Abstract
In the treatment of dental caries, less invasive methods are strongly required. However, conventional dental lasers cannot always achieve selective removal of caries or good bonding with a composite resin. Based on the optical absorption characteristics of dentin, wavelengths around 6 μm are promising in this regard. Our previous study indicated the possibility of selective removal of demineralized dentin using a nanosecond pulsed laser at wavelengths around 6 μm. In the present study, the optimal laser irradiation conditions were investigated for achieving selective removal of demineralized dentin. Bovine dentin was used, and its laser ablation characteristics were evaluated. The results indicated that demineralized dentin could be selectively removed, without causing cracking or damage to sound dentin, at laser wavelengths of 5.75 and 5.80 μm and average power densities of 30–40 W/cm2. These optimal laser irradiation conditions also realized higher bonding strength with a composite resin than was possible using an Er:YAG laser. The use of nanosecond pulses allowed the thermal confinement condition to be satisfied, leading to a reduction in tissue damage, including degradation of dental pulp vitality. Thus, a nanosecond pulsed laser at 5.8 μm was found to be effective for less invasive caries treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Less invasive treatment and preservation of teeth, referred to as minimal intervention (MI), are strong requirements in dentistry [1]. The use of Er:YAG (λ = 2.94 μm) and Er,Cr:YSGG lasers (λ = 2.78 μm) has already been introduced as an alternative approach to conventional dental drills because it leads to increased levels of comfort due to the lack of noise or vibration. However, it has been reported that these lasers sometimes exhibit poor selectivity for dental caries removal and that the bonding strength between the irradiated dentin surface and a composite resin can be low [2–4]. Therefore, there is a need to develop new laser techniques for less invasive treatment of caries.
The interaction between a laser beam and biological tissue depends mainly on the optical absorption characteristics of the target tissue. In general, there are three sets of absorption bands at wavelengths of about 3, 6, and 9 μm in dentin. Conventional dental lasers operate at wavelengths of about 3 μm, where strong absorption by water occurs. This can result in either excessive or insufficient ablation of carious dentin because slight changes in moisture level can have a significant impact on the ablation rate [2, 5]. Furthermore, thermal damage induced by Er:YAG laser irradiation of a dentin surface leads to a reduction in bonding strength with a composite resin [3, 4, 6]. A laser beam with a wavelength of about 9 μm is strongly absorbed by calcium phosphate but is inappropriate because sound dentin exhibits stronger absorption than caries and is thus more effectively removed. However, at wavelengths of about 6 μm, the organic materials that form the basis of demineralized dentin have strong absorption bands referred to as amide 1 and amide 2 bands. In our previous study, the fundamental ablation properties of dentin at laser wavelengths of 5.6–6.6 μm were investigated [7, 8]. The results indicated that selective removal of demineralized dentin, due to a difference in the amount of ablation for sound and demineralized dentin, could be achieved with less damage to sound dentin, especially at wavelengths around 5.8 μm.
The purpose of the present study was to optimize the laser irradiation conditions for the selective removal of bovine demineralized dentin, based on the fact that it has a different mineral content to sound dentin. This was a basic in vitro study for realizing less invasive treatment of dental caries. Laser ablation tests were carried out at wavelengths around 5.8 μm using a mid-infrared tunable nanosecond pulsed laser. After optimization of the laser irradiation conditions, the bonding strength between the irradiated sound dentin surface and a composite resin was evaluated in order to determine the compatibility of this approach with dental adhesive procedures.
Materials and methods
Sample preparation
Sound bovine dentin plates were prepared by cutting bovine anterior teeth to produce dentin discs with dimensions of about 5 × 5 × 1 mm3. The samples were cut from the interior of the teeth, at a distance of at least 0.5–1 mm from the dentin–enamel junction. Demineralized dentin plates, which are carious dentin models with lower mineral content, were prepared by immersing sound dentin plates in a 0.1 M lactic acid solution (20006-75, Nacalai Tesque Inc., Japan) for 24 h at 37 °C while stirring [9]. The sound and demineralized dentin plates were dried at room temperature and used for the laser irradiation experiments.
The samples were prepared using a rigid protocol and had consistent mechanical properties and mineral contents. Table 1 shows the Vickers hardness and Ca content of the bovine dentin samples. The Vickers hardness was measured at ten positions in each sample using a dynamic microhardness testing machine (DUH-211, SHIMADZU, Japan) with a maximum load of 196 mN and an indentation depth of 5 μm. The Ca content was also measured at ten positions in each sample using an energy dispersive X-ray spectrometer (JED-2300, JEOL, Japan) at an accelerating voltage of 20 kV and a magnification of 37×. No appreciable variation in Vickers hardness or Ca content was found within the same dentin group, indicating the consistency of the sample preparation process.
Figure 1 shows absorption spectra for sound and demineralized bovine dentin in the mid-infrared range. The absorption coefficient was measured by a Fourier transform infrared (FTIR) spectrometer (MB3000, ABB, Switzerland) using the KBr method (KBr-FTIR) [10]. The absorbance of the demineralized dentin, which was soft enough to be sliced with a cryostat microtome (CM1850, Leica Microsystems, Germany), was measured using the FTIR spectrometer coupled with an infrared microscope (μMax, Pike Technologies, USA). The thickness of the sliced dentin was measured using a confocal laser microscope (LEXT OLS3100, Olympus, Japan). From the measured absorption spectra and thicknesses of the demineralized dentin discs, the absorption coefficient μ a was calculated using Beer–Lambert’s law.
Optical absorption spectra for sound and demineralized bovine dentin. Hydroxyapatite was eluted during the demineralization process, and no absorption band associated with PO stretching was observed for demineralized dentin. Absorption bands due to OH stretching and amide bands were stronger in demineralized dentin than in sound dentin
Light source
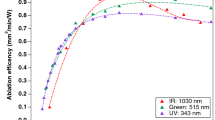
A nanosecond pulsed laser beam produced by difference-frequency generation (DFG) was used. Figure 2 shows a schematic of the DFG laser setup. The DFG laser was jointly developed by RIKEN, Japan, and Kawasaki Heavy Industries, Ltd., Japan [11]. It has a tunable wavelength range of 5.5–10 μm, a pulse duration of 5 ns, and a repetition rate of 10 Hz. Mid-infrared output was obtained by DFG by inserting two AgGaS2 crystals between a Q-switched Nd:YAG laser (Tempest 10, New Wave Research Inc., USA) with a wavelength of 1064 nm and a tunable Cr:forsterite laser with a wavelength range of 1150–1350 nm. The Cr:forsterite laser was pumped by a Q-switched Nd:YAG laser (Tempest 300, New Wave Research Inc., USA), and the wavelength was tuned by rotating the rear mirror of an optical resonator. In this study, a DFG laser wavelength range of 5.70–6.00 μm was used.
Irradiation setup
Sound and demineralized bovine dentin samples were arranged horizontally on an XYZ-stage and irradiated with a laser beam with a diameter of about 100–150 μm focused using a parabolic mirror (f = 10 cm). The average power density was varied in the range 10–40 W/cm2, and the irradiation time was set to 1 s using an electric shutter (F77-4, Suruga Seiki, Japan).
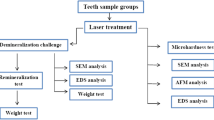
Evaluation
After the irradiation experiments, a gold coating was applied to the samples using an ion sputtering system (E-1010, Hitachi, Japan) for 60 s at a discharge current of 15 mA. The irradiated regions were then observed using a scanning electron microscope (SEM; JCM-5700, JEOL, Japan). The ablation depths were measured using the confocal laser microscope.
Tensile bonding strength tests
The compatibility of the irradiated sound dentin surface with adhesive restoration procedures was evaluated by tensile bonding strength tests. Five sound bovine dentin plates were first prepared, with dimensions of about 1 × 1 cm2 and with dental tubules running perpendicular to the irradiated surface. A motorized stage (SG SP 20-20, Sigma Koki, Japan), which was moved linearly at a constant rate, was used. The scanning speed was calculated by dividing the beam size by the irradiation time per spot (1 s). An area of about 5 × 5 mm2 was irradiated using the DFG laser with a wavelength of 5.80 μm and an average power density of 30 W/cm2, and an Er:YAG laser (Erwin® AdvErL, Morita, Japan) with a pulse energy of 100 mJ, a repetition rate of 10 Hz, a pulse duration of ∼200 μs, and a water flow rate of 2 ml/min. The irradiation conditions for the Er:YAG laser were the same as those used in clinical settings. To simulate a clinical situation, the samples were kept soaked in normal saline solution before and after laser irradiation. After irradiation, the samples were mounted on a brass jig, leaving a circular region with a diameter of 3 mm exposed for the tensile bonding strength tests. A self-etching primer (Clearfil® Mega Bond, Kuraray Medical, Japan) was applied to the irradiated dentin surface, and then a composite resin (Clearfil® AP-X, Kuraray Medical, Japan) was bonded to the surface. The samples were kept in water at 37 °C for 24 h, and the tensile bonding strength was then measured using a universal testing machine (IM-20, Intesco, Japan) at a crosshead speed of 0.3 mm/min.
Results
Dependence of ablation characteristics on laser irradiation conditions
Figure 3 shows SEM images of the surface morphology of sound and demineralized dentin irradiated at wavelengths of 5.80 and 6.00 μm with different power densities. As can be seen, for a wavelength of 5.80 μm, a large amount of demineralized dentin was removed compared with sound dentin. On the other hand, at a wavelength of 6.00 μm, the irradiation spots had similar sizes for sound and demineralized dentin, so that selective removal of demineralized dentin was not realized.
Table 2 shows differences in ablation depth for sound and demineralized dentin under different irradiation conditions. The values in brackets represent the actual ablation depths (in microns) for sound and demineralized dentin, respectively. Ablation depth differences of less than 0.5 μm were considered to be within the experimental error and were listed as zero. For almost all irradiation conditions, demineralized dentin was removed faster than sound dentin, leading to differences in ablation depth. In terms of high ablation speed for demineralized dentin and minimal damage to sound dentin, wavelengths of 5.75–5.80 μm, and average power densities of 30–40 W/cm2 were found to be optimal.
Figure 4 shows cross-sectional SEM images of the boundary (indicated by the dotted line) between the sound and demineralized dentin after irradiation at wavelengths of 5.80 and 6.00 μm for different times. Here, the demineralization time was about 12 h and this produced a demineralized layer with a thickness of about 50 μm on the plates. A single sample was used for each laser wavelength, and different regions of the two samples were irradiated for different times. It can be seen that longer irradiation times led to larger ablation depths. In the case of the wavelength of 6.00 μm, the ablation process did not terminate when the boundary was reached, so that for longer irradiation times, sound dentin was also removed. In contrast, at a wavelength of 5.8 μm, the ablation process is naturally terminated at the boundary, indicating highly selective removal of demineralized dentin.
Tensile bonding strength measurements
Figure 5 shows the results of tensile bonding strength measurements for an unirradiated sample, a sample irradiated using the DFG laser, and a sample irradiated using a standard Er:YAG dental laser. It can be seen that for optimized DFG laser conditions, the bonding strength is significantly higher than that obtained using the Er:YAG laser and is comparable with that for the unirradiated surface. This indicates that the DFG laser is compatible with dental restoration procedures using composite resin.
Discussion
The absorption coefficients (μ a) for the sound and demineralized dentin were 415 and 155 cm−1, respectively, at a wavelength of 5.80 μm. At the absorption peak wavelength of 6.00 μm, the corresponding values were 1024 and 2266 cm−1, respectively. The thermal relaxation time τ therm and stress relaxation time τ stress are given by
where δ p is the optical penetration depth (= 1/μ a), α is the thermal diffusivity, and c s is the speed of sound. The α value for dentin was taken to be 1.83 × 10−3 [12], and the c s values for the sound and demineralized dentin were taken to be 3.68 × 105 and 1.60 × 105 cm/s, respectively [13]. Using these parameters, τ therm and τ stress were calculated, and the results are shown in Table 3.
The interval between DFG laser pulses in the present study was 0.1 s, which is longer than τ therm for dentin. Thus, the interaction time τ int corresponds to the pulse duration (5 ns). Because τ int is comparable with τ stress, photomechanical interactions were induced. Under the conditions used in this study, it is considered that vaporization of organic material or hydroxyapatite was the dominant mechanism involved in ablation. In addition, when the demineralized dentin was irradiated at a wavelength of 5.80 μm, stress waves were generated because the stress confinement condition (τ int < τ stress) was satisfied.
As shown in Table 2, demineralized dentin was removed more rapidly than sound dentin, and differences in ablation depth were observed for almost all irradiation conditions. One reason for this is thought to be a difference in hardness between the sound and demineralized dentin. During the demineralization process, hydroxyapatite was eluted, leaving organic material as the basis of the demineralized dentin [14–18]. The increased ablation depth for demineralized dentin has been previously reported to be the result of its lower mechanical strength [19]. The ablation rate is considered to depend on mechanical properties such as hardness or elasticity. Neglecting the effects of bacteria or bacterial products, the demineralized dentin produced in the present study is expected to be very similar to carious dentin. Therefore, carious dentin is also expected to have a reduced hardness, allowing it to be selectively removed [20].
It has been reported that the mechanical properties are strongly affected by whether the tests are carried out under wet or dry conditions [17, 21–23]. In the present study, the dentin was completely dried, but in clinical situations, it may be wet or only dry on the surface. Angker et al. reported that sound dentin had almost the same hardness and elastic modulus whether it was wet or dry, whereas carious dentin was significantly softer when wet. This suggests that under clinical conditions, an even larger difference in ablation rate between sound and carious dentin would exist.
Selective removal of demineralized dentin was realized at a wavelength of 5.80 μm, since the stress confinement condition was satisfied, so that stress waves were generated in addition to vaporization. At other wavelengths, the stress confinement condition was not satisfied, so that the ablation process involved only vaporization of dentin tissue. Thus, a wavelength of 5.8 μm is superior for selective removal of demineralized dentin.
The tensile bonding strength between the composite resin and the dentin surface irradiated by the DFG laser was significantly higher than that for the surface irradiated using a standard dental Er:YAG laser. One factor that leads to a reduction in bonding strength is thought to be thermal damage to the irradiated dentin surface. This leads to degradation of the organic material which is the basis of demineralized dentin. The degree of thermal damage can be considered in terms of the thermal confinement condition, which is expressed as τ int < < τ therm. In the present study, τ int corresponds to the pulse duration τ d. If this condition is satisfied, the temperature rise in the dentin can be limited to the optical penetration region, and thermal damage does not extend into wider areas [24, 25]. Since for DFG laser irradiation at 5.80 μm, the τ d value of 5 ns is much smaller than the τ therm value of 800 μs, the thermal confinement condition is satisfied. Thus, less thermal damage to the dentin surface and good tensile bonding strength with the composite resin can be achieved. On the other hand, for the Er:YAG laser at a wavelength of 2.94 μm, the τd value is 250 μs, which is actually larger than the τ therm value of 140 μs, so that the thermal confinement condition is not satisfied. This leads to extended thermal damage over a wide area and a lower tensile bonding strength due to degradation of the dentin substrate. These results highlight the advantages of short laser pulses for achieving less thermal damage to the dentin surface and good tensile bonding strength.
Thermal effects on dental pulp vitality should be also considered when carrying out laser treatment for caries. In irradiated tissue, the optical penetration depth δ p (= 1/μ a) is defined as the depth at which the energy of incident light decreases to 1/e (= 37 %) of its original value and beyond this depth thermal effects can be considered to be small. For sound bovine dentin, δ p is about 24 μm at a wavelength of 5.80 μm, which is close to the dentin surface and far from the dental pulp. Therefore, no thermal effects on dental pulp vitality are expected, based on the optical properties of the tissue involved. However, further experiments taking pathological or biochemical effects into consideration should be carried out to determine if this is in fact the case.
Conclusion
The use of a nanosecond pulsed laser with a wavelength of 5.8 μm allowed the realization of selective removal of demineralized dentin with minimal damage to sound dentin. The irradiated surface exhibited a high tensile bonding strength with a composite resin, because the thermal confinement condition was satisfied. A future study will focus on the application of this method to human carious dentin.
References
Tyas MJ, Anusavice KJ, Frencken JE, Mount GJ (2000) Minimal intervention dentistry-a review. Int Dent J 50:1–12
Celiberti P, Francescut P, Lussi A (2006) Performance of four dentine excavation methods in deciduous teeth. Caries Res 40(2):117–123
Chimello-Sousa DT, de Souza AE, Chinelatti MA, Pecora JD, Palma-Dibb RG, Milori Corona SA (2006) Influence of Er:YAG laser irradiation distance on the bond strength of a restorative system to enamel. J Dent 34:245–251
Dunn WJ, Davis JT, Bush AC (2005) Shear bond strength and SEM evaluation of composite bonded to Er:YAG laser-prepared dentin and enamel. Dent Mater 21:616–624
Neves AA, Coutinho E, Munck JD, Meerbeek BV (2011) Caries-removal effectiveness and minimal-invasiveness potential of caries-excavation techniques: a micro-CT investigation. J Dent 39:154–162
Neves AA, Coutinho E, Cardoso MV, Munck JD, Meerbeek BV (2011) Micro-tensile bond strength and interfacial characterization of an adhesive bonded to dentin prepared by contemporary caries-excavation techniques. Dent Mater 27:552–562
Saiki M, Ishii K, Yoshikawa K, Yasuo K, Yamamoto K, Awazu K (2011) Selective treatment of carious dentin using a mid-infrared tunable pulsed laser at 6 μm wavelength range. Proc SPIE 7887:78840L
Saiki M, Ishii K, Yoshikawa K, Yasuo K, Yamamoto K, Awazu K (2011) Ablation of demineralized dentin using a mid-infrared tunable nanosecond pulsed laser at 6 μm wavelength range for selective excavation of carious dentin. Proc 33rd IEEE EMBS 318–321
Choi K, Oshida Y, Platt JA, Cochran MA, Matis BA, Yi K (2006) Microtensile bond strength of glass ionomer cements to artificially created carious dentin. Oper Dent 31(5):590–597
Uchizono T, Heya M, Awazu K, Sunada K, Yoshikawa K, Inoue K (2005) Comparison of absorption properties in the 9-μm-waveband between human and bovine dental enamels using a KBr-FTIR method. J Jpn Soc Laser Surg Med 25(4):265–272
Hazama H, Takatani Y, Awazu K (2007) Integrated ultraviolet and tunable mid-infrared laser source for analyses of proteins. Proc SPIE 6455:645507
Brown WS, Dewey WA, Jacobs HR (1970) Thermal properties of teeth. J Dent Res 49:752–755
Yasuda G, Inage H, Takamizawa T, Kurokawa H, Rikuta A, Miyazaki M (2007) Determination of elastic modulus of demineralized resin-infiltrated dentin by self-etch adhesives. Eur J Oral Sci 115:87–91
Featherstone JD, ten Cate JM, Shariati M, Arends J (1983) Comparison of artificial caries-like lesions by quantitative microradiography and microhardness profiles. Caries Res 17:385–391
Arends J, ten Bosch JJ (1992) Demineralization and remineralization evaluation techniques. J Dent Res 71:924–928
Kodaka T, Debari K, Yamada M, Kuroiwa M (1992) Correlation between microhardness and mineral content in sound human enamel (short communication). Caries Res 26:139–141
Kinney JH, Balooch M, Marshall SJ, Marshall GW Jr, Weihs TP (1996) Hardness and Young’s modulus of human peritubular and intertubular dentine. Arch Oral Biol 41:9–13
Angker L, Nockolds C, Swain MV, Kilpatrick N (2004) Correlating the mechanical properties to the mineral content of carious dentine—a comparative study using an ultra-micro indentation system (UMIS) and SEM-BSE signals. Arch Oral Biol 49:369–378
Osuka K, Amagai T, Kukidome N, Takase Y, Aida S, Hirai Y (2009) Effect of dentin hardness on ablation rate with Er:YAG laser. Photomed Laser Surg 27(3):395–399
Pugach MK, Strother J, Darling CL, Fried D, Gansky SA, Marshall SJ, Marshall GW (2009) Dentin caries zones: mineral, structure, and properties. J Dent Res 88(1):71–76
Kinney JH, Balooch M, Marshall GW, Marshall SJ (1993) Atomic-force microscopic study of dimensional changes in human dentine during drying. Arch Oral Biol 38:1003–1007
Marshall GW Jr (1993) Dentin: microstructure and characterization. Quintessence Int 24:606–617
Angker L, Nijhof N, Swain MV, Kilpatrick NM (2004) Influence of hydration and mechanical characterization of carious primary dentine using an ultra-micro indentation system (UMIS). Eur J Oral Sci 112:231–236
Youn JI, Holcomb JD (2012) Ablation efficiency and relative thermal confinement measurements using wavelengths 1,064, 1,320, and 1,444 nm for laser-assisted lipolysis. Lasers Med Sci 28(2):519–527
Heya M, Uchizono T, Awazu K (2005) Basic interactions of dental hard tissue with lasers. J Jpn Soc Laser Surg Med 36(4):323–331
Acknowledgments
This work was supported by JSPS KAKENHI Grant No. 24241029 and Tateishi Science and Technology Foundation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kita, T., Ishii, K., Yoshikawa, K. et al. In vitro study on selective removal of bovine demineralized dentin using nanosecond pulsed laser at wavelengths around 5.8 μm for realizing less invasive treatment of dental caries. Lasers Med Sci 30, 961–967 (2015). https://doi.org/10.1007/s10103-013-1517-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-013-1517-9