Abstract
Objective
The aim of this study was to investigate clinical periodontal parameters after treatment using the Minimally Invasive Surgical Technique (MIST), Modified Minimally Invasive Surgical Technique (M-MIST), and/or any technique for papilla preservation, such as Entire Papilla Preservation (EPP), modified-papilla preservation technique (M-PPT), or simplified-papilla preservation technique (SPPT).
Methods
The focus question was “For patients with periodontal intrabony defects (P), what is the best minimally invasive regenerative approach (I), comparing MIST, M-MIST, and papilla preservation techniques’ outcomes (C) to improve PD, CAL, GR, and periodontal stability (O)?” An online search was conducted on PubMed, Cochrane Library, and Embase. Only randomized clinical trials and case series with a minimum of 10 enrolled patients were included. The risk of bias was evaluated using the Critical Appraisal tools in JBI Systematic Reviews. The meta-analysis compared the data obtained for the periodontal parameters analyzed, and the heterogeneity was verified.
Results
After the screening, nine articles were included. Seven studies applied MIST and its modifications; two used M-PPT, one SPPT, and one approached EPP. A general statistically significant PD reduction and CAL gain were noted between the groups, comparing baseline and follow-up for all articles, independently of the technique or materials used. Also, all studies showed a non-significant increase in the gingival recession. Four studies had a low risk of bias, four had a moderate risk, and only 1 had a high risk. Moderate heterogeneity was found in one analysis for CAL (65.73%); moderate and substantial heterogeneity was found in the PD results (71.91% and 89.19%); and no heterogeneity was found within all analyses for gingival recession (0%).
Conclusion
MIST, M-MIST, and papilla preservation techniques demonstrated their potential and efficacy to improve periodontal conditions of sites with intrabony defects with minimal morbidity.
Similar content being viewed by others
Introduction
Periodontal regenerative therapy aims to reconstruct intrabony defects, which is defined as a “periodontal defect within the bone surrounded by one, two, or three bony walls or a combination thereof”1. Several factors can interfere with the biological response and outcomes obtained. They may be associated with local or systemic factors, surgical technique, or strategy chosen2. Focusing on the surgical procedure, in 1995, a minimally invasive periodontal treatment was introduced3. It minimizes the wound size and flap reflection and permits the gentle handling of the soft and hard tissues. Then, the “minimally invasive surgery” and “microsurgery“4,5,6,7 era was launched. In addition, it permits the use of operating microscopes/loupes and microsurgical instruments8,9,10. This era had new flap designs and the use of biomaterials, which can be considered the most relevant improvement. Moreover, this approach has limited morbidity and discomfort and increased the predictability and success rate4,5,11,12.
In the ‘90 s, two minimally invasive surgical techniques were developed: the modified papilla preservation technique (1995)13 and the simplified papilla preservation technique (1999)14. In 2007, the minimally invasive surgical technique (MIST)6 with minimal flap elevation emerged; in 2009, modified MIST (M‐MIST), performing a minimal elevation only of the buccal area of the interdental papilla4; and in 2017, entire papilla preservation (EPP) technique15. These surgical procedures keep the flap as short as possible, with minimal exposure to the residual bone crest4, reaching a stable primary wound closure to seal the regenerated region13,14, and permit an incident-free healing phase9,11,12,16.
Those minimally invasive techniques have significantly increased the clinical success rate, using specific incisions on the interdental papilla where there is a bone defect, avoiding compromising the volume and integrity of the interdental tissues15. Also, it is possible to have early soft tissue healing and minimize papilla trauma, with a lower risk of apical migration of the gingival margin (gingival recession)17,18, and to minimize surgical trauma and chair time, to increase flap stability, to allow stable primary closure of the wound, and to reduce discomfort and side effects.
Thus, researchers and clinicians have worked intensely to find the most conservative approach for treating periodontal defects. The objective of this systematic study was to investigate clinical periodontal parameters (pocket depth [PD], clinical attachment level [CAL], and gingival recession [GR]) after treatment with Minimally Invasive Surgical Technique (MIST), Modified-Minimally Invasive Surgical Technique (M-MIST), and/or any technique for papilla preservation, such as Entire Papilla Preservation (EPP), modified-papilla preservation technique (M-PPT), or simplified-papilla preservation technique (SPPT). The null hypothesis was that no techniques improved the clinical parameters compared to the control group.
Materials and methods
Protocol and focus questions
This systematic review followed the PRISMA (Preferred Reporting Items Systematic Review and Meta-Analyses) guidelines. Only articles with scientific evidence in treating intraosseous defects within minimally invasive periodontal surgery were investigated. For the development of this study, it was formulated the following focused questions using the P.I.C.O. strategy (Population, Intervention, Comparison, and Outcome): “For patients with periodontal intrabony defects (P), what is the best minimally invasive regenerative approach (I), comparing MIST, M-MIST, and papilla preservation techniques’ outcomes (C) to improve PD, CAL, GR, and periodontal stability?”
Search strategy
Electronic research was carried out in PubMed/MEDLINE, Cochrane Central Register of Controlled Trials, and Embase databases to identify studies applying MIST (Minimally Invasive Surgical Technique), M-MIST (Modified-Minimally Invasive Surgical Technique), and papilla preservation procedures. Moreover, a manual search was conducted on specific journals: Journal of Clinical Periodontology, Journal of Periodontology, Clinical Oral Investigations, The International Journal of Periodontics & Restorative Dentistry, and Journal of Periodontal Research. The references of the included papers were crosschecked for possible additional studies, and the authors were contacted to clarify any doubt about the data.
Limitations were implemented, such as articles published within the last 10 years (February 2012–February 2022) and in English. The combination of MeSH terms and keywords associated with Boolean operators were: “minimally invasive” OR “periodontal regeneration” OR “intrabony defect” OR intraosseous OR intrabony OR angular OR vertical OR “papilla preservation” AND “buccal access flap” OR “guided tissue regeneration”. The primary outcomes measured were (i) CAL gain, (ii) PD reduction, and (iii) GR reduction. All parameters must present baseline and follow-up data of the treated sites.
Eligibility criteria
The inclusion criteria were: (i) human studies, (ii) last 10 years (February 2012 – February 2022), (iii) publications in English language, (iv) randomized controlled trials (RCTs) describing MIST, M-MIST, and/or papilla preservation surgical procedures in the field of periodontal surgery, (vi) a minimum of 10 patients must be reported with clinical, radiographic, and/or patient-related outcomes, and (vii) at least 6-month follow-up after the procedures. The exclusion factors were: (i) secondary studies (bibliographic review, narrative review, systematic review, and meta-analysis), (ii) in vitro studies, (iii) case reports, case series, retrospective study, (iv) studies without CAL, PD, and/or GR, and (v) inclusion of patients with systemic diseases.
Selection of articles and data extraction
Two independent reviewers (EP and FC) performed the appraisal, and a third reviewer (GVOF) was consulted in case of disagreement. The reviewers discussed the results based on the inclusion/exclusion criteria. Duplicate articles were removed. Firstly, it was analyzed the title and abstract. Subsequently, the studies that met the eligibility criteria and those with insufficient data in the abstract were selected for full-text evaluation. The following information was extracted from the articles: (i) author and year of publication, (ii) follow-up, (iii) sample size and the number of defects, and (iv) clinical characteristics and details (CAL gain, PD reduction, and GR reduction).
Quality assessment and risk of bias
The main domains used to assess the certainty of the evidence are risk of bias, inconsistency, indirectness of evidence, imprecision, and publication bias. Then, two independent investigators (FC and EP) performed the quality assessment, and in the case of divergences, a third researcher was consulted (GVOF). Critical Appraisal tool in JBI Systematic Reviews was used to determine the possibility of bias. Seven main quality criteria were examined, with 12 questions: (i) sequence generation, (ii) allocate concealment, (iii) blinding of participants and personnel, (iv) blinding of outcome assessors, (v) incomplete data, (vi) selective outcome, and (vii) other sources of bias (such as funding or conflict of interest).
The risk of bias was sorted as below19: (a) low risk of bias (plausible bias unlikely to seriously alter the results) if all criteria were met (all green [yes]) or at maximum 2 unclear; (b) moderate risk of bias (“plausible bias” data raises some doubt about the results) if one “no” (red) is found or up to 4 “unclear” criteria were met; (c) high risk of bias (plausible bias that seriously weakens confidence in the results) if honor more criteria were not met (at least 2 “no” (red) or ≥5 “unclear” is found); and (d) risk evaluation not applicable to this context.
Statistical analysis
The meta-analysis involved comparing the data obtained for the periodontal parameters analyzed. The observation period varied, and only studies with similar follow-ups were compared. All analyses were performed in Microsoft Excel (v. 16.73, Microsoft, Redmond, USA), where the fixed effect model was applied with a significance level of 5%. Heterogeneity between studies was quantified using the I2 inconsistency test. Values between 0% and 30% were considered might not be important; between 31% and 50% may represent low heterogeneity; between 51% and 75% may represent moderate; and >75% were considered an indication of substantial heterogeneity.
Results
Search screening
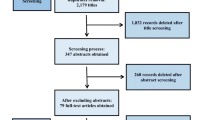
A total of 1491 articles were found through the electronic search (384 articles on PubMed, 363 at the Cochrane Library, and 744 articles on Embase), and 2 more articles were manually added. All duplicate articles (n = 337) were removed, resting 1156 articles. After analyzing the eligibility criteria, all non-relevant studies (n = 1141) were taken out (k = 0.92). Thereby, 15 studies followed for full-text reading (k = 0.98). Six were removed due to a lack of details or information, and less than 10 patients were treated, resulting in 9 articles included (Fig. 1).
Demographic data and Follow-up
All RCTs included (n = 9) are detailed in Tables 1 and 2. 193 patients (59 females and 134 males) were enrolled, with a mean age of 44.16 (±7.965) years, were enrolled; 222 intrabony defects were treated. Three articles presented 6-month follow-up2,20,21; 6 had 1-year follow-up; only 2 studies showed periods larger than 1 year, Aimetti et al. (2017)22 had 1 and 2-year follow-up, and Cortellini et al. (2017)23 had 1 and 20 years. Three articles excluded smokers to avoid bias; 19 current and 4 former smokers were found. No influence or adverse event was reported related to smokers. There were ten dropouts with the following justifications: (1) root fracture before the 6-month visits and (2) moved to another country or city.
Studies’ details
Six studies used enamel matrix derivative (EMD) as adjunctive material2,18,22,24,25,26. One used open flap debridement (OFD) as the control group21; Aimetti et al. (2017)22 used the flapless technique as the control group, whereas Cortellini et al. (2017)23 used the modified Widman flap approach as the control; Farina et al. (2012)2 also used different types of materials: (a) hydroxyapatite bone graft with a resorbable collagen membrane, (b) hydroxyapatite bone graft only, and (c) hydroxyapatite bone graft with EMD, or only collagen membrane for guided-tissue/bone regeneration (GTR/GBR)26. One study used a bovine bone graft26, and another used a titanium membrane23.
Seven studies applied MIST and its modifications2,20,21,22,24,25,26; two studies used Modified-papilla preservation technique (M-PPT)23,24; one used simplified-papilla preservation technique (SPPT)24; and one study approached EPP18.
Technically, the rationale for applying the MIST, M-MIST, or papilla preservation resides in preserving an intact interdental papilla, which may facilitate flap repositioning and suturing. Thus, it optimizes wound closure for primary intention healing and accelerates the re-establishment of the local vascular supply. MIST was described as an elevation of the interdental papillary tissues to uncover the interdental space, gaining complete access to the intrabony defect. In contrast, M-MIST proposed an approach/elevation with small buccal flap access to achieve the defect without elevation of the interdental papilla. The papilla preservation techniques were designed as tunnel-like approaches to the defect-associated inter-dental papilla.
Clinical findings
All findings are detailed in Table 2. All studies suggested the techniques evaluated, independently of the control or test group, had great regenerative potential and reached comparable clinical outcomes. A general statistically significant PD reduction and CAL gain were noted between the groups studied, comparing baseline and follow-up for all articles, independently of the technique or materials used (Fig. 2). Otherwise, no significant result was reported comparing groups when available. Also, there was a non-statistically significant increase in the gingival recession in all studies, demonstrating that, even though clinical success was reached, this variable did not present improvement. Defects with non-supportive anatomy and a thin-scalloped gingival phenotype were identified as risk factors for increased buccal recession.
Regardless of whether used and adjunctive biomaterial, MIST and M-MIST demonstrated a greater improvement in periodontal tissue attachment and pocket depth reduction. Oppositely, all groups studied had a slight increase in GR. Studies that applied papilla preservation showed uneventful early healing and 100% wound closure maintained during the entire healing period. Tunnel-like “EPP” technique may limit the risk of wound failure, particularly in the early healing phase, thereby preventing exposure to regenerative biomaterials, possibly enhancing the stabilization of blood clots in deep intrabony defects, and leading to optimal clinical outcomes.
A controversy was found when applying EMD as an adjunct biomaterial. Grezzi et al. (2016)26, Aslan et al. (2020)18, and Windisch et al. (2021)24 had a non-significant improvement in the clinical results, which was controversial in Liu et al.’s (2022)25 study, where the regenerative materials did not show an additional effect on the outcomes.
Risk of bias and meta-analysis
All included studies were qualitatively assessed (Fig. 3). A low risk of bias was found in four studies (Windisch et al., 2021 – 124; Aslan et al., 2020 – 318; Aimetti et al., 2017 – 622; Schincaglia et al., 2015 – 720); other four studies had a moderate risk of bias (Liu et al., 2022 – 225; Cortellini et al., 2017 – 423; Grezzi et al., 2016 – 526; Elsalam et al., 2020 – 921); whereas only one had a high risk (Farina et al., 2012 – 82).
Risk of Bias of the included studies (Windisch et al., 2021 – 1; Liu et al., 2022 – 2; Aslan et al., 2020 – 3; Cortellini et al., 2017 – 425; Grezzi et al., 2016 – 5; Aimetti et al., 2017 – 626; Schincaglia et al., 2015 – 727; Farina et al., 2012 – 82; Cosyn et al., 2012 – 9; Elsalam et al., 2020 – 10 29; Aslan et al., 2017 – 11; Aslan et al., 2020 – 12).
CAL assessment showed a general gain for all groups, slightly favoring the test groups. No significant differences in the overall outcome between 6 and 12 months, respectively 1.62 [1.20, 2.04] and 1.81 [1.53, 2.09]. The funnel plots present the existence of moderate heterogeneity only in the 12-month analysis for this parameter (65.73%) (Fig. 4). Contrasting CAL in the control group versus the test group, both six and 12-month evaluation presented results favoring the test group, even though there was no statistical significance, respectively 0.39 [–0.19, 0.96] and 0.13 [–0.11, 0.36]. A low heterogeneity was found within the groups’ comparison at 12 months (I2 = 44.98%).
Similar results were observed in the variable PD, which improved during the appraisal period. The overall outcome between 6 and 12 months had no significant differences, respectively 2.87 [2.35, 3.39] and 2.66 [2.33, 3.00]. Low heterogeneity was found in the results at six months (I2 = 32.11%), whereas substantial heterogeneity was found in the PD results at 12 months (89.19%). Comparing the control and test for the PD outcome, after 6 and 12 months, no statistically significant result was found, respectively 0.15 [−0.42, 0.71] and 0.34 [0.0, 0.48]. However, at six months, no heterogeneity was reported (I2 = 0%); otherwise, at 12 months, a moderate level of heterogeneity was found (71.91%) (Fig. 5).
No heterogeneity was found within all analyses for gingival recession (I2 = 0%). A good balance was observed between groups and periods for the results on this parameter, as observed in Fig. 6.
Discussion
Minimally invasive techniques are a reality. They have demonstrated a more conservative intervention for decades, providing greater patient comfort and improved results. This systematic review investigated clinical periodontal parameters (PD, CAL, and GR), comparing the baseline data and outcomes for MIST, M-MIST, or any papilla preservation technique studied (EPP, M-PPT, or SPPT). Since minimally invasive techniques and flaps are based on reduced surgical access in the interdental area27, using membrane alone or combined with bone grafts may be challenging28,29.
It is essential to evaluate the PD associated with intrabony components. In our systematic study, the minimum baseline mean value found was 5.3 mm, but most studies had >6 mm for this parameter. In fact, deep intrabony defects (>6 mm) would require a more extended flap to provide adequate visibility for instrumentation30, facilitating the use of a membrane. Three out of 9 studies included used some type of membrane. Grezzi et al. (2016)26 compared MIST with EMD and DBBM against MIST with resorbable membrane (GTR), reporting no significant results when comparing outcomes of all clinical parameters evaluated (p > 0.05). Farina et al. (2012)2 used a hydroxyapatite bone graft with resorbable collagen membrane in 7 defects/patients; no membrane exposure or exfoliation of the biomaterial was observed after 2 weeks. All results had non-significant results for all defect studies (p > 0.05). Both aforementioned studies had non-valuable results to justify the use of a membrane, a fact that agrees with the literature. Otherwise, in a case series study, Aslan et al. (2020)5 applied EPP with GBR (collagen membrane) and found significant improvement for CAL and PD, contrasting previous studies. Similar findings using membrane were reported by Cortellini et al. (2017)23, who treated patients with M-PPT and titanium membrane (non-resorbable); the authors presented significative CAL gain (5.3 ± 2.2 mm, p < 0.0001) and PD reduction (3.4 ± 2.4 mm, p = 0.001). Then, it is possible to observe a contrast in the results found in the literature. The M-PPT and SPPT were originally proposed for membrane use, and for this reason, the residual margin of the crestal bone must be exposed for about 2-3 mm; the fact that mobilization is no longer necessary when applied EMD has led to the development of MIST and M-MIST.
Then, some studies considered the application of EMD as a co-adjuvant in intra-bony defect treatment. Even though EMD in combination with a minimally invasive surgical flap can be applicable in any bone defect30, when used in 3-wall intrabony defects associated with papilla preservation flaps, it yielded a 269% higher success chance than 1-wall defects to gain 3 mm CAL or more31. Another study (case series), Aslan et al. (2017)15, had significant data for the gain of CAL (gain of 6.83 ± 2.51 mm, P < 0.001) and reduction of PD (7.0 ± 2.8 mm, P < 0.001) when applied EPP with EDM. In our systematic review, observing other approaches (MIST or M-MIST with EMD22,24, MIST with EMD and DBBM18, and EPP with EMD18), the outcomes were favorable for the parameters analyzed, although sometimes without significance. On the other hand, comparing MIST with a modified suture against MIST with EMD25, lower values were found for the group that used EMD. Moreover, in the most non-contained intrabony defects (79.3%) treated by means of EMD and papilla preservation flaps, a residual PD ≥ 6 mm was recorded after 12 months of follow-up32; at the same follow-up period, inferior data was presented by all other studies that used EMD, disagreeing of the Siciliano et al.’s results, with final mean PD ranging from 2.75 ± 0.75 mm to 4.31 ± 1.5 mm. For these reasons, non-contained intrabony defects were excluded from the present study.
The CAL gains observed in the included studies are compatible with the literature22,29,33. Therefore, some studies had lower CAL gains, 2.54mm21, while others had higher CAL gains, 6.83mm15. This discrepancy may be due to the defect selection (morphology of the intrabony defects), materials used, and professional experience. In the present review, statistically significant CAL gain and PD reduction were measured in each group at 6 or 12 months, with no statistically significant differences recorded between the control and test groups, with a slight deviation favoring the test groups, as observed in the forest plots. The surgical approach may explain the small variance in the difference found between groups.
A common finding in all studies and groups was a minimal gingival recession increase, except for using MIST modified in sutures25, with a non-significant recession coverage mean of 0.03 (±1.19). This fact may be explained by the passive coronal displacement of the vestibular extension of the flap during suturing20. The GR had no heterogeneity, and the statistical result showed a similar standard of minimal increase. In addition, the choice of suturing material can exert any undesirable effect, i.e., it may be hypothesized that 5-0 monofilament sutures have a higher tendency to cause more compression on the wound, which might influence the healing. Wound closure is normally ensured with 6-0 or 7-0 sutures4,6 for MIST or M-MIST. Nevertheless, there is insufficient evidence demonstrating a negative influence of the size of the sutures on the clinical outcomes obtained in intrabony defects after regenerative surgery.
Two essential factors to be observed as inclusion criteria are if the patient had any systemic condition or was a smoker. In this study, no patients with systemic problems were included. Three articles excluded smokers; the other 6 included 19 current and 4 former smokers. Favorably, no adverse event was reported considering the smoking condition.
As a limitation of the present study, we observed a lack of standards in comparing techniques and types of co-adjuvant biomaterials implemented (EMD, resorbable or non-resorbable membranes, and different kinds of bone grafts). Also, we analyzed different minimally invasive techniques, which had different approaches and eligibility criteria, such as smokers. We included clinical studies with the presence of RCTs and CS; this fact can be considered a limitation due to the limited number of RCTs published on this topic. Moreover, some studies (RCTs) had two groups for comparison; otherwise, other studies (CS) did not have a control group. Another limitation was the date limitation, including articles published between 2012 and 2022. A last limitation found was the short-term analysis done in a great part of the studies, six months and one year; we suggested more studies with longer-term evaluation.
Conclusion
Within the limitation of this review, MIST, M-MIST, and papilla preservation techniques are an actual reality in the field of periodontal regeneration, depending on the esthetic site and facility/ability of the flap repositioning, suturing, and initial clinical parameters. RCTs have demonstrated their potential and efficacy to improve periodontal conditions of sites with intrabony defects. The null hypothesis raised was accepted. The improvements are consistently associated with minimal patient morbidity. The chair time required to perform such surgery is shorter than that required for conventional surgical approaches. Therefore, all data must be carefully analyzed because of heterogeneity among studies.
Data availability
All data is available within the manuscript.
References
Lang NP. Focus on intrabony defects—conservative therapy. Periodontology. 2000;22:51–58.
Farina R, Simonelli A, Rizzi A, Pramstraller M, Cucchi A, Trombelli L. Early postoperative healing following buccal single flap approach to access intraosseous periodontal defects. Clin Oral Investig. 2013;17:1573–83.
Harrel SK, Rees TD. Granulation tissue removal in routine and minimally invasive surgical procedures. Comp Cont Educ Dent. 1995;16:960–7.
Cortellini P, Tonetti MS. Improved wound stability with a modified minimally invasive surgical technique in the regenerative treatment of isolated interdental intrabony defects. J Clin Periodontol. 2009;36:157–63.
Aslan S, Buduneli N, Cortellini P. Reconstructive surgical treatment of isolated deep intrabony defects with guided tissue regeneration using entire papilla preservation technique: A prospective case series. J Periodontol. 2020;92:488–95.
Cortellini P, Tonetti MS. A minimally invasive surgical technique with an enamel matrix derivative in the regenerative treatment of intra-bony defects: a novel approach to limit morbidity. J Clin Periodontol. 2007;34:87–93. https://doi.org/10.1111/j.1600-051X.2006.01020.x
Rasperini G, Ricci G, Silvestri M. Surgical technique for treatment of infrabony defects with enamel matrix derivative (Emdogain): 3 case reports. Int J Periodontics Restorative Dent. 1999;19:578–87.
Maia VTG, Kahn S, Souza AB, Fernandes GVO. Deepithelialized connective tissue graft and the remaining epithelial content after harvesting by the harris technique: a histological and morphometrical case series. Clin Adv Periodontics. 2021;11:150–4. https://doi.org/10.1002/cap.10151
Cortellini P, Tonetti MS. Microsurgical approach to periodontal regeneration. Initial evaluation in a case cohort. J Periodontol. 2001;72:559–69.
Cortellini P, Tonetti MS. Clinical performance of a regenerative strategy for intrabony defects. Scientific evidence and clinical experience. J Periodontol. 2005;76:341–50.
Kahn S, Araújo E, Tajra I, Dias AT, Souza AB, Chambrone L, et al. Histologic and histomorphometric analysis of connective tissue grafts harvested by the parallel incision method: a pilot randomized controlled trial comparing macro- and microsurgical approaches. Quint Int. 2021;52:772–8.
Kahn S, Oliveira LZ, Dias AT, Fernandes GVO. Clinical evaluation and biological understanding of the early step-by-step healing after periodontal microsurgery: A case report with PES analysis comparing initial and 31-day result. J Adv Periodontol Implant Dent. 2022;14:141–5. https://doi.org/10.34172/japid.2022.016
Cortellini P, Pini Prato G, Tonetti MS. The modified papilla preservation technique. A new surgical approach for interproximal regenerative procedures. J Periodontol. 1995;66:261–6.
Cortellini P, Pini Prato G, Tonetti MS. The simplified papilla preservation flap. A novel surgical approach for the management of soft tissues in regenerative procedures. Int J Periodontics Restorative Dent. 1999;19:589–99.
Aslan S, Buduneli N, Cortellini P. Entire papilla preservation technique in the regenerative treatment of deep intrabony defects: 1-year results. J Clin Periodontol. 2017;44:926–32.
Tibbetts LS, Shanelec D. Periodontal microsurgery. Dent Clin North Am. 1998;42:339–59.
Takei HH, Han TJ, Carranza FA Jr, Kenney EB, Lekovic V. Flap technique for periodontal bone implants. Papilla preservation technique. J Periodontol. 1985;56:204–10. https://doi.org/10.1902/jop.1985.56.4.204
Aslan S, Nurcan B, Cortellini P. Clinical outcomes of the entire papilla preservation technique with and without biomaterials in the treatment of isolated intrabony defects: A randomized controlled clinical trial. J Clin Periodontol. 2020;47:470–8.
Ochôa C, Castro F, Bulhosa JF, Manso C, Fernandes JCH, Fernandes GVO. Influence of the Probiotic L. reuteri on periodontal clinical parameters after nonsurgical treatment: a systematic review. Microorganisms. 2023;11:1449 https://doi.org/10.3390/microorganisms11061449
Schincaglia GP, Hebert E, Farina R, Simonelli A, Trombelli L. Single versus double flap approach in periodontal regenerative treatment. J Clin Periodontol. 2015;42:557–66. https://doi.org/10.1111/jcpe.12409
Elsalam MGA, Elsamad AA, Elbarbary AM, Abuldahab OM. Evaluation of gain in clinical attachment and bone levels after treatment of patients with intra-bony defects by minimally invasive surgical technique versus open flap debridement: a randomized controlled clinical trial. Ain Shams Dental J. 2020;13:239–46.
Aimetti M, Ferrarotti F, Mariani GM, Romano F. A novel flapless approach versus minimally invasive surgery in periodontal regeneration with enamel matrix derivative proteins: a 24-month randomized controlled clinical trial. Clin Oral Invest. 2017;21:327–37. https://doi.org/10.1007/s00784-016-1795-2
Cortellini P, Buti J, Pini Prato G, Tonetti MS. Periodontal regeneration compared with access flap surgery in human intra-bony defects 20-year follow-up of a randomized clinical trial: tooth retention, periodontitis recurrence and costs. J Clin Periodontol. 2017;44:58–66. https://doi.org/10.1111/jcpe.12638
Windisch P, Iorio-Siciliano V, Palkovics D, Ramaglia L, Blasi A, Sculean A. The role of surgical flap design (minimally invasive flap vs. extended flap with papilla preservation) on the healing of intrabony defects treated with an enamel matrix derivative: a 12-month two-center randomized controlled clinical trial. Clin Oral Investig. 2022;26:1811–21.
Liu B, Ouyang X, Kang J, Zhou S, Suo C, Xu L, et al. Efficacy of periodontal minimally invasive surgery with and without regenerative materials for treatment of intrabony defect: a randomized clinical trial. Clin Oral Investig. 2022;26:1613–23.
Ghezzi C, Ferrantino L, Bernardini L, Lencioni M, Masiero S. Minimally invasive surgical technique in periodontal regeneration: a randomized controlled clinical trial pilot study. Int J Periodontics Restorative Dent. 2016;36:475–82. https://doi.org/10.11607/prd.2550
Cosyn J, Cleymaet R, Hanselaer L, De Bruyn H. Regenerative periodontal therapy of infrabony defects using minimally invasive surgery and a collagen-enriched bovine-derived xenograft: a 1-year prospective study on clinical and aesthetic outcome. J Clin Periodontol. 2012;39:979–86. https://doi.org/10.1111/j.1600-051X.2012.01924.x
Harrel SK, Wilson TH Jr, Nunn ME. Prospective assessment of the use of enamel matrix proteins with minimally invasive surgery. J Periodontol. 2005;76:380–4. https://doi.org/10.1902/jop.2005.76.3.380
Riberio FV, Casarin RC, Junior FH, Sallum EA, Casati MZ. The role of enamel matrix proteins in minimally invasive surgery in treating intrabony defects in single-rooted teeth: a randomized clinical trial. J Periodontol. 2011;82:522–32. https://doi.org/10.1902/jop.2010.100454
Cortellini P, Tonetti MS. Clinical concepts for regenerative therapy in intrabony defects. Periodontol 2000. 2015;68:202–307. https://doi.org/10.1111/prd12048
Tonetti MS, Lang NP, Cortellini P, Suvan JE, Adriaens P, Dubravec D, et al. Enamel matrix proteins in the regenerative therapy of deep intrabony defects. A multicenter randomized controlled clinical trial. J Clin Periodontol. 2002;29:317–25. https://doi.org/10.1034/j.1600-051x.2002.290407.x
Siciliano VI, Andreuccetti G, Siciliano AI, Blasi A, Sculean T, Salvi GE. Clinical outcomes after treatment of non-contained intrabony defects with enamel matrix derivative or guided tissue regeneration: a 12-months randomized controlled clinical trial. J Periodontol. 2011;82:62–71. https://doi.org/10.1902/jop.2010.100144
Cortellini P, Tometti MS. Clinical and radiographic outcomes of modified minimally invasive surgical technique with and without regenerative materials: a randomized-controlled trial in intrabony defects. J Clin Periodontol. 2011;38:565–73. https://doi.org/10.1111/j.1600-051x2011.01705.x
Author information
Authors and Affiliations
Contributions
EP, FC, DC, AM, AH, MHS, JCHF, and GVOF were responsible for the conceptualization and design of the project. EP, FC, and GVOF were responsible for the data collection. EP, FC, DC, AM, AH, MHS, JCHF, and GVOF were responsible for the analysis and interpretation of data. EP, FC, DC, AM, AH, MHS, JCHF, and GVOF participated in the investigation, data curation, and drafting of the manuscript and contributed to revising the manuscript. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pasqualini, E., Castro, F., Curado, D. et al. Minimally invasive periodontal regeneration with the buccal approach: a systematic review and meta-analysis of clinical studies. Evid Based Dent 25, 54 (2024). https://doi.org/10.1038/s41432-023-00964-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41432-023-00964-7
- Springer Nature Limited