Abstract
Objective
This systematic review aims to answer the following question: What is the psychological impact of orthognathic surgery on patients with dentofacial deformities undergoing orthodontic-surgical treatment?
Material and methods
The search was adapted for each of the following databases: American and Caribbean Center on Health Sciences (LILACS), Cochrane Library, Embase, Psychinfo, PubMed/Medline, Scopus and Web of Science, and gray literature using Google Scholar, OpenGrey, and ProQuest. The risk of bias was assessed using the Joanna Briggs Institute Critical Assessment Checklist. This study performed estimates of interest, random-effects meta-analyses, and calculated heterogeneity using Higgins inconsistency index (I2).
Results
A total of 6751 references were found in all searches. After applying the eligibility criteria after full-text reading, 37 studies comprised the final qualitative synthesis. Thirteen studies were included in quantitative synthesis, and it was possible to meta-analyze data from the following questionnaires: GHQ-28, MMPI, RSES, and SCL-90-R. There was an improvement in psychological aspects related to depression, hysteria, self-esteem, anxiety, obsessive-compulsiveness, interpersonal sensitivity, paranoid ideas, and psychoticism (p < 0.05).
Conclusions
Correction of dentofacial deformity through orthodontic-surgical treatment is associated with improvements observed in several psychological domains, especially in relation to depressive states.
Clinical relevance.
This result highlights the importance of surgeons and orthodontists in promoting adequate control of patients’ expectations and treatment goals taking into account the individual's psychological aspects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Orthodontic-surgical treatment through a combination of orthognathic surgery and orthodontic treatment is the ideal option for the correction of dentofacial deformities [1,2,3]. This procedure consists, in general, in repositioning the maxillary bones, providing a harmonization of the facial bone structure and consequent anatomical-functional corrections [4]. It thus matches biological, functional, and especially aesthetic aspects [5]. This type of treatment involves some phases, such as initial planning, orthodontic preparation, the surgical act repositioning the facial skeleton in a more harmonious position through orthognathic surgery, post-surgical orthodontic refinement, and the containment phase after removal of the fixed orthodontic appliance [3].
Orthodontic-surgical treatment, by making facial changes of patients, both in the preoperative and the postoperative period, may affect the individual's psychosocial factors and their interaction in society [6]. Thus, knowledge of these aspects is of paramount importance for dental professionals since the psychosocial state, in addition to being able to interfere at a macro level, such as influencing the behavior and interpersonal relationships of individuals, may also interfere with parameters of the surgical process itself, such as the motivation to seek treatment and satisfaction with results [7].
To date, there are three systematic reviews addressing the relationship between orthodontic-surgical treatment and psychosocial aspects [8,9,10]. Hunt, O.T. et al. (2001) reported the benefits of orthognathic surgery and studied parameters of self-confidence and social consonance [10]. On the other hand, Alanko, O.M. et al. (2010) did not find great differences in the psychic and social dimensions of the studied patients [8]. The most recent systematic review on this topic [9] did not find scientific evidence attesting the effects of this treatment on the intended outcome due to a high risk of bias presented by the studies included. However, the analyses did not include all available evidence on the subject, making clinical decision-making difficult. The assessment of risk of bias was performed using a tool designed for a different type of study, not consistent with the studies included. This may have resulted in an inadequate assessment of the risk of bias of these studies [11]. No review presented a quantitative synthesis of the findings through meta-analysis. Also, new studies were published on this subject, thus justifying a new systematic review.
Considering this scenario, this systematic review aims to answer the following question: What is the psychological impact of orthognathic surgery on patients with dentofacial deformities undergoing orthodontic-surgical treatment?
Methods
This systematic review was developed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Checklist (PRISMA) [12].
Eligibility criteria
To consider the eligibility of studies to be included/excluded in this review, “PICOS” was used:
- Population (P):
-
Patients with dentofacial deformities;
- Intervention (I):
-
Carrying out orthodontic-surgical treatment;
- Comparison (C):
-
Comparison of the moment before surgery (baseline) with the moment after surgery, or a control group without dentofacial deformity;
- Outcomes (O):
-
Psychosocial aspects assessed using a validated psychometric scale;
- Studies design (S):
-
Randomized clinical studies, pseudo-randomized, non-randomized, observational cohort, or cross-sectional studies.
Inclusion criteria
Studies whose objective was to evaluate psychological aspects through validated questionnaires applied before and after orthodontic-surgical treatment in patients with dentofacial deformities (longitudinal assessment) were included. Studies that evaluated patients undergoing orthodontic-surgical treatment, comparing them to a control group of patients with good facial harmony (cross-sectional assessment) were also included. There was no restriction on age, language, and time of publication. Cross-sectional, cohort, case–control, randomized clinical trials, pseudo-randomized, or non-randomized studies were included.
Exclusion criteria
The following exclusion criteria were applied: 1) reviews, letters, posters, conference abstracts, case reports, expert opinions, and articles that were not available for full reading were excluded; 2) works applying psychological questionnaires only before or only after orthognathic surgery; 3) studies that applied questionnaires without validation or those developed by the authors themselves; 4) studies that evaluated patients with syndromes or diseases associated with craniofacial anomalies, orofacial neoplasms, patients with cleft lip/palate (only in the lip or palate), or patients who did not undergo orthognathic surgery; 5) Patients being treated for sleep apnea; 6) orthodontic-surgical treatments in the “surgery-first” modality (orthognathic surgery without preoperative orthodontic preparation) or when combined with other specialties, except for orthodontics.
Information sources and search strategy
Detailed and tailored individual search strategies were developed for each of the following bibliographic databases: American and Caribbean Center on Health Sciences (LILACS), Cochrane Library, Embase, Psychinfo, PubMed/Medline, Scopus, and Web of Science. A gray literature search was performed using Google Scholar, OpenGrey, ProQuest and medRxiv. The search was carried out on February 8, 2020, in all databases and updated on March 17, 2021. The list of references cited in the articles included was also verified and an expert in the field was consulted about any publication relevant to this study.
Appropriate combinations of truncation and words were done and adapted for each database query (online resource 1). All references were managed by the appropriate reference software (EndNote® Web—Thomson Reuters, Philadelphia, PA), and duplicates were removed.
Selection process
The selection was carried out in two phases. In phase 1, two reviewers (I.B.B. and C.M.A.) independently and blindly reviewed the titles and abstracts of all citations collected from identified electronic databases. Articles that did not meet the inclusion criteria were discarded. In phase 2, the same reviewers applied the eligibility criteria to the full text of the articles. The reference list of selected studies was critically evaluated by both examiners (I.B.B. and C.M.A.).
To facilitate independent reading in both phases, the Rayyan website (http://rayyan.qcri.org) was used. Reviewers were blinded in all evaluations, and a third team member (O.G.F.) acted as moderator [13]. In addition, to ensure a correct calibration between both reviewers, the calculation of the Kappa coefficient of agreement was performed, and the reading started only when the agreement value was > 0.7, indicating a good agreement.
Data collection process
Two authors (I.B.B. and A.A.M.) collected information from the selected articles, such as study characteristics (author, year of publication, country, and study design), population characteristics (total number, total sample, number of cases and control, gender, age), Angle’s classification of malocclusion, questionnaires evaluating psychological aspects, results, and conclusions. Any disagreements were excluded through discussion and mutual agreement between reviewers. When the two authors did not reach a consensus, a third reviewer (O.G.F.) intervened to make the final decision.
If any data were missing or incomplete in the article, attempts were made to contact the authors to obtain pertinent unpublished information. Three attempts were made to contact the first author, the corresponding author, and the last author of the article, and the time interval between attempts was one week. In case of no response, the article was excluded with due justification.
Data items
The mean scores for each validated questionnaire were extracted from the studies included considering the time of assessment during the treatment. To increase the reliability of the extracted measures, only scores originating from psychometric instruments and validated in the literature were accepted.
Assessment of risk of bias
The risk of bias was assessed separately by three reviewers (I.B.B., A.A.M., and F.M.G.) using the Joanna Briggs Institute Critical Assessment Checklist [14], specific to the design of the studies included. The included articles were judged as “high risk,” “moderate risk,” and “low risk” when the domains with “yes” answers represented 0–49%, 50–69%, 70% or more, respectively, of the other domains. A meeting with the three reviewers solved any disagreements. A fourth reviewer (K.V.M.T) contributed if necessary.
Effect measures
When the results were presented on the same scale, the difference between the means (MD) of scores was calculated by comparing the two groups (baseline and post-intervention).
Conversely, if the measurements were in different scales, even if using the same questionnaire, the standardized difference between means (SMD) was used as a summary measure (Hedges’s g). SMD values of 0.2–0.5 were considered small, values of 0.5–0.8 were considered medium, and values > 0.8 were considered large effect size[15].
Synthesis method
To calculate the estimates of interest, random effects meta-analyses were performed, weighted by the inverse variance method using the DerSimonian and Laird estimator to estimate the variance by the value of Tau2. The Higgins inconsistency index was used to calculate heterogeneity (I2) [16]. To analyze the influence of heterogeneity on the interval estimates of the analyses, 95% prediction intervals (PI95%) were calculated for the estimated global effect.
The summary effect estimate was calculated through the mean difference between the moments of interest (baseline and post-intervention) and the measurements of MD and SMD. Sensitivity analyses were performed when a study classified as with a high risk of bias was included, or when there was the inclusion of a cross-sectional study, even evaluating a sample of pre-surgical and post-surgical patients, to see if there was a change in the effect size due to the inclusion of different study designs. As the randomization process did not influence the estimate (only performed pre and post-surgery evaluation—patients as their own control), sensitivity analysis was not necessary for these cases. Possible confounding factors, were evaluated by meta-regression with random effect models to verify whether the variance in the observed effect estimates was explained by these covariables, generating a bubble plot graph for the analysis. The significance level adopted was 5%, and the Forest Plots graphs were generated by the statistical software R, version 1.2.1335 (Rstudio Inc, Boston, USA) and Stata version 16.0 (Stata Corp LLC, College Station, USA).
Reporting bias assessment
In the impossibility of performing an evaluation using the funnel graph (n < 10) to reduce the probability of occurrence of publication bias, a broad search was carried out in several databases, including a database in a language other than English (LILACS), and in gray literature.
Certainty of evidence
The level of evidence was evaluated using the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) [17]. It grades the quality of evidence in four levels: very low, low, moderate, and high. ‘‘High quality’’ suggests that the actual effect lies close to the estimate of the effect. ‘‘Very low quality’’ suggests that there is very little confidence in the effect estimate, and the estimate reported can be substantially different from what was measured. This tool considers five aspects for rating the quality of evidence [18].
Results
Study selection
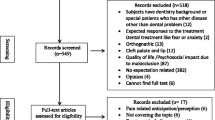
In Phase 1, 6751 references were found in all searches. After duplicates were removed, 4967 articles remained for screening of titles and abstracts. After screening, both reviewers selected 84 references to proceed to phase 2. After applying the eligibility criteria on full text reading, 49 further articles were excluded (online resource 2). After performing a search update, the authors included one more article. In addition, they included a thesis found in gray literature. Thus, 37 studies remained in the final qualitative synthesis (online resource 3). Figure 1 shows a flowchart of the identification process, inclusion, and exclusion of studies.
Study characteristics
Most studies included in the analysis were observational studies (no intervention control); nine were cross-sectional, one was a case control, and nineteen were cohort studies. In addition, five studies had a mixed design (cross-sectional and longitudinal assessment). Three studies were randomized controlled trials. Of all the included studies, only six included studies performed in a cross-sectional assessment, comparing scores of individuals before surgery with control groups with good facial harmony, to demonstrate the psychosocial impact of the deformity before correction with orthodontic-surgical treatment [19,20,21,22,23,24]. All other studies compared scores in a pre-surgical time with a post-surgical or post-treatment time.
The studies were published between 1982 and 2021 and conducted in the following countries: Austria, Brazil, China, Croatia, Denmark, Finland, France, Italy, Japan, Jordan, South Korea, Taiwan, Turkey, USA, and UK.
The study sample ranged from 29 to 1196 patients, and ages ranged from 11 years at the beginning of orthodontic treatment to 69 years. The most used questionnaires to assess psychological aspects in orthodontic-surgical patients were Symptom Checklist-90-Revised (SCL-90-R), Minnesota Multiphasic Personality Inventory (MMPI), The General Health Questionnaire-28 (GHQ-28), and Rosenberg Self-esteem Scale (RSES). Online resource 3 presents the characteristics of the studies included in the synthesis.
Risk of bias
Among the 37 studies included, three articles were classified as with a high risk of bias, eighteen as having a moderate risk, and the others as low risk of bias. The domains with the greatest number of methodological flaws were related to the control of confounding factors and strategies to deal with them, and the absence of a description of the complete follow-up in longitudinal studies. The randomized clinical trials included in the analysis were classified as having a low risk of bias, but none of them cited adequate blinding strategies (Fig. 2 and online resource 4).
Of the studies included in the meta-analysis, only one study had a high risk of bias.
Results of individual studies
All patients who sought orthodontic-surgical treatment reported aesthetic or functional complaints or followed the recommendation of professionals in the area. The main motivation of orthognathic surgery was due to facial aesthetics and functional objectives. Some psychological changes may be related to dentofacial deformities, significantly improving the results obtained after surgical treatment [19, 21, 25,26,27,28,29,30,31]. Psychological support throughout the treatment was also reported as a facilitator to achieve aesthetic and functional success [32].
Finlay P.M. et al. (1995) showed that most patients were motivated by aesthetics, and only 31% by impaired orofacial function [28]. Alanko, O.M. et al. (2014) observed that 15% of the sample of patients who sought orthognathic surgery were bullied, and 23 to 57% of their sample had some significant psychiatric symptom during their daily lives [19].
Self-esteem has a tendency to decrease at the beginning of orthodontic treatment, remaining low up to six months after surgery [33]. After this period, compared to patients who did not undergo surgical treatment, self-esteem is significantly higher [28, 34, 35]. Class III patients showed a greater insecurity regarding appearance, sensitivity to criticism, greater anxiety, and lower self-esteem in the pre-surgical period [34, 36,37,38].
After undergoing orthognathic surgery, at least one subscale, such as self-confidence, social interaction, facial body image, depression, or anxiety, was significantly higher than that of patients in the control group without orthognathic surgery, even though they had some functional problem, such as paresthesia after the surgery [19, 21, 23, 25, 27, 30, 31, 33,34,35, 37, 39,40,41,42,43,44,45,46]. There was disagreement in the literature when evaluating self-esteem in individuals with the skeletal discrepancy in the pre- and post-treatment moments or in a control group with good facial harmony. Studies showed improvement in self-esteem or no statistical difference [19, 33, 40, 47, 48]. Pain, paresthesia, post-surgical discomfort, and functional problems were predictors of emotional issues related to self-esteem in the post-surgery period; however, there was a decrease over time [49, 50].
Some studies show that the greater the severity of skeletal discrepancy, the higher the score for depression [40, 51,52,53]. As for symptoms of depression, Brunault, P. et al. (2016) demonstrated that demographic factors do not directly influence the results for depression among men and women or marital status, but the highest score obtained for depression was associated with the length of treatment and the type of orofacial deformity [52]. Also, there was a decrease in these psychological symptoms after an average time of 12 months after surgery [52, 54].
Younger patients (21–34 years) showed more psychological problems, while older patients showed more physiological complaints. They are associated with poor post-surgical results [55]. On the other hand, a study by Brunault, P. et al. (2016) found no significant age-related effects [52].
Hatch, JP. et al. (1997) suggested that psychosocial changes remain stable in surgical groups immediately after surgery, and that after an average time of 2 years they tend to decrease, reaching a lower level than in the pre-operative period. This shows that there is no relationship between psychological function before surgery and satisfaction with the treatment results [37]. In this same line of study, Motegi, E. et al. (2003) demonstrates that from 2 to 5 years after surgery psychological changes are not significant, as well as immediately after surgery [56].
Orthognathic patients had significantly higher levels of social anxiety than the general population [57]. Gender was a significant factor associated with anxiety. Overall, women showed a greater anxiety than men [52, 53]. Self-reporting regarding the personality of surgical patients improved compared to the preoperative period in relation to some disorders such as depression, anxiety, psychoticism, obsessive–compulsive symptoms, and interpersonal sensitivity, in addition to improving self-identity, self-satisfaction, and social conflicts [39, 58, 59].
Synthesis of results
Thirteen studies were included in the quantitative synthesis. It was possible to meta-analyze data from the following questionnaires: GHQ-28, MMPI, RSES, and SCL-90-R.
When the scores for the domains somatic symptoms, anxiety/insomnia, social dysfunction, and severe depression were evaluated, the only domain of the GHQ-28 questionnaire to show a statistical significance (p < 0.05) was that related to severe depression: there was a decrease in means by -0.82 when comparing the time before orthognathic surgery and six-12 months after surgery [CI95% = -1.35 – -0.28; I2 = 0%], indicating a slight improvement in mental health regarding aspects related to depression in six to 12 months after surgery (Fig. 3). There was no statistical significance for the overall effect for this questionnaire. These results were the same even with the performance of a sensitivity analysis, excluding the study classified as a high risk of bias or cross-sectional design (online resource 5).
When evaluating the personality of these individuals through the MMPI questionnaire, no domains when evaluated in isolation, showed statistically significant difference (p > 0.05). When considering the overall effect, there was a mean decrease of -1.30 in scores of individuals over a period of six months after surgery (MD = -1.30; CI95% = -2.18–-0.42; I2 = 52%) (Fig. 4). However, the prediction interval includes the null difference value, thus denoting low robustness of these results [PI95% = -3.71–1.11].
When assessing the self-esteem of patients undergoing orthodontic-surgical treatment compared to individuals with a normal face or already treated, there was a significant increase in self-esteem scores according to the Rosenberg scale [SMD = 0.56; CI95% = 0.25–0.88] (Fig. 5), reflecting an improvement in the individual’s self-image, with a moderate effect size. Despite the low heterogeneity between the effects of the included studies (I2 = 34%), the small number of included studies made the analysis present a wide prediction range [PI95% = -0.27–1.40], denoting a low robustness of these findings. For the SCL-90-R questionnaire, seven of the nine domains showed a statistically significant improvement for psychological symptoms related to obsessive-compulsiveness [SMD = -0.30; CI95% = -0.57–-0.04; I2 = 32%], interpersonal sensitivity [SMD = -0.71; CI95% = -0.98–-0.44; I2 = 32%], depression [SMD = -0.56; CI95% = -0.77–-0.35; I2 = 0%], anxiety [SMD = -0.42; CI95% = -0.64–-0.20; I2 = 6%], phobic anxiety [SMD = -0.46; CI95% = -0.78–-0.13; I2 = 53%], paranoid ideation [SMD = -0.43; CI95% = -0.74–-0.11; I2 = 51%], and psychoticism [SMD = -0.37; CI95% = -0.57–-0.16; I2 = 0%]. It was also possible to observe a decrease in the overall effect [SMD = -0.42; CI95% = -0.51–-0.33; I2 = 34%], thus evidencing a decrease in the psychopathological symptoms of these individuals when undergoing orthodontic-surgical treatment to correct the dentofacial deformity. The domains related to somatization and hostility were not statistically significant (Fig. 6).
When the scores for the depression domain of the different questionnaires were standardized by the same effect size (Hedges’s g), it was possible to see a significant improvement in this outcome for individuals undergoing orthodontic-surgical treatment [SMD = -0.28; CI95% = -0.38–-0.18; p < 0.05] (Fig. 7a). The postoperative time covariate proved to be a significant predictor, explaining 100% of the heterogeneity observed in the analysis [R2 = 100%; p = 0.034], showing a decrease in scores related to depression as the postoperative time passes. (Fig. 7b).
Confidence in cumulative evidence
The certainty of the evidence assessed by the GRADE tool was considered very low. The main factors for the decrease in the certainty of the evidence generated were the methodological limitations, generating a potential risk of bias, inconsistency (presence of uncontrolled confounding factors, generating statistical heterogeneity), and imprecision (wide prediction interval generated by the existing heterogeneity or by the low number of studies) (online resource 6).
Discussion
This systematic review and meta-analysis analyzed the psychological aspects of patients with skeletal facial deformities undergoing orthodontic-surgical treatment. The search for this type of treatment occurs mostly for aesthetic reasons, corresponding to 52% of the cases, while only 31% seek treatment due to functional reasons [28]. The included studies that evaluated the psychological aspects before and after treatment found a high frequency of depression, anxiety, and self-esteem scores as the main changes that affect these patients when undergoing treatment.
The depressive state may directly influence the quality of life of individuals with dentofacial deformities, significantly interfering in the vitality, mental health, and social aspects of these individuals [60]. Orthognathic patients with severe dentofacial deformity may be more likely to suffer psychological distress and even depression [61]. In the present review, the domain related to depression showed a statistically significant difference, denoting a decrease in the depressive state of these patients. General health and quality of life are affected in orthognathic patients [60], and the correction of these aspects can be an explanation for the improvement in the depressive state of these patients.
Treatments that involve cosmetic aspects in addition to functional aspects are closely related to psychological well-being. Patients who seek cosmetic surgery often show high levels of anxiety [62]. The psychological assessment obtained by the SCL-90-R questionnaire showed improvement in two domains related to anxiety levels, indicating that the orthodontic-surgical treatment positively affects the psychosocial state. Orthognathic patients may be at an increased risk of social anxiety disorder regardless of age, gender, or severity of deformity [57]. Taking into account the stress generated in the pre-surgical orthodontic treatment stage, it is necessary to carry out an assessment of prior anxiety. The main complaints reported in the initial consultation should be considered. After the treatment, it is essential to follow the evolution of patients to monitor any problems and/or dissatisfaction in the postoperative period [38], thus providing a more structured future follow-up [29, 52, 56].
Patients with dentofacial deformity and Class III malocclusion show a significant decrease in self-esteem compared to individuals without dentofacial deformation [34]. According to Araujo, C.M. et al. [63], after an average of four months after surgery, there is an evident increase in quality of life in domains related to facial esthetics and function. The summary of results of the studies included showed a significant increase in self-esteem after orthodontic-surgical treatment. It was equivalent to that of patients in the control group at the initial time of studies [33, 40]. Characteristics such as gender, age, and severity of malocclusion were factors that could affect the results obtained in these patients. Changes in aesthetic aspects may explain our findings, as aesthetics are improved. This might have influenced the increase in these patients' self-esteem scores. In addition, after correction of dentofacial deformity, sensitivity to criticism and social appearance anxiety tend to decrease in these individuals [34]. However, despite the low heterogeneity of studies in the scientific literature on the subject, there is a need for more studies that assess this outcome to increase its robustness.
There is evidence that psychological problems may be correlated with different types of dentofacial deformities [36, 38, 40]. In general, patients with Class III malocclusion tend to have a greater insecurity, depression, and psychological stress compared to other types of malocclusion [36], as it is more difficult to disguise skeletal discrepancy due to the protrusion of the jaw and concavity of the facial profile, which is considered less attractive [38, 40]. According to Gerzanic, L. et al., patients with Class III malocclusion undergo orthognathic surgery approximately 4 years earlier than in other deformities, reaffirming that there are psychological reasons that affect the decision to undergo surgical correction [36]. Gender was one of the factors associated with changes in emotional behavior, depression, and self-esteem. Females experience the most dramatic changes with the change in the facial profile [33, 36, 44, 52, 56]. Age can also be a determining factor. Younger individuals were the most likely to have some psychiatric disorders and emotional difficulties as they are in a stage of development and construction of an identity where a negative body image may cause vulnerability [29]. The lack of control of these confounding factors in the studies included decreased the degree of certainty of the evidence generated by this synthesis according to the GRADE tool. In the present review, the only possible outcome to be analyzed through a regression analysis was the time of postoperative evaluation, showing to be a significant predictor for this outcome.
After analyzing the studies included in this systematic review, the importance of psychological assessment of the patient prior to orthodontic-surgical treatment is evident in order to observe the psychological characteristics and align aesthetic with functional expectations in the final surgical result.
Limitations
The certainty of evidence assessed by the GRADE tool resulted in low and very low certainty of evidence. The presence of several confounding factors inherent to the topic, such as age, gender, type of malocclusion, and patients’ expectations of orthodontic-surgical treatment, may affect the estimates generated, especially when they are not controlled by appropriate methods of sampling and randomization. Most of the analysis was based on uncontrolled observational studies, and thus there was no control of the exposure factor and also the impossibility of random allocation methods. These factors reduce the certainty of evidence and may have generated inaccuracy and inconsistency. Thus, based on the current literature on this subject, it is recommended to carry out randomized clinical studies with adequate sampling methods, controlling possible confounding factors.
Conclusion
Based on the results of this systematic review and meta-analysis, the evidence suggests an improvement in psychosocial aspects related to hysteria, self-esteem, anxiety, obsessive-compulsiveness, interpersonal sensitivity, paranoid ideas, psychoticism, and an improvement in the depressive state. The postoperative time being an important covariate for the improvement of scores related to the depressive state in these patients. This result highlights the importance of surgeons and orthodontists in promoting adequate control of patients’ expectations and treatment goals taking into account the individual's psychological aspects.
Other information
The protocol for this systematic review was registered in the International Prospective Register of Systematic Reviews (PROSPERO) under no. CRD42021228447.
References
Denadai R, Chou PY, Su YY, Lo CC, Lin HH, Ho CT, Lo LJ (2019) Facial Appearance and Psychosocial Features in Orthognathic Surgery: A FACE-Q- and 3D Facial Image-Based Comparative Study of Patient-, Clinician-, and Lay-Observer-Reported Outcomes. J Clin Med 8:909. https://doi.org/10.3390/jcm8060909
Zamboni R, de Moura FRR, Brew MC, Rivaldo EG, Braz MA, Grossmann E, Bavaresco CS (2019) Impacts of Orthognathic Surgery on Patient Satisfaction, Overall Quality of Life, and Oral Health-Related Quality of Life: A Systematic Literature Review. Int J Dent 2019:2864216. https://doi.org/10.1155/2019/2864216
Palomares NB, Celeste RK, Miguel JA (2016) Impact of orthosurgical treatment phases on oral health-related quality of life. Am J Orthod Dentofacial Orthop 149:171–181. https://doi.org/10.1016/j.ajodo.2015.07.032
Su YY, Denadai R, Ho CT, Lai BR, Lo LJ (2020) Measuring patient-reported outcomes in orthognathic surgery: Linguistic and psychometric validation of the Mandarin Chinese version of FACE-Q instrument. Biomed J 43:62–73. https://doi.org/10.1016/j.bj.2019.05.011
Larsson P, Bondemark L, Haggman-Henrikson B (2021) The impact of oro-facial appearance on oral health-related quality of life: A systematic review. J Oral Rehabil 48:271–281. https://doi.org/10.1111/joor.12965
Brucoli M, Baena RRY, Boffano P, Benech A (2019) Psychological profiles in patients undergoing orthognathic surgery or rhinoplasty: a preoperative and preliminary comparison. Oral Maxillofac Surg 23:179–186. https://doi.org/10.1007/s10006-019-00758-1
Cunha HS, da Costa Moraes CA, de Faria VDR, da Rosa ELS (2020) Accuracy of three-dimensional virtual simulation of the soft tissues of the face in OrtogOnBlender for correction of class II dentofacial deformities: an uncontrolled experimental case-series study. Oral Maxillofac Surg 25:319–335. https://doi.org/10.1007/s10006-020-00920-0
Alanko OM, Svedstrom-Oristo AL, Tuomisto MT (2010) Patients’ perceptions of orthognathic treatment, well-being, and psychological or psychiatric status: a systematic review. Acta Odontol Scand 68:249–260. https://doi.org/10.3109/00016357.2010.494618
Broers DLM, van der Heijden G, Rozema FR, de Jongh A (2017) Do patients benefit from orthognathic surgery? A systematic review on the effects of elective orthognathic surgery on psychosocial functioning and patient satisfaction. Eur J Oral Sci 125:411–418. https://doi.org/10.1111/eos.12371
Hunt OT, Johnston CD, Hepper PG, Burden DJ (2001) The psychosocial impact of orthognathic surgery: a systematic review. Am J Orthod Dentofacial Orthop 120:490–497. https://doi.org/10.1067/mod.2001.118402
Brignardello-Petersen R (2018) No evidence about the effects of orthognathic surgery in psychosocial functioning owing to limitations in the systematic review. J Am Dental Assoc 149:e21. https://doi.org/10.1016/j.adaj.2017.09.047
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hrobjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71. https://doi.org/10.1136/bmj.n71
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A (2016) Rayyan-a web and mobile app for systematic reviews. Syst Rev 5:210. https://doi.org/10.1186/s13643-016-0384-4
Institute TJB (2014) Joanna Briggs Institute Reviewers' Manual. The Joanna Briggs Institute, Australia
Andrade C (2020) Mean Difference, Standardized Mean Difference (SMD), and Their Use in Meta-Analysis: As Simple as It Gets. J Clin Psychiatry 81:20f13681. https://doi.org/10.4088/JCP.20f13681
Higgins JP (2011) Cochrane handbook for systematic reviews of interventions. Version 5.1. 0 The Cochrane Collaboration.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, Schunemann HJ, Group GW (2008) GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 336:924–6. https://doi.org/10.1136/bmj.39489.470347.AD
Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, Norris S, Falck-Ytter Y, Glasziou P, DeBeer H, Jaeschke R, Rind D, Meerpohl J, Dahm P, Schunemann HJ (2011) GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol 64:383–394. https://doi.org/10.1016/j.jclinepi.2010.04.026
Alanko OM, Svedstrom-Oristo AL, Peltomaki T, Kauko T, Tuomisto MT (2014) Psychosocial well-being of prospective orthognathic-surgical patients. Acta Odontol Scand 72:887–897. https://doi.org/10.3109/00016357.2014.920107
Burden DJ, Hunt O, Johnston CD, Stevenson M, O’Neill C, Hepper P (2010) Psychological status of patients referred for orthognathic correction of skeletal II and III discrepancies. Angle Orthod 80:43–48. https://doi.org/10.2319/022709-114.1
Lee L, Chen SH, Yu CC, Lo LJ, Lee SR, Chen YR (2007) Stigma, body image, and quality of life in women seeking orthognathic surgery. Plast Reconstr Surg 120:225–231. https://doi.org/10.1097/01.prs.0000264100.57630.c7
Ryan FS, Moles DR, Shute JT, Clarke A, Cunningham SJ (2016) Social anxiety in orthognathic patients. Int J Oral Maxillofac Surg 45:19–25. https://doi.org/10.1016/j.ijom.2015.05.021
Williams DM, Bentley R, Cobourne MT, Gibilaro A, Good S, Huppa C, Matthews NS, O’Higgins E, Patel S, Newton JT (2009) Psychological characteristics of women who require orthognathic surgery: comparison with untreated controls. Br J Oral Maxillofac Surg 47:191–195. https://doi.org/10.1016/j.bjoms.2008.07.187
Yao S, Zhou J, Li ZB (2014) Psychologic Health Status of Patients Undergoing Orthognathic Surgery. Journal of Craniofacial Surgery 25:E540–E543. https://doi.org/10.1097/SCS.0000000000001042
Gobic BM, Kralj M, Harmicar D, Cerovic R, Mady Maricic B, Spalj S (2021) Dentofacial deformity and orthognatic surgery: Influence on self-esteem and aspects of quality of life. J Craniomaxillofac Surg 49:277–281. https://doi.org/10.1016/j.jcms.2021.01.024
Al-Bitar ZB, Al-Ahmad HT (2017) Anxiety and post-traumatic stress symptoms in orthognathic surgery patients. Eur J Orthod 39:92–97. https://doi.org/10.1093/ejo/cjw029
Auerbach SM et al (1984) Psychological factors in adjustment to orthognathic surgery. J Oral Maxillofac Surg 42:435–440
Finlay PM, Moos SF, Atkinson JM (1995) Orthognathic surgery: patient expectations; psychological profile and satisfaction with outcome. Brit J Oral Maxillofac Surg 33:9–14
Kim SJ, Kim MR, Shin SW, Chun YS, Kim EJ (2009) Evaluation on the psychosocial status of orthognathic surgery patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 108:828–832. https://doi.org/10.1016/j.tripleo.2009.07.044
Lazaridou-Terzoudi T, Kiyak HA, Moore R, Athanasiou AE, Melsen B (2003) Long-term assessment of psychologic outcomes of orthognathic surgery. J Oral Maxillofac Surg 61:545–552. https://doi.org/10.1053/joms.2003.50107
Oland J, Jensen J, Elklit A, Melsen B (2011) Motives for surgical-orthodontic treatment and effect of treatment on psychosocial well-being and satisfaction: a prospective study of 118 patients. J Oral Maxillofac Surg 69:104–113. https://doi.org/10.1016/j.joms.2010.06.203
Suen KS, Lai Y, Ho SMY, Cheung LK, Choi WS (2018) A longitudinal evaluation of psychosocial changes throughout orthognathic surgery. PLoS ONE 13:e0203883. https://doi.org/10.1371/journal.pone.0203883
Alanko O, Tuomisto MT, Peltomaki T, Tolvanen M, Soukka T, Svedstrom-Oristo AL (2017) A longitudinal study of changes in psychosocial well-being during orthognathic treatment. Int J Oral Maxillofac Surg 46:1380–1386. https://doi.org/10.1016/j.ijom.2017.05.004
Agirnasligil MO, Gul Amuk N, Kilic E, Kutuk N, Demirbas AE, Alkan A (2019) The changes of self-esteem, sensitivity to criticism, and social appearance anxiety in orthognathic surgery patients: A controlled study. Am J Orthod Dentofacial Orthop 155:482-489 e2. https://doi.org/10.1016/j.ajodo.2018.05.019
Guimarães FR, Oliveira EC, Gomes TR, Souza TD (2014) Quality of life in patients who undergo orthognathic surgery: oral health and self-esteem. Psicologia: Ciência e Profissão 34:242–251
Gerzanic L, Jagsh R, Watzke IM (2002) Psychologic implications of orthognathic surgery in patients with skeletal Class II or Class III malocclusion. Int J Adult Orthod Orthognath Surg 17:75–81
Hatch JPRJ, Bays RA, Van Sickels JE, Keeling SD, Clark GM (1999) Psychological function in orthognathic surgical patients before and after bilateral sagittal split osteotomy with rigid and wire fixation. Am J Orthod Dentofac Orthop 115:536–543
Takatsuji H, Kobayashi T, Kojima T, Hasebe D, Izumi N, Saito I, Saito C (2015) Effects of orthognathic surgery on psychological status of patients with jaw deformities. Int J Oral Maxillofac Surg 44:1125–1130. https://doi.org/10.1016/j.ijom.2015.02.003
Flanary CM (1990) Impact of orthognathic surgery on normal and abnormal personality dimensions: a 2-year follow-up study of 61 patients. Am J Orthodont Dentofac Orthoped 98:313–322
Jung MH (2016) Quality of Life and Self-Esteem of Female Orthognathic Surgery Patients. J Oral Maxillofac Surg 74(1240):e1-7. https://doi.org/10.1016/j.joms.2016.01.046
Kiyak HA, Hohl T, West RA, McNeill RW (1984) Psychologic changes in orthognathic surgery patients: a 24-month follow up. J Oral Maxillofac Surg 42:506–512. https://doi.org/10.1016/0278-2391(84)90009-0
Kiyak HAV, P.P., Crinean, J. (1988) Patients’ Expectations as Predictors of Orthognathic Surgery Outcomes. Health Psychol 7:251–268
Kiyak HA, West RA, Hohi T, McNeill RW (1982) The psychological impact of orthognathic surgery: A g-month follow-up. Am J Orthod 81:404–412
Nicodemo D, Peirera MD, Ferreira LM (2008) Self-esteem and depression in patients presenting angle class III malocclusion submitted for orthognathic surgery. Med Oral Patol Oral Cir Bucal 13:48–51
Sar C, Soydan SS, Ozcirpici AA, Uckan S (2015) Psychosocial and functional outcomes of orthognathic surgery: Comparison with untreated controls. J Oral Maxillofac Surg Med Pathol 27:451–457. https://doi.org/10.1016/j.ajoms.2014.03.001
Yao S, Zhou J, Li Z (2014) Psychologic health status of patients undergoing orthognathic surgery. J Craniofac Surg 25:e540–e543. https://doi.org/10.1097/SCS.0000000000001042
Belusic Gobic M, Kralj M, Harmicar D, Cerovic R, Mady Maricic B, Spalj S (2021) Dentofacial deformity and orthognatic surgery: Influence on self-esteem and aspects of quality of life. J Craniomaxillofac Surg 49:277–281. https://doi.org/10.1016/j.jcms.2021.01.024
Cunningham SJ, Hunt NP, Feinmann C (1996) Perceptions of outcome following orthognathic surgery. Br J Oral Maxillofac Surg 34:210–213. https://doi.org/10.1016/s0266-4356(96)90271-5
Kiyak HA, McNeill RW, West RA, Hohl T, Bucher F, Sherrick P (1982) Predicting psychologic responses to orthognathic surgery. J Oral Maxillofac Surg 40:150–155. https://doi.org/10.1016/0278-2391(82)90046-5
Kiyak HA, Mcneill RW, West RA (1985) The emotional impact of orthognathic surgery and conventional orthodontics. Am J Orthodont Dentofac Orthoped 88:224–234
Burden DJHO, Johnston CD, Stevenson M, O’Neill C, Hepper P (2010) Psychological status of patients referred for orthognathic correction of skeletal II and III discrepancies. Angle Orthod 80:43–48. https://doi.org/10.2139/022709-114.1
Brunault P, Battini J, Potard C, Jonas C, Zagala-Bouquillon B, Chabut A, Mercier JM, Bedhet N, Réveillère C, Goga D, Courtois R (2016) Orthognathic surgery improves quality of life and depression, but not anxiety, and patients with higher preoperative depression scores improve less. Int J Oral Maxillofac Surg 45:26–34. https://doi.org/10.1016/j.ijom.2015.07.020
Battini J (2013) Impact psychologique des interventions en chirurgie orthognathique. Université François - Rabelais de Tours.
Brucoli M, Zeppegno P, Benech R, Boffano P, Benech A (2019) Psychodynamic Features Associated With Orthognathic Surgery: A Comparison Between Conventional Orthognathic Treatment and “Surgery-First” Approach. J Oral Maxillofac Surg 77:157–163. https://doi.org/10.1016/j.joms.2018.06.005
Scott AA et al (1999) Psychosocial predictors of high-risk patients undergoing orthognathic surgery. Int J Adult Orthodont Orthognathic Surg 14:113–124
Motegi E, Hatch JP, Rugh JD, Yamaguchi H (2003) Health-related quality of life and psychosocial function 5 years after orthognathic surgery. Am J Orthod Dentofac Orthop 124:138–143. https://doi.org/10.1016/s0889-5406(03)00391-3
Ryan FS, Moles DR, Shute JT, Clarke A, Cunningham SJ (2016) Social Anxiety in Orthognathic Patients. Int J Oral Maxillofac Surg 45:19–25
Li XR, Chen LQ, Li YL, Sun J (2015) The change of patients’ psychosomatic symptoms after orthognathic surgery. Shanghai Kou Qiang Yi Xue 24:107–110
Lovius BBJ, Jones RB et al (1990) The specific psychosocial effects of orthognathic surgery. J Cranio-Maxillofac Surg 18:339–342
de Avila ED, de Molon RS, Loffredo LC, Massucato EM, Hochuli-Vieira E (2013) Health-related quality of life and depression in patients with dentofacial deformity. Oral Maxillofac Surg 17:187–191. https://doi.org/10.1007/s10006-012-0338-5
Kovalenko A, Slabkovskaya A, Drobysheva N, Persin L, Drobyshev A, Maddalone M (2012) The association between the psychological status and the severity of facial deformity in orthognathic patients. Angle Orthod 82:396–402. https://doi.org/10.2319/060211-363.1
Qian H, Ling Y, Wang C, Lenahan C, Zhang M, Zheng M, Shao A (2021) A Correlative Study Between Personality Traits and the Preference of Site Selection in Cosmetic Treatment. Front Psychiatry 12:648751. https://doi.org/10.3389/fpsyt.2021.648751
de Araujo CM, Schroder AGD, de Araujo BMM, Cavalcante-Leao BL, Stechman-Neto J, Zeigelboim BS, Santos RS, Guariza-Filho O (2020) Impact of orthodontic-surgical treatment on quality of life: a meta-analysis. Eur J Orthod 42:281–289. https://doi.org/10.1093/ejo/cjz093
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Basso, I., Gonçalves, F., Martins, A. et al. Psychosocial changes in patients submitted to orthodontic surgery treatment: a systematic review and meta-analysis. Clin Oral Invest 26, 2237–2251 (2022). https://doi.org/10.1007/s00784-021-04304-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-021-04304-w