotype: a study in Dutch twins. Biol Psychiatry 60(9):912–920. doi:10.1016/j.biopsych.2006.02.028
Althoff RR, Rettew DC, Ayer LA, Hudziak JJ (2010) Cross-informant agreement of the dysregulation profile of the child behavior checklist. Psychiatry Res 178(3):550–555. doi:10.1016/j.psychres.2010.05.002
Faraone SV, Althoff RR, Hudziak JJ, Monuteaux M, Biederman J (2005) The CBCL predicts DSM bipolar disorder in children: a receiver operating characteristic curve analysis. Bipolar Disord 7(6):518–524. doi:10.1111/j.1399-5618.2005.00271.x
Mick E, Biederman J, Pandina G, Faraone SV (2003) A preliminary meta-analysis of the child behavior checklist in pediatric bipolar disorder. Biol Psychiatry 53(11):1021–1027. doi:10.1016/s0006-3223(03)00234-8
Althoff RR, Ayer LA, Rettew DC, Hudziak JJ (2010) Assessment of dysregulated children using the child behavior checklist: a receiver operating characteristic curve analysis. Psychol Assess 22(3):609–617. doi:10.1037/a0019699
Althoff RR, Rettew DC, Faraone SV, Boomsma DI, Hudziak JJ (2006) Latent class analysis shows strong heritability of the child behavior checklist-juvenile bipolar phenotype. Biol Psychiatry 60(9):903–911. doi:10.1016/j.biopsych.2006.02.025
Ayer L, Althoff R, Ivanova M, Rettew D, Waxler E, Sulman J, Hudziak J (2009) Child behavior checklist juvenile bipolar disorder (CBCL-JBD) and CBCL posttraumatic stress problems (CBCL-PTSP) scales are measures of a single dysregulatory syndrome. J Child Psychol Psychiatry 50(10):1291–1300. doi:10.1111/j.1469-7610.2009.02089.x
Diler RS, Birmaher B, Axelson D, Goldstein B, Gill M, Strober M, Kolko DJ, Goldstein TR, Hunt J, Yang M, Ryan ND, Iyengar S, Dahl RE, Dorn LD, Keller MB (2009) The child behavior checklist (CBCL) and the CBCL-bipolar phenotype are not useful in diagnosing pediatric bipolar disorder. J Child Adolesc Psychopharmacol 19(1):23–30. doi:10.1089/cap.2008.067
Meyer SE, Carlson GA, Youngstrom E, Ronsaville DS, Martinez PE, Gold PW, Hakak R, Radke-Yarrow M (2009) Long-term outcomes of youth who manifested the CBCL-pediatric bipolar disorder phenotype during childhood and/or adolescence. J Affect Disord 113(3):227–235. doi:10.1016/j.jad.2008.05.024
Hazell PL, Carr V, Lewin TJ, Sly K (2003) Manic symptoms in young males with ADHD predict functioning but not diagnosis after 6 years. J Am Acad Child Psychiatry 42(5):552–560. doi:10.1097/01.chi.0000046830.95464.33
Holtmann M, Buchmann AF, Esser G, Schmidt MH, Banaschewski T, Laucht M (2011) The Child Behavior Checklist-dysregulation profile predicts substance use, suicidality, and functional impairment: a longitudinal analysis. J Child Psychol Psychiatry 52(2):139–147. doi:10.1111/j.1469-7610.2010.02309.x
Althoff RR, Verhulst FC, Rettew DC, Hudziak JJ, van der Ende J (2010) Adult outcomes of childhood dysregulation: a 14 year follow-up study. J Am Acad Child Adolesc Psychiatry 49(11):1105–1116. doi:10.1016/j.jaac.2010.08.006
Althoff RR, Rettew DC, Boomsma DI, Hudziak JJ (2009) Latent class analysis of the child behavior checklist obsessive-compulsive scale. Compr Psychiatry 50(6):584–592. doi:10.1016/j.comppsych.2009.01.005
Althoff RR, Ayer LA, Crehan ET, Rettew DC, Baer JR, Hudziak JJ (2012) Temperamental profiles of dysregulated children. Child Psychiatry Hum Dev 43(4):511–522. doi:10.1007/s10578-012-0280-7
Rettew DC, Althoff RR, Dumenci L, Ayer L, Hudziak JJ (2008) Latent profiles of temperament and their relations to psychopathology and wellness. J Am Acad Child Adolesc Psychiatry 47(3):273–281. doi:10.1097/chi.0b013e318160b403
Halperin JM, Rucklidge JJ, Powers RL, Miller CJ, Newcorn JH (2011) Childhood CBCL bipolar profile and adolescent/young adult personality disorders: a 9-year follow-up. J Affect Disord 130(1–2):155–161. doi:10.1016/j.jad.2010.10.019
De Clercq B, De Fruyt F, Widiger TA (2009) Integrating a developmental perspective in dimensional models of personality disorders. Clin Psychol Rev 29(2):154–162. doi:10.1016/j.cpr.2008.12.002
Clark LA (2007) Assessment and diagnosis of personality disorder: perennial issues and an emerging reconceptualization. Annu Rev Psychol 58:227–257. doi:10.1146/annurev.psych.57.102904.190200
Widiger TA, Trull TJ (2007) Plate tectonics in the classification of personality disorder—shifting to a dimensional model. Am Psychol 62(2):71–83. doi:10.1037/0003-066x.62.2.71
Wright AGC, Thomas KM, Hopwood CJ, Markon KE, Pincus AL, Krueger RF (2012) The hierarchical structure of the DSM-5 pathological personality traits. J Abnorm Psychol 121(4):951–957. doi:10.1037/a0027669
Hopwood CJ, Thomas KM, Wright AGC, Markon KA, Krueger RF (2012) DSM-5 personality traits and DSM-IV personality disorders. J Abnorm Psychol 121(2):424–432. doi:10.1037/a0026656
De Bolle M, De Fruyt F, Decuyper M (2010) The affect and arousal Scales: psychometric properties of the Dutch version and multigroup confirmatory factor analyses. Assessment 17(2):241–258. doi:10.1177/1073191109358175
Goodman LA (1974) Exploratory latent structure-analysis using both identifiable and unidentifiable models. Biometrika 61(2):215–231. doi:10.1093/biomet/61.2.215
Muthén LK, Muthén BO (1998-2010) Mplus user’s guide. Sixth edn. CA: Muthén and Muthén, Los Angeles
Akaike H (1987) Factor-analysis and AIC. Psychometrika 52(3):317–332. doi:10.1007/bf02294359
Schwarz G (1978) Estimating dimension of a model. Ann Stat 6(2):461–464. doi:10.1214/aos/1176344136
Paris J (2003) Personality disorders over time: Precursors, course, and outcome. American Psychiatric Publishing, Inc., Washington
Jucksch V, Salbach-Andrae H, Lenz K, Goth K, Doepfner M, Poustka F, Freitag CM, Lehmkuhl G, Lehmkuhl U, Holtmann M (2011) Severe affective and behavioural dysregulation is associated with significant psychosocial adversity and impairment. J Child Psychol Psychiatry 52(6):686–695. doi:10.1111/j.1469-7610.2010.02322.x
Links PS, Gould B, Ratnayake R (2003) Assessing suicidal youth with antisocial, borderline or narcissistic personality disorder. Can J Psychiatry 48(5):301–310
Shaffer D, Widiger TA, Pincus HA (1998) DSM-IV child disorders, part II: final overview. In: Widiger TA, Frances AJ, Pincus HA et al. (eds) DSM-IV sourcebook, vol 4. American Psychiatric Association, Washington, pp 963–977
Penney SR, Moretti MM (2010) The roles of affect dysregulation and deficient affect in youth violence. Crim Justice Behav 37(6):709–731. doi:10.1177/0093854810365446
Cicchetti D, Crick NR (2009) Precursors and diverse pathways to personality disorder in children and adolescents. Dev Psychopathol 21(3):683–685. doi:10.1017/s0954579409000388
Bemporad JR, Smith HF, Hanson G, Cicchetti D (1982) Borderline syndromes in childhood—criteria for diagnosis. Am J Psychiatry 139(5):596–602
Wolke D, Waylen A, Samara M, Steer C, Goodman R, Ford T, Lamberts K (2009) Selective drop-out in longitudinal studies and non-biased prediction of behaviour disorders. Brit J Psychiatry 195(3):249–256. doi:10.1192/bjp.bp.108.053751
Cohen J (1988) Statistical power analysis for the behavioral sciences (second ed.). Lawrence Erlbaum Associates
Acknowledgments
The authors wish to thank Prof. Dr. Robert Althoff and Prof. Dr. Filip De Fruyt for their helpful comments on an earlier version of this manuscript. The quality of this manuscript improved secondary to the comments of the anonymous reviewers and we thank them for their efforts.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
De Caluwé, E., Decuyper, M. & De Clercq, B. The child behavior checklist dysregulation profile predicts adolescent DSM-5 pathological personality traits 4 years later. Eur Child Adolesc Psychiatry 22, 401–411 (2013). https://doi.org/10.1007/s00787-013-0379-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-013-0379-9