Abstract
Objectives
This retrospective study evaluated the visibility, location, and morphology of the primary maxillary ostium (PMO), as well as the presence and number of accessory maxillary ostia (AMO) in the maxillary sinus using cone beam computed tomography (CBCT).
Materials and methods
CBCT scans with a large field of view with both maxillary sinuses entirely visible, acquired from February 2016 to February 2018, were initially screened. Patients were included if there was no history of surgical intervention/trauma in the sinus region. Two observers evaluated the CBCTs for PMO and AMOs independently. PMO and AMOs were evaluated in axial, coronal, and sagittal CBCT views. In case of disagreement, a third observer served as a referee. The findings were correlated with age, gender, condition of the sinus mucosa, and status of the dentition to assess for potential influencing factors.
Results
A total of 184 patients (368 maxillary sinuses) were included. PMO was present and patent in 346 (94.0%) of the 368 analyzed sinuses. Most of the PMOs were located above the attachment of and in the middle third of the inferior turbinate (76.1%) and exhibited a slit shape (71.1%). An AMO was present in 167 (45.5%) of the 368 analyzed sinuses, and 66 (17.9%) sinuses had multiple AMOs. Gender and sinus mucosa morphology were found to be influencing factors for the patency of the PMO. Furthermore, gender seems to be influencing the presence of an AMO.
Conclusions
Most of the analyzed maxillary sinus cavities in the present population had a patent PMO. Being male and having morphological changes of the sinus mucosa were factors associated with a reduced prevalence of a patent PMO.
Clinical relevance
A maxillary sinus with pathological findings of the mucosa seems to have a reduced prevalence of patent PMOs. Therefore, clinicians should take care to assess any clinical and radiographical sign indicating a potential maxillary sinusitis prior to surgical interventions in this region, especially in cases with planned sinus floor elevation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Sinus floor elevation (SFE) procedures using a transcrestal or lateral window approach have become well-accepted surgical options in order to regenerate missing vertical bone in the atrophic posterior maxilla to facilitate the insertion of dental implants [1]. In addition to SFE, other oral surgical procedures such as apical surgery or the removal of impacted teeth in the posterior maxilla also risk to impinge on the integrity of the sinus, and thus, could cause pathological changes [2, 3]. It is therefore critical to confirm healthy conditions of the maxillary sinuses prior to oral surgical procedures in close relation to the sinus and to detect pathological changes of the sinus that might not only compromise the surgical outcome but also be aggravated following these surgical interventions. For assessment of maxillary sinus conditions, the preoperative use of a cone beam computed tomography (CBCT) has been recommended by various authors [4,5,6].
Timmenga and co-workers reported that following SFE procedures, a postoperative swelling of the Schneiderian membrane is a characteristic sequela [7]. Although the mucosa of the sinus seems to reconstitute itself quite rapidly after surgical interventions, its healing can be delayed and the risk of acute sinusitis is increased in case of a preexisting chronic sinusitis or an unfavorable anatomy of the ostiomeatal complex [7]. The development of postoperative maxillary sinusitis following SFE, although less common, is considered as a quite severe complication, since it not only compromises the outcome of sinus augmentation but it also affects the overall health of the patient [8]. Therefore, extending the CBCT’s field of view (FOV) to include the ostiomeatal complex may be justified to avoid postoperative complications [5].
The primary maxillary ostium (PMO) is an important anatomical entity since its patency ensures adequate mucociliar clearance and drainage of the sinus into the middle meatus of the nasal cavity to maintain a healthy sinus [9]. The PMO has been reported to be located on the superomedial aspect of the maxillary sinus [10], and blockage may result in a maxillary sinusitis, which may even spread to other paranasal sinuses, and thus results in a pansinusitis [11]. Inflammation in the maxillary sinus induces a mucosal thickening, which can be seen in computed tomography (CT) or CBCT images and may result in a total opacification of the affected maxillary sinus [11].
An accessory maxillary ostium (AMO) arises from a membranous area on the medial maxillary wall, situated between the uncinate process and the inferior concha, which is only covered by mucoperiosteum [9]. This area is known as “fontanelle” and has been reported to be potentially perforated by the pressure of pus and edema from recurrent episodes of sinusitis [4]. Interestingly, an AMO has been seen in 30% of the patients with chronic maxillary sinusitis in comparison to 10–20% in healthy subjects [12, 13].
Emphasizing the importance of a pneumatized ostium for common surgical procedures in dental medicine including SFE, apical surgery, or removal of impacted teeth in the posterior maxilla, the objective of the present study was to assess presence, location, shape and (radiographic) patency of PMOs, and presence and multiplicity of AMOs, using CBCT images. Additionally, potential influencing factors such as gender, age, changes of the sinus mucosa, and dentoalveolar pathology were evaluated.
Materials and methods
Study sample
This retrospective study included CBCT scans that were performed at Oral and Maxillofacial Radiology, Faculty of Dentistry, The University of Hong Kong. The indications for these CBCT scans varied from dental implant treatment planning, analysis prior to orthognathic surgery, removal of impacted teeth, to evaluation of cysts and neoplasias. Each scan was performed using a ProMax 3D Mid (Planmeca, Helsinki, Finland). All CBCTs were performed during a 2-year period (from February 2016 to February 2018) and were initially screened for inclusion of both maxillary sinuses on the scan. CBCTs were excluded, if one of the following exclusion criteria was present:
- 1.
Both maxillary sinuses are not entirely visible;
- 2.
History of surgical intervention/trauma to the maxillary sinus;
- 3.
Pathology from anterior teeth (canine-to-canine) impinged into the maxillary sinuses;
- 4.
Examinations exhibited insufficient image quality in the sinus region due to artifacts from acquisition or patient movement.
The medical history of the included patients was searched for their demographic data, including gender and age at the time of imaging. The study was conducted in full accordance with the Declaration of Helsinki 2013 (www.wma.net) concerning research on human subjects. The study protocol was approved by the local institutional review board (IRB) of the University of Hong Kong (HKU)/Hospital Authority Hong Kong West Cluster (approval number UW 18-227), and registered in the HKU Clinical Trials Registry (study identifier HKUCTR-2426).
CBCT image analysis
CBCT images were analyzed on a Philips 223 V LED monitor with a resolution of 1920 × 1080 pixels (Philips, Amsterdam, Netherlands). Data was reconstructed with slices of 0.5 mm thickness and a 0.4 mm voxel size. The image observations were performed using ROMEXIS Version 4.4.0.R software (Planmeca, Helsinki, Finland). Two examiners (NC and CM) read all images to test for inter-observer reproducibility and one examiner (NC) read them twice with a time gap of a minimum of 4 weeks between each observation to test for intra-observer repeatability. For each scan, the patient’s right sinus was assessed first, followed by the left sinus. A third examiner (AY) assessed the deviating findings from both observers to reach a final diagnosis, which was then utilized for further statistical analyses.
First, the presence of the primary ostium (PMO) was evaluated as:
- 1.
Radiologically absent or
- 2.
Radiologically present
If present, the patency of the PMO was assessed as:
- 1.
Obstructed or
- 2.
Patent
The location of the PMO was analyzed from its position on the medial maxillary sinus wall. The medial wall has a trapezoidal shape with a larger posterior side and is divided into a cranial and caudal part by the inferior turbinate [6]. PMO location was assessed in relation to the level of the inferior turbinate (IT) as visualized in Figs. 1 and 2:
- 1.
PMO location above attachment of and in the anterior third of the IT;
- 2.
PMO location above attachment of and in the middle third of the IT;
- 3.
PMO location above attachment of and in the posterior third of the IT;
- 4.
PMO location below attachment of and in the anterior third of the IT;
- 5.
PMO location below attachment of and in the middle third of the IT; or
- 6.
PMO location below attachment of and in the posterior third of the IT.
Schematic drawing of the medial wall of the maxillary sinus used for the localization of the primary maxillary ostium (PMO). The asterisk represents a possible localization for the PMO. This position (A) will be transferred to the inferior turbinate for classification (B; represented by the arrow). 1 = PMO location above attachment of and in the anterior third of the IT; 2 = PMO location above attachment of and in the middle third of the IT; 3 = PMO location above attachment of and in the posterior third of the IT; 4 = PMO location below attachment of and in the anterior third of the IT; 5 = PMO location below attachment of and in the middle third of the IT; 6 = PMO location below attachment of and in the posterior third of the IT
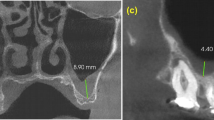
Representative CBCT images illustrating how the PMO position was determined. The actual antero-posterior position of the PMO in the a coronal image is represented by the green line on the b axial image. Meanwhile, the blue line indicates the level of height of the axial image. The transferred level of height is shown in the c coronal and d axial images. Panels a and c differ by only a change in the level of the axial plane as represented by the white arrow. The PMO depicted here would thus be classified as localized in region 2 (IT, inferior turbinate)
Based on findings from a cadaveric study by Prasanna et al. [14], the shape of the PMO was classified into one of the following forms:
- 1.
Round
- 2.
Ovaloid or
- 3.
Slit-shaped
Subsequently, for each maxillary sinus visible on the CBCT scan, the presence of an accessory ostium (AMO), within the fontanelle region of the medial maxillary wall, was assessed as (Fig. 3):
- 1.
Radiologically absent or
- 2.
Radiologically present
In addition, the potential presence of multiple AMOs in the fontanelle region was coded as follows:
- 1.
Single or
- 2.
Multiple
Secondary variables regarding the status of the maxillary sinus and the dentition were included to assess a potential correlation with PMO patency, AMO presence, and number. For the Schneiderian membrane and its bony lining, the status was recorded according to adapted classification from Soikkonen and Ainamo (1995) as used in previous studies [15,16,17,18,19]:
- 1.
Inconspicuous or up to 4 mm thickening of the sinus membrane;
- 2.
Flat, shallow thickening of the Schneiderian membrane (> 4 mm);
- 3.
Semispheric thickening of the membrane (suspected mucous retention cyst);
- 4.
Complete opacification of the sinus;
- 5.
Mixed flat and semispherical thickenings; or
- 6.
Other (e.g., bone destruction, cyst, foreign body, and suspected neoplasia).
For all patients included, the status of the dentition distal to the maxillary canine, with inclusion of the third molar, was classified into:
- 1.
Dentate
- 2.
Partially edentulous or
- 3.
Completely edentulous
If teeth were present in the posterior maxilla, their statuses were evaluated to account for potential endodontic or periodontal pathology that could influence the status of the maxillary sinus. The endodontic status of teeth in the respective posterior maxilla was classified into (assigning the largest code value whenever applicable):
- 1.
No endodontic pathology or treatment;
- 2.
Endodontic treatment(s) without visible pathology; or
- 3.
Apical lesion(s) with or without visible endodontic treatment(s).
Similarly, teeth with periodontal pathology were classified into (assigning the largest code value whenever applicable):
- 1.
No periodontal lesions;
- 2.
Horizontal and/or vertical periodontal bone lesions deeper than the midlevel of the respective root without furcation involvement; or
- 3.
Periodontal lesions with furcation involvement.
Statistical analysis
All data were analyzed descriptively first. Cohen kappa values were calculated for intra-observer repeatability and inter-observer reproducibility [20]. The evaluations of influencing factors on PMO patency and AMO presence and multiplicity were done on a patient level (age and gender) and a sinus level (PMO location and shape, morphology of the Schneiderian membrane and its bony lining, status of dentition, endodontic, and periodontal pathology), respectively. Potential influencing factors on PMO patency and AMO presence or number were evaluated with either chi-square test, Mann–Whitney U test, or Fisher’s exact tests. The significance level chosen for all statistical tests was p < 0.05. All analyses were performed in SPSS (Version 25.0, IBM Corp., Armonk, New York, USA).
Results
Patient population
Initially, a total of 250 CBCT scans with a medium to large FOV were screened. From these, 66 CBCT scans were excluded. Thus, a total of 184 CBCT scans (368 sinuses) fulfilled the inclusion criteria. The 184 patients consisted of 119 females and 65 males with a mean age of 30.9 years (range from 18 to 86 years). The FOV (in millimeter, diameter × height) of the CBCT scans was 20 × 17 for 150 patients, 20 × 10 for 27 patients, 10 × 10 for 5 patients, and 10 × 6 for 2 patients.
The majority of the sinuses was considered to be healthy or with a shallow Schneiderian membrane thickening of < 4 mm (72.6%) and associated with a dentate dentition (63.6%) with no endodontic pathology or treatment (91.2%) and no periodontal bone loss (76.7%; Table 1). The most frequent morphological change of the Schneiderian membrane were semispheric mucosal thickenings (17.7%).
Intra- and inter-observer agreement
Intra-observer repeatability (Table 2) was very high regarding the presence, patency, location, and shape of the PMO (Kappa values/κ = 0.90, 0.88, 0.88, and 0.87, respectively), and the presence and number of the AMOs (κ = 0.92 and 0.97, respectively). The inter-observer reproducibility regarding the presence and patency of the PMO exhibited substantial values (κ = 0.63 and 0.71, respectively). The reproducibility regarding the location and shape of the PMO and the presence and number of the AMO exhibited a low to moderate agreement (Table 2).
Characteristics of PMO and AMO
A PMO was present and patent in 346 (94.0%) of the 368 analyzed sinuses (Table 3). Nine PMOs were present but diagnosed as obstructed (Table 3). All of these nine PMO obstructions were unilateral cases. Most of the PMOs were located above the attachment of and in the middle third of the IT (76.1%) (Table 3). None of the PMOs were located below the attachment of the IT. The majority of the PMOs were slit-shaped (71.1%) followed by an ovoloid shape (22.3%). Meanwhile, an AMO was present in 167 (45.5%) of the 368 analyzed sinuses (Table 4). Multiple AMOs were observed in 66 (17.9%) of the 368 sinuses.
Potential influencing factors on the characteristics of PMO and AMO
For the PMO and AMO, the analysis for potential influencing factors showed that the location, shape, endodontic, and periodontal pathology did not have a significant influence on patency, AMO presence, and number (Table 5). Meanwhile, a significantly higher ratio of females had a patent PMO (96.2 versus 90.0%, p = 0.016) and was also diagnosed with the presence of an AMO (51.7 versus 33.8%, p = 0.001). A PMO was also more likely to be patent if the sinus was healthy instead of exhibiting mucosal changes/pathology (95.5 versus 82.2%, p < 0.001).
Age seemed to be an influencing factor on the number of AMOs diagnosed, as patients with multiple AMOs (median age = 23.7 years) were generally younger than those without or only one AMO (median age = 26.4; p = 0.018). The status of the dentition was also an influencing factor on the number of detected AMOs, with dentate patients having a higher ratio of multiple AMOs, followed by partially edentulous and finally completely edentulous patients (47.4% versus 30.2% versus 14.3%, p = 0.036).
Discussion
The present study included CBCT images of 368 maxillary sinuses from 184 patients to assess morphological characteristics of PMOs and AMOs as seen on radiographic images, and also to investigate whether age, gender, pathological changes of the sinus mucosa, or dentoalveolar pathology may be factors that influence these features. Results showed that a PMO was present and patent in 94.0% of maxillary sinuses and over 70% of them present as slit-shaped. The middle third above the attachment of the inferior turbinate is the most common location for the PMO. Females had a significant higher incidence of PMO patency than males. PMOs in combination with pathological changes of the sinus mucosa present a lower incidence of PMO patency compared to healthy maxillary sinuses. Furthermore, this study also reported that the presence of an AMO was observed in 45.5% (167/368) of maxillary sinuses, and 17.9% (66/368) of the sinuses present multiple AMOs.
Previous CT/CBCT studies have reported that the incidence of patent PMOs ranged from 73.5 to 89.2% [21,22,23]. One cadaveric study reported that a PMO was present in 36 (90%) of the 40 specimens [14]. Our study found that 96.5% (355/368) of the maxillary sinuses evaluated had a clearly visible PMO, of which 94.0% (346/355) were patent. The PMO was not detected in very few maxillary sinuses (3.5%, 13/368), and this was due to mucosal thickening at the sinus ostium region or complete obstruction of the maxillary sinus. Previous studies have reported that most of the PMOs presented in the upper third, few in the middle third, and none in the lower third of the medial wall of the maxillary sinus [24, 25]. Additionally, Prasanna et al. [14] and Singhal et al. [26] reported in a cadaveric study that most PMOs (52.5 and 84.2%) were located in the posterior third of the infundibulum. Another cadaveric study described that the PMOs were mostly found (71.8%) in the posterior third of the uncinate groove [27]. Similar to these investigations, the present study found that all observed PMOs were located above the attachment of the interior turbinate and mostly (76.1%, 270 out of 355) in the middle third in relation to the anterior-posterior direction.
Blockage of the PMO could compromise sinus drainage, and therefore result in a maxillary sinusitis or even a pansinusitis [11]. Obstruction of the ostium can be a direct result of surgical interventions in the maxillary sinus [28] and has also been described more specifically following SFE procedures [7, 21]. Some studies stated that performing SFE in patients with an obstructed PMO may increase the risk of developing a sinusitis [29, 30]. This shows that not only PMO obstruction occurs as a result of sinus pathology, but sinus pathology may also develop as a result of PMO obstruction. Carmeli et al. reported that a sinus membrane thickening of > 5 mm is associated with a progressively increasing risk for PMO obstruction following sinus grafting [23]. Moreover, apical lesions can exhibit an intimate relation with the floor of the maxillary sinus, which increases the risk of oro-antral communications following an apical surgery [2]. As reported in previous studies [21,22,23], sinuses with mucosal changes/pathology had a significantly higher incidence of having an obstructed PMO in the population assessed in the present study. Therefore, if maxillary sinuses exhibit clinical or radiographic signs of sinus pathology, and particularly if there is a need for a surgical intervention that requires a considerable amount of grafting, the patency and location of the PMO should be carefully assessed prior to the procedure to avoid iatrogenic blockage of the ostium.
Several cadaveric and endoscopic studies have reported the incidence of an AMO varying from 0 to 43% [31]. Some studies reported that approximately one-half to one-third of the sinuses with an AMO exhibited more than one [9, 31, 32]. Compared to cadaveric and endoscopic examinations, CBCT imaging may increase the accuracy of identifying small anatomical variations in the maxillary sinus [33]. In the current study, using 3D radiography, the presence of an AMO was found in 167 (45.5%) of the 368 sinuses, which is slightly above the range reported by previous studies. Similar to the previous studies, approximately one-third (39.5%, 66/167) of the sinuses had more than one AMO. Although it has been reported in the literature that an AMO can emerge as a result of a pathological change within the respective maxillary sinus, and then tends to stay open [9], our results were unable to demonstrate this association between the presence of an AMO and sinus pathology.
Interestingly, being female has been shown to be of a main influencing factor for a higher incidence of PMO patency in this study. This finding might be related to differences in the sinus conditions between females and males. In the present study, females presented a higher incidence of healthy maxillary sinus than males, and a healthy maxillary sinus was associated with a significantly higher incidence of PMO patency.
The ideal field of view (FOV) needed for CBCTs to assess PMOs and AMOs is not yet clearly defined in the literature [33]. There is insufficient evidence to recommend a general use of large FOVs for preoperative CBCT examinations for sinus-related surgeries including SFE, apical surgery, or the removal of impacted teeth in the posterior maxilla [33]. Moreover, it is worth noting that potential negative effects to the eye lens of large volume 3D craniofacial imaging have been mentioned [34, 35]. To adhere to ALADA (i.e., “As Low As Diagnostically Acceptable”) principles [36], it should be emphasized not to indiscriminately scan bilateral sinuses entirely to limit radiation dose exposure to the field of interest only. Extending the FOV to include the entire maxillary sinus with the PMO is thus only recommended when there are obvious clinical or radiographic signs indicating sinus pathology including an impaired sinus drainage that could jeopardize the outcome of surgical procedures [5, 33].
One of the major limitations of the present study is that the CBCT images analyzed were retrospectively collected from patients referred for implant treatment planning, orthognathic surgery, impacted teeth, cysts, and neoplasias. Furthermore, the included patients were generally younger (mean age 31 years). Considering that CBCT diagnostic imaging in patients referred to receive implant placement in the posterior maxilla comprises a generally older subject group [37], a prospective study specifically addressing differences of PMO patency prior to SFE would be needed to further assess its clinical relevance.
Conclusions
Based on the findings of this retrospective analysis of 184 CBCT scans, the following conclusions can be made:
PMOs were present and patent in 346 (94.0%) of the 368 analyzed sinuses.
Most of the PMOs were located in the middle third above the attachment of the inferior turbinate (76.1%) and exhibited a slit shape (71.1%).
An AMO was present in 167 (45.5%) of the 368 analyzed sinuses, and 66 (17.9%) sinuses had multiple AMOs.
Regarding PMOs, gender and sinus mucosal morphology were influencing factors for their patency.
Regarding AMOs, gender was an influencing factor on presence, and patient age and status of dentition were influencing factors on number.
References
Wallace SS, Tarnow DP, Froum SJ, Cho S-C, Zadeh HH, Stoupel J, Del Fabbro M, Testori T (2012) Maxillary sinus elevation by lateral window approach: evolution of technology and technique. J Evid Based Dent Pract 12:161–171
Hauman C, Chandler N, Tong D (2002) Endodontic implications of the maxillary sinus: a review. Int Endod J 35:127–141
Hasegawa T, Tachibana A, Takeda D, Iwata E, Arimoto S, Sakakibara A, Akashi M, Komori T (2016) Risk factors associated with oroantral perforation during surgical removal of maxillary third molar teeth. Oral Maxillofac Surg 20:369–375
Ali IK, Sansare K, Karjodkar FR, Vanga K, Salve P, Pawar AM (2017) Cone-beam computed tomography analysis of accessory maxillary ostium and Haller cells: prevalence and clinical significance. Imaging Sci Dent 47:33–37
Harris D, Horner K, Gröndahl K, Jacobs R, Helmrot E, Benic GI, Bornstein MM, Dawood A, Quirynen M (2012) E.A.O. Guidelines for the use of diagnostic imaging in implant dentistry 2011. A consensus workshop organized by the European Association for Osseointegration at the Medical University of Warsaw. Clin Oral Implants Res 23:1243–1253
Rege IC, Sousa TO, Leles CR, Mendonça EF (2012) Occurrence of maxillary sinus abnormalities detected by cone beam CT in asymptomatic patients. BMC Oral Health 12:30
Timmenga NM, Raghoebar GM, Liem RS, Van Weissenbruch R, Manson WL, Vissink A (2003) Effects of maxillary sinus floor elevation surgery on maxillary sinus physiology. Eur J Oral Sci 111:189–197
Chirilă L, Rotaru C, Filipov I, Săndulescu M (2016) Management of acute maxillary sinusitis after sinus bone grafting procedures with simultaneous dental implants placement–a retrospective study. BMC Infect Dis 16(Suppl 1):94
Kumar H, Choudhry R, Kakar S (2001) Accessory maxillary ostia: topography and clinical application. J Anat Soc India 50:3–5
Sarna A, Hayman LA, Laine FJ, Taber KH (2002) Coronal imaging of the osteomeatal unit: anatomy of 24 variants. J Comput Assist Tomogr 26:153–157
Laine F, Smoker W (1992) The ostiomeatal unit and endoscopic surgery: anatomy, variations, and imaging findings in inflammatory diseases. AJR Am J Roentgenol 159:849–857
Joe JK, Ho SY, Yanagisawa E (2000) Documentation of variations in sinonasal anatomy by intraoperative nasal endoscopy. Laryngoscope 110:229–235
Jones N (2002) CT of the paranasal sinuses: a review of the correlation with clinical, surgical and histopathological findings. Clin Otolaryngol Allied Sci 27:11–17
Prasanna L, Mamatha H (2010) The location of maxillary sinus ostium and its clinical application. Indian J Otolaryngol Head Neck Surg 62:335–337
Bornstein MM, Horner K, Jacobs R (2017) Use of cone beam computed tomography in implant dentistry: current concepts, indications and limitations for clinical practice and research. Periodontol 2000 73:51–72
Schneider AC, Brägger U, Sendi P, Caversaccio MD, Buser D, Bornstein MM (2013) Characteristics and dimensions of the sinus membrane in patients referred for single-implant treatment in the posterior maxilla: a cone beam computed tomographic analysis. Int J Oral Maxillofac Implants 28:587–596
Soikkonen K, Ainamo A (1995) Radiographic maxillary sinus findings in the elderly. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 80:487–491
Yeung AWK, Tanaka R, Khong PL, von Arx T, Bornstein MM (2018) Frequency, location, and association with dental pathology of mucous retention cysts in the maxillary sinus. A radiographic study using cone beam computed tomography (CBCT). Clin Oral Investig 22:1175–1183
Bornstein MM, Yeung AWK, Tanaka R, von Arx T, Jacobs R, Khong PL (2018) Evaluation of health or pathology of bilateral maxillary sinuses in patients referred for cone beam computed tomography using a low-dose protocol. Int J Periodontics Restorative Dent 38:699–710
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Shanbhag S, Karnik P, Shirke P, Shanbhag V (2014) Cone-beam computed tomographic analysis of sinus membrane thickness, ostium patency, and residual ridge heights in the posterior maxilla: implications for sinus floor elevation. Clin Oral Implants Res 25:755–760
Dobele I, Kise L, Apse P, Kragis G, Bigestans A (2013) Radiographic assessment of findings in the maxillary sinus using cone-beam computed tomography. Stomatologija 15:119–122
Carmeli G, Artzi Z, Kozlovsky A, Segev Y, Landsberg R (2011) Antral computerized tomography pre-operative evaluation: relationship between mucosal thickening and maxillary sinus function. Clin Oral Implants Res 22:78–82
Souza AD, Rajagopal KV, Ankolekar VH, Souza ASD, Kotian SR (2016) Anatomy of maxillary sinus and its ostium: a radiological study using computed tomography. CHRISMED J Health Res 3:37–40
May M, Sobol SM, Korzec K (1990) The location of the maxillary os and its importance to the endoscopic sinus surgeon. Laryngoscope 100:1037–1042
Singhal MD, Singhal D (2013) Maxillary sinus ostium - morphology and its clinical relevance. CIBTech J Surg 2:26–29
Van Alyea OE (1936) The ostium maxillare: anatomic study of its surgical accessibility. Arch Otolaryngol 24:553–569
Brook I (2009) Sinusitis. Periodontol 2000(49):126–139
Manor Y, Mardinger O, Bietlitum I, Nashef A, Nissan J, Chaushu G (2010) Late signs and symptoms of maxillary sinusitis after sinus augmentation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 110:e1–e4
Doud Galli SK, Lebowitz RA, Giacchi RJ, Glickman R, Jacobs JB (2001) Chronic sinusitis complicating sinus lift surgery. Am J Rhinol 15:181–186
Mahajan A, Mahajan A, Gupta K, Verma P, Lalit M (2017) Anatomical variations of accessory maxillary sinus ostium: an endoscopic study. Int J Anat Res 5:3484–3490
Singhal M, Singhal D (2014) Anatomy of accessory maxillary sinus ostium with clinical application. Int J Med Sci Public Health 3:327–329
Vogiatzi T, Kloukos D, Scarfe WC, Bornstein MM (2014) Incidence of anatomical variations and disease of the maxillary sinuses as identified by cone beam computed tomography: a systematic review. Int J Oral Maxillofac Implants 29:1301–1314
Pauwels R, Zhang G, Theodorakou C, Walker A, Bosmans H, Jacobs R, Bogaerts R, Horner K (2014) Effective radiation dose and eye lens dose in dental cone beam CT: effect of field of view and angle of rotation. Br J Radiol 87(1042):20130654
Seals K, Lee E, Cagnon C, Al-Hakim R, Kee S (2016) Radiation-induced cataractogenesis: a critical literature review for the interventional radiologist. Cardiovasc Intervent Radiol 39:151–160
Jaju PP, Jaju SP (2015) Cone-beam computed tomography: time to move from ALARA to ALADA. Imaging Sci Dent 45:263–265
Brugger OE, Bornstein MM, Kuchler U, Janner SF, Chappuis V, Buser D (2015) Implant therapy in a surgical specialty clinic: an analysis of patients, indications, surgical procedures, risk factors, and early failures. Int J Oral Maxillofac Implants 30:151–160
Acknowledgments
The authors are grateful to Ms. Kar Yan Li, Centralised Research Lab, Faculty of Dentistry, The University of Hong Kong, for her valuable assistance regarding the statistical analysis.
Funding
This study has been funded by departmental funds only. No external funding has been received.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed were in accordance with the ethical standards of the institutional and/or national research committee and with the Declaration of Helsinki (2013). The study protocol was submitted to and approved by the local institutional review board (IRB) of the University of Hong Kong/Hospital Authority Hong Kong West Cluster (approval number UW 18-227).
Informed consent
For this type of study (retrospective study) formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yeung, A.W.K., Colsoul, N., Montalvao, C. et al. Visibility, location, and morphology of the primary maxillary sinus ostium and presence of accessory ostia: a retrospective analysis using cone beam computed tomography (CBCT). Clin Oral Invest 23, 3977–3986 (2019). https://doi.org/10.1007/s00784-019-02829-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-019-02829-9