Abstract
Objective
The aim of this systematic review was to explore the efficacy of different minimal invasive surgical (MIS) and non-surgical (MINST) approaches for the treatment of intra-bony defect in terms of clinical attachment level (CAL) gain and periodontal pocket depth (PPD) reduction.
Methods
A detailed review protocol was designed according to PRISMA guideline. Online search was conducted on PubMed, Cochrane library and Embase. Only randomized clinical trials (RCTs) testing MIS or MINST procedure, with or without the application of a regenerative tool for the treatment of intra-bony defect, were included. Cochrane checklist for risk of bias assessment was used. Network meta-Analysis (NMAs) was used to rank the treatment efficacy.
Results
Nine RCTs accounting for 244 patients and a total of 244 defects were included. Only two studies were at low risk of bias. CAL gain for included treatment ranged from 2.58 ± 1.13 mm to 4.7 ± 2.5 mm while PPD reduction ranged from 3.19 ± 0.71 mm to 5.3 ± 1.5 mm. On the basis of the ranking curve, MINST showed the lowest probability to be the best treatment option for CAL gain. Pairwise comparisons and treatment rankings suggest superiority for regenerative approaches (CAL difference 0.78 mm, (0.14–1.41); P < 0.05) and surgical treatment elevating only the buccal or palatal flap (CAL difference: 0.95 mm, (0.33–1.57); P < 0.05).
Conclusions
Minimally invasive surgical (MIS) and non-surgical (MINST) periodontal therapy show promising results in the treatment of residual pocket with intra-bony defect.
Clinical relevance
MIS procedures represent a reliable treatment for isolated intra-bony defect.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Residual periodontal pockets following cause-related therapy are associated with risk of disease progression during supportive periodontal therapy and further surgical treatment is strongly recommended [1]. Among the possible surgical treatment modalities, periodontal regeneration for the treatment of residual intra-bony defect is aimed to restore lost periodontal tissues favouring clinical attachment level (CAL) gain and bone fill along with periodontal pocket depth (PPD) reduction [2, 3]. Several clinical studies showed higher benefits of periodontal regeneration compared with access flaps in term of clinical and radiographic parameters [3,4,5,6,7]. Among the possible regenerative tools, the use of barrier membranes or enamel matrix proteins is associated with true histological regeneration and generalizability of clinical outcomes [8, 9]. Optimal stability of the outcomes has been confirmed at the 10-year follow-up for compliant patients enrolled in supportive periodontal care program [10].
In the last two decades, a growing body of evidence has demonstrated the influence of such factors on clinical outcomes of periodontal regeneration, including patient-related factors as smoking habits and residual plaque level along with surgical-related factors as the use of papillary preservation flaps to maintain the primary closure over the treated intra-bony defect. The reduction of surgical flap extension along with papilla preservation (minimal invasive surgery-MIS) has been suggested to improve wound stability and reduce morbidity [11, 12], showing promising benefits in improving periodontal parameters [13]. Subsequent modifications of the original technique included further reduction of flap extension alone or in combination with biomaterials and/or biologicals and with minimal elevation of interdental papilla over the defect [14, 15]. Cohort studies and early RCTs demonstrated the reliability of these techniques in the treatment of residual pockets with associated intra-bony defect [16, 17]. Minimally invasive non-surgical techniques (MINST) were also introduced to manage single intra-bony defects in order to accomplish an optimal root debridement with no flap elevation at the corresponding defect [18, 19]. To date, no systematic evaluation of the possible benefit of minimally invasive periodontal therapy has been tested in a meta-analysis.
The aim of this systematic review was to explore and to rank the efficacy of minimal invasive surgical (MIS) and non-surgical (MINST) treatments for single intra-bony defect applying a network meta-analysis (NMA) using both direct and indirect evidence from RCTs.
Materials and methods
Protocol development
A detailed review protocol was designed according to the PRISMA (preferred reporting items for systematic review and meta-analyses) extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions [20, 21].
The focused question of this systematic review was the following: what is the efficacy of minimal invasive surgical (MIS) and non-surgical (MINST) treatments for single intra-bony defect applying a network meta-analysis (NMA) using both direct and indirect evidence from RCTs.
Eligibility criteria
Criteria used in this systematic review (SR) for studies’ selection were based on the PICOS method and were the following:
(P) Type of Participants: patients with a clinical diagnosis of periodontal disease, presenting at least one isolated inter-dental intra-bony defect detected clinically or on X-ray after revaluation of causal therapy.
(I) Type of Interventions: any type of minimally invasive surgical (MIS) approach alone or in combination with regenerative tool (biomaterials, membranes, wound enhancers or combinations) or any type of minimally invasive non-surgical therapy (MINST) alone or in combination with any type of wound modulators. MIS therapy was considered only when preservation of interdental soft tissue, limited mesio-distal extension of the flap and no use of vertical incisions was clearly specified in the text by the author. MINST procedure was considered when a site-specific treatment aimed to careful root debridement was performed applying specific instrumentations under magnification system.
(C) Comparison between interventions: any type of possible comparison between the interventions proposed in the included RCTs applying network meta-analysis (NMA), thus ranking the outcomes of all included treatments.
(O) Type of Outcome measures: primary outcome was CAL gain. Secondary outcomes were PPD reduction, REC, tooth loss and pocket closure.
Only RCTs published in English language and with at least 6 months of follow-up were considered.
Studies treating single intra-bony defect not using a MIS or a MINST, treating multiple defects, treating furcation defects were not considered in this review.
Information sources and search
Three online databases (PubMed MEDLINE, Cochrane Central Register of Controlled Trials (CENTRAL) and EMBASE) were checked up to and including March 2019. A detailed search protocol is presented in supplementary material 1.
Additionally, hand search covering the last 10 years was performed on Journal of Clinical Periodontology, Journal of Periodontology, Clinical Oral Investigations, The International Journal of Periodontics and Restorative Dentistry and Journal of Periodontal Research. The references of included and relevant papers were checked for possible additional studies, and authors were contacted to clarify any doubt about data.
Study selection and data collection process
After duplicates’ removal, the titles and abstracts were independently screened by two review authors (LB, FS). For the studies meeting the inclusion criteria and in case of insufficient data from the abstract, the full text was obtained. Eligibility process was then conducted on full text to identify all studies meeting the inclusion criteria. The inter-rater agreement for article inclusion between reviewers was calculated. Disagreements were solved by discussion with a third reviewer (MLM). Two investigators (LB, FS) independently extracted data from included full-text papers using apposite case-report form. All investigators reviewed all data to ensure accuracy before analysis.
Outcome measures
Clinical attachment level (CAL) gain, periodontal pocket depth (PPD) reduction and gingival recession (REC) had to be expressed as the average difference baseline/follow-up of the treated sites in millimetres. The reviewers did not make any additional calculations on CAL gain, PPD reduction and REC.
Tooth loss had to be reported as the number of teeth lost during the follow-up. Pocket closure was defined as PPD ≤ 4 mm at final follow-up.
Risk of bias in individual studies
Two review authors (LB, ZK) performed the quality assessment of the included studies using the tools for assessing risk of bias of Cochrane Handbook for Systematic Reviews of Interventions. Disagreements were solved by discussion [22]. Seven main quality criteria were examined: sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessors, incomplete outcome data and selective outcome reporting.
Risk of bias in the included studies was categorised as below:
- (A)
Low risk of bias (plausible bias unlikely to seriously alter the results) if all criteria were met.
- (B)
Unclear risk of bias (plausible bias that raises some doubt about the results) if one or more criteria were partly met.
- (C)
High risk of bias (plausible bias that seriously weakens confidence in the results) if one or more criteria were not met.
Data synthesis and network meta-analysis
The examined outcomes were continuous variables; therefore, the estimate of effect for each treatment was expressed as mean and standard deviation (SD). The statistical unit was the patient.
Considering the presence of several and heterogeneous interventional approaches not allowing a standard meta-analysis, a network meta-analysis (NMA) was planned. The NMA allows for comparison of more than two interventions simultaneously, as well as for indirect comparison between interventions when no direct comparison from original studies is available. Furthermore, NMA allows ranking of the treatments considering the corresponding probability of being the best approach [23].
Two different hypotheses of data synthesis were planned in two separated NMA:
- (a)
to compare and rank all surgical and not surgical treatment without categories to identify the most performing approach.
- (b)
to explore the influence of the flap extension and of the adding of regeneration tool on MIS procedure. For this second NMA, the treatments were clustered into four groups as below:
raising the sole flap at both sides,
raising the flap at both sides with a regenerative tool applied,
raising a single flap only at buccal or palatal side,
raising a single flap only at buccal or palatal side with a regenerative tool applied.
Following a network meta-analysis frame, the direct comparisons between treatments were visually represented through a network diagram. Briefly, the nodes represent the treatments while connecting lines represent the direct evidence (i.e. comparison among treatments) [24]. Trials not connected in the diagram were excluded from the NMA.
Network meta-analysis summary treatment effects with their 95% confidence interval were calculated for each pairwise comparison. The overall rank score for the effectiveness of each treatment in terms of a specific outcome was expressed through cumulative rank probabilities and expressed as surface under the cumulative ranking curve (SUCRA). The higher the surface under the curve, the higher the probability to be the best treatment [23].
Prior to conducting a NMA, the assumptions of transitivity and consistency between comparisons were examined [24, 25]. The transitivity assumption was evaluated by checking relevant differences between studies in terms of inclusion criteria, patients’ characteristics, interventions and methodology. Potential sources of heterogeneity were identified, and distribution of effect modifiers was conceptually evaluated. When substantial differences were identified, data syntheses were not to be implemented. To assess the presence of statistical inconsistency, both local and global approaches were considered. When closed loops of interventions were present (information from direct and indirect comparison), consistency was planned to be estimated through the loop-specific method using the ifplot command on Stata. The global inconsistency was to be assessed using a design-by-intervention interaction model [25].
All statistical analyses and summarizing graphics were generated using the network package routines in the Stata 13 (Stata Statistical Software, release 13.0, StataCorp).
Results
Study selection and characteristics
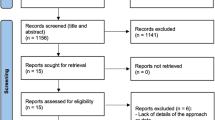
The electronic search provided a total of 4231 titles. The hand search provided 5 additional articles. The screening process left 197 articles, and 9 were included in the review. Inter-rater agreement for study selection estimated through Cohen’s kappa was 94.42% (kappa = 0.531). The PRISMA flow chart of the screening and selection process is reported in supplementary material 2.
A total of 244 patients and 244 treated intra-bony defects were finally included in the SR.
According to description by authors, two main clusters of surgical approaches were considered after analysis of included studies:
MIS raising the papilla at both buccal and palatal side: minimally invasive surgical technique (MIST) and the double flap approach (DFA).
MIS raising the papilla only at buccal or palatal side: modified-MIST (M-MIST) and the single flap approach (SFA)
Additionally, enamel matrix derivative (EMD), grow factors (GF), dental pulp stem cells (DPSCs), xenograft (demineralized bovine bone mineral; DBBM), hydroxyapatite (HA), beta-tricalcium phosphate (b-TCP) and collagen membrane (CM) were used as regenerative tool alone or in possible combinations.
Fourteen different treatment combinations were identified from the included studies. Outcomes and characteristics of the included studies are reported in Table 1. All had short-term (6–24 months) follow-up. No tooth loss was reported in the included studies. Only two included studies reported data on pocket closures (Table 1).
Risk of bias in the included studies
Two studies [18, 26] were at low risk of bias, six [16, 27,28,29,30,31] were at unclear and one [32] at high risk (Supplementary material 3).
Summary of network geometry
The first NMA aimed to explore the efficacy of different procedures and included 7 studies [16, 18, 26, 29,30,31,32]. Two studies [27, 28] were excluded from this NMA because had no common treatment comparison with the included studies.
Network meta-analysis was conducted for the three outcomes CAL gain, PPD reduction and REC. Because specific pairwise comparisons were present in no more than 2 studies, single meta-analysis was not conducted.
Interventions investigated in the included studies were classified into the following categories:
- 1.
MIST/DFA
- 2.
M-MIST/SFA
- 3.
M-MIST/SFA + HA + CM
- 4.
M-MIST/SFA + EMD
- 5.
M-MIST/SFA + EMD + DBBM
- 6.
MIST/DFA + EMD
- 7.
MINST
- 8.
MIST/DFA + DPSCs
- 9.
MINST + EMD
For the three outcomes, the same studies were included in the NMA, and direct, indirect and mixed effect pairwise comparisons between interventions were conducted. The generated network was mainly a star shape and including only one closed loop (Fig. 1a).
a Network plot for fist NMA. b Network plot for second NMA. MIST, minimally invasive surgical technique; M-MIST, modified-MIST; SFA, single flap approach; DFA, double flap approach; MINST, minimally invasive non-surgical technique; EMD, enamel matrix derivative; DBBM, demineralized bovine bone mineral; DPSCs, dental pulp stem cells; CM, collagen membrane; rh-PDGF-bb, recombinant human-derived platelet growth factor; bTCP, beta tricalcium phosphate; HA, hydroxyapatite
The second NMA aimed to explore the influence of the surgical techniques and of the regenerative tools. For this analysis, 6 studies were included [16, 26, 28, 30,31,32]. Interventions were grouped into the aforementioned categories:
- 1.
MIST/DFA
- 2.
MIST/DFA + regenerative tool
- 3.
M-MIST/SFA
- 4.
M-MIST/SFA + regenerative tool
Similarly, to the first NMA, no single pairwise meta-analysis was possible because of the limited number of studies. The generated network plot was a 4-node closed loop (Fig. 1b). Network meta-analysis was conducted for the three outcomes CAL gain, PPD reduction and REC.
Results of the NMA
For the first NMA, all pairwise summary comparisons with respective summary estimates and 95% CI for CAL gain and PPD reduction are represented in Figs. 2 and 3, respectively. In terms of CAL gain, the majority of pairwise comparisons produced differences of no particular statistical or clinical relevance (all 95% CI crossing the no-effect line) excepting for M-MIST/SFA vs MIST/DFA (mean 0.85 mm; 95% CI 0.07, 1.63).
CAL pairwise comparisons for first NMA (see legend in Fig. 1)
PPD reduction pairwise comparisons for first NMA (see legend in Fig. 1)
For PPD, the same pairwise comparison resulted significant (mean 0.92 mm; 95% CI 0.13, 1.70) alongside with M-MIST/DFA + DPSCs vs MIST/DFA (mean 0.94; 95% CI 0.17, 1.71), MINST vs M-MIST/SFA (mean − 1.28; 95% CI − 2.37, − 0.18) and MIST/DFA + DPSCs vs MINST (mean 1.30; 95% CI 0.21, 2.38).
Based on ranking calculation, M-MIST/SFA and M-MIST/SFA + EMD had the greatest likelihood of being the most effective treatment for CAL gain and PPD reduction. The MINST group showed the lowest probability of being the best treatment (Table 2). REC increase showed difference of no particular statistical or clinical interest for all pairwise comparisons (Supplementary material 4).
For the second NMA, the pairwise comparisons for CAL gain favours the M-MIST/SFA (mean 0.95; 95% CI 0.33, 1.57) and M-MIST/SFA + regenerative tool groups (mean 0.78; 95% CI 0.14, 1.41) compared with the MIST/DFA group. These differences were statistically significant (95% CI not crossing the no-effect line; Figs. 4 and 5). Pairwise comparisons for PPD reduction showed similar outcomes.
PPD reduction pairwise comparisons for second NMA (see legend in Fig. 4)
The surface under the cumulative ranking curve showed the highest probabilities for M-MIST/SFA to be the most effective treatment followed by MIST/SFA + regeneration (Table 3). REC increase showed difference of no particular statistical interest (Supplementary material 4).
The transitivity was estimated conceptually, and no relevant sources of heterogeneity were identified between studies. In terms of inconsistency, as every treatment was informed by a very limited number of studies, statistical calculation of inconsistency factors was not possible. Considering the large contribution that indirect evidence had on the overall effect estimate, NMA was conducted following an inconsistency model [33].
Discussion
Intra-bony defects associated with residual periodontal pockets predict disease progression and tooth loss in the long term [1, 34]. SRs investigating the efficacy of regenerative strategies applied to treat intra-bony defects reported the superiority of these approaches compared with open flap surgery alone [4, 35,36,37]. Improvements of regenerative approaches in terms of reduction of patient morbidity and clinical parameters were recently proposed [13, 14]. These techniques, frequently supported by specific instruments and magnification systems, promote periodontal regeneration and related clinical outcomes, enhancing stability of the wound area after surgery [11]. Even if different modifications have been described [15, 16], this group of surgical procedures was characterized by the complete papilla preservation and minimal flap reflection. Prospective trials supported the efficacy of these procedures with significant CAL gain and PPD reduction [16, 17]. Moreover, non-surgical minimally invasive treatments under magnification have been also proposed [19].
The present SR explored and ranked the efficacy of minimally invasive periodontal techniques for the treatment of single intra-bony defect in terms of CAL gain and PPD reduction, including surgical and non-surgical approaches. Nine RCTs accounting for 244 patients and a total of 244 defects were included. Only two studies were rated at low risk of bias. All the included studies used at least a MIS technique in one of the study harm. Surgical procedures yielded to a significant mean CAL gain ranging from 2.80 ± 1.14 mm to 4.7 ± 2.5 mm and PPD reduction ranging from 3.4 ± 1.7 mm to 5.3 ± 1.5 mm. These data support the efficacy of MIS in improving clinical variables, even if a consistent heterogeneity among studies has been reported.
The first NMA was aimed to rank the efficacy of all investigated treatments. The groups M-MIST/SFA and M-MIST/SFA + EMD showed higher probabilities to be the best treatment, only M-MIST/SFA group was better than the MIST/DFA in both pairwise comparison for CAL gain (difference: 0.85 mm (0.07–1.63); P < 0.05) and PPD reduction (difference: 0.92 mm (0.13–1.70); P < 0.05). The present data seems to suggest that flap design and primary wound stability are more critical than adding a regenerative tool by itself into the defect. This observation confirmed data of a previous SR showing that papilla preservation flap yielded to significant higher CAL gain than that of classical flap surgery [38].
Interestingly, two of the included studies compared a surgical procedure with MINST [18, 19]. Non-surgical techniques showed the lowest probability to be the best treatment on this SR, and this seems to confirm the higher magnitude of clinical benefits in applying surgery to accomplish root debridement at intra-bony defect [39]. On the contrary, considering data from a single study enclosed in this SR comparing surgical and non-surgical treatment, a small clinical difference was reported in terms of CAL gain (2.58 ± 1.3 mm MINST vs 2.80 ± 1.14 mm MIST). Additionally, using a non-surgical approach, a mean CAL gain of 3.5 mm was reported in a 5-year prospective study [40], and this finding seems to support the stability of achieved outcomes when a stringent supportive periodontal care program is performed.
Reported differences in this study may be explained by a number of reasons, as depth of pockets and anatomy of involved defect, that may have affected outcomes. However, only a limited number of RCTs clarified details of defect configuration in entry criteria [16, 30, 32]. Due to limited and heterogenous information, no further analysis is possible, and this may be considered as a limit of the study. However, the reader should keep in mind that prevalently, 3-wall configuration or defects with minimal extension at palatal side are associated with improved wound stability and better clinical outcomes, and this may have influenced the outcomes of minimally invasive treatments.
Along the possible clinical benefits, it is mandatory to analyse the cost and the morbidity of the procedures. Data from this SR are inconclusive. In studies comparing MIS vs MINST [18, 19], treatment chair time was significantly higher for MIS approaches. On the other hand, no statistically significant difference in terms of hardship perception of the procedure and pain/discomfort during the first week after surgery was reported. Further investigations to explore cost-benefit ratio MIS and MINST are mandatory.
The second NMA was aimed to explore the influence of the surgical technique and the use of regeneration tools, clustering the papilla elevation only at buccal/palatal side or at both sides and adding or not a regenerative tool. The outcomes of this NMA showed superior results in terms of CAL gain for studies elevating the flap only at buccal/palatal side with or without a regenerative tool applied compared with the studies elevating the flap at both sides (M-MIST/SFA vs MIST/DFA; difference: 0.95 mm (0.33–1.57]; P < 0.05) (M-MIST/SFA + regenerative tool vs MIST/DFA; difference: 0.78 mm (0.14 to 1.41); P < 0.05). It can be speculated that flap surgery involving both buccal and lingual sides decreases wound stability thus hindering the healing process. However, the reader should consider some possible factors incorporated from the single studies that may condition review outcomes, as depth of pockets and anatomy of involved defect. Furthermore, the experimental cluster in NMA grouped several techniques that may lead to possible heterogeneity among procedures (i.e. growth factor, EMD, HA, DBBM) thus limiting the clinical relevance of these results. Conversely, when applying a double flap approach, the addition of regenerative device improves the outcomes compared with the flap surgery alone, thus suggesting the importance of biomaterials in stabilizing the wound area when an access at both sides is mandatory due to extension of the treated defect. Finally, when assessing literature regarding regeneration, it should be taken in mind also that a significant heterogeneity may exist among different clinical centres, thus impacting on the reported outcomes [3].
Limits
The major limit of this review was the great heterogeneity of the techniques in the included studies and the lack of at least two studies comparing the same techniques, thus hindering the possibility to perform a standard meta-analysis.
Furthermore, studies with low risk of bias and long-term outcomes are mandatory.
Conclusions
In conclusion, this study suggests the following:
- 1.
Minimally invasive surgical (MIS) and non-surgical (MINST) periodontal therapy showed promising results in the treatment of residual pocket associated with intra-bony defect.
- 2.
Among surgical procedures, techniques with single flap approach and papilla preservation (M-MIST/SFA) seem to provide better outcomes than the double flap (MIST/DFA).
- 3.
Considering the heterogeneity among included studies, further investigations are necessary to evaluate the possible generalizability of the outcomes.
References
Matuliene G, Pjetursson BE, Salvi GE, Schmidlin K, Brägger U, Zwahlen M, Lang NP (2008) Influence of residual pockets on progression of periodontitis and tooth loss: results after 11 years of maintenance. J Clin Periodontol 35:685–695. https://doi.org/10.1111/j.1600-051X.2008.01245.x
Pagliaro U, Nieri M, Rotundo R et al (2008) Italian Society of Periodontology. Clinical guidelines of the Italian Society of Periodontology for the reconstructive surgical treatment of angular bony defects in periodontal patients. J Periodontol 79(12):2219–2232. https://doi.org/10.1902/jop.2008.080266
Cortellini P, Tonetti MS (2015) Clinical concepts for regenerative therapy in intrabony defects. Peridontology 2000(68):282–307. https://doi.org/10.1111/prd.12048
Needleman IG, Worthington HV, Giedrys-Leeper E, Tucker RJ (2006) Guided tissue regeneration for periodontal infra-bony defects. Cochrane Database Syst Rev 19:CD001724. https://doi.org/10.1002/14651858.CD001724.pub2
Sanz M, Tonetti MS, Zabalegui I, Sicilia A, Blanco J, Rebelo H, Rasperini G, Merli M, Cortellini P, Suvan JE (2004) Treatment of intrabony defects with enamel matrix proteins or barrier membranes: results from a multicenter practice-based clinical trial. J Periodontol 75(5):726–733. https://doi.org/10.1902/jop.2004.75.5.726
Tonetti MS, Lang NP, Cortellini P et al (2002) Enamel matrix proteins in the regenerative therapy of deep intrabony defects. J Clin Periodontol 29(4):317–325
Esposito M, Grusovin MG, Papanikolaou N, Coulthard P, Worthington HV (2009) Enamel matrix derivative (Emdogain(R)) for periodontal tissue regeneration in intrabony defects. Cochrane Database Syst Rev Oct 7(4):CD003875. https://doi.org/10.1002/14651858.CD003875.pub3
Tonetti MS, Cortellini P, Susan JE, Suvan JE, Adriaens P, Baldi C, Dubravec D, Fonzar A, Fourmousis I, Magnani C, Muller-Campanile V, Patroni S, Sanz M, Vangsted T, Zabalegui I, Pini Prato G, Lang NP (1998) Generalizability of the added benefits of guided tissue regeneration in the treatment of deep intrabony defects. Evaluation in a multi-center randomized controlled clinical trial. J Periodontol 69(11):1183–1189. https://doi.org/10.1902/jop.1998.69.11.1183
Reynolds MA, Kao RT, Camargo PM et al (2015) Periodontal regeneration – intrabony defects: a consensus report from the AAP regeneration workshop. J Periodontol Feb 86(2 Suppl):S105–S107. https://doi.org/10.1902/jop.2015.140378
Sculean A, Kiss A, Miliauskaite A, Schwarz F, Arweiler NB, Hannig M. (2008) Ten-year results following treatment of intra-bony defects with enamel matrix proteins and guided tissue regeneration. J Clin Periodontol. Sep;35(9):817-824.: https://doi.org/10.1111/j.1600-051X.2008.01295.x
Harrel SK, Rees TD (1995) Granulation tissue removal in routine and minimally invasive surgical procedures. Compend Contin Educ Dent 16:960–967
Harrel SK (1998) A minimally invasive surgical approach for periodontal bone grafting. Int J Periodontics Restorative Dent. Apr 18(2):161–169
Harrel SK (1999) A minimally invasive surgical approach for periodontal regeneration: surgical technique and observations. Journal of Periodontology Dec 70(12):1547–1557. https://doi.org/10.1902/jop.1999.70.12.1547
Cortellini P, Tonetti MS (2007) A minimally invasive surgical technique (MIST) with enamel matrix derivate in the regenerative treatment of intrabony defects: a novel approach to limit morbidity. J Clin Periodontol 34:87–93. https://doi.org/10.1111/j.1600-051X.2006.01020.x
Trombelli L, Farina R, Franceschetti G (2007) Single flap approach in periodontal surgery. Dental Cadmos 75(8):15–25
Cortellini P, Tonetti MS (2011) Clinical and radiographic outcomes of the modified minimally invasive surgical technique with and without regenerative materials: a randomized-controlled trial in intra-bony defects. J Clin Peridontol 38:365–373. https://doi.org/10.1111/j.1600-051X.2011.01705.x
Cosyn J, Cleymaet R, Hanselaer L, De Bruyn H (2012) Regenerative periodontal therapy of infrabony defects using minimally invasive surgery and a collagen-enriched bovine-derived xenograft: a 1-year prospective study on clinical and aesthetic outcome. J Clin Periodontol 39:979–986. https://doi.org/10.1111/j.1600-051X.2012.01924.x
Aimetti M, Ferrarotti F, Mariani GM, Romano F (2017) A novel flapless approach versus minimally invasive surgery in periodontal regeneration with enamel matrix derivative proteins: a 24-month randomized controlled clinical trial. Clin Oral Invest Jan 21(1):327–337. https://doi.org/10.1007/s00784-016-1795-2
Ribeiro FV, Casarin RC, Palma MA, Jùnior FH, Sallum EA, Casati MZ (2011a) Clinical and patient-centered outcomes after minimally invasive non-surgical or surgical approaches for the treatment of intrabony defects: a randomized clinical trial. J Periodontol 82:1256–1266. https://doi.org/10.1902/jop.2011.100680
Hutton B, Salanti G, Caldwell DM et al (2015) The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med Jun 2 162(11):777–784. https://doi.org/10.7326/M14-2385
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 62(10):1006–1012. https://doi.org/10.1371/journal.pmed.1000097
Higgins JPT, Altman DG, Sterne JAC. (2011) Chapter 8: assessing risk of bias in included studies. In: Higgins JPT, Green S (eds). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration, 2011
Buti J, Glenny AM, Worthington HV, Nieri M, Baccini M (2011) Network meta-analysis of randomised controlled trials: direct and indirect treatment comparisons. Eur J Oral Implantology 4:55–62
Chaimani A, Higgins JPT, Mavridis D, Spyridonos P, Salanti G (2013) Graphical tools for network meta-analysis in STATA. PLoS One 8(10):e76654. https://doi.org/10.1371/journal.pone.0076654
Salanti G, Del Giovane C, Chaimani A, Caldwell DM, Higgins JP. (2014) Evaluating the quality of evidence from a network meta-analysis. PLoS One Jul 3; 9(7): e99682. https://doi.org/10.1371/journal.pone.0099682
Ferrarotti F, Romano F, Gamba MN et al (2018) Human intrabony defect regeneration with micrografts containing dental pulp stem cells: a randomized controlled clinical trial. J Clin Periodontol Jul 45(7):841–850. https://doi.org/10.1111/jcpe.12931
Ghezzi C, Ferrantino L, Bernardini L, Lencioni M, Masiero S (2016) Minimally invasive surgical technique in periodontal regeneration: a randomized controlled clinical trial pilot study. Int J Periodontics Restorative Dent 36:475–482. https://doi.org/10.11607/prd.2550
Schincaglia GP, Hebert E, Farina R, Simonelli A, Trombelli L (2015) Single versus double flap approach in periodontal regenerative treatment. J Clin Periodontol 42:557–566. https://doi.org/10.1111/jcpe.12409
Ribeiro FV, Casarin RCV, Palma MAG, Jùnior FHN, Sallum EAS, Casati MZ (2013) Clinical and microbiological changes after minimally invasive therapeutic approaches in intrabony defects: a 12-month follow-up. Clin Oral Invest 17:1635–1644. https://doi.org/10.1007/s00784-012-0855-5
Trombelli L, Simonelli A, Schincaglia GP, Cucchi A, Farina R (2012) Single-flap approach for surgical debridement of deep intraosseous defects: a randomized controlled trial. J Periodontol 83:27–35. https://doi.org/10.1902/jop.2011.110045
Ribeiro FV, Casarin RC, Palma MA, Jùnior FH, Sallum EA, Casati MZ (2011b) The role of enamel matrix derivative protein in minimally invasive surgery in treating intrabony defects in single rooted teeth: a randomized clinical trial. J Periodontol 82:522–532. https://doi.org/10.1902/jop.2010.100454
Trombelli L, Simonelli A, Pramstraller M, Wikesjo UME, Farina R (2010) Single flap approach with and without guided tissue regeneration and a hydroxyapatite biomaterial in the management of intraosseous periodontal defects. J Periodontol 81:1256–1126. https://doi.org/10.1902/jop.2010.100113
Jackson D, Barrett JK, Rice S, White IR, Higgins JPT (2014) A design-by-treatment interaction model for network meta-analysis with random inconsistency effects. Statist Med 33:3639–3654. https://doi.org/10.1002/sim.6188
Papapanou PN, Wennstrom JL (1991) The angular bony defect as indicator of further alveolar bone loss. J Clin Periodontol 18:317–322
Stoecklin-Wasmer C, Rutjes AW, da Costa BR, Salvi GE, Jüni P, Sculean A (2013) Absorbable collagen membranes for periodontal regeneration: a systematic review. J Dent Res Sep 92(9):773–781. https://doi.org/10.1177/0022034513496428
Kao RT, Nares S, Reynolds MA (2015) Periodontal regeneration – intrabony defects: a sistematic review from AAP regeneration workshop. J Periodontol 86(Suppl):S77–S104. https://doi.org/10.1902/jop.2015.130685
Reynolds MA, Aichelmann-Reidy ME, Branch-Mays GL, Gunsolley JC (2003) The efficacy of bone replacement grafts in the treatment of periodontal osseous defects. A systematic review. Ann Periodontol 8:227–265. https://doi.org/10.1902/annals.2003.8.1.227
Graziani F, Gennai S, Cei S, Cairo F, Baggiani A, Miccoli M, Gabriele M, Tonetti M (2012) Clinical performance of access flap surgery in the treatment of the intrabony defect. A systematic review and meta-analysis of randomized clinical trials. J Clin Periodontol 39:145–156. https://doi.org/10.1111/j.1600-051X.2011.01815.x
Rosling B, Nyman S, Lindhe J, Jern B (1976) The healing potential of the periodontal tissues following different techniques of periodontal surgery in plaque-free dentitions. A 2-year clinical studies. J Clin Periodontol Nov 3(4):233–250
Nibali L, Yeh YC, Pometti D, Tu YK (2018) Long-term stability of intrabony defects treated with minimally invasive non-surgical therapy. J Clin Periodontol Dec 45(12):1458–1464. https://doi.org/10.1111/jcpe.13021
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Barbato, L., Selvaggi, F., Kalemaj, Z. et al. Clinical efficacy of minimally invasive surgical (MIS) and non-surgical (MINST) treatments of periodontal intra-bony defect. A systematic review and network meta-analysis of RCT’s. Clin Oral Invest 24, 1125–1135 (2020). https://doi.org/10.1007/s00784-020-03229-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-020-03229-0