Abstract
Objective
The aim of the present study was to evaluate the in vitro biocompatibility of Theracal PT, Theracal LC, and MTA Angelus, considered as bioactive materials used for vital pulp treatment, on human dental pulp stem cells (hDPSCs).
Materials and methods
Human dental pulp stem cells (hDPSCs) were isolated from third molars, and material eluates were prepared (undiluted, 1:2, and 1:4 ratios). The hDPSC cytotoxicity, adhesion, morphology, viability, and cell migration were assessed. The mineralization nodule formation was determined by Alizarin red S staining (ARS). The odonto/osteogenic differentiation potential was assessed by osteo/odontogenic marker expression real-time qPCR. The chemical composition and ion release of the vital pulp materials were determined by energy dispersive X-ray (EDX) and inductively coupled plasma-mass spectrometry (ICP-MS), respectively. Statistical differences were assessed by ANOVA and Tukey’s test (p < 0.05).
Results
The three vital pulp materials showed variable levels of calcium, tungsten, silicon, and zirconium release and in their chemical composition. Cytocompatibility assays revealed higher hDPSC viability and migration rates when treated with Theracal PT than with Theracal LC. The lowest cell adhesion and spreading were observed in all Theracal LC-treated groups, whereas the highest were observed when treated with MTA. Theracal PT and MTA promoted the upregulation of DSPP and RUNX2 gene expression (p < 0.05). After 21 days, both MTA Angelus and Theracal PT–treated cells exhibited a significantly higher mineralized nodule formation than the negative control (p < 0.05).
Conclusions
This study demonstrates the favorable in vitro cytocompatibility and bioactive properties of the recently introduced Theracal PT and the well-established MTA Angelus on hDPSCs, as opposed to Theracal LC. More studies, including in vivo animal testing are suggested before these new formulations might be used in the clinical setting.
Clinical relevance
Theracal PT is a new material that could be clinically suitable for vital pulp therapy. Further studies considering its biocompatibility and bioactivity are necessary.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dental pulp cells can be exposed to a number of different potentially harmful stimuli, such as dental caries, trauma, or even iatrogenic factors; which can compromise their survival. The dentin-pulp complex presents a number of physiological defensive mechanisms, which are encompassed within the term reparative dentinogenesis [1, 2]. Thus, the maintenance of pulp vitality is the ultimate goal of biologically based minimally invasive therapeutic approaches. Within this framework, vital pulp treatment (VPT) has gained interest among daily dental practice, including procedures which range from indirect and direct pulp capping to partial and full pulpotomy [3,4,5].
Previous studies have reported the ability of human dental pulp stem cells (hDPSCs) to regenerate dentin, measured by the expression of odontogenic genes in vitro and/or dentin bridge formation in vivo in the process of dentinogenesis [6, 7]. Under favorable circumstances, hDPSCs are thought to differentiate into odontoblast-like cells and produce reparative dentin, which is the goal of VPT. However, the characteristics and extent of the tissue repair resulting from VPT depend on the clinical situation of the affected tooth and the type of materials used for vital pulp therapy. In fact, one of the ideal requirements of vital pulp materials is to induce and modulate the healing process and repair of the dentin-pulp complex [8, 9].
Traditionally, the material considered as the gold standard for the treatment of pulp exposures was calcium hydroxide, until studies demonstrated the superior clinical performance of calcium silicate-based materials, e.g., mineral trioxide aggregate (MTA) [1, 10]. Both materials have similar mechanisms of action, but calcium silicate–based cements induce the formation of a mineralized barrier with a higher uniformity and thickness, and elicit lower inflammatory responses and pulp tissue necrosis. Due to their favorable biological, physical, and mechanical properties, new versions of calcium silicate–based materials have been developed for their use as vital pulp materials [11]. These materials can enhance the process of mineralized-tissue formation by inducing the differentiation of precursor cells into mineral-secreting cells [12]. They also stimulate odontoblast-like differentiation and the secretion of growth factors and modulators of tissue repair [13].
Theracal LC (Bisco, Inc., Schamburg, IL, US) is a light-curable resin–modified tricalcium silicate–based material with easy handling, greater release of calcium ions compared to MTA and Dycal (Dentsply, York, PA, USA), but with controversial biological properties, which hinder its recommendation as pulp capping materials [14, 15]. Recently, Theracal PT (Bisco, Inc., Schamburg, IL, USA), a new dual-cured, resin-modified calcium silicate material designed for VPT, has been presented for clinical use. According to its manufacturer, this material maintains tooth vitality by acting as a barrier to protect the dentin-pulp complex. Due to its recent introduction to the market, to the authors’ knowledge, there are no studies regarding this material for VPT.
Studies assessing cytotoxicity act as the preliminary analysis of the biological responses of a variety of dental materials. The advantage of these studies is that they present a controlled design for the evaluation of different properties of the materials, while evaluating their possible health risks [16, 17].
Accordingly, this study aimed to evaluate the bioactivity and biological properties of Theracal PT, and to compare these properties to those of MTA (Angelus, Londrina, PR, Brazil) and Theracal LC. The null hypothesis was that there is no difference between the tested materials in relation to their cytocompatibility and bioactivity potential on hDPSCs.
Materials and methods
Preparation of vital pulp material extracts
MTA (Angelus, Londrina, PR, Brazil), Theracal LC (Bisco Inc., Schamburg, IL, USA) and Theracal PT (Bisco, Inc., Schamburg, IL, USA) were prepared following their respective manufacturers’ instructions into 5-mm diameter and 2-mm high sterile cylindrical rubber molds, sterilized under ultraviolet irradiation for 15 min and stored in an incubator at 37 °C, 5% CO2, and 95% humidity, for 48 h to achieve complete setting. TheraCal LC (Bisco) was light-cured with a LED curing light (Bluephase 20i, Ivoclar Vivadent, Schaan, Liechtenstein) at an output of 1200 mW/cm2 for 20 s with a 2-mm light-curing distance; the intensity of the light was measured using a Marc Resin Calibrator (BlueLight Analytics, Halifax, Canada). Their complete compositions are described in Table 1 obtained from the data sheet available at the respective manufacturers’ websites.
In accordance with the International Organization for Standardization (ISO), the eluates of the different materials were extracted in sterile conditions, using DMEM culture medium as an extraction vehicle. The extraction procedure was performed as follows: the materials were stored in the culture medium for 24 h at 37 °C in a humid atmosphere containing 5% CO2 with agitation. The ratio of material surface area to medium volume was set at approximately 3 cm2/mL in accordance with the guidelines of the International Organization for Standardization 10993-12 [18]. Finally, serial dilutions of the extraction medium were prepared at 1/1, 1/2, and 1/4 ratios [19].
Ion release of vital pulp material extracts
Specimens (n = 3) were prepared from each vital pulp material. The ion release of each material in deionized water (Milli-Q; Merck KGaA, Darmstadt, Germany) was analyzed using inductively coupled plasma-optical emission spectrometry (ICP-MS; Agilent 7900, Stockport, UK). The proportion of aluminium (Al), silicon (Si), sulfur (S), calcium (Ca), strontium (Sr), barium (Ba), and tungsten (W) released from each material was analyzed at 1 day in triplicate, and the elements were calibrated with pure deionized water.
Scanning electronic microscopy and energy-dispersive spectroscopy
Disks of each cell-free material (n = 9) were immersed in Ca2+/Mg2+-free Hank’s balance salt solution (HBSS; Gibco, Gaithersburg, MD, USA) at 3 cm2/mL and stored at 37 °C for 24 h. Once set, the disks underwent a carbon-coating process in a CC7650 SEM Carbon Coater unit (Quorum Technologies Ltd, East Sussex, UK). Then, the element distribution was analyzed using a scanning electron microscope with an energy-dispersive X-ray spectrometer (SEM-EDX, JSM-610LV; JEOL, Tokyo, Japan). A qualitative analysis was conducted for the surface element distribution.
Isolation and culture of hDPCs
Cells were obtained from impacted third molars (n = 10) from 10 healthy subjects (18–30 years old). The human dental pulp (hDP) isolation protocol was approved by the Human Research Ethics Committee from the University of Murcia (protocol ID: 2199/2018). hDP was obtained from the pulp chamber and root canals using a barber broaches. After extraction, hDP was thoroughly rinsed with HBSS, and subjected to collagenase-A digestion (3 mg/mL) (Sigma-Aldrich, St. Louis, MO, USA) for 1 h at 37 °C. Then, cells were maintained in Dulbecco’s Modified Eagle Medium (DMEM Gibco BRL, CA, USA) supplemented with 10% fetal bovine serum (FBS) (Gibco), 1% L-glutamine, 100-U/ml penicillin, and 100-μg/ml streptomycin (Gibco). Finally, cells were incubated at 37 °C in a 5% CO2 humidified atmosphere. For subsequent experiments, hDPCs were used from culture passage 2 up to 6.
Characterization of hDPSCs
Cultured cells were identified following the guidelines of the International Society of Cellular Therapy (ISCT) to confirm their mesenchymal stem cell phenotype [20]. The surface antigens of the hDPSCs were analyzed using antibodies conjugated to fluorophores under flow cytometry. The antibodies used were CD73-APC (clone AD2), CD90-FITC (clone DG3), CD105-PE (clone 43A4E1), CD34-PerCP (clone AC136), CD19-PerCP (clone LT20.B4), CD14-PerCP (clone TÜK4), and CD45-PerCP (clone 5B1) (Human MSC Phenotyping Cocktail, Miltenyi Biotec, Bergisch Gladbach, Germany). Flow cytometry analysis was performed using a FACS Calibur Flow cytometer (Becton Dickinson, Franklin Lakes, NJ, USA). Furthermore, hDPSCs were cultured in osteogenic, adipogenic and chondrogenic medium (Miltenyi Biotech) to evaluate the in vitro trilineage mesenchymal differentiation, as previously described [21].
Cytotoxicity assay
Cytotoxicity was assessed by analyzing the mitochondrial activity by means of a 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) assay. The extracts were placed in contact with the cell culture and cell metabolic activity was measured at 24 h, 48 h and 72 h of culture, as described by Sequeira et al. [22]. Cells cultured in growth medium w/o any extract were used as the negative control. According to the manufacturer's instructions, the MTT reagent (Sigma-Aldrich) was added to the wells for 4 h. When the purple precipitate was visibly noticeable, dimethylsulfoxide (DMSO) (Sigma-Aldrich) was added to solubilize the formazan dye (100 μl/well). Covered plates were kept in the dark for 2–4 h. Finally, the absorbance at 570-nm wavelength in each well was measured in a microplate reader (ELx800; Bio-Tek Instruments, Winooski, VT, USA). Each experimental condition was performed in triplicate and analyzed in three independent experiments.
Cell migration
Cell migration was evaluated using an in vitro wound healing assay. Cells were seeded onto 12-well plates (2 × 104 hDPSCs per well, n = 3 for each dilution) and left to proliferate until confluent. The culture medium was then replaced with serum-free culture medium and cultured for an additional 24 h. Then, a scratch was created using a sterilized-pipette tip and the cells were exposed to complete growth medium alone (control) or complete growth medium containing 1:1, 1:2, or 1:4 dilutions of the tested materials, and imaged using a phase-contrast microscope at 0, 24, 48, and 72 h. The percentage of open wound area was quantified using Image J software (National Institutes of Health, Bethesda, MD, USA). The data are expressed as the mean of three independent experiments ± standard deviation (SD).
Cell adhesion evaluation
To test the effect of surface chemistry of the different cements on cell adhesion and growth, scanning electronic microscopy (SEM) was used. Sample discs with the aforementioned standardized dimensions were obtained (n = 15) for each of the materials and allocated into three groups (n = 5). hDPSCs were directly seeded onto the material´s surface and cultured in normal growth medium. After 72 h, cells were fixed with 3% glutaraldehyde (Sigma-Aldrich) in PBS for 30 min. The specimens were then dehydrated using a graded ethanol series, followed by hexamethyldisilazane (Sigma-Aldrich) treatment for 5 min. The samples were gold sputter–coated and observed under SEM using × 100, × 300, and × 1500 magnifications.
Cell cytoskeleton staining
Phalloidin staining was used to analyze possible changes in cell morphology and in the actin cytoskeleton structure and organization of hDPSCs cultured with the different material eluates. Briefly, cells were seeded on glass coverslips, allowed to adhere, and cultured in complete growth medium alone (control) or in complete growth medium containing 1:1, 1:2, or 1:4 dilutions of the different eluates for 72 h at 37°C. Then, hDPSCs were rinsed twice with prewarmed PBS at 37 °C, fixed in 4% formaldehyde solution (Merck Millipore, Darmstadt, Germany) for 10 min, permeabilized with 0.25% Triton X-100 solution (Sigma-Aldrich) for 5 min, and rinsed 3 times with PBS. Cell cytoskeleton and nuclei were then stained with AlexaFluor™594-conjugated phalloidin (Invitrogen, Carlsbad, CA, USA) and 4,6-diamidino-2-phenylindole dihydrochloride (DAPI) (ThermoFisher Scientific, Waltham, MA, USA), respectively. Finally, immunofluorescence images were observed under a Leica TCS SP2 confocal microscope (Leica, Wetzlar, Germany). Each experimental condition was carried out in triplicate for each VTP material and analyzed in three independent experiments.
Apoptosis/necrosis assay
To evaluate hDPSC viability after exposure to the different materials, hDPSCs were cultured in complete growth medium alone (control) or in complete growth medium containing 1:1, 1:2, or 1:4 dilutions of the different eluates for 72 h at 37 °C. Cell viability was assessed by Annexin-V-FITC and 7-AAD staining (BD Biosciences, San Jose, CA, USA) following the manufacturer’s instructions. Samples were analyzed in a FACS Calibur Flow cytometer (Becton Dickinson) within 1 h of staining. Finally, the percentages of viable (double negative), early apoptotic (Annexin-V-FITC positive, 7AAD negative), and late apoptotic and necrotic (double positive and Annexin-V-FITC negative/7-AAD positive respectively) cells were determined. Each experimental condition was performed in triplicate for each VPT material and analyzed in three independent experiments.
Odontogenic marker expression (RT-qPCR)
The induction of odontogenic differentiation of hDPSCs cultured with undiluted material-conditioned medium was evaluated by analyzing the expression of a series of odontogenic markers by real-time quantitative reverse-transcriptase polymerase chain reaction (RT-qPCR). The sequences of primers for the odontogenic markers used were as follows (forward/reverse): alkaline phosphatase (ALP): 5´- TCAGAAGCTCAACACCAACG-3´/5´-TTGTACGTCTTGGAGAGGGC-3´; collagen type 1 (Col1A1): 5´-CCCGGGTTTCAGAGACAACTTC-3´/5´- TCCACATGCTTTATTCCAGCAATC-3´; osteonectin (ON): 5´-GCATCAAGCAGAAGGATA-3´/5´-AATAGTTAAGTTACAGCTAAGAAT-3´; dentin sialophosphoprotein (DSPP): 5´-GCATTTGGGCAGTAGCATGG-3´/5´-CTGACACATTTGATCTTGCTAGGAG-3´; runt-related transcription factor 2 (RUNX2): 5´-TCCACACCATTAGGGACCATC-3´/5´-TGCTAATGCTTCGTGTTTCCA-3´; and Bone Sialoprotein Progenitor (BSP): 5´-TGCCTTGAGCCTGCTTCCT-3´/ 5´-CTGAGCAAAATTAAAGCAGTCTTCA-3´. Glyceraldehyde 3-phosphate dehydrogenase (GAPDH) was used as a housekeeping gene to quantify and normalize the results, with the following primers sequences (forward/reverse): 5´-TCAGCAATGCCTCCTGCAC-3´/5´-TCTGGGTGGCAGTGATGG-3´.
hDPSCs (2 × 104 cells/well n = 3) were seeded onto 12-well plates with the material-conditioned medium (1:1) and cultured for 7 days. The analysis of relative gene expression data was calculated using the 2-ΔΔCT method. Cells cultured in unconditioned medium (DMEM) acted as the negative control, and an osteo/odontogenic medium (OsteoDiff media; Miltenyi Biotec) acted as the positive control.
Mineralization assay (Alizarin red S staining)
Alizarin Red S staining was used to assess the mineralization potential of hDPSCs in contact with Theracal PT, Theracal LC, and MTA Angelus. Cells were seeded onto 12-well plates (2 × 104 cells/well, n = 3) and left to proliferate until confluent. Then, hPDLSCs were cultured in undiluted material-conditioned medium for 21 days. After the culture period, the samples were washed (PBS) and fixed with 70% ethanol for 1 h, and then stained with 2% Alizarin Red S solution (Sigma Aldrich) for 30 min in the dark at room temperature. The staining was solubilized with 10% cetylpyridinium chloride monohydrate (Sigma-Aldrich, MO, USA) solution and the absorbance was measured at 570 nm using a spectrophotometer. hDPSCs cultured in unconditioned medium (DMEM) acted as the negative control, and OsteoDiff media (Miltenyi Biotec) acted as the positive control.
Statistical analysis
All of the in vitro assays were performed in triplicate, and analyzed in three independent experiments. After confirming the homogeneity of variance and normal distribution of the data, we performed one-way ANOVA followed by pair-wise Tukey’s post hoc test using Graph-Pad Prism v8.1.0 (GraphPad Software, San Diego, CA, USA). Data are expressed as mean ± standard deviations (SD). Statistical significance was considered at p < 0.05.
Results
Ion release
The analysis of the ion release demonstrated by ICP-MS is presented in Table 2. The results revealed that silicon (Si) ion release was higher in Theracal PT and Theracal LC compared to MTA Angelus (p < 0.05), while barium (Ba) and tungsten (W) ion release was significantly increased in MTA (p < 0.05). Calcium (Ca) ion release was significantly lower in MTA Angelus compared to Theracal PT and Theracal LC (p < 0.05).
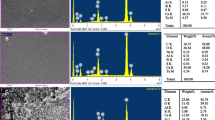
SEM-EDS analysis
The qualitative analysis of the chemical elements on the specimens’ surfaces was comparable to the material composition according to the manufacturers’ information, as shown in Fig. 1 and Table 1. MTA showed the highest Ca content. Theracal PT, on the other hand, exhibited the highest percentage of zirconium (Zr) and Si. Interestingly, the percentage of Si in Theracal PT was higher than Theracal LC and MTA Angelus. However, fluoride (F) was not detected in Theracal PT. Additionally, the SEM-EDS analysis disclosed other elements not mentioned in the manufacturers’ information: Aluminium (Al) was found in Theracal LC and Theracal Pt and W was found in Theracal LC and Theracal PT.
SEM-EDS analysis results for MTA Angelus (a), Theracal LC (b), and Theracal PT (c) disks (n = 9). The first column presents SEM micrographs of each materials (scale bar: 100 μm). The second column illustrates the EDS plots with correspondent peaks detected. The third column classifies the list of elements present per materials by weight and atomic weight
hDPSC characterization
The results of flow cytometry showed that isolated hDPSCs were CD73 (99.9%), CD90 (99.7%), and CD105 (99.9%) positive; and negative for CD34, CD45, CD14, and CD20 (2.5%) (Fig. 2a). The percentages are presented relative to the proper expression of mesenchymal stem cell surface markers. Furthermore, hDPSCs exhibited ability to differentiate into osteoblasts, chondroblasts, and adipocyte-like cells (Fig. 2b).
Cytotoxicity assay
hDPSCs were exposed to several dilutions of Theracal PT, Theracal LC and MTA Angelus for 72 h, and cell viability was determined using an MTT assay (Fig. 3). Theracal LC showed a significant reduction in cell viability compared to the negative control in all concentrations and time-points (p < 0.001), whereas MTA Angelus exhibited no significant differences in cell viability. Theracal PT 1:1 and 1:2 showed a discrete cell viability compared to the control, while in the 1:4 dilution, no difference was found compared to the control group in the first time-points (24 and 48 h).
MTT assay. In vitro cytotoxicity of hDPSCs after exposure to extracted medium prepared from MTA Angelus, Theracal LC, and Theracal PT. Data are presented absorbance values (570 nm) at 24, 48, and 72 h of exposure of the material eluates to hDPSCs, compared to the control. *p < 0.05; **p < 0.01; ***p < 0.001. Each experimental condition was performed in triplicate for each VPT material and analyzed in three independent experiments
Migration assay
An in vitro wound healing assay was performed to evaluate cell migration. Cells cultured in medium without any material eluate were employed as the negative control. 1:1 and 1:2 Theracal LC displayed a statistically significant decreased cell migration after 24, 48, and 72 h of culture (p < 0.001), while no significant differences were found between 1:4 Theracal LC and the negative control (Fig. 4). Cell migration rates exhibited by hDPSCs cultured with undiluted Theracal PT were significantly lower at 24, 48, and 72 h compared to the control group (p < 0.001), while this inhibitory effect was not so evident with Theracal PT 1:2 and 1:4. Regarding MTA Angelus, the cell migration rate was similar than that of control group at all time-periods and dilutions (Fig. 4).
Cell migration was evaluated using a scratch assay. Cells were exposed to undiluted (1:1) and diluted (1:2 and 1:4) eluates from materials. The control condition was cells maintained in normal growth medium. Graphical results are presented as mean RWC percentages at each of the time points, relative to the total wound area at 0 h. Asterisk designates significant differences compared with the control. *p < 0.05; **p < 0.01; ***p < 0.001. Each experimental condition was performed in triplicate for each VPT material and analyzed in three independent experiments
Cell adhesion
The analysis of cell adherence and morphology of hDPSCs on the surfaces of the different material specimens showed the presence of few cells and debris in the Theracal LC samples, evidencing cell death, whereas abundant and functionally oriented cells were exhibited by MTA. Theracal PT samples exhibited a moderate growth of elongated cells (Fig. 5).
Sample discs with the aforementioned standardized dimensions were obtained (n = 15) for each of the materials and allocated into three groups (n = 5). Representative SEM micrographs illustrate the adhesion of hDPSCs directly seeded on Theracal PT, MTA Angelus and Theracal LC. Magnifications: × 100, × 300, and × 1500. Scale bars: 500 μm, 100 μm, and 30 μm
Cell cytoskeleton staining
In the MTA group, at all dilutions, a high number of well-adhered and spread cells with a fibroblastic spindle-shaped morphology and increased F-actin content were observed, similar to that observed on the cells from the negative control group (Fig. 6). 1:1 and 1:2 Theracal LC showed lower numbers of attached cells, some of them exhibiting an aberrant morphology, while Theracal LC 1:4 specimens exhibited a similar number of cells with well-evident actin cytoskeleton compared to the control group. Conversely, cells from the Theracal PT specimens showed a favorable growth and similar well-organized F-actin filaments compared to the control group, especially at 1:2 and 1:4 dilutions (Fig. 6).
Analysis of cell morphology changes, in the actin cytoskeleton structure and organization on hDPSCs after treatment with Theracal PT, MTA Angelus and Theracal LC by confocal fluorescence microscopy. F-actin fibers were stained with AlexaFluor™ 594-conjugated phalloidin (red), whereas cell nuclei were counterstained with DAPI (blue). Confocal fluorescence microscopy images shown are representative from n = 3 separate experiments. Scale bar: 100 μm. Each experimental condition was performed in triplicate for each VPT material and analyzed in three independent experiments
Apoptosis/necrosis assay
The apoptosis/necrosis rate in each group was obtained by flow cytometry. As shown in Fig. 7, undiluted materials displayed the following percentage of viable cells: MTA Angeluls (90.5%) > Theracal PT (80.5%) > Theracal LC (10.5%). At 1:2 dilutions all materials displayed a high percentage of viable cells (> 89%), except Theracal LC (21.1%). Similarly, at 1:4 dilution, all materials displayed a similar biocompatibility compared to the control medium, exhibiting more than 89% of viable cells, excluding Theracal LC (64.6%). These findings were in agreement with those obtained in the MTT and migration assays.
Flow cytometry analysis of cell apoptosis and necrosis induced by the different vital pulp material extracts on hDPSCs by annexin V-PE/7-AAD staining. Numbers inside dot plots represent percentages of live (Q4 quadrants), early apoptotic (Q3 quadrants), and late apoptotic and necrotic cells (Q1 and Q2 quadrants). Dot plots shown are representative from n = 3 separate experiments
RT-qPCR assay
The mRNA expression of odonto/osteogenic markers was evaluated at day 7 after culturing hDPSCs with the different materials (Fig. 8). GAPDH expression was used to normalize the results. Due to the in vitro toxicity exhibited by Theracal LC in the aforementioned assays, this material was not employed in the cell differentiation assays. The MTA Angelus group displayed an upregulation of ALP, DSPP, RUNX2 (p < 0.001), ON, Col1A1 (p < 0.01), and BSP genes (p < 0.05) compared to the negative control, while the Theracal PT group showed an upregulation of DSPP and RUNX2 (p < 0.001). Interestingly, the expression of DSPP and RUNX2 was significantly different in the Osteodiff group (positive control) compared to the negative control at day 7. However, a marked decrease in the expression Col1A1 and ALP was observed.
Mineralization assay
Calcium deposition, as a final product of the odonto/osteogenic differentiation process, was assessed by using Alizarin Red S staining on day 21 (Fig. 9). There were significant differences between the tested groups, with Osteodiff (positive control) exhibiting the highest amounts of calcium deposition (p < 0.001). In contrast, Theracal LC exhibited the lowest amounts of mineralized nodules. MTA Angelus and Theracal PT showed higher amounts of mineralized nodules when compared to the negative control (p < 0.001).
Calcium deposition, as a final product of the odonto/osteogenic differentiation process, was assessed by using Alizarin Red S staining on day 21. *p < 0.05; **p < 0.01; ***p < 0.001. Each experimental condition was performed in triplicate for each VPT material and analyzed in three independent experiments
Discussion
The present study investigated the effects of the three vital pulp materials on the viability, morphology, migration, adhesion, osteo/odontoblastic differentiation, and mineralization potential of hDPSCs. It is crucial that the material placed in direct contact with the pulp tissue during VPT procedures presents, at least, an adequate biocompatibility and ideally, a bioactive effect. A lack of biocompatibility will result in an intense irritation to the pulp tissue, which can irreversibly compromise its defensive mechanisms and in turn, its vitality [23,24,25]. For this reason, mesenchymal stem cells from dental pulp where used as the target cells for the cytotoxicity analyses.
A high number of quantitative and qualitative assessments of in vitro and in vivo cytotoxicity highlight the effectiveness of vital pulp materials [26]. These studies were generally performed to gain an increased understanding of the biological mechanisms involved in tertiary dentin formation. However, the limitations of those reports were the types of target cells used, the duration of the exposure to the tested materials, and the formulation of such materials [4]. The biological properties of well-established vital pulp materials have been extensively described among available literature. However, to our knowledge, this the first study assessing Theracal PT.
ICP-MS and SEM-EDS assays showed calcium content and ion release in all materials, as previously reported for other vital pulp materials: NeoMTA Plus (Avalon Biomed, Houston, TX, USA), MTA Repair HP (Angelus), or Biodentine (Septodont, Saint-Maur-des-Fossés, France) [27]. Furthermore, ytterbium (Yb) was detected in Theracal PT. It has been described that the incorporation of Yb as a radiopacifying agent for calcium silicate–based cements does not alter their physicochemical and biological properties, and preserves their bioactive potential [28]. Also, Si release was higher from Theracal PT than from Theracal LC samples after setting (p < 0.05). Previous studies demonstrated that Si ions from silicate bioceramics stimulated the osteogenic differentiation of mesenchymal stem cells [29]. Thus, the differences in ion release may influence the biological effects or, at least, the characteristics of the mineral attachment formed to the dentin substrate.
The materials used for VPT, in addition to possessing antiinflammatory properties, play an important role in the proliferation, migration, and mineralization of dental pulp stem cells [30]. In the present study, the MTT assays revealed that Theracal LC negatively affected hDPSC viability at all extraction medium concentrations, whereas this effect was lower in the Theracal PT group. Unsurprisingly, MTA group exhibited a higher cell viability compared to the other materials and the control. These findings were in agreement with previous reports demonstrating that Theracal LC exhibited a cytotoxic effect [15, 31].
It is well known that bioactive materials release substances that could potentially delay or enhance the healing process [32]. For this reason, wound healing assays were performed in order to preliminarily predict how the coordinated migration of hDPSC would occur during pulp inflammation or after injury. The marked decrease in cell migration in the Theracal LC–treated group could be due to the effect of this material on cell viability. Nevertheless, no significant differences were observed in 1:2 and 1:4 Theracal PT groups, evidencing an optimal biological response with these dilutions. The cell migration results correlated with the cell attachment and spreading results, as expected, since cells require an adequate attachment and spreading on a surface for subsequent migration. Low cell attachment and F-actin fibers content and an aberrant morphology were evidenced in the 1:1 and 1:4 Theracal LC–treated group as observed by phalloidin staining and SEM. Hence, their migration would also be affected.
Apoptosis/necrosis assay evidenced a reduced number of viable cells in Theracal LC–treated group. This phenomenon was less evident in Theracal PT–treated group. It has been speculated that the cytotoxicity of Theracal LC may be due to remaining unpolymerized resin monomers which leads to their leaching [25, 33]. Furthermore, other authors have demonstrated that cured Theracal LC released specific additives such as ethyl-4-(dimethylamino) benzoate and camphorquinone [34]. Primary human pulp fibroblasts exposed to camphorquinone evidenced increased reactive oxygen species production [35, 36]. Taken together, it can be suggested that the light curing additives released from Theracal LC may induce cell death by increasing the production of reactive oxygen species.
To evaluate the potential effects of the tested materials for VTP on the osteo/odontoblastic differentiation of hDPSCs, expressions of ALP (alkaline phosphatase), BSP (bone sialoprotein), Col1A1 (collagen type I alpha 1), DSPP (dentin sialophosphoprotein), ON (osteonectin), and RUNX2 (runt-related transcription factor 2) genes were used as markers of different phases of this process. As mentioned previously, the marked cytotoxicity exhibited by Theracal LC resulted in its exclusion from the differentiation assays, since no gene upregulation was to be expected. MTA exhibited an upregulation of all of the tested markers. A similar outcome was observed in a previous study, in which the cytotoxicity and osteogenic potential of MTA and Theracal LC, among other materials, was assessed together with hDPSCs [37]. Theracal LC exhibited no upregulation of osteo/odontogenic markers, while MTA showed a significant upregulation of ALP, OCN (osteocalcin), BSP, DSPP, and DMP1 (Dentin matrix acidic phosphoprotein 1) at 7 days when compared to a control (p < 0.05). In contrast with our study, however, MTA did not induce an upregulation of RUNX2.
In addition, both MTA and Theracal PT–cultured cells showed a significant upregulation of DSPP and RUNX2 genes at day 7. Since, to the authors’ knowledge, this is the first study to assess the biological properties of Theracal PT, these results cannot be compared with other studies. Nevertheless, the upregulation of RUNX2, a key transcription factor for osteoblast differentiation [38], and DSPP, involved in the process of mineralization of dentin [39], highlights the potential influence of both of the assessed materials on hDPSC osteo/odontogenic differentiation.
Regarding the mineralization potential of the tested materials for VPT, a similar pattern was observed. hDPSCs treated with Theracal LC exhibited the lowest calcified nodule formation, and both MTA and Theracal PT–treated cells showed a significant mineralization potential. These results are in accordance with previous studies: in direct contact with stem cells from human exfoliated deciduous teeth (SHEDs), MTA showed a higher mineralization potential than Theracal LC [40]; and significantly higher mineralized nodule formation compared to a negative control when cultured with human dental pulp cells (hDPCs) [41]. Again, no available evidence was found regarding Theracal PT. Nonetheless, the results from the mineralization assays from the present study highlight its comparable mineralization potential to that exhibited by MTA. In VPT procedures, the materials used should possess the ability to induce the superficial mineralization of the viable pulp tissue to form a calcified bridge. However, in order to preserve the correct functioning of the pulp tissue, its diffused calcification should be avoided, as it will lead to pulp inflammation and loss of vitality, and eventually to treatment failure [42].
Altogether, the biological properties and bioactive potential of hydraulic calcium silicate–based cements, such as those assessed in the present study, have been evidenced by numerous studies [5]. Still, the rapid introduction of new material compositions into the market calls for an updated biological and chemical-mechanical profiling of each new composition before its clinical use. This highlights the importance and relevance of in vitro studies as a preliminary approach to the assessment of new materials. However, results from these assays should be interpreted with caution, since the behavior of the tested materials could be potentially influenced by a number of external factors in the clinical setting.
Conclusions
This study demonstrates the favorable in vitro cytocompatibility and bioactive properties of the recently introduced Theracal PT and the well-established MTA Angelus on hDPSCs, as opposed to Theracal LC. More studies, including in vivo animal testing are suggested before these new formulations might be used in the clinical setting.
References
da Rosa WLO, Piva E, da Silva AF (2018) Disclosing the physiology of pulp tissue for vital pulp therapy. Int Endod J 51:829–846. https://doi.org/10.1111/iej.12906
Tran XV, Gorin C, Willig C, Baroukh B, Pellat B, Decup F, Opsahl Vital S, Chaussain C, Boukpessi T (2012) Effect of a calcium-silicate-based restorative cement on pulp repair. J Dent Res 91:1166–1171. https://doi.org/10.1177/0022034512460833
Hanna SN, Perez Alfayate R, Prichard J (2020) Vital pulp therapy an insight over the available literature and future expectations. Eur Endod J 5:46–53. https://doi.org/10.14744/eej.2019.44154
Meschi N, Patel B, Ruparel NB (2020) Material pulp cells and tissue interactions. J Endod 46:S150–S160. https://doi.org/10.1016/j.joen.2020.06.031
Parirokh M, Torabinejad M, Dummer PMH (2018) Mineral trioxide aggregate and other bioactive endodontic cements: an updated overview - part I: vital pulp therapy. Int Endod J 51:177–205. https://doi.org/10.1111/iej.12841
Rosa V, Zhang Z, Grande RH, Nor JE (2013) Dental pulp tissue engineering in full-length human root canals. J Dent Res 92:970–975. https://doi.org/10.1177/0022034513505772
Tatullo M, Codispoti B, Sied J, Makeeva I, Paduano F, Marrelli M, Spagnuolo G (2019) Stem cells-based and molecular-based approaches in regenerative dentistry: a topical review. Curr Stem Cell Res Ther 14:607–616. https://doi.org/10.2174/1574888X14666190626111154
Youssef AR, Emara R, Taher MM, Al-Allaf FA, Almalki M, Almasri MA, Siddiqui SS (2019) Effects of mineral trioxide aggregate, calcium hydroxide, biodentine and Emdogain on osteogenesis, Odontogenesis, angiogenesis and cell viability of dental pulp stem cells. BMC Oral Health 19:133. https://doi.org/10.1186/s12903-019-0827-0
Zaen El-Din AM, Hamama HH, Abo El-Elaa MA, Grawish ME, Mahmoud SH, Neelakantan P (2020) The effect of four materials on direct pulp capping: an animal study. Aust Endod J 46:249–256. https://doi.org/10.1111/aej.12400
Dahake PT, Panpaliya NP, Kale YJ, Dadpe MV, Kendre SB, Bogar C (2020) Response of stem cells from human exfoliated deciduous teeth (SHED) to three bioinductive materials - an in vitro experimental study. Saudi Dent J 32:43–51. https://doi.org/10.1016/j.sdentj.2019.05.005
Pelepenko LE, Saavedra F, Antunes TBM, Bombarda GF, Gomes B, Zaia AA, Camilleri J, Marciano MA (2020) Physicochemical, antimicrobial, and biological properties of White-MTAFlow. Clin Oral Investig 25:663–672. https://doi.org/10.1007/s00784-020-03543-7
Sauro S, Babbar A, Gharibi B, Feitosa VP, Carvalho RM, Azevedo Rodrigues LK, Banerjee A, Watson T (2018) Cellular differentiation, bioactive and mechanical properties of experimental light-curing pulp protection materials. Dent Mater 34:868–878. https://doi.org/10.1016/j.dental.2018.02.008
Wongwatanasanti N, Jantarat J, Sritanaudomchai H, Hargreaves KM (2018) Effect of bioceramic materials on proliferation and odontoblast differentiation of human stem cells from the Apical Papilla. J Endod 44:1270–1275. https://doi.org/10.1016/j.joen.2018.03.014
Kunert M, Lukomska-Szymanska M (2020) Bio-inductive materials in direct and indirect pulp capping-a review article. Materials (Basel) 13. https://doi.org/10.3390/ma13051204
Jeanneau C, Laurent P, Rombouts C, Giraud T, About I (2017) Light-cured tricalcium silicate toxicity to the dental pulp. J Endod 43:2074–2080. https://doi.org/10.1016/j.joen.2017.07.010
Peters OA (2013) Research that matters - biocompatibility and cytotoxicity screening. Int Endod J 46:195–197. https://doi.org/10.1111/iej.12047
Peters OA, Galicia J, Arias A, Tolar M, Ng E, Shin SJ (2015) Effects of two calcium silicate cements on cell viability, angiogenic growth factor release, and related gene expression in stem cells from the apical papilla. Int Endod J 49:1132–1140. https://doi.org/10.1111/iej.12571
ISO 10993-12 (2012) Biological evaluation of medical devices—Part 12: sample preparation and reference materials. Geneva, Switzerland
Collado-Gonzalez M, Garcia-Bernal D, Onate-Sanchez RE, Ortolani-Seltenerich PS, Alvarez-Muro T, Lozano A, Forner L, Llena C, Moraleda JM, Rodriguez-Lozano FJ (2017) Cytotoxicity and bioactivity of various pulpotomy materials on stem cells from human exfoliated primary teeth. Int Endod J 50:e19–e30. https://doi.org/10.1111/iej.12751
Dominici M, Le Blanc K, Mueller I, Slaper-Cortenbach I, Marini F, Krause D, Deans R, Keating A, Prockop D, Horwitz E (2006) Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy 8:315–317. https://doi.org/10.1080/14653240600855905
Rodriguez-Lozano FJ, Collado-Gonzalez M, Tomas-Catala CJ, Garcia-Bernal D, Lopez S, Onate-Sanchez RE, Moraleda JM, Murcia L (2019) GuttaFlow Bioseal promotes spontaneous differentiation of human periodontal ligament stem cells into cementoblast-like cells. Dent Mater 35:114–124. https://doi.org/10.1016/j.dental.2018.11.003
Sequeira DB, Seabra CM, Palma PJ, Cardoso AL, Peca J, Santos JM (2018) Effects of a new bioceramic material on human apical papilla cells. J Funct Biomater 9. https://doi.org/10.3390/jfb9040074
Pedano MS, Li X, Li S, Sun Z, Cokic SM, Putzeys E, Yoshihara K, Yoshida Y, Chen Z, Van Landuyt K, Van Meerbeek B (2018) Freshly-mixed and setting calcium-silicate cements stimulate human dental pulp cells. Dent Mater 34:797–808. https://doi.org/10.1016/j.dental.2018.02.005
Pedano MS, Li X, Yoshihara K, Landuyt KV, Van Meerbeek B (2020) Cytotoxicity and bioactivity of dental pulp-capping agents towards human tooth-pulp cells: a systematic review of in-vitro studies and meta-analysis of randomized and controlled clinical trials. Materials (Basel) 13. https://doi.org/10.3390/ma13122670
Li X, Pedano MS, Li S, Sun Z, Jeanneau C, About I, Hauben E, Chen Z, Van Landuyt K, Van Meerbeek B (2020) Preclinical effectiveness of an experimental tricalcium silicate cement on pulpal repair. Mater Sci Eng C Mater Biol Appl 116:111167. https://doi.org/10.1016/j.msec.2020.111167
Nam OH, Kim JH, Choi SC, Kim Y (2020) Time-dependent response of human deciduous tooth-derived dental pulp cells treated with TheraCal LC: functional analysis of gene interactions compared to MTA. J Clin Med 9. https://doi.org/10.3390/jcm9020531
Tomas-Catala CJ, Collado-Gonzalez M, Garcia-Bernal D, Onate-Sanchez RE, Forner L, Llena C, Lozano A, Moraleda JM, Rodriguez-Lozano FJ (2017) Biocompatibility of new pulp-capping materials NeoMTA Plus, MTA Repair HP, and Biodentine on human dental pulp stem cells. J Endod 44:126–132. https://doi.org/10.1016/j.joen.2017.07.017
Costa BC, Guerreiro-Tanomaru JM, Bosso-Martelo R, Rodrigues EM, Bonetti-Filho I, Tanomaru-Filho M (2018) Ytterbium oxide as radiopacifier of calcium silicate-based cements. Physicochemical and Biological Properties. Braz Dent J 29:452–458. https://doi.org/10.1590/0103-6440201802033
Dong X, Wang X, Xing M, Zhao C, Guo B, Cao J, Chang J (2020) Inhibition of the negative effect of high glucose on osteogenic differentiation of bone marrow stromal cells by silicon ions from calcium silicate bioceramics. Regen Biomater 7:9–17. https://doi.org/10.1093/rb/rbz030
Giraud T, Jeanneau C, Rombouts C, Bakhtiar H, Laurent P, About I (2019) Pulp capping materials modulate the balance between inflammation and regeneration. Dent Mater 35:24–35. https://doi.org/10.1016/j.dental.2018.09.008
Collado-Gonzalez M, Garcia-Bernal D, Onate-Sanchez RE, Ortolani-Seltenerich PS, Alvarez Muro T, Lozano A, Forner L, Llena C, Moraleda JM, Rodriguez-Lozano FJ (2017) Cytotoxicity and bioactivity of various pulpotomy materials on stem cells from human exfoliated primary teeth. Int Endod J 50:e19–e30. https://doi.org/10.1111/iej.12751
Lopez-Garcia S, Myong-Hyun B, Lozano A, Garcia-Bernal D, Forner L, Llena C, Guerrero-Girones J, Murcia L, Rodriguez-Lozano FJ (2020) Cytocompatibility, bioactivity potential, and ion release of three premixed calcium silicate-based sealers. Clin Oral Investig 24:1749–1759. https://doi.org/10.1007/s00784-019-03036-2
Koutroulis A, Kuehne SA, Cooper PR, Camilleri J (2019) The role of calcium ion release on biocompatibility and antimicrobial properties of hydraulic cements. Sci Rep 9:19019. https://doi.org/10.1038/s41598-019-55288-3
Nilsen BW, Jensen E, Ortengren U, Michelsen VB (2017) Analysis of organic components in resin-modified pulp capping materials: critical considerations. Eur J Oral Sci 125:183–194. https://doi.org/10.1111/eos.12347
Atsumi T, Ishihara M, Kadoma Y, Tonosaki K, Fujisawa S (2004) Comparative radical production and cytotoxicity induced by camphorquinone and 9-fluorenone against human pulp fibroblasts. J Oral Rehabil 31:1155–1164. https://doi.org/10.1111/j.1365-2842.2004.01357.x
Engelmann J, Volk J, Leyhausen G, Geurtsen W (2005) ROS formation and glutathione levels in human oral fibroblasts exposed to TEGDMA and camphorquinone. J Biomed Mater Res B Appl Biomater 75:272–276. https://doi.org/10.1002/jbm.b.30360
Bortoluzzi EA, Niu LN, Palani CD, El-Awady AR, Hammond BD, Pei DD, Tian FC, Cutler CW, Pashley DH, Tay FR (2015) Cytotoxicity and osteogenic potential of silicate calcium cements as potential protective materials for pulpal revascularization. Dent Mater 31:1510–1522. https://doi.org/10.1016/j.dental.2015.09.020
Feng G, Zhang J, Feng X, Wu S, Huang D, Hu J, Zhu S, Song D (2016) Runx2 modified dental pulp stem cells (DPSCs) enhance new bone formation during rapid distraction osteogenesis (DO). Differentiation 92:195–203. https://doi.org/10.1016/j.diff.2016.06.001
Siew Ching H, Thirumulu Ponnuraj K, Luddin N, Ab Rahman I, Nik Abdul Ghani NR (2020) Early odontogenic differentiation of dental pulp stem cells treated with nanohydroxyapatite-silica-glass ionomer cement. Polymers (Basel) 12. https://doi.org/10.3390/polym12092125
Rodrigues EM, Cornelio AL, Mestieri LB, Fuentes AS, Salles LP, Rossa-Junior C, Faria G, Guerreiro-Tanomaru JM, Tanomaru-Filho M (2016) Human dental pulp cells response to mineral trioxide aggregate (MTA) and MTA Plus: cytotoxicity and gene expression analysis. Int Endod J 50:780–789. https://doi.org/10.1111/iej.12683
Mello-Moura ACV, Santos AMA, Bonini G, Zardetto C, Moura-Netto C, Wanderley MT (2017) Pulp calcification in traumatized primary teeth - classification, clinical and radiographic aspects. J Clin Pediatr Dent 41:467–471. https://doi.org/10.17796/1053-4628-41.6.9
Bakhtiar H, Nekoofar MH, Aminishakib P, Abedi F, Naghi Moosavi F, Esnaashari E, Azizi A, Esmailian S, Ellini MR, Mesgarzadeh V, Sezavar M, About I (2017) Human pulp responses to partial pulpotomy treatment with TheraCal as compared with biodentine and ProRoot MTA: a clinical trial. J Endod 43:1786–1791. https://doi.org/10.1016/j.joen.2017.06.025
Funding
This work was supported by the Spanish Network of Cell Therapy (TerCel), RETICS subprograms of the I+D+I 2013-2016 Spanish National Plan, project “RD16/0011/0001” funded by the Instituto de Salud Carlos III to JMM and cofunded by the European Regional Development Fund.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
The study protocol was approved by the Clinical Research Ethics Committee of the University of Murcia (procedure number: 2199/2018). Likewise, permission was obtained from the Health Department authorities to use the information contained in the CDHs, previously anonymized by one of the investigators belonging to the medical staff of the Health Department in order to protect patient confidentiality. All the information was processed in abidance with the confidentiality regulations defined under Act 15/1999 referred to personal data protection.
Informed consent
Informed consent was obtained from the parents of all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rodríguez-Lozano, F.J., López-García, S., García-Bernal, D. et al. Cytocompatibility and bioactive properties of the new dual-curing resin-modified calcium silicate-based material for vital pulp therapy. Clin Oral Invest 25, 5009–5024 (2021). https://doi.org/10.1007/s00784-021-03811-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-021-03811-0