Abstract
Objectives
To perform a review on the influence of preheating and/or heating of resinous and ionomeric materials on their physical and mechanical properties and to discuss the benefits and methods of preheating/heating that have been used.
Material and methods
A search was performed in the Pubmed, Scopus, Scielo, and gray literature databases. In vitro studies published from 1980 until now were searched using the descriptors “composite resins OR glass ionomer cements OR resin cements OR adhesives AND heating OR preheating.” Data extraction and quality of work evaluation were performed by two independent evaluators.
Results
At the end of reading the search titles and abstracts, 74 articles were selected. Preheating of composite resins reduces viscosity, facilitates adaptation to cavity preparation walls, increases the degree of conversion, and decreases the polymerization shrinkage. Preheating of resin cements improves strength, adhesion, and degree of conversion. Dental adhesives showed good results such as higher bond strength to dentin. However, unlike resinous materials, ionomeric materials have an increase in viscosity upon heating.
Conclusions
Preheating improves the mechanical and physical properties. However, there is a lack of clinical studies to confirm the advantages of preheating technique.
Clinical relevance
Preheating of dental restorative materials is a simple, safe, and successful technique. In order to achieve good results, agility and training are necessary so the material would not lose heat until the restorative procedure. Also, care is necessary to avoid bubbles and formation of gaps, which compromises the best restoration performance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There are currently a wide variety of restorative materials available for dentists. Since early formulations, resinous materials and glass ionomer cements had been improving their clinical behavior, with good success rates [1,2,3,4,5]. On the other hand, these restorative options still present some limitations and more improvements are needed, including the influence of individuals’ variables on the quality and longevity of the restoration [6, 7].
Several innovations and new techniques have been done in order to increase durability and clinical behavior of restorative materials, including the change in material composition, such as the bulk-fill resins [8] and new glass ionomer cements [9]; the development of alternative photoinitiators and new multi-peak LED light-curing units with a larger spectral emission profile [10], and the minimally invasive approach that conserves more tooth structures [11]. Another proposed alternative for optimizing the characteristics of dental materials has been preheating [12, 13].
The preheating of the resin-based materials has been performed by commercial devices, such as the Calset (AdDent Inc., Danbury CT, USA) [14,15,16], ENA Heat (Micerium SpA, Avegno GE, Italy) [17, 18], Hotset [19], HeatSync [20], and Caps Warmer (VOCO GmbH, Cuxhaven NI, Germany) [21]. Also, it is being used with a water bath [22,23,24], incubator [25,26,27], and digital wax heaters [28]. The glass ionomer cements have already been heated using [9, 29, 30] LED light as an externally applied “command set” and ultrasound to mechanically energized GICs rather than directly preheat them [30], which provide energy in the form of heat, as well as obtaining heated capsules by water bath [31]. The heating can be done prior to manipulation and insertion into the cavity/tooth (preheating) or after the restorative materials have been mixed.
Although many studies have addressed the performance of different materials with preheating techniques, there is lack of evidence that restorative materials' preheating improves the quality and durability of restorations. Some advantages reported in the literature with the preheating technique of resinous materials include increased degree of conversion [27], improved marginal adaptation of restorations due to reduce the viscosity [14, 16, 22], and decreased polymerization contraction [15]. Thus, the objectives of this study were (1) to perform a systematic review on the influence of preheating and/or heating of resinous and ionomeric commercial materials on their physical and mechanical properties and (2) to discuss the benefits and methods of preheating/heating that have been used for resin-based and ionomeric materials.
Material and methods
This is a systematic review of the literature to answer the following question: Does preheating/heating of restorative materials (resin, resin cement, adhesive, and glass ionomer cement) influence physical and mechanical properties?
Eligibility criteria
In vitro studies published from 1980 onwards reported the influence of preheating/heating of restorative materials on physical and mechanical properties (degree of conversion, microhardness, viscosity, color, compressive strength, flexural strength, adhesion) without restriction of language were included.
Studies were excluded if (1) did not evaluate preheated/heated restorative materials; (2) no control group; (3) in vivo studies or clinical study; (4) studies that evaluated orthodontics adhesive systems or experimental materials.
Database and search strategy
A search was conducted in the PubMed (US National Library of Medicine National Institutes of Health), Scopus (Elsevier) Scielo, and gray literature databases until July 2020. MeSH terms were used along with the listed entry terms to construct a highly sensitive search strategy. The search strategy used for PubMed was: (“composite resins” [MeSH Terms] OR (“composite” [All Fields] AND “resins” [All Fields]) OR “composite resins” [All Fields]) OR (“glass ionomer cements” [MeSH Terms] OR (“glass” [All Fields] AND “ionomer” [All Fields] AND “cements” [All Fields]) OR “glass ionomer cements” [All Fields])) OR (“resin cements” [MeSH Terms] OR (“resin” [All Fields] AND “cements” [All Fields]) OR “resin cements” [All Fields])) OR (“adhesives” [Pharmacological Action] OR “adhesives” [MeSH Terms] OR “adhesives” [All Fields])) AND (“heating” [MeSH Terms] OR “heating” [All Fields])) OR preheating [All Fields], and complemented with references being cited in the selected papers.
Selection of studies and calibration of investigators
Initially, titles and abstracts were selected and evaluated by two independent researchers (LCPL and FMT). Selected studies were included for reading the full article. Each selected article was independently analyzed by the researchers and included or not in the review, based on the inclusion and exclusion criteria. In case of disagreement between the investigators, a third reviewer (RSST) evaluated the article to reach a consensus.
Risk of bias and quality of work
Data extraction and quality of work evaluation were performed by two independent evaluators (LCPL and FMT). The risk of bias assessment was performed following the guidelines of the Guidelines OHAT Risk of Bias Tool (National Health and Medical Research Council, 2015) [32], taking into account 11 criteria. Each item analyzed received the answers according to the guideline: ++definitely low risk of bias; +probably low risk of bias; − probably high risk of bias; −−definitely high risk of bias.
Results
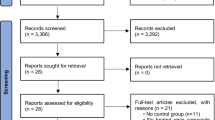
We found 1921 articles in the Pubmed database, 179 articles in the Scopus database, and 288 in Scielo. At the end of reading the search titles and abstracts, 83 articles from the Pubmed database and 71 articles from the Scopus database and 1 article from Scielo database were selected. After reading the full texts, excluding repeated titles and evaluating the eligibility criteria, 65 articles were selected and 9 references cited from the selected articles were included, totaling 74 articles at the end (Fig. 1). After analyzing the risk of bias based on the guidelines of the OHAT Risk of Bias Tool Guidelines [32], it was found that the included articles were classified as probably low risk of bias, since most studies presented at least 2 items assessed as “definitely low risk of bias” and at least 5 or more items rated “probably low risk of bias.” Only 4 papers had at least 1 “probably high risk of bias” response and only 1 paper had 5 items rated “definitely high risk of bias.”
The articles selected were from 20 different countries (Table 1). Most of the selected studies evaluated composite resin (73.9%), followed by glass ionomer cement (11.5%), resin cements (10.1%), and adhesives (4.3%).
Table 2 presents a summary of the heating methods that have been employed depending on the restorative material and the heating protocol and Table 3 the main results obtained.
Discussion
Preheating dental restorative materials have been used for almost 40 years. The first material to be subjected to the preheating technique was a composite resin of regular consistency [12] and subsequently fluid resins and resin cements. Preheating apparently increases the flowability of regular consistency composites [45], which improves the adaptation of the material in the cavity walls [38, 39]. Another situation that preheating would be indicated was for dentists who store the resins in a refrigerator, following the manufacturer’s guidelines. In this context, some authors report that the cooling of composite resins may disrupt some characteristics and it is important that they return to environment temperature before use [40]. Also, incomplete polymerization and unreacted monomers may leach into saliva promoting undesirable consequences and acting plasticizers that decrease mechanical strength and dimensional stability, color change, and allow bacterial growth. Unreacted monomers can also cause allergic and sensitivity reactions [14].
The heating technique has been applied to glass ionomer cements after manipulation using external heat energy as a command set to improve mechanical properties too. Some studies [31, 83] have shown that the application of heat in glass ionomer cements after mixing increases surface microhardness by up to 4 mm, improves marginal adaptation, and reduces working time and crack propagation.
Various types of resin-based materials (hybrid composite resin, methacrylates, silorane, resin cements) have been tested in the laboratory to evaluate the influence of preheating on their physical, mechanical, and photoactivation properties. The average preheating temperature found in the literature is 54-68 °C, considered a safe temperature for some authors [29, 50, 69], since it does not cause damage to the pulp tissue. Clinically, other situations can commonly cause increased pulp temperature such as the use of diamond burs during cavity preparation and photoactivation of resin materials. Possibly, the heating caused by the use of high irradiance from light-curing units is similar or greater than the heating of restorative materials. The temperature of the heated material placed into the cavity is not the same, as there is a rapid dropping of approximately 50% in 2 min counted after removing the material from the heating device [40]. A pulp temperature rise of 5.5 °C is considered as the potential damaging threshold for human pulp tissue [88] and the remaining dentin thickness still appears to be one of the most important factors for the protection of the pulp since dentin acts as a thermal barrier against harmful stimuli [69]. However, Knezevic et al. [48], when assessing cellular toxicity resulting from preheating of resins at 68 °C suggested that this procedure may not be safe.
Another important consideration about preheating is the required time to achieve good fluidity and improvement of restorative material properties. Not all papers mention this information. From studies that mentioned the required time for material heating, the minimum and maximum times found were 40 s to 24 h, i.e., there is a very wide variation. However, a reasonable clinical time is approximately 15 min, as used in some studies [24, 26, 65, 69, 72]. For another study, 11 min was enough to reach the temperature required [40].
The most common device for preheating is Calset (AdDent Inc, Danbury, CT, USA). The manufacturer’s instructions recommend it to preheating many types of instruments and materials like compules or syringes of composite resins, composite dispenser, anesthetics, spatulas, and laminate venners. The device is presented with different trays, depending on what the clinician needs for preheating. It offers three different temperatures and permits preheat or maintain the temperature at 37 °C, 54 °C, or 68 °C, as Caps Warmer (VOCO) [21]. Another devices, ENA Heat (Micerium SpA, Avegno GE, Italy) offers two different temperatures 39 °C and 55 °C, Hotset 39 °C and 69 °C [19] and HeatSync 68 °C [20].
The composite resins reduce their viscosity when heated, facilitating the adaptation to the walls of the cavity preparation [14, 16, 22, 37, 39, 40, 42, 58, 76, 78] and there is an improvement of many physical properties [17, 18, 24, 26, 38, 45, 46, 61, 65, 72], such as a higher degree of conversion [27, 44, 57, 60, 61, 71, 73] and lower polymerization shrinkage [15]. Preheating of resin-based materials enhances conversion without hastening the time at which maximum cure rate occurs. This enhancement is probably attained by increased molecular mobility and collision frequency of reactive species. The phenomenon involves a postponement of diffusion-controlled propagation, reaction-diffusion-controlled termination, and autodeceleration, thereby allowing the system to reach higher limiting conversions before vitrification [89]. It is further known that, in addition to preheating, resin properties can be improved due to other situations such as increased light-activation time and the power of the LED light-curing units [38, 45, 77, 78]. Usually, the temperature used to enhance these properties is 54 °C to 68 °C, depending on the type of device available. At this moment no work searched the differences between preheating at 54 °C or 68 °C.
It should be considered that resin composites with different compositions may take different times to reach stable temperature and sufficient time is mandatory for they reach and maintain the temperature [40]. Also, when the effect of compules/composite types on temperature values was evaluated, it seems that different compule types did not affect temperature values and maximum compule temperature attained was 48.3 ± 0.7 °C when the Calset unit was preset to 54 °C, and 54.7 ± 1.9 °C when preset to 60 °C [40]. But the composite compule already loaded into a delivery syringe was more efficient: higher temperatures were attained with this method as opposed to preheating the compule separately.
Although much work has shown the benefits of preheating composite resins, others have shown that preheating did not influence on some physical and mechanical properties of resin [49], such as flexural strength [16, 54], microhardness [59], degree of conversion [47, 64, 90], polymerization shrinkage [62] and marginal microleakage [74]. Repeated heating of the resin may not be detrimental to flexural strength [55] but can cause color change [77]. Also, re-heating of unused composite may not affect its degree of conversion, thus decreasing material waste [40]. These results may be a function of different methodologies, but the benefits of preheating are achieved when light-activation is performed with the resin still warm [39, 41]. Thus, to succeed with this technique, it is important to insert the material into the cavity quickly and efficiently, also avoiding the formation of bubbles and gaps [41]. The success of the technique also depends on other variables, such as the formulation of the material itself [56, 91], quantity and organic matrix type [92], inorganic load filling [17], heating time and temperature, light-activation technique [38, 49], in addition to the operator variability [39, 52].
The same preheating technique has also been applied to adhesives with incongruent results. Some studies have reported dentin bond strength of Adper Single Bond improvement [23], degree of conversion increasing and less solubility for Adper Single Bond 2 [25], solubility and water sorption increasing for XP Bond adhesive [25], and others have not found a significant difference in dentin bond strength, using Scotchbond Multipurpose Adhesive [33], Prime&Bond 2.1 and Adper Single Bond 2 [34], and Clearfil SE Bond [23].
There are many manufacturers developing resin cements with color and consistency appropriate for esthetic and efficient cementation. However, there are alternative materials to be used in prosthetic cementation. The greatest benefit of preheating composite resins is the reduction in viscosity, enabling the use for cementation of indirect restorations [28]. Clinically, it looks easier to apply than resin cements. Preheating of regular consistency resins also appears to reduce cement line thickness by 24% [28, 35]. Composite resins may perform better than resin cement on restoration margins due to more inorganic load filling and the long term color stability should be better because they do not have the autopolymerization reaction [28]. On the other hand, the benefits of preheating resin cements are still controversial. Lima et al. [70] observed that preheating of luting agents at 54 °C for 15 s reduced water sorption and oral solubility. Improvement in microtensile strength has been reported for dual-cure resin cements at 50 °C [86], because the monomeric conversion increasing following a specific light-activation, condition [93]. However, some authors have reported that heating at 60 °C was not beneficial [84], leading to hardening of RelyX Unicem cement before being dispensed from the syringe [87] or reduction of resin cement bonding in the root canal [85]. In contrast, other types of resin cements such as Panavia 2.0 and self-adhesives had their bond strength improved [87]. The divergence of results is probably due to differences in research methodologies and material composition, light-activation time, or even technical and operator variability.
Although some studies have reported that intraradicular temperature [94] and relative humidity [95] do not interfere in the bond strength, it is important to consider that despite the fact laboratory studies were careful and well-conducted, they do not bring clinical evidence. There are few case reports or clinical trials showing the advantages of preheating resinous materials in these conditions. Also, as mentioned above, according to Daronch et al. [40], when a compound is heated to 60 °C and removed from the heat source, its temperature drops 50% after 2 min and 90% after 5 min. So, the clinician must work very fast to ensure the least temperature drop possible. The clinician should dispense the material, adapt it, remove the excess and sculp it if necessary and light-cured while the material is still heated to obtain the advantages of higher monomeric conversion.
Another concern is related with time necessary for the composite resins stored in the refrigerator to reach room temperature. The clinician should wait at least 11 min before using composite within a compule stored in a refrigerator [72]. This time should be higher when the clinician uses a bigger compule or a syringe, for example.
Unlike resin materials, heating of glass ionomer cements promotes an increase in viscosity. Heating is believed to increase the ion diffusion rate, accelerating the reaction, reducing working time, and hardening time [82]. However, it can be seen that heating glass ionomer cements after mixing promotes an improvement in their physical and chemical properties. The heating of the ionomeric materials have been performed with LED light or mechanically energized with ultrasound and there was improvement in marginal adaptation; reduction in microleakage [30]; increase in flexural strength [9, 79], increase in microhardness [81], increase in bond strength [80], and acceleration of gelification reaction that protects the material in the early periods that are most critical against contamination with saliva [9]. Glass ionomer cement showed the smallest dimensional change when heated to 50 °C [67]. O’Brien [31] observed that the preheating of glass ionomer capsules before mixing had a better influence on the depth microhardness than heat application after mixing with ultrasound and LED light.
It is suggested that the heating of the glass ionomer cement after mixing promotes water evaporation and this promotes acceleration of the chemical reaction of the material [96]. The positive effect of preheating on the glass ionomer cement is not well established and clear yet, because there are few reports on this matter. The differences in the results can be attributed to complexity of the material setting reaction. It is known that the reaction of glass ionomer cement happens not only by the neutralization of polyacids but also the phosphates proved to be key components in the reaction [97, 98]. Also, any change in the proportion of components, such as the polyacid concentration, size, and shape of the glass particles may influence the end result of the reaction [99]. Preheating glass ionomer cement is also considered to be a safe procedure as it does not raise the pulp temperature significantly [29]. There are still few studies that make it clear whether heating of glass ionomer cement is really beneficial, so more research is needed to confirm this promising technique.
Despite the fact that the investigated commercial materials are not specifically designed for preheating/heating and more clinical results are necessary, heating or preheating is still a technique to be more investigated. There are new resins in the market like Viscalor [21, 36] designed specifically for preheating/heating with easy manipulation due to enhanced handling properties. Because the indication of injectable composite resin technique is increasing, further in vitro and in vivo studies are necessary to answer the performance of these new techniques and heated materials.
Conclusions
Based on the results of laboratory studies, preheating procedures for dental restorative materials is a simple, safe, and relatively successful technique. In general, for resinous materials, there is an increase in microhardness and degree of conversion, reduction in viscosity, and better adaptation to cavity walls. For ionomeric materials, heating promotes reduction of setting time, working time, and porosity and increase of microhardness. However, there is a lack of clinical research proving the advantages of indication of the preheating technique. In order to achieve good results, agility and training are necessary so the material would not lose heat until the restorative procedure. Also, care is necessary to avoid bubbles and formation of gaps, which compromises the best restoration performance.
References
de Amorim RG, Leal SC, Frencken JE (2012) Survival of atraumatic restorative treatment (ART) sealants and restorations: a meta-analysis. Clin Oral Investig 16(2):429–441. https://doi.org/10.1007/s00784-011-0513-3
Lempel EE, Tóth Á, Fábián T, Krajczár K, Szalma J (2015) Retrospective evaluation of posterior direct composite restorations: 10-year findings. Dent Mater 31(2):115–122. https://doi.org/10.1016/j.dental.2014.11.001
Mangani F, Marini S, Barabanti N, Preti A, Cerutti A (2015) The success of indirect restorations in posterior teeth: a systematic review of the literature. Minerva Stomatol. 64(5):231–240
De Souza GM, Braga RR, Cesar PF, Lopes GC (2015) Correlation between clinical performance and degree of conversion of resin cements: a literature review. J Appl Oral Sci 23(4):358–368. https://doi.org/10.1590/1678-775720140524
Dias AGA, Magno MB, Delbem ACB, Cunha RF, Maia LC, Pessan JP (2018) Clinical performance of glass ionomer cement and composite resin in Class II restorations in primary teeth: a systematic review and meta-analysis. J Dent 73(6):1–13. https://doi.org/10.1016/j.jdent.2018.04.004
Demarco FF, Collares K, Correa MB, de Cenci RR, Moraes MS, Opdam NJ (2017) Should my composite restorations last forever? Why are they failing? Braz Oral Res 31(suppl 1):92–99. https://doi.org/10.1590/1807-3107BOR-2017.vol31.0056
Cumerlato CBF, Demarco FF, Barros AJD, Peres MA, Peres KG, Cascaes AM, Camargo MBJ, dos Santos IS, Matijasevich A, Corrêa MB (2019) Reasons for direct restoration failure from childhood to adolescence: a birth cohort study. J Dent 89:103183. https://doi.org/10.1016/j.jdent.2019.103183
Ferracane JL (2011) Resin composite - state of the art. Dent Mater 27(1):29–38. https://doi.org/10.1016/j.dental.2010.10.020
Gorseta K, Borzabadi-Farahani A, Moshaverinia A, Glavina D, Lynch E (2017) Effect of different thermo–light polymerization on flexural strength of two glass ionomer cements and a glass carbomer cement. J Prosthet Dent 118(1):102–107. https://doi.org/10.1016/j.prosdent.2016.09.019
Rueggeberg FA, Giannini M, Arrais CAG, Price RBT (2017) Light curing in dentistry and clinical implications: a literature review. 31(suppl1):64–91. https://doi.org/10.1590/1807-3107BOR-2017.vol31.0061
Rosenberg JM (2017) Minimally invasive dentistry: a conservative approach to smile makeover. Compend Contin Educ Dent 38(1):38–42
Bausch JR, de Lange C, Davidson CL (1981) The influence of temperature on some physical properties of dental composites. J Oral Rehabil 8(4):309–317. https://doi.org/10.1111/j.1365-2842.1981.tb00505.x
Lovell LG, Newman SM, Bowman CN (1999) The effects of light intensity, temperature, and comonomer composition on the polymerization behavior of dimethacrylate dental resins. J Dent Res 78(8):1469–1476. https://doi.org/10.1177/00220345990780081301
Deb S, Di Silvio L, MacKler HE, Millar BJ (2011) Pre-warming of dental composites. Dent Mater 27(4):e51–e59. https://doi.org/10.1016/j.dental.2010.11.009
Tauböck TT, Tarle Z, Marovic D, Attin T (2015) Pre-heating of high-viscosity bulk-fill resin composites: effects on shrinkage force and monomer conversion. J Dent 43(11):1358–1364. https://doi.org/10.1016/j.jdent.2015.07.014
Fróes-Salgado NR, Silva LM, Kawano Y, Francci C, Reis A, Loguercio AD (2010) Composite pre-heating: Effects on marginal adaptation, degree of conversion and mechanical properties. Dent Mater 26(9):908–914. https://doi.org/10.1016/j.dental.2010.03.023
Dionysopoulos D, Papadopoulos C, Koliniotou-Koumpia E (2015) Effect of temperature, curing time, and filler composition on surface microhardness of composite resins. J Conserv Dent 18(2):114–118. https://doi.org/10.4103/0972-0707.153071
Theodoridis M, Dionysopoulos D, Koliniotou-Koumpia E, Dionysopoulos P, Gerasimou P (2017) Effect of preheating and shade on surface microhardness of silorane-based composites. J Investig Clin Dent 8(2):1–6. https://doi.org/10.1111/jicd.12204
Coelho NF, Barbon FJ, Machado RG, Bocato N, Moraes RR (2019) Response of composite resins to preheating and the resulting strengthening of luted feldspar ceramic. Dent Mater 35(10):1430–1438. https://doi.org/10.1016/j.dental.2019.07.021
Abdulmajeed AA, Donovan TE, Cook R, Sulaiman TA (2019) Effect of preheating and fatiguing on mechanical properties of bulk-fill and conventional composite resin. Oper Dent 45:387–395. https://doi.org/10.2341/19-092-l
Yang J, Silikas N, Watts DC (2019) Pre-heating effects on extrusion force, stickiness and packability of resin-based composite. Dent Mater 35(11):1594–1602. https://doi.org/10.1016/j.dental.2019.08.101
Davari A, Daneshkazemi A, Behniafar B, Sheshmani M (2014) Effect of pre-heating on microtensile bond strength of composite resin to dentin. J Dent 11(5):569–575
Sharafeddin F, Nouri H, Koohpeima F (2015) The effect of temperature on shear bond strength of Clearfil SE Bond and Adper Single Bond adhesive systems to dentin. J Dent 16(1):10–16
Mohammadi N, Jafari-Navimipour E, Kimyai S, Ajami AA, Bahari M, Ansarin M, Ansarin M (2016) Effect of pre-heating on the mechanical properties of silorane-based and methacrylate-based composites. J Clin Exp Dent 8(4):373–378. https://doi.org/10.4317/jced.52807
Vale MR, Afonso FA, Borges BC, Freitas AC Jr, Farias-Neto A, Almeida EO, Souza-Junior EJ, Geraldeli S (2014) Preheating impact on the degree of conversion and water sorption/solubility of selected single-bottle adhesive systems. Oper Dent 39(6):637–643. https://doi.org/10.2341/13-201-L
Sharafeddin F, Motamedi M, Fattah Z (2015) Effect of preheating and precooling on the flexural strength and modulus of elasticity of nanohybrid and silorane-based composite. J Dent 16:224–229
Theobaldo JD, Aguiar FHB, Pini NIP, Lima DANL, Liporoni PCS, Catelan A (2017) Effect of preheating and light-curing unit on physicochemical properties of a bulk fill composite. Clin Cosmet Investig Dent 9:39–43. https://doi.org/10.2147/CCIDE.S130803
Goulart M, Borges Veleda B, Damin D, Bovi Ambrosano GM, Coelho de Souza FH, Erhardt MCG (2018) Preheated composite resin used as a luting agent for indirect restorations: effects on bond strength and resin-dentin interfaces. Int J Esthet Dent 13(1):86–97
Gavic L, Gorseta K, Glavina D, Czarnecka B, Nicholson JW (2015) Heat transfer properties and thermal cure of glass-ionomer dental cements. J Mater Sci Mater Med 26(10):1–6. https://doi.org/10.1007/s10856-015-5578-0
Gorseta K, Glavina D, Skrinjaric I (2012) Influence of ultrasonic excitation and heat application on the microleakage of glass ionomer cements. Aust Dent J 57(4):453–457. https://doi.org/10.1111/j.1834-7819.2012.01724.x
O’Brien T, Shoja-Assadi F, Lea SC, Burke FJ, Palin WM (2010) Extrinsic energy sources affect hardness through depth during set of a glass-ionomer cement. J Dent 38(6):490–495. https://doi.org/10.1016/j.jdent.2010.03.004
OHAT (2015) OHAT Risk of bias rating tool for human and animal studies, 1–37. https://ntp.niehs.nih.gov/ntp/ohat/pubs/riskofbiastool_508.pdf. Accessed 14 Aug 2019
Holanda DB, França FM, do Amaral FL, Flório FM, Basting RT (2013) Influence of preheating the bonding agent of a conventional three-step adhesive system and the light activated resin cement on dentin bond strength. J Conserv Dent 16(6):536–539. https://doi.org/10.4103/0972-0707.120965
Reis A, Klein-Júnior CA, Accorinte M d L, Grande RH, dos Santos CB, Loguercio AD (2009) Effects of adhesive temperature on the early and 6-month dentin bonding. J Dent 37(10):791–798. https://doi.org/10.1016/j.jdent.2009.06.007
Dionysopoulos D, Tolidis K, Gerasimou P, Koliniotou-Koumpia E (2014) Effect of preheating on the film thickness of contemporary composite restorative materials. J Dent Sci 9(4):313–319. https://doi.org/10.1016/j.jds.2014.03.006
Yang J, Silikas N, Watts DC (2020) Pre-heating time and exposure duration: Effects on post-irradiation properties of a thermo-viscous resin-composite. Dent Mater 36(6):787–793. https://doi.org/10.1016/j.dental.2020.03.025
da Costa J, McPharlin R, Hilton T, Ferracane J (2009) Effect of heat on the flow of commercial composites. Am J Dent 22(2):92–96
Muñoz CA, Bond PR, Sy-Muñoz J, Tan D, Peterson J (2008) Effect of pre-heating on depth of cure and surface hardness of light-polymerized resin composites. Am J Dent 21(4):215–222
Wagner W, Asku M, Neme AML, Linger JB, Pink FE, Walker S (2008) Effect of pre-heating resin composite on restoration microleakage. Oper Dent 33(1):72–78. https://doi.org/10.2341/07-41
Daronch M, Rueggeberg FA, Moss L, de Goes MF (2006) Clinically relevant issues related to preheating composites. J Esthet Restor Dent 18(6):340–350. https://doi.org/10.1111/j.1708-8240.2006.00046.x
Karaarslan ES, Usumez A, Ozturk B, Cebe MA (2012) Effect of cavity preparation techniques and different preheating procedures on microleakage of class V resin restorations. Eur J Dent 6(1):87–94. https://doi.org/10.1055/s-0039-1698935
Kramer MR, Edelhoff D, Stawarczyk B (2016) Flexural strength of preheated resin composites and bonding properties to glass-ceramic and dentin. Materials (Basel) 9(2):83. https://doi.org/10.3390/ma9020083
Elsayad I (2009) Cuspal movement and gap formation in premolars restored with preheated resin composite. Oper Dent 34(6):725–731. https://doi.org/10.2341/09-012-L
El-Korashy DI (2010) Post-gel shrinkage strain and degree of conversion of preheated resin composite cured using different regimens. Oper Dent 35(2):172–179. https://doi.org/10.2341/09-072-L
Ayub KV, Santos GC Jr, Rizkalla AS, Bohay R, Pegoraro LF, Rubo JH, Santos MJ (2014) Effect of preheating on microhardness and viscosity of 4 resin composites. J Can Dent Assoc (Tor) 80:e12
Mundim FM, Garcia Lda F, Cruvinel DR, Lima FA, Bachmann L, Pires-de-Souza Fde C (2011) Color stability, opacity and degree of conversion of pre-heated composites. J Dent 39(Suppl 1):e25–e29. https://doi.org/10.1016/j.jdent.2010.12.001
Erhardt M, Goulart M, Jacques RC, Rodrigues JA, Pfeifer CS (2020) Effect of different composite modulation protocols on the conversion and polymerization stress profile of bulk-filled resin restorations. Dent Mater 36(7):829–837. https://doi.org/10.1016/j.dental.2020.03.019
Knezevic A, Zeljezic D, Kopjar N, Duarte S Jr, Par M, Tarle Z (2018) Toxicity of pre-heated composites polymerized directly and through CAD/CAM overlay. Acta Stomatol Croat 52(3):203–217. https://doi.org/10.15644/asc52/3/4
Tantbirojn D, Chongvisal S, Augustson DG, Versluis A (2011) Hardness and postgel shrinkage of preheated composites. Quintessence Int 42(3):51–60
El-Deeb HA, Abd El-Aziz S, Mobarak EH (2015) Effect of preheating of low shrinking resin composite on intrapulpal temperature and microtensile bond strength to dentin. J Adv Res 6(3):471–478. https://doi.org/10.1016/j.jare.2014.11.013
Demirbuga S, Ucar FI, Cayabatmaz M, Zorba YO, Cantekin K, Topçuoğlu HS, Kilinc HI (2016) Microshear bond strength of preheated silorane- and methacrylate-based composite resins to dentin. Scanning 38(1):63–69. https://doi.org/10.1002/sca.21242
Jafarzadeh-Kashi TS, Mirzaii M, Erfan M, Fazel A, Eskandarion S, Rakhshan V (2011) Polymerization behavior and thermal characteristics of two new composites at five temperatures: refrigeration to preheating. J Adv Prosthodont 3(4):216–220. https://doi.org/10.4047/jap.2011.3.4.216
Uctasli MB, Arisu HD, Lasilla LV, Valittu PK (2008) Effect of preheating on the mechanical properties of resin composites. Eur J Dent 2(4):263–268. https://doi.org/10.1055/s-0039-1697390
D’Amario M, De Angelis F, Vadini M, Marchili N, Mummolo S, D’Arcangelo C (2015) Influence of a repeated preheating procedure on mechanical properties of three resin composites. Oper Dent 40(2):181–189. https://doi.org/10.2341/13-238-L
D’Amario M, Pacioni S, Capogreco M, Gatto R, Baldi M (2013) Effect of repeated preheating cycles on flexural strength of resin composites. Oper Dent 38(1):33–38. https://doi.org/10.2341/11-476-L
Dionysopoulos D, Tolidis K, Gerasimou P (2016) The effect of composition, temperature and post-irradiation curing of bulk fill resin composites on polymerization efficiency. Mater Res 19(2):466–473. https://doi.org/10.1590/1980-5373-MR-2015-0614
Prasanna N, Pallavi RY, Kavitha S, Lakshmi Narayanan L (2007) Degree of conversion and residual stress of preheated and room-temperature composites. Indian J Dent Res 18(4):173–176
Choudhary N, Kamat S, Mangala TM, Thomas M (2011) Effect of pre-heating composite resin on gap formation at three different temperatures. J Conserv Dent 14(2):191–195. https://doi.org/10.4103/0972-0707.82618
Osternack FH, Caldas DB, Almeida JB, Souza EM, Mazur RF (2013) Effects of preheating and precooling on the hardness and shrinkage of a composite resin cured with QTH and LED. Oper Dent 38(3):50–57. https://doi.org/10.2341/11-411-l
Silva JC, Rogério Vieira R, Rege IC, Cruz CA, Vaz LG, Estrela C, Castro FL (2015) Pre-heating mitigates composite degradation. J Appl Oral Sci 23(6):571–579. https://doi.org/10.1590/1678-775720150284
da Silva-Júnior ME, de Fz LR, Bagnato VS, Tonetto MR, Simões F, Borges ÁH, Bandéca MC, de Andrade MF (2018) Effect of the curing temperature of dental composites evaluated with a fluorescent dye. J Contemp Dent Pract 19(1):3–12. https://doi.org/10.5005/JP-JOURNALS-10024-2204
Walter R, Swift EJ Jr, Sheikh H, Ferracane JL (2009) Effects of temperature on composite resin shrinkage. Quintessence Int 40(10):843–847
Gugelmin BP, Miguel L, Baratto Filho F, Cunha L, Correr GM, Gonzaga CC (2020) Color stability of ceramic veneers luted with resin cements and pre-heated composites: 12 months follow-up. Braz Dent J 31(1):69–77. https://doi.org/10.1590/0103-6440202002842
Lohbauer U, Zinelis S, Rahiotis C, Petschelt A, Eliades G (2009) The effect of resin composite pre-heating on monomer conversion and polymerization shrinkage. Dent Mater 25(4):514–519. https://doi.org/10.1016/j.dental.2008.10.006
Marcinkowska A, Gauza-Wlodarczyk M, Kubisz L, Hedzelek W (2017) The electrical properties and glass transition of some dental materials after temperature exposure. J Mater Sci Mater Med 28(12):186. https://doi.org/10.1007/s10856-017-5996-2
Elkaffass AA, Eltoukhy RI, Elnegoly SA, Mahmoud SH (2020) Influence of preheating on mechanical and surface properties of nanofilled resin composites. J Clin Exp Dent 12(5):e494–e500. https://doi.org/10.4317/jced.56469
Yan Z, Sidhu SK, Carrick TE, McCabe JF (2007) Response to thermal stimuli of glass ionomer cements. Dent Mater 23(5):597–600. https://doi.org/10.1016/j.dental.2006.05.001
Ebrahimi Chaharom ME, Bahari M, Safyari L, Safarvand H, Shafaei H, Jafari Navimipour E, Alizadeh Oskoee P, Ajami AA, Abed Kahnamouei M (2020) Effect of preheating on the cytotoxicity of bulk-fill composite resins. J Dent Res Dent Clin Dent Prospects 14(1):19–25. https://doi.org/10.34172/joddd.2020.003
Karacan AO, Ozyurt P (2019) Effect of preheated bulk-fill composite temperature on intrapulpal temperature increase in vitro. J Esthet Restor Dent 31(6):583–588. https://doi.org/10.1111/jerd.12503
Lima MO, Catelan A, Marchi GM, Lima DANL, Martins LRM, Aguiar FHB (2018) Influence of pre-heating and ceramic thickness on physical properties of luting agents. J Appl Biomater Funct Mater 16:252–259. https://doi.org/10.1177/2280800018782842
Trujillo M, Newman SM, Stansbury JW (2004) Use of near-IR to monitor the influence of external heating on dental composite photopolymerization. Dent Mater 20(8):766–777. https://doi.org/10.1016/j.dental.2004.02.003
Lucey S, Lynch CD, Ray NJ, Burke FM, Hannigan A (2010) Effect of pre-heating on the viscosity and microhardness of a resin composite. J Oral Rehabil 37(4):278–282. https://doi.org/10.1111/j.1365-2842.2009.02045.x
Daronch M, Rueggeberg F, De Goes MF (2005) Monomer conversion of pre-heated composite. J Dent Res 84(7):663–667. https://doi.org/10.1177/154405910508400716
dos Santos RE, Lima AF, Soares GP, Ambrosano GM, Marchi GM, Lovadino JR, Aguiar FH (2011) Effect of preheating resin composite and light-curing units on the microleakage of class II restorations submitted to thermocycling. Oper Dent 36(1):60–65. https://doi.org/10.2341/10-226-LR1
Watts DC, Alnazzawi A (2014) Temperature-dependent polymerization shrinkage stress kinetics of resin-composites. Dent Mater 30(6):654–660. https://doi.org/10.1016/j.dental.2014.03.004
Jongsma LA, Kleverlaan CJ (2015) Influence of temperature on volumetric shrinkage and contraction stress of dental composites. Dent Mater 31(6):721–725. https://doi.org/10.1016/j.dental.2015.03.009
Abed Kahnamouei M, Gholizadeh S, Rikhtegaran S, Daneshpooy M, Kimyai S, Alizadeh Oskoee P, Rezaei Y (2017) Effect of preheat repetition on color stability of methacrylate- and silorane-based composite resins. J Dent Res Dent Clin Dent Prospects 11(4):222–228. https://doi.org/10.15171/joddd.2017.039
Ahn KH, Lim S, Kum KY, Chang SW (2015) Effect of preheating on the viscoelastic properties of dental composite under different deformation conditions. Dent Mater J 34(5):702–706. https://doi.org/10.4012/dmj.2015-042
Fabián Molina G, Cabral RJ, Mazzola I, Brain Lascano L, Frencken JE (2013) Biaxial flexural strength of high-viscosity glass-ionomer cements heat-cured with an LED lamp during setting. Biomed Res Int 2013:1–6. https://doi.org/10.1155/2013/838460
Goršeta K, Škrinjarić T, Glavina D (2012) The effect of heating and ultrasound on the shear bond strength of glass ionomer cement. Coll Antropol 36(4):1307–1312
Dionysopoulos D, Tolidis K, Sfeikos T, Karanasiou C, Parisi X (2017) Evaluation of surface microhardness and abrasion resistance of two dental glass ionomer cement materials after radiant heat treatment. Adv Mater Sci Eng 2017:1–8. https://doi.org/10.1155/2017/5824562
Algera TJ, Kleverlaan CJ, Prahl-Andersen B, Feilzer AJ (2006) The influence of environmental conditions on the material properties of setting glass-ionomer cements. Dent Mater 22(9):852–856. https://doi.org/10.1016/j.dental.2005.11.013
Khoroushi M, Karvandi TM, Sadeghi R (2012) Effect of prewarming and/or delayed light activation on resin-modified glass ionomer bond strength to tooth structures. Oper Dent 37(1):54–62. https://doi.org/10.2341/11-137-L
Cantoro A, Goracci C, Carvalho CA, Coniglio I, Ferrari M (2009) Bonding potential of self-adhesive luting agents used at different temperatures to lute composite onlays. J Dent 37(6):454–461. https://doi.org/10.1016/j.jdent.2009.02.006
Alizadeh Oskoee P, Nooroloyouni A, Pornaghi Azar F, Sajjadi Oskoee J, Pirzadeh Ashraf A (2015) Effect of resin cement pre-heating on the push-out bond strength of fiber post to root canal dentin. J Dent Res Dent Clin Dent Prospects 9(4):233–238. https://doi.org/10.15171/joddd.2015.042
Morais A, dos Santos ARA, Giannini M, Reis AF, Rodrigues JA, Arrais CAG (2012) Effect of pre-heated dual-cured resin cements on the bond strength of indirect restorations to dentin. Braz Oral Res 26(2):170–176. https://doi.org/10.1590/S1806-83242012000200014
Cantoro A, Goracci C, Papacchini F, Mazzitelli C, Fadda GM, Ferrari M (2008) Effect of pre-cure temperature on the bonding potential of self-etch and self-adhesive resin cements. Dent Mater 24(5):577–583. https://doi.org/10.1016/j.dental.2007.06.012
Gross DJ, Dávila-Sánchez A, Runnacles P, Zarpellon DC, Kiratcz F, Campagnoli EB, Alegría-Acevedo LF, Coelho U, Rueggeberg FA, Arrais C (2020) In vivo temperature rise and acute inflammatory response in anesthetized human pulp tissue of premolars having Class V preparations after exposure to Polywave® LED light curing units. Dent Mater S0109-5641(20):30168–30168. https://doi.org/10.1016/j.dental.2020.05.015
Daronch M, Rueggeberg FA, De Goes MF, Giudici R (2006) Polymerization kinetics of pre-heated composite. J Dent Res 85(1):38–43. https://doi.org/10.1177/154405910608500106
Almeida LN, Mendes GAM, Favarão IN, Kasuya AVB, Borges MG, Menezes MS, Fonseca RB (2018) Influence of preheating and post-curing on a novel fiber-reinforced composite post material. Braz Oral Res 32:e97. https://doi.org/10.1590/1807-3107bor-2018.vol32.0097
Zhao S, Qian Y, Liu H, Jiang L, Zhou L (2012) The effect of preheating on light cured resin composites. J Hard Tissue Biol 21(3):273–278. https://doi.org/10.2485/jhtb.21.273
Ban S, Takahashi Y, Tanase H, Hasegawa J (1990) Heat curing investigated behavior of light-cured by dynamic differential composite resins scanning calorimetry. Dent Mater J 9(2):153–162. https://doi.org/10.4012/dmj.9.153
França FÁ, de Oliveira M, Rodrigues JA, Arrais CAG (2011) Pre-heated dual-cured resin cements: analysis of the degree of conversion and ultimate tensile strength. Braz Oral Res 25(2):174–179. https://doi.org/10.1590/S1806-83242011000200013
Caiado ACRL, Azevedo CGS, Giannini M, De Goes MF, Rueggeberg FA (2019) In vivo measurement of root canal wall temperature at different stages prior to fiber post cementation. Eur J Dent 13(1):69–74. https://doi.org/10.1055/s-0039-1688539
Saraiva LO, Aguiar TR, Costa L, Cavalcanti AN, Giannini M, Mathias P (2015) Influence of intraoral temperature and relative humidity on the dentin bond strength: An in situ study. J Esthet Restor Dent 27(2):92–99. https://doi.org/10.1111/jerd.12098
Nicholson JW, Czarnecka B (2009) Role of aluminum in glass-ionomer dental cements and its biological effects. J Biomater Appl 24(4):293–308. https://doi.org/10.1177/0885328209344441
Wasson EA, Nicholson JW (1993) New aspects of the setting of glass-ionomer cements. J Dent Res 72(2):481–483. https://doi.org/10.1177/00220345930720020201
Shahid S, Billington RW, Pearson GJ (2008) The role of glass composition in the behaviour of glass acetic acid and glass lactic acid cements. J Mater Sci Mater Med 19(2):541–545. https://doi.org/10.1007/s10856-007-0160-z
Xie D, Brantley WA, Culbertson BM, Wang G (2000) Mechanical properties and microstructures of glass-ionomer cements. Dent Mater 16(2):129–138. https://doi.org/10.1016/S0109-5641(99)00093-7
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lopes, L.C.P., Terada, R.S.S., Tsuzuki, F.M. et al. Heating and preheating of dental restorative materials—a systematic review. Clin Oral Invest 24, 4225–4235 (2020). https://doi.org/10.1007/s00784-020-03637-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-020-03637-2