Abstract
Objectives
The aim of this study was to longitudinally evaluate, after a 4-year period, the clinical longevity of composite resin restoration compared to the baseline, after selective caries removal in permanent molars using Er:YAG laser or bur preparation with biomodification of dentin with the use of chlorhexidine.
Methods
Selective caries removal was performed on 80 teeth of 20 individuals who each had at least four active carious lesions. These lesions, located on occlusal surfaces of permanent molar counterparts, were removed using (i) Er:YAG laser biomodified with chlorhexidine, (ii) Er:YAG laser and application of deionized water, (iii) bur preparation biomodified with chlorhexidine, and (iv) bur preparation and application of deionized water. At the end of 4 years, 64 of the 80 restorations were evaluated in 16 individuals (n = 16). The restorations were evaluated, both clinically and photographically, using scanning electron microscopy (SEM) and pulp vitality analysis. The experimental data were statistically evaluated by kappa, Fisher’s, and chi-square tests, with a significance level of 5%. The Kaplan–Meier test and the Cox regression analysis were used to evaluate the survival of the restorations.
Results
After 4 years of follow-up, there was a statistically significant difference in marginal discoloration criteria for all of the groups evaluated. For marginal adaptation criteria, there was a statistically significant difference for the Er:YAG laser group biomodified with chlorhexine (p = 0.050). For clinical and radiographic evaluation of pulp vitality, there were no statistically significant differences among the groups (p = 0.806).
Conclusion
Er:YAG laser can be used for selective caries removal, regardless of dentin biomodification with chlorhexidine or application of deionized water, once it produced promising results in composite resin restorations after 4 years of follow-up, according to the criteria evaluated. The selective caries removal using Er:YAG laser or bur and the biomodification of dentin with the use of chlorhexidine did not influence the survival of composite resin restorations after the 4-year follow-up period.
Clinical relevance
Composite resin restorations applied after selective caries removal using Er:YAG laser or burs, regardless of dentin biomodification with the use of chlorhexidine or application of deionized water, showed adequate clinical behavior after 4 years of follow-up.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Selective caries removal has been successfully performed on primary [1,2,3,4] and permanent teeth [5,6,7,8]. This removal of carious tissue is performed in medium cavities where selective removal of firm dentin should be performed prioritizing the restoration longevity. In deep cavities with vital pulp, selective removal of soft dentin should be carried out, preserving pulpal health over restoration success. Demineralized tissues close to the pulp or bacterially contaminated tissues do not need to be removed from the cavities [9].
Selective caries removal creates conditions for long-lasting restorations, keeps healthy dental structure, maintains pulpal health by preventing pulp exposures, reduces levels of cariogenic microorganisms in dentin tissue, and prevents the progression of carious lesions [2, 7, 9, 10].
Er:YAG laser can be used for selective caries removal [4, 5] since its wavelength (2.94 μm) coincides with the maximum absorption peak of the water and the hydroxyl group [11, 12]. The caries is removed by means of micro-explosions resulting from the evaporation of water contained in the mineralized tissues [12, 13].
Er:YAG laser promotes microstructural alterations, micro-ruptures, and denaturation of collagen fibers [14,15,16]. The exposure of the collagen fibers interferes with the adhesion of resinous materials, because adhesion to the dental surface depends directly upon the resinous monomer engagement [17].
Conversely, Er:YAG laser increases acid resistance to demineralization of dental enamel, reduces the dissolution of acids, and prevents the occurrence of secondary caries [18].
Physical changes observed in dental enamel, such as melting and recrystallization, frequently result in pores that create a rough surface, providing a micromechanical attachment between the dental substrate and the adhesive systems [19]. In addition, the dentinal tubules remain open and without smear layer formation [20, 21].
The application of chlorhexidine, used as a means of biomodification of dentin, is considered to be a broad-spectrum protease inhibitor, since it preserves the bond strength [22, 23] between adhesive restorative materials and dental substrates. Moreover, the preservation of the hybrid layer was also verified by the inhibition of MMPs [22, 24,25,26], not interfering in vitro with the dentin adhesion process after irradiation with Er:YAG laser [27].
The restorations performed in laser-prepared cavities of permanent molars and biomodified with chlorhexidine did not influence the retention and marginal adaption of restorations evaluated in a 1-year period [5]. After a 6-month period, restorations performed with diamond burs, using a high-speed handpiece and biomodified with chlorhexidine application, showed potential benefits in lowering the occurrence of microleakage in extracted pre-molars [23].
Due to the absence of clinical studies that longitudinally evaluated occlusal composite resin restorations, performed after selective caries removal in permanent molars using Er:YAG laser and the bur preparation method, biomodified with chlorhexidine or application of deionized water, the null hypothesis tested was as follows:
The clinical longevity of composite resin restoration performance, after a 4-year period, was similar when comparing the methods used for selective caries removal and the type of biomodification used in the dentin.
Material and methods
Experimental design
The factors under study were the methods used for selective caries removal, bur preparation or Er:YAG laser and biomodification of the dentin with chlorhexidine and control groups, application of deionized water, followed by the longitudinal clinical evaluation of composite resin restorations, performed by Galafassi et al. [5], after 4 years of performing restorations. The experimental sample consisted of 20 patients (n = 20) and 80 composite resin restorations performed on the occlusal surface in homologous permanent molars. The experimental design was performed in randomized complete blocks. The longitudinal clinical evaluation of the composite resin restorations was conducted using blind testing, whereby the examiners used modified USPHS (US Public Health System) criteria along with the photographic qualitative analysis of the restorations as response variables. This was followed by a pulp vitality analysis by clinical and radiographic examination, as well as the quantitative analysis of the marginal integrity of the restorations by scanning electron microscopy (SEM).
Ethical aspects
This study was approved by the Research Ethics Committee of the Ribeirão Preto School of Dentistry, University of São Paulo (FORP/USP, Case No. 2016.1.586.58.4). It was registered in the Brazilian Registry of Clinical Trials (ReBEC) under a register number (RBR-8n5n3v). Parents or guardians of the individuals signed the Terms of Consent, agreeing to participate in the research.
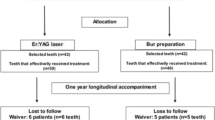
The CONSORT guide [28] for randomized clinical trials was followed for the study design and the recruitment, allocation, follow-up, and analysis of research subjects are arranged in Fig. 1.
During the monitoring period (4 years), four individuals were not followed up, leaving a total of n = 16 participants (10 boys and 6 girls) and 64 restorations for the final analysis. The data of individuals without the 4-year follow-up period were not considered in the statistical analysis.
Selective caries removal
Approximately, 3200 children were examined in eight public schools. A confidence level of 95% was established with the presence of approximately 16 individuals.
The experimental sample consisted of 20 individuals between 8 and 12 years of age, of both genders, having a group total of 80 homologous permanent molars that presented moderately deep cavitated lesions reaching the dentin located on the occlusal surface. Clinical and radiographic examinations were performed for the diagnosis of active caries lesions. The presence of four active carious lesions on the occlusal surfaces (class I) of contralateral permanent first molars—with vital pulps and the absence of sealants, amalgam, glass ionomer cement, or composite resin restorations—established the inclusion criteria. A drawing was used to assist in determining the type of treatment that would be performed on each tooth.
Images of restored teeth on a computer screen were used to facilitate the calibration of the operator and two examiners (kappa test = 0.91). Selective caries removal and biomodification of the dentin tissue [5] were performed at four levels: (i) Er:YAG laser (Fidelis Er III, Fotona, Ljubljana, Slovenia) using the parameters; MSP mode, pen (R02), noncontact mode and focal distance of 12 mm, pulse energy of 260 mJ, pulse frequency of 4 Hz (for cavity preparation and selective caries removal) [4, 29], output beam diameter of 0.9 mm, energy density of 41 J/cm2, water spray (15 mL/min) [30], biomodified with chlorhexidine; (ii) Er:YAG laser (260 mJ/4 Hz for cavity preparation and selective caries removal) and application of deionized water; (iii) bur preparation (high-speed turbine for cavity preparation and low-speed turbine mounted drills for selective caries removal) biomodified with chlorhexidine; and (iv) bur preparation (high-speed turbine for cavity preparation and low-speed turbine mounted drills for selective caries removal) and application of deionized water. Removal of carious tissue in the permanent molars using Er:YAG laser and bur preparation was performed according to the clinical protocol proposed by Valério et al. [4], following the concepts of selective removal of carious dentin described in the literature. [10, 31]. The high absorption of laser irradiation in moist surfaces such as dentin caries tissues causes an audible “popping” sound that aids the clinician in distinguishing between the ablation of sound and carious tissues [32]. Clinical hardness criteria were determined using curettes to confirm that all of the carious tissue was removed from lateral walls in order to promote proper sealing conditions [33, 34].
Restorations were employed with a 100% nanoparticle composite containing zirconia and silica. Clinical follow-up was conducted in the baseline, after 6 and 12 months using the protocol described by Galafassi et al. [5]. In the evaluation period, SEM was used to analyze replicas of the restorations.
Preliminary procedures
The 20 patients (n = 20) who received restorative treatment in four permanent molars, following Galafassi et al. [5], returned to the School of Dentistry for follow-up. Prophylaxis was performed with pumice paste and water (SS White (Jon, São Paulo, SP, Brazil) on smooth surfaces using a rubber cup (Jon, São Paulo, SP, Brazil) and brush (by Robinson) on the occlusal surfaces, both connected to a micromotor (Gnatus, Ribeirão Preto, SP, Brazil). Patients who were not found after numerous attempts by our institution as well as those who did not attend the scheduled appointments were excluded from the study. The clinical examination was performed under adequate lighting, followed by topical application of fluoride and individualized oral hygiene instruction. The permanent molars that needed retreatment due to problems related to caries recurrence, marginal infiltration and discoloration or even loss of restorative material, had the restorations replaced or, if applicable, repaired. If the need for endodontic intervention was verified after clinical and radiographic examination, this procedure was performed at the Endodontics Clinic of the School of Dentistry.
If the patient had other teeth that needed treatment, but which were not part of the research, they were treated at this same institution. If in any of the cases, orthodontic evaluation was necessary, those patients were referred to the Orthodontics Clinic.
Clinical and photographic evaluation of restorations
The restored teeth were carefully evaluated through clinical and photographic analysis 4 years after the restorative procedures.
The clinical analysis of the restorations, performed by the same two examiners [5] who were previously calibrated, was compared to the baseline. The examiners were not informed about which method of selective caries removal, or which method of biomodification of the affected dentin had been used in that restoration. The latter was evaluated (blind test) by means of visual and tactile examination, using an active tip instrument following the modified USPHS criteria [35], which includes the analysis of retention, marginal discoloration, secondary caries, and marginal adaptation.
The restorations were classified into three categories—Alpha, Bravo, and Charlie—following the modified USPHS criteria used to evaluate composite resin restorations by Valerio et al. [4]. The examiners indicated one of the scores—Alpha, Bravo, or Charlie—for each clinical criterion evaluated (Table 1).
In order to perform the clinical analysis of the restorations, standardized photographs of the restored teeth were taken by an experienced professional following the protocol used by Valério et al. [4]. The same examiners who performed the clinical analysis verified the photographs of the restored molars on a high-resolution flat-panel monitor (kappa test = 0.96) and were able to compare the results from the clinical analysis with those of the photographic one, thus reaching an accurate result.
Clinical and radiographic evaluation of pulp vitality
The clinical analysis of pulp vitality used the following criteria: presence or absence of painful symptomatology percussion or spontaneous sensitivity and fistula and edema in the region of restored permanent molars. The thermal test using Endofrost (Roeko, Langenau, Germany) was applied as the most common method of performing pulp vitality evaluation and considered to be an accessible method with a simple technique, providing reproducible and safe results [36] since this type of cold test has an accuracy of 86% as compared to other tests [37].
This coolant was sprayed on a large cotton ball and applied to the midline of the vestibular face of restored permanent molars and adjacent teeth and “normal” contralaterals that were also tested to establish a baseline response.
Interproximal radiographs of the restored molars were examined to verify possible caries lesions and adaptation of the restorations using the digital radiography sensor (CDR Elite, Fona, São Paulo, SP, Brazil) and positioner. The periapical radiographs using digital radiography sensor (CDR Elite, Fona, São Paulo, SP, Brazil) and positioner were used to verify the pulp vitality through the presence of radiolucency in the furcation and periapice region, increased periodontal ligament thickening and internal or external tooth resorption, using Strindberg’s index, in which each variable received one of the three scores used: 1, healthy; 2, uncertain (doubtful); and 3, unhealthy [38].
Clinical and radiographic analysis of pulp vitality was performed by two examiners within a 4-year period of the restorative procedures. The examiners who completed the analysis were not informed as to which method of selective caries removal had been used in that restored permanent molar, nor the mode of biomodification of the dentin (blind test).
Calibration of the evaluators was conducted through the evaluation of interproximal and periapical radiographs of permanent molars seen on a computer screen (kappa test = 0.98).
Evaluation of the marginal integrity of the restorations using scanning electron microscopy
The restorations were molded 4 years after the restorative procedures. The moldings were formed used perforated aluminum partial molds (Golgran Ind. Odontológica, São Paulo, SP, Brazil) with additional silicone (Aquasil Ultra, Dentsply Caulk, Milford, DE, USA), using the simultaneous molding technique. The molds were disinfected with 2% chlorhexidine spray (Neo Química Laboratory, Anápolis GO, Brazil). They were then cast with epoxy resin (Epo Heat, Buehler, Chicago, USA), which was manipulated and poured over the molding, awaiting final prey to obtain the models. The molds were cut and the replicates of the restorations obtained were fixed onto aluminum stubs with double-sided carbon tape, metallized (Metalizadora and Evaporator Bal-Tec SCD 050, Los Angeles CA, USA) with fine gold coverage, and analyzed in SEM Scanning Electron ZEISS EVO 50, Thornwood, NY, USA) with 20 and 200× magnification.
The analyses were performed by two calibrated examiners with experience in scanning electron microscopy. They were not aware of the methods used to perform the restorations (blind test). The calibration of the evaluators was assessed by scanning electron microscopy in restored permanent molars seen on a computer screen (kappa test = 0.93). The artifacts of the model were disregarded. The adaptation of the composite resin restoration was verified, and the percentage of the marginal integrity was calculated by measurement of the integrated area and the area that presented a gap in relation to the margin of the restoration [39].
Statistical analysis
The experimental data were statistically evaluated by kappa, Fisher’s, and the chi-square tests with a significance level of 5%. The Kaplan–Meier test was used to generate the survival curves of composite resin restorations in the 4-year follow-up period. The Cox regression analysis pertaining to the independent variables was used to evaluate the survival of the restorations. Calibrated examiners (kappa score > 0.80) were blinded from information regarding the experimental groups. The statistical analysis was performed using SPSS software for Windows, version 12.0 (SPSS Inc., Chicago, IL, USA).
Results
The final condition for analysis was performed with 16 individuals and 64 composite resin restorations. Four individuals and 16 composite resin restorations were not followed up. The demographic characteristics of the sample are set in Table 2.
Clinical and photographic evaluation of restorations was statistically analyzed using Fisher’s exact test (p < 0.05). The results showed that there was no statistically significant difference between the groups tested for the retention criteria when one composite resin restoration (performed after selective caries removal using Er:YAG laser biomodified with chlorhexidine) had to be replaced. For marginal discoloration criteria, there was a statistically significant difference for all of the groups evaluated, in which five composite resin restoration presented Bravo score for the bur group with the application of deionized water, five for the bur group biomodified with chlorhexine, 13 for the Er:YAG laser group with application of deionized water, and nine for the Er:YAG laser group biomodified with chlorhexine. This was after selective caries removal in a 4-year follow-up compared to the baseline. For marginal adaptation criteria, there was a statistically significant difference for the Er:YAG laser group biomodified with chlorhexine. In this group, six composite resin restorations presented Bravo score, after selective caries removal in a 4-year follow-up, as compared to the baseline. For secondary caries criteria, there was no statistically significant difference between the evaluated groups. One composite resin restoration performed after selective caries removal using a bur with the application of deionized water and two restorations using the laser biomodified with chlorhexidine group presented recurrence of caries and were repaired as shown in Table 3. The results presented in Table 3 show that there was no statistically significant difference between the treatments of the studied groups, bur preparation or Er:YAG laser and biomodification of the dentin with chlorhexidine and control groups, and application of deionized water. There was a statistically significant difference between the periods of analysis (baseline and 4 years of follow-up).
The restoration survival was statistically analyzed using Kaplan–Meier test. The distribution of composite resin restorations was described according to the independent variables (Table 4) in frequency, valid percentage, success, and failure. Twenty-four composite resin restorations (37.5%) were performed in female patients and 40 (62.5%) in male patients. After 4 years of clinical follow-up, seven restorations had some type of failure. The Er:YAG laser group biomodified with chlorhexine presented the highest frequency of failures 5 (7.81%). One composite resin restoration (1.56%) presented Charlie score for the retention criteria, one (1.56%) Charlie score for the marginal adaptation criteria, one (1.56%) Charlie score for the marginal discoloration criteria, and 2 (3.12%) Charlie scores for the secondary caries criteria. The laser group with the application of deionized water did not present any failures. The bur group with application of deionized water presented one restoration of composite resin (1.56%), with Charlie score for the secondary caries criteria. The bur group biomodified with chlorhexidine presented one composite resin restoration (1.56%) with Charlie score for the marginal discoloration criteria. The survival of the composite resin restorations was verified using Cox regression analysis. The Er:YAG laser group biomodified with chlorhexidine (p = 0.54), Er:YAG laser with application of deionized water (p = 1.00), bur biomodified with chlorhexidine (0.95), and bur with application of deionized water (0.95) did not significantly affect the survival of composite resin restorations after 4 year of clinical follow-up.
Clinical evaluation of pulp vitality by means of presence or absence of pain, symptomatology percussion or spontaneous sensitivity, fistula, and edema criteria in the region of restored permanent molars were statistically analyzed using Fisher’s exact test (p < 0.05). The results showed no statistically significant differences among the groups (p = 0.806), since two restorations of the Er:YAG laser group with application of deionized water presented pain and fistula as shown in Fig. 2.
Radiographic evaluation of pulp vitality, performed by Strindberg’s index, was statistically analyzed using Fisher’s exact test (p < 0.05). The results showed no statistically significant differences among the groups (p = 0.806), since two restorations of the Er:YAG laser group with application of deionized water showed the presence of radiolucency in the furcation and periapice region and increased periodontal ligament, receiving the scores “unhealthy” and “uncertain” (doubtful) as shown in Fig. 3.
Compared to the baseline, the replicas of the composite resin restorations evaluated by SEM showed no gaps or irregularities in the restored teeth regardless of the method used for selective caries removal and the biomodification of the dentin with chlorhexidine (Fig. 4).
Representative photographs of treatments: (1) Scanning electron microscopy at the baseline and (2) scanning electron microscopy after 4-year follow-up. (A) In a bur preparation biomodified with chlorhexidine, (B) Er:YAG laser preparation with application of deionized water, (C) bur preparation with application of deionized water, and (D) Er:YAG laser preparation biomodified with chlorhexidine
Discussion
Er:YAG laser irradiation has advantages as compared to the bur preparation method, regardless of the minimally invasive approach, which promotes less pressure, noise, vibration, and pain, providing greater comfort to patients [40, 41]. Furthermore, when this type of tool is used for selective caries removal, it presents advantages regardless of the conventional caries removal method, such as preserving healthy and remineralizable tissues, maintaining pulpal health, and promoting greater longevity for the restorations [9, 31].
The null hypothesis presented was accepted, since the clinical longevity of composite resin restorations performed after a 4-year period were similar between the methods used for selective caries removal and the type of biomodification used in the dentin.
Although the results of this study showed a statistically significant difference for the marginal discoloration criteria in all the studied groups, the polymerization shrinkage stress of resin composite materials can be responsible for this situation. Extrinsic factors, such as dietary habits with the ingestion of dyes, can affect the marginal surface of restorations. However, these factors are irrelevant, since it is not necessary to replace the restoration, especially in posterior teeth, without compromising the patient’s dental esthetic [5, 42]. This same relationship was verified by Galafassi et al. [5], after a 1-year follow-up period.
The literature shows that occlusal restorations performed in permanent molars were clinically evaluated over a 2-year period using USPHS criteria [35], after the total removal of caries lesions performed with conventional methods and Er,Cr:YSGG laser, respectively presenting (5.6% and 7.4%) Bravo score for marginal discoloration criteria as in Yazici et al. [43]. In a longitudinal clinical study, Hamidi et al. [44] evaluated occlusal composite resin restorations using modified USPHS criteria [35], after the total caries removal using Er:YAG laser in a 5-year period in which 46.3% of the restorations employed were classified with Bravo score. The limitation of this study is related to the non-use of a control group.
Regarding the marginal adaptation criteria, there was a statistically significant difference for the Er:YAG laser group biomodified with chlorhexidine that presented a Bravo score after a 4-year follow-up period, albeit clinically acceptable. The same relation was not observed in the scanning electron microscopy analysis, compared to the baseline, agreeing with Galafassi et al. [5], which found a non-expressive number of restorations showing gaps and irregularities of tooth-restoration interface after 6 and 12 months as compared to the baseline.
After the total removal of caries lesions using conventional methods and Er,Cr:YSGG laser, Yazici et al. [43] showed 13% of patients received Bravo scores for marginal adaptation evaluated over a 2-year period in a laser group, and after total caries removal using Er:YAG laser in a 5-year period, five restorations (12.2%) received Bravo ratings for marginal adaptation [44]. Comparing different restorative resins, Yazici et al. [45] showed a statistically significant difference for marginal adaptation criteria, receiving Bravo scores after a 3-year follow-up period and de Andrade et al. [46], after a 54-month period and comparing different restorative resins, showed statistically significant differences in the marginal adaptation criteria.
In primary molars, occlusal composite resin restorations were clinically and photographically evaluated by the modified USPHS criteria [35] after partial caries removal (1-year period) in a randomized split-mouth clinical trial, using Er:YAG laser or bur preparation. There were no significant differences between the restorations employed [4]. In a randomized controlled trial comparing Er:YAG laser irradiation and rotary bur, Sarmadi et al. [47] over a 2-year period showed no statistically significant differences between the restorations performed after excavation with the two methods, either in quality or survival of restorations using the USPHS criteria [35].
This positive result can be justified by the fact that Er:YAG laser promotes physical changes on the surface of dental substrates, such as melting and recrystallization with pores, which create a coarse surface that provides a micromechanical bond for adhesives [18]. Regarding the occurrence of secondary caries, these were probably not observed in this study because Er:YAG laser irradiation increases the resistance of enamel to acid demineralization while reducing the acid dissolution [19, 48].
In dentin, Er:YAG laser can increase the microhardness, as well as the quantities of Ca of the laser-prepared cavities [13]. Er:YAG laser irradiation on dentin might promote changes in the percentage of O, C, and Mg independently of energy density. Additionally, morphological changes, such as the absence of smear layer and exposed dentinal tubules, were observed [49]. Er:YAG laser irradiation increased microhardness of residual caries-affected dentin biomodified with chitosan, changing its surface morphology and chemical composition in vitro [50].
In caries-affected dentin, Koyuturk et al. [51] showed an increase in bond strength using Er:YAG laser irradiation to cavities in primary canines prepared with self-etch primers; Er:YAG laser’s bond strength was found to be similar to the bur preparation method [52]. Using Er:YAG and Er,Cr:YSGG lasers can decrease microleakage to the level of bur preparation in primary canine teeth in vitro, as seen by Malekafzali et al. [21].
The results herein showed that there were no statistically significant differences for the response variable clinical and radiographic evaluation of pulp vitality. These results can be explained as a function of irradiation with Er:YAG laser being a safe and effective tool [4] for the removal of caries lesions when using safe parameters. This is because this type of laser, by its wavelength (2.94 μm), through thermo-mechanical ablation process involving micro-explosions [53], has a great potential for hard-tissue ablation. This is due to its high absorbability in water and hydroxyapatite. It has been shown to remove enamel and dentin using a pulsed laser beam combined with water spray [30]. In addition, it has an affinity for moist surfaces, such as infected dentin [54], it does not damage the remaining dental structures [55], and there is no noticeable pulp temperature increase [56, 57]. Vogel and Venugopalan [58] demonstrated that ablation thresholds of dental tissues are reduced at shorter laser pulses than the thermal time relaxation of the ablated surface; therefore, less heat is transferred to the surrounding tissues, leading to faster ablation and a smaller amount of residual heat deposition [59].
It is difficult to compare these results of response variable clinical and radiographic evaluation of pulp vitality after selective caries removal using Er:YAG laser with biomodification of the dentin with those presented in the literature, since there are no similar studies published. The partial removal of carious lesions using burs in primary molars [60] showed satisfactory clinical and radiographic outcomes, while not showing internal or external resorption or periapical lesion. A case report Stafuzza et al. [61] showed that in an 18-month follow-up exam, after selective caries removal in primary molars using burs, the teeth did not present painful symptomatology, periapical lesions, fistulas, or abscesses.
Although two restorations of the Er:YAG laser group with application of deionized water presented problems related to pulp vitality evaluated through clinical and radiographic analysis, this may have occurred due to serious occlusal trauma reported by individuals that generated fracture in the permanent molar and also because of the patient’s delay in seeking our institution, keeping the dental tissues exposed to the oral environment for a long time. The same relation has been demonstrated by Hamidi et al. [44], in which two teeth were submitted to endodontic treatment because of pulp inflammation between the baseline and a 4-year follow-up period after class I preparation using Er:YAG laser irradiation.
To preserve the hybrid layer and to promote bond durability, studies have applied chlorhexidine (CHX) to its antibacterial activity as a potential inhibitor of endogenous proteases such as matrix metalloproteinases (MMPs). MMPs are zinc- and calcium-dependent proteases that require calcium ions to maintain their tertiary structure as well as zinc ions to catalyze the hydrolysis process. These enzymes degrade extracellular matrix proteins and regulate the physiological and pathological metabolism of collagen-based tissues [62, 63].
CHX can interact with organic components of dentin matrix. This interaction occurs through electrostatic forces, between CHX protonated amine groups, mineral phosphates, and non-collagenous phosphoproteins that in turn are closely related to collagen fibrils [64].
The preservation of collagen integrity in the hybrid layer occurs through the interaction of CHX with the sulfhydryl group on domain or cysteine located at the active site of MMPs. That may distort MMPs molecules and prevent them from binding to substrates, thus competing for the binding of calcium and zinc ions to MMPs because of their chelating action. Without these ions, MMPs lose their catalytic activities [65].
When dentin was exposed to a 0.2% CHX solution after the etching protocol and before the application of the dentin adhesive, no improvement or adverse effects on bond strength were verified [66]. However, Stanislawczuk et al. [67] described that the use of 2% CHX, associated or not with phosphoric acid, preserved resin–dentin bond durability. In the same way, Montagner et al. [68] concluded that the application of CHX as an MMP inhibitor used as a coadjutant in dentin adhesion did not influence the retention of class V restorations after 6 months of follow-up. In turn, class V cavities prepared in vitro using Er:YAG laser can be rinsed with chlorhexidine since this procedure did not interfere in the adhesion process [27].
In caries-affected dentine, the wettability of the surface was higher than in sound dentin, and chlorhexidine did not influence this property using flat dentin surfaces in vitro [69]. In vivo, the use of chlorhexidine as an adjuvant to the adhesion to dentin did not produce any detrimental effect to the immediate bond strength and was capable of reducing the rate of resin–dentin bond degradation [70].
After 2 years of water storage, Malaquias et al. [71] concluded that chlorhexidine, up to 0.2%, is a viable method by which to provide an adhesive drug release system to maintain stable resin–dentin adhesive interfaces. In this study, after selective caries removal and biomodification of the dentin with chlorhexidine, no statistically significant difference was observed in the restorations performed after a 4-year follow-up. To our knowledge, there are no similar clinical studies in the literature that allow a greater comparison of these results regarding the biomodification of the dentin using chlorhexidine.
Considering the lack of scientific studies that provide a better discussion of the data obtained and the difficulties related to the development of in vivo studies, we can state that Er:YAG laser is considered to be a promising technology for caries removal. Further research should investigate a larger number of longitudinal clinical studies using Er:YAG laser irradiation.
Conclusions
According to the results, it was possible to conclude that Er:YAG laser can be used for selective caries removal, regardless of dentin biomodification with chlorhexidine or application of deionized water, once it produced promising results in composite resin restorations performed after a 4-year follow-up period, according to the evaluated criteria.
The selective caries removal using Er:YAG laser or bur and the biomodification of dentin with chlorhexidine did not influence the survival of composite resin restorations after a 4-year follow-up.
References
Lula EC, Monteiro-Neto V, Alves CM, Ribeiro CC (2009) Microbiological analysis after complete or partial removal of carious dentin in primary teeth: a randomized clinical trial. Caries Res 43:354–358. https://doi.org/10.1159/000231572
Elhennawy K, Finke C, Paris S, Reda S, Jost-Brinkmann PG, Schwendicke F (2018) Selective vs stepwise removal of deep carious lesions in primary molars: 12-months results of a randomized controlled pilot trial. J Dent 77:72–77. https://doi.org/10.1016/j.jdent.2018.07.011
Pinto S, de Araújo FB, Franzon R, Figueiredo MC, Henz S, García-Godoy F, Maltz M (2006) Clinical and microbiological effect of calcium hydroxide protection in indirect pulp capping in primary teeth. Am J Dent 19:382–386
Valério RA, Borsatto MC, Serra MC, Polizeli SA, Nemezio MA, Galo R, Aires CP, Dos Santos AC, Corona SA (2016) Caries removal in deciduous teeth using an Er:YAG laser: a randomized split-mouth clinical trial. Clin Oral Investig 20:65–73. https://doi.org/10.1007/s00784-015-1470-z
Galafassi D, Scatena C, Galo R, Curylofo-Zotti FA, Corona SAM, Borsatto MC (2017) Clinical evaluation of composite restorations in Er:YAG laser-prepared cavities re-wetting with chlorhexidine. Clin Oral Investig 21:1231–1241. https://doi.org/10.1007/s00784-016-1897-x
Mertz-Fairhurst EJ, Curtis JW Jr, Ergle JW, Rueggeberg FA, Adair SM (1998) Ultraconservative and cariostatic sealed restorations: results at year 10. J Am Dent Assoc 129:55–66
Bjørndal L, Reit C, Bruun G, Markvart M, Kjaeldgaard M, Näsman P, Thordrup M, Dige I, Nyvad B, Fransson H, Lager A, Ericson D, Petersson K, Olsson J, Santimano EM, Wennström A, Winkel P, Gluud C (2010) Treatment of deep caries lesions in adults: randomized clinical trials comparing stepwise vs. direct complete excavation, and direct pulp capping vs. partial pulpotomy. Eur J Oral Sci 118:290–297. https://doi.org/10.1111/j.1600-0722.2010.00731.x
Banerjee A (2013) Minimal intervention dentistry: part 7. Minimally invasive operative caries management: rationale and techniques. Br Dent J 214:107–111. https://doi.org/10.1038/sj.bdj.2013.106
Schwendicke F, Frencken JE, Bjørndal L, Maltz M, Manton DJ, Ricketts D, Van Landuyt K, Banerjee A, Campus G, Doméjean S, Fontana M, Leal S, Lo E, Machiulskiene V, Schulte A, Splieth C, Zandona AF, Innes NP (2016) Managing carious lesions: consensus recommendations on carious tissue removal. Adv Dent Res 28:58–67. https://doi.org/10.1177/0022034516639271
Thompson V, Craig RG, Curro FA, Green WS, Ship JA (2008) Treatment of deep carious lesions by complete excavation or partial removal: a critical review. J Am Dent Assoc 139:705–712
Aoki A, Ishikawa I, Yamada T, Otsuki M, Watanabe H, Tagami J, Ando Y, Yamamoto H (1998) Comparison between Er:YAG laser and conventional technique for root caries treatment in vitro. J Dent Res 77:1404–1414
Tao S, Li L, Yuan H, Tao S, Cheng Y, He L, Li J (2017) Erbium laser technology vs traditional drilling for caries removal: a systematic review with meta-analysis. J Evid Based Dent Pract 17:324–334. https://doi.org/10.1016/j.jebdp.2017.05.004
Hibst R, Keller U (1989) Experimental studies of the application of the Er:YAG laser on dental hard substances: I. Measurement of the ablation rate. Lasers Surg Med 9:338–344
Martinez-Insua A, Da Silva DL, Rivera FG, Santana-Penin UA (2000) Differences in bonding to acid-etched or Er: YAG-laser-treated enamel and dentin surfaces. J Prosthet Dent 84:280–288
Ceballo L, Osorio R, Toledano M, Tay F, Marshall GW (2002) Bonding to Er:YAG laser treated dentin. J Dent Res 81:119–122
Aranha AC, De Paula EC, Gutknecht N, Marques MM, Ramalho KM, Apel C (2007) Analysis of the interfacial micromorphology of adhesive systems in cavities prepared with Er,Cr:YSGG, Er:YAG laser and bur. Microsc Res Tech 70:745–751
Schein MT, Bocangel JS, Nogueira GEC, Schein PAL (2003) SEM evaluation of interaction pattern dentin and resin after cavity preparation using Er:YAG laser. J Dent 31:127–135
Apel C, Birker L, Meister J, Weiss C, Gutknecht N (2004) The caries-preventive potential of subablative Er:YAG and Er:YSGG laser radiation in an intraoral model: a pilot study. Photomed Laser Surg 22:312–317
Wen X, Liu L, Nie X, Zhang L, Deng M, Chen Y (2010) Effect of pulse Nd:YAG laser on bond strength and microleakage of resin to human dentine. Photomed Laser Surg 28:741–746. https://doi.org/10.1089/pho.2009.2579
Matsumoto K, Nakamura Y, Makesi K, Kimura Y (1996) Clinical dental application of Er:YAG laser for class V cavity preparation. J Clin Laser Med Surg 14:123–127
Malekafzali B, Asnaashari M, Javadi F (2017) Comparison of marginal microleakage of flowable composite restorations in primary canine teeth prepared with high-speed diamond bur, Er:YAG laser and Er,Cr:YSGG laser. Laser Ther 26:195–202. https://doi.org/10.5978/islsm.17-OR-15
Hebling J, Pashley DH, Tjäderhane L, Tay FR (2005) Chlorhexidine arrests subclinical degradation of dentin hybrid layers in vivo. J Dent Res 84:741–746
Ramezanian Nik I, Baradaran Naseri E, Majidinia S, Ramezanian Nik S, Jafari Giv M (2017) Effect of chlorhexidine and ethanol on microleakage of composite resin restoration to dentine. Chin J Dent Res 20:161–168. https://doi.org/10.3290/j.cjdr.a38771
Gendron R, Grenier D, Sorsa T, Mayrand D (1999) Inhibition of the activities of matrix metalloproteinases 2, 8, and 9 by chlorhexidine. Clin Diagn Lab Immunol 6:437–439
Pashley DH, Tay FR, Yiu C, Hashimoto M, Breschi L, Carvalho RM, Ito S (2004) Collagen degradation by host-derived enzymes during aging. J Dent Res 83:216–221
Favetti M, Schroeder T, Montagner AF, Correa MB, Pereira-Cenci T, Cenci MS (2017) Effectiveness of pre-treatment with chlorhexidine in restoration retention: a 36-month follow-up randomized clinical trial. J Dent 60:44–49. https://doi.org/10.1016/j.jdent.2017.02.014
Geraldo-Martins VR, Robles FR, Matos AB (2007) Chlorhexidine’s effect on sealing ability of composite restorations following Er:YAG laser cavity preparation. J Contemp Dent Pract 18:26–33
Schulz KF, Altman DG, Moher D (2010) CONSORT Group—statement: updated guidelines for reporting parallel group randomised trials. Ann Intern Med 152:726–732
Krause F, Braun A, Lotz G, Kneist S, Jepsen S, Eberhard J (2008) Evaluation of selective caries removal in deciduous teeth by a fluorescence feedback-controlled Er:YAG laser in vivo. Clin Oral Investig 12:209–215. https://doi.org/10.1007/s00784-007-0169-1
Colucci V, do Amaral FL, Pécora JD, Palma-Dibb RG, Corona SA (2009) Water flow on erbium:yttrium-aluminum-garnet laser irradiation: effects on dental tissues. Lasers Med Sci 24:811–818. https://doi.org/10.1007/s10103-008-0563-1
Kidd EA (2004) How ‘clean’ must a cavity be before restoration? Caries Res 38:305–313
Clark J, Symons AL, Diklic S, Walsh LJ (2001) Effectiveness of diagnosing residual caries with various methods during cavity preparation using conventional methods, chemo-mechanical caries removal, and Er: YAG laser. Aust Dent J 46:S20
Massara MI, Alves JB, Brandao PR (2002) Atraumatic restorative treatment: clinical, ultrastructural and chemical analysis. Caries Res 36:430–436
Maltz M, Oliveira EF, Fontanella V, Carminatti G (2007) Deep caries lesions after incomplete dentine caries removal: 40-month follow-up study. Caries Res 41:493–496
Cvar JF, Ryge G (2005) Reprint of criteria for the clinical evaluation of dental restorative materials. Clin Oral Investig 9:215–232
Jones VR, Rivera EM, Walton RE (2002) Comparison of carbon dioxide versus refrigerant spray to determine pulpal responsiveness. J Endod 28:531–533
Petersson K, Söderström C, Kiani-Anaraki M, Lévy G (1999) Evaluation of the ability of thermal and electrical tests to register pulp vitality. Endod Dent Traumatol 15:127–131
Tarcin B, Gumru B, Iriboz E, Turkaydin DE, Ovecoglu HS (2015) Radiologic assessment of periapical health: comparison of 3 different index systems. J Endod 41:1834–1838. https://doi.org/10.1016/j.joen.2015.08.010
Garcia-Godoy F, Krämer N, Feilzer AJ, Frankenberger R (2010) Long-term degradation of enamel and dentin bonds: 6-year results in vitro vs. in vivo. Dent Mater 26:1113–1118. https://doi.org/10.1016/j.dental.2010.07.012
Keller U, Hibst R (1997) Effects of Er:YAG laser in caries treatment: a clinical pilot study. Lasers Surg Med 20:32–38
Bohari MR, Chunawalla YK, Ahmed BM (2012) Clinical evaluation of caries removal in primary teeth using conventional, chemomechanical and laser technique: an in vivo study. J Contemp Dent Pract 13:40–47
Kurokawa H, Takamizawa T, Rikuta A, Tsubota K, Miyazaki M (2015) Three-year clinical evaluation of posterior composite restorations placed with a single-step self-etch adhesive. J Oral Sci 57:101–108. https://doi.org/10.2334/josnusd.57.101
Yazici R, Baseren M, Gorucu J (2010) Clinical comparison of bur- and laser-prepared minimally invasive occlusal resin composite restorations: two-year follow-up. Oper Dent 35:500–507. https://doi.org/10.2341/09-339-C
Hamidi MM, Ercan E, Dülgergil ÇT, Çolak H (2015) Evaluation of the clinical success of class I cavities prepared by an Er:YAG laser-5-year follow-up study. Lasers Med Sci 30:1895–1901. https://doi.org/10.1007/s10103-015-1751-4
Yazici AR, Ustunkol I, Ozgunaltay G, Dayangac B (2014) Three-year clinical evaluation of different restorative resins in class I restorations. Oper Dent 39:248–255. https://doi.org/10.2341/13-221-C
de Andrade AK, Duarte RM, Medeiros e Silva FD, Batista AU, Lima KC, Monteiro GQ, Montes MA (2014) Resin composite class I restorations: a 54-month randomized clinical trial. Oper Dent 39:588–594. https://doi.org/10.2341/14-067-C
Sarmadi R, Andersson EV, Lingström P, Gabre P (2018) A randomized controlled trial comparing Er:YAG laser and rotary bur in the excavation of caries—patients’ experiences and the quality of composite restoration. Open Dent J 12:443–454. https://doi.org/10.2174/1874210601812010443
Chinelatti MA, Rocha CT, Colucci V, Serra MC, Rodrigues-Júnior AL, Corona SA (2017) Effect of Er:YAG laser on dentin demineralization around restorations. Lasers Med Sci 32:413–418. https://doi.org/10.1007/s10103-016-2136-z
Moosavi H, Ghorbanzadeh S, Ahrari F (2016) Structural and morphological changes in human dentin after ablative and subablative Er:YAG laser irradiation. J Lasers Med Sci 7:86–91. https://doi.org/10.15171/jlms.2016.15
Curylofo-Zotti FA, Tanta GS, Zucoloto ML, Souza-Gabriel AE, Corona SAM (2017) Selective removal of carious lesion with Er:YAG laser followed by dentin biomodification with chitosan. Lasers Med Sci 32:1595–1603. https://doi.org/10.1007/s10103-017-2287-6
Koyuturk AE, Ozmen B, Cortcu M, Tokay U, Tosun G, Erhan SM (2014) Effects of Er:YAG laser on bond strength of self-etching adhesives to caries-affected dentin. Microsc Res Tech 77:282–288. https://doi.org/10.1002/jemt.22340
Yamada Y, Hossain M, Nakamura Y, Murakami Y, Matsumoto K (2002) Microleakage of composite resin restoration in cavities prepared by Er:YAG laser irradiation in primary teeth. Eur J Paediatr Dent 3:39–45
Van Meerbeek B, De Munck J, Mattar D, Van Landuyt K, Lambrechts P (2003) Microtensile bond strengths of an etch & rinse and self-etch adhesive to enamel and dentin as a function of surface treatment. Oper Dent 28:647–660
Schwass DR, Leichter JW, Purton DG, Swain MV (2013) Evaluating the efficiency of caries removal using an Er:YAG laser driven by fluorescence feedback control. Arch Oral Biol 58:603–610. https://doi.org/10.1016/j.archoralbio.2012.09.017
Kita T, Ishii K, Yoshikawa K, Yasuo K, Yamamoto K, Awazu K (2015) In vitro study on selective removal of bovine demineralized dentin using nanosecond pulsed laser at wavelengths around 5.8 μm for realizing less invasive treatment of dental caries. Lasers Med Sci 30:961–967. https://doi.org/10.1007/s10103-013-1517-9
Oelgiesser D, Blasbalg J, Ben-Amar A (2003) Cavity preparation by Er-YAG laser on pulpal temperature rise. Am J Dent 16:96–98
Baraba A, Kqiku L, Gabrić D, Verzak Ž, Hanscho K, Miletić I (2018) Efficacy of removal of cariogenic bacteria and carious dentin by ablation using different modes of Er:YAG lasers. Braz J Med Biol Res 51:e6872. https://doi.org/10.1590/1414-431X20176872
Vogel A, Venugopalan V (2003) Mechanisms of pulsed laser ablation of biological tissues. Chem Rev 103:577–644
Zhegova GG, Rashkova MR, Yordanov BI (2014) Perception of pain of Er_YAG dental caries treatment in adolescents—a clinical evaluation. J IMAB 20:500–503
Mello B, C Stafuzza T, Vitor L, Rios D, Silva T, Machado M, M Oliveira T (2018) Evaluation of dentin-pulp complex response after conservative clinical procedures in primary teeth. Int J Clin Pediatr Dent 11:188–192. https://doi.org/10.5005/jp-journals-10005-1509
Stafuzza TC, Vitor LLR, Rios D, Cruvinel Silva T, Machado MAAM, Oliveira TM (2018) Clinical and radiographic success of selective caries removal to firm dentin in primary teeth: 18-month follow-up. Case Rep Dent 26:9213681. https://doi.org/10.1155/2018/9213681
Chaussain-Miller C, Fioretti F, Goldberg M, Menashi S (2006) The role of matrix metalloproteinases (MMPs) in human caries. J Dent Res 85:22–32
Feitosa SA, Palasuk J, Geraldeli S, Windsor LJ, Bottino MC (2018) Physicochemical and biological properties of novel chlorhexidine-loaded nanotube-modifieddentin adhesive. J Biomed Mater Res B Appl Biomater doi: https://doi.org/10.1002/jbm.b.34183
Carrilho MR, Carvalho RM, Sousa EN, Nicolau J, Breschi L, Mazzoni A, Tjaderhane L, Tay FR, Agee K, Pashley DH (2010) Substantivity of chlorhexidine to human dentin. Dent Mater 26:779–785. https://doi.org/10.1016/j.dental.2010.04.002
De Munck J, Van den Steen PE, Mine A, Van Landuyt KL, Poitevin A, Opdenakker G et al (2009) Inhibition of enzymatic degradation of adhesive-dentin interfaces. J Dent Res 88:1101–1106
Perote LC, Kamozaki MB, Gutierrez NC, Tay FR, Pucci CR (2015) Effect of matrix metalloproteinase-inhibiting solutions and aging methods on dentin bond strength. J Adhes Dent 17:347–352. https://doi.org/10.3290/j.jad.a34594
Stanislawczuk R, Amaral RC, Zander-Grande C, Gagler D, Reis A, Loguercio AD (2009) Chlorhexidine-containing acid conditioner preserves the longevity of resin-dentin bonds. Oper Dent 34:481–490. https://doi.org/10.2341/08-016-L
Montagner AF, Perroni AP, Corrêa MB, Masotti AS, Pereira-Cenci T, Cenci MS (2015) Effect of pre-treatment with chlorhexidine on the retention of restorations: a randomized controlled trial. Braz Dent J 26:234–241. https://doi.org/10.1590/0103-6440201300009
Ricci HA, Scheffel DL, de Souza Costa CA, dos Santos FJ, Jafelicci M Jr, Hebling J (2014) Wettability of chlorhexidine treated non-carious and caries-affected dentine. Aust Dent J 59:37–42. https://doi.org/10.1111/adj.12150
Ricci HA, Sanabe ME, de Souza Costa CA, Pashley DH, Hebling J (2010) Chlorhexidine increases the longevity of in vivo resin-dentin bonds. Eur J Oral Sci 118:411–416. https://doi.org/10.1111/j.1600-0722.2010.00754.x
Malaquias P, Gutierrez MF, Hass V, Stanislawczuk R, Bandeca MC, Arrais C, Farago PV, Reis A, Loguercio AD (2018) Two-year effects of chlorhexidine-containing adhesives on the in vitro durability of resin-dentin interfaces and modeling of drug release. Oper Dent 43:201–212. https://doi.org/10.2341/16-333-L
Acknowledgments
The author thanks the Ribeirão Preto, School of Dentistry / University of São Paulo (FORP/USP), for giving all the necessary support for accomplishing this research and the São Paulo Research Foundation (FAPESP) for its financial support (2012/06910-6).
Funding
São Paulo Research Foundation (FAPESP) process number (2012/06910-6).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
This study was approved by the Research Ethics Committee of the Ribeirao Preto School of Dentistry, University of São Paulo (FORP/USP—Case No. 2016.1.586.58.4). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Valério, R.A., Galo, R., Galafassi, D. et al. Four-year clinical prospective follow-up of resin composite restoration after selective caries removal using Er:YAG laser. Clin Oral Invest 24, 2271–2283 (2020). https://doi.org/10.1007/s00784-019-03082-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-019-03082-w