Abstract
Extensive research supports an association between radiation exposure and cataractogenesis. New data suggests that radiation-induced cataracts may form stochastically, without a threshold and at low radiation doses. We first review data linking cataractogenesis with interventional work. We then analyze the lens dose typical of various procedures, factors modulating dose, and predicted annual dosages. We conclude by critically evaluating the literature describing techniques for lens protection, finding that leaded eyeglasses may offer inadequate protection and exploring the available data on alternative strategies for cataract prevention.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The lens is a highly radiosensitive tissue, with an association between cataracts and radiation exposure being postulated within a year of Roentgen discovering the X-ray [1]. The latency period between irradiation and cataract formation is inversely proportional to dose and ranges from years to decades [2]. Radiation is traditionally associated with the posterior subcapsular cataract (PSC), an uncommon cataract type often secondary to diabetes or systemic corticosteroids [3].
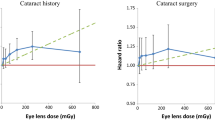
A point of contention in the literature is whether radiation-induced cataractogenesis is a stochastic or deterministic phenomenon. Initially, researchers believed that cataracts develop deterministically and thus require a threshold radiation dose and damage to multiple cells [4]. This is presumed by the current International Commission on Radiological Protection (ICRP) model, which defines exposure thresholds below which opacities do not form. New data suggests that cataracts may form stochastically, without a threshold dose and potentially in response to the damage of a single cell [5]. Multiple studies in non-interventionist populations have predicted threshold values statistically equivalent to or near zero [6–8]. If cataracts develop deterministically, increased exposure levels will result in more severe cataracts [9]. If they develop stochastically, however, dose will influence the likelihood but not the severity of the cataract. Further, a stochastic mechanism suggests that any low radiation dose has the potential to cause damage.
Many researchers have studied the mechanism of radiation-induced cataractogenesis. Brown reviews general mechanisms of radiation tissue damage, which include both direct, and free radical mediated injury [10]. Ocular radiation primarily affects the germinative dividing cells of the anterior lens epithelium [7]. These aberrant cells migrate to the posterior pole, creating the classic radiation-associated PSC. Given the avascular nature of the lens, there is no mechanism for removal of damaged cells, and they accumulate with time to form a cataract. An intermediate stage in cataract formation, posterior subcapsular opacification, occurs prior to the development of symptomatic cataract as these cells accumulate [5]. Although this process is irreversible, symptomatic cataract can be avoided if radiation exposure is limited during this intermediate stage. Cataract formation is believed to relate to the genotoxicity of radiation exposure [5]. This is supported by heightened cataractogenesis in animals with mutations in genes critical to the regulation of cell division and DNA repair, including Atm, Brca1, and Rad9 [4, 11]. This genetic basis for cataract development is consistent with stochastic behavior in which damage to a single aberrant cell is passed to future cells to form a cataract.
The lens of the interventionist is exposed to radiation primarily due to scatter from the patient [12]. Despite the need for excellent stereotactic vision in interventional work, interventionists often pay little attention to basic lens protection practices, with data showing that leaded eyeglasses are worn by <30 % of operators [13, 14] and dosimeter use is inconsistent [15]. This practice is believed to relate to either discomfort associated with leaded glasses or a lack of knowledge regarding radiation safety [16]. We believe the current review is important given data showing that radiation safety education improves outcomes, both increasing eyeglass use and decreasing interventionist dose [17, 18].
In this review, we examine radiation-induced cataractogenesis from the perspective of the interventional radiologist. We first review literature linking radiation exposure and cataract development. We then review research describing the lens dose typical of various interventional procedures, factors modulating dose, and predicted annual doses. We conclude by reviewing techniques for lens protection, focusing on their strengths and weaknesses, and the optimal protection strategy for the interventional radiologist.
Radiation Exposure and Cataract Development
Many studies have shown a relationship between lens exposure and cataract development. The ICRP, an independent international organization of radiation experts whose recommendations are frequently the basis for radiation protection programs [19], previously defined the threshold dose for protracted radiation causing detectable opacities or symptomatic cataracts as 5 and 8 Sv, respectively. These values were derived from early research that was limited by short follow-up times, high exposure doses, and poor sensitivity for detecting early lens changes [20]. Later work revealed that cataracts form at lower doses, potentially without a threshold. These studies examined an assortment of populations, including atomic bomb survivors [21], Chernobyl cleanup workers [8], astronauts [22], radiologic technicians [23], and patients exposed to radiotherapy [24]. These data motivated the ICRP to modify their guidelines in 2011, decreasing the threshold for detectable opacities or symptomatic cataract to 0.5 Sv [20]. Further, they reduced the occupational dose limit for lens equivalent dose to 20 mSv/year averaged over defined 5-year periods with no single year exceeding 50 mSv. Previously, 150 mSv/year was recommended. The Nuclear Regulatory Commission (NRC), a federal regulatory agency in the United States, is reviewing the ICRP recommendations for possible implementation into federal US guidelines [25].
Many excellent reviews summarize the data across multiple populations supporting the ICRP threshold reduction [1, 2, 4, 5, 26]. The current review will describe the data that is specific to interventionist populations. Given the similarities in technique between interventional radiology (IR) and cardiology (IC), we will review data describing cataracts in both of these groups. Further, given data showing that IR doses are higher than IC doses [27], it follows that studies showing cataract risk in cardiologists imply a comparable or higher risk in interventional radiologists.
Early research raised suspicion that interventional radiologists are at risk of cataract formation. Vano provided a case series on cataract development in IR suites not optimized for interventional work [28], finding dot-like subcapsular cataracts in multiple staff members and bilateral posterior subcapsular condensation in one physician. Another early study examined cataract development in 59 interventional radiologists, with no lens opacification in 53 %, posterior subcapsular dot-like opacities in 37 %, and PSCs in 8 % [29]. The authors state that cataract risk increased with years of interventional work and that compliance with protective eyewear appears to reduce cataract risk.
The occupational cataracts and lens opacities in interventional cardiology (O’CLOC) study explored cataract development in the interventional cardiologist [16]. In this study, 106 French cardiologists were compared with a control group of 99 unexposed employees of a radiation safety agency. A questionnaire regarding work history quantified cumulative lens dose. Posterior subcapsular opacities were three times more common in cardiologists, with a significant increase in risk after correcting for age, sex, smoking, and various other confounders. The majority of the opacities were low grade (83 % LOCS III stage 1), and nuclear and cortical cataract rates did not differ significantly between groups. Increased risk was not seen in interventionists using lead glasses at least 75 % of the time. Adjusted odds ratio increased with more years of interventional work, although there was not a clear relationship between odds ratio and the starting date of IC activity or the cumulative number of procedures.
The retrospective evaluation of lens injuries and dose (RELID) trial, which consisted of multiple studies, examined cataracts in interventional cardiologists and paramedical personnel attending cardiology conferences [21, 30–32]. The control group consisted of conference attendees without history of radiation exposure and interventionist lens dose was quantified using a work history questionnaire. In all RELID studies, interventionalists were found to have a significantly increased risk of posterior lens opacification. Support staff, however, displayed significantly increased risk in only two of the four studies. Most lens opacities were low grade, with only 5 % of opacities seen in one study exceeding the lowest grading score [32]. The influence of these opacities on vision is unclear, as only one study assessed vision and this was done in a preliminary manner without a control group [31]. Multiple studies demonstrated increased posterior opacity risk with increased total lens dose [31, 32], although one study showed higher risk in individuals with less exposure [21]. This inconsistency was likely due to inaccuracy in the questionnaire method of dose assessment. One study demonstrated that interventionists with opacities had more years of work experience and less use of dosimetry, eyeglasses, and protective screens [31]. Additionally, this study showed positive correlation between lens dose and cataract severity.
In conjunction with decades of research across diverse populations linking radiation exposure and cataracts, these data suggest that interventional radiologists are at risk of cataract development. A summary of the data is provided in Table 1. While most opacities in these studies are small and without influence on visual acuity, the natural history of these inconsequential opacities is evolution into larger lesions that reduce vision and require surgery [30]. The current research has a number of limitations. A retrospective questionnaire approach cannot accurately estimate lens dose, as operator recall regarding decades of work is questionable and numerous complex factors influence dose that may differ between facilities and operators. It is crucial that future research uses dosimetry to quantify lens dose. Correlating lens dose with cataract severity may offer insight into the stochastic versus deterministic nature of radiation-induced cataractogenesis, as only a deterministic mechanism predicts worse cataract at higher lens dose. Another flaw in the current literature is that study cohorts are small, the largest being the 106 cardiologists of the O’CLOC study. Larger trials are needed to confirm the generalizability of these findings and decrease the probability of selection bias. Selection bias is of particular concern in the RELID trials, which utilize experimental and control groups comprised volunteers attending cardiology conferences. In the future, a larger trial using prospective dosimetry and careful sample selection is essential to refining our understanding of cataract risk in IR.
Quantifying Lens Exposure in Interventional Radiology
Many studies quantify lens irradiation during interventional procedures. If lens dose during these procedures exceeds the cataract threshold, radiologists are at risk of cataract development. As we detailed previously, significant controversy exists regarding this threshold, with some arguing that there is cataract risk for any lens dose. In this review, we examine IR doses from the perspective of the widely accepted ICRP guidelines. The ICRP states that cataracts may develop above a threshold cumulative absorbed dose of 0.5 Sv, recommending an annual occupational dose limit of 20 mSv [20]. In this section, we summarize the available data on lens dose in a wide variety of interventional procedures, analyzing findings from both phantom and human studies.
A rich source of data describing lens dose in IR was provided by the optimization of radiation protection of medical staff (ORAMED) study [14]. ORAMED was designed to acquire standardized data on lens and extremity exposure in IR and IC procedures, with lens doses quantified for nearly 1300 procedures across 34 institutions. Studied procedures included radiofrequency ablation, embolization, and angiography/angioplasty. Ceiling-suspended shields were used for lens protection in some, but not all, cases. The highest lens dose was seen in embolization, with a mean of 60 µSv. Although the mean values for other procedures were lower, maximal doses of approximately 1 mSv were seen occasionally in most procedures. This illustrates the wide dosing variability seen in IR, which is believed to relate to operator experience, case complexity, image acquisition protocol, and many other factors. Table 2 summarizes the ORAMED data for various procedures. The authors also estimated total annual lens dose for 16 operators, with six physicians (37.5 %) meeting or exceeding the current ICRP occupational dose limit.
Another ORAMED study also examined lens dose in a variety of IR procedures [33]. Lens dose was quantified for two operators, with both exceeding the ICRP dose limit at estimated annual doses of 49.3 and 71.6 mSv/year. Of note, the operator with the higher dose performed embolization using the biplane technique, which was found in another study to increase dose-area-product by 36 % and is believed to increase lens irradiation [34, 35]. Embolization resulted in the highest single procedure lens dose (2.4 mSv) as well as the highest lens dose/KAP. A second component of this study used a PMMA phantom to estimate lens dose during a variety of fluoroscopy projections. Dose rate was lowest for the caudal projection and highest for the LAO90 projection, with a relatively high dose for RAO90 and low doses for the PA and RAO30 projections.
Research by Hidajat explored the amount of radiation delivered to interventionists performing the transjugular intrahepatic portosystemic shunt (TIPS) procedure [36]. This procedure delivers a high radiation dose to patients since fluoroscopy time is high and patient ascites often necessitates high voltage and tube current [37]. As such, high operator dose is anticipated due to scatter. Data were collected for 18 TIPS procedures utilizing a ceiling-suspended screen, with average lens doses of 0.403 and 0.229 mSv for the right and left eye, respectively, and a mean fluoroscopy time of 77.8 min. Under the current ICRP guidelines, physicians performing 50 TIPS procedures annually would exceed the cataract dose limit. This number would likely be considerably lower in the absence of shielding.
Vano quantified lens exposure in a phantom study using imaging protocols typical of various interventional procedures [38]. Data were collected using seven imaging systems performing fluoroscopy, DSA, and cine cardiac imaging. Imaging parameters used in specific IR procedures were gathered from the literature [39]. There was considerable variability in lens dose between the seven fluoroscopic systems, with dose rate in high-dose fluoroscopy ranging from 0.37 to 2.44 mSv/h. Lens dose increased with patient phantom thickness, consistent with increased patient scatter in a larger patient. Dose rate varied substantially between projections, with the highest dose in LAO90 and low doses for the RAO30 and PA projections, in agreement with the Koukorava study [33]. The greatest lens doses in the simulated procedures were seen in cranial neuroembolization (11.20 mSv), spinal neuroembolization (11.00 mSv), and TIPS (3.72 mSv). Given a standard workload of 3–5 procedures/day, these data suggest that IR physicians likely exceed the cataract dose limit if lens protection is not used.
A number of additional studies provide valuable lens dose information. One study found low lens doses in neurointerventional procedures performed using a ceiling-suspended shield [40]. Efstathopoulos showed that, despite using a ceiling-suspended shield, a radiologist performing vertebroplasty with monoplane fluoroscopy was predicted to exceed the ICRP dose limit at 27.9 mSv/year [27]. Harstall studied orthopedic surgeons performing vertebroplasty with C-arm fluoroscopy and predicted a lower annual dose of 11.9 mSv [41]. Directly comparing these studies is difficult, however, given differences in technique between C-arm and monoplane fluoroscopy. Another study analyzed CT-guided biopsies and drainages, finding low lens doses unlikely to exceed the ICRP dose limit [42]. A topic of interest in future lens dose research is CT fluoroscopy, which is known to deliver higher radiation doses than single-slice CT acquisition [43]. One study found that, over 82 consecutive procedures, CT fluoroscopy delivered a median per procedure eye level dose of 0.21 mSv [44]. Another study analyzing 220 CT fluoroscopy procedures found a low operator lens dose of 0.010 mSv/procedure, likely due to selection of a low milliampere value and usage of a quick-check technique similar to conventional CT [45]. More data is needed to further characterize the cataract risk and lens dose characteristics of CT fluoroscopy.
The literature discussed in this section highlights the potential for cataract induction in a standard IR workload. A summary of lens dose in various interventions is seen in Table 2. A number of procedures result in a particularly high lens exposure, including embolization, vertebroplasty, and TIPS. Values in these studies may underestimate clinical reality, as experimental subjects may modify their behavior to minimize lens dose. Dose variability for the same procedure within and across studies is high, often exceeding an order of magnitude. Dosimeter type, calibration, and positioning likely contribute to this variability. Other factors include case complexity, operator experience, operator height, patient body habitus, imaging technique, age of imaging equipment, and shield use and placement strategy. This variability underscores the importance of dosimetry, as numerous complex factors influence lens dose such that it is difficult to make predictions for a particular case based on values seen in the literature. As such, the available data is not particularly useful in the quantitative dose values it provides. Rather, it is useful in that multiple studies predict a lens dose that approaches or exceeds the ICRP dose limit for cataract formation. It is thus critical that radiologists utilize lens protection and perform careful dosimetry to quantify the lens dose characteristic of their clinical practice as recommended by the Society of Interventional Radiology (SIR), Cardiovascular and Interventional Society of Europe (CIRSE), and ICRP [19].
Techniques for Minimizing Lens Exposure
Various techniques have been used to minimize radiation exposure to the physician and support staff during interventional procedures. In this section, we review lens protection techniques. While the scope of this review is limited to techniques that directly relate to the lens, general radiation safety practices can also substantially reduce lens dose and should always be followed [19]. A general protection technique of particular interest is the development of improved fluoroscopy systems using novel hardware and image processing techniques that may substantially reduce patient and operator radiation dose [46–49]. Additional research is needed to determine the impact of these novel systems on operator lens dose.
Leaded eyeglasses are perhaps the most fundamental technique for lens protection. Research has shown great variability in the protection afforded by leaded glasses, with one review finding an attenuation range across studies from 35 to >95 % [50]. Phantom studies offer important insight into the protective effect of leaded eyeglasses. One study assessed an interventionist phantom wearing three eyeglass models, two with higher lead equivalence (0.75 mm) and a third model with larger lenses of lower lead equivalence (0.07 mm) [51]. With the phantom facing the source, higher lead equivalence resulted in better protection. When the phantom was placed at increasing angles to the source, however, lens geometry became increasingly important and the thinner, larger lens was more effective than one of the thicker models. Another study assessed the influence of operator head position [52]. For frontal irradiation of the phantom placed at the level of the simulated patient, dose reduction between eyeglass models ranged from a factor of 7.9–10. With the phantom situated above the table in an orientation similar to an IR physician, however, the protective effect of the eyeglasses was diminished. Similarly, another phantom study showed inferior protection for radiation from below rather than frontal radiation [53]. The dependence on radiation angle and eyeglass geometry seen in these studies likely relates to the presence of vulnerable regions not protected by the eyeglasses, such as the openings where the eyeglasses interface with the cheek and nose. Geber evidenced this point with films showing the distribution of radiation within the phantom [53] and further support was provided by Monte Carlo simulations [54].
Research has also measured the in vivo dose reduction offered by leaded eyeglasses. Comparing 10 lens types, including lenses capable of attenuating a direct X-ray beam >1000 times in phantom studies, one study found that lens irradiation during patient fluoroscopy was reduced at best by a factor of 5.3 [55]. Challa found that eyeglasses reduced lens dose in cardiology procedures to the left and right eye by 67 and 45 %, respectively [56], and a similar cardiology study found a left eye dose reduction of only 35 % [57]. Another study assessed eyeglass protection in a wide range of interventional procedures, finding a dose reduction factor of 2.1 for the left (tube-side) eye and no significant dose reduction for the right eye [52].
These data suggest that the lens protection afforded by leaded eyeglasses is variable and incomplete in certain circumstances (Table 3). Nonetheless, data consistently show that eyeglasses offer some benefit, including a study demonstrating a lower rate of cataractogenesis with consistent eyeglass use [16]. The variability in efficacy may relate to the fit between a particular eyeglass model and the unique facial anatomy of the operator, a topic that should be studied further to optimize eyeglass design. This concept is supported by both the phantom studies discussed above and Monte Carlo simulations suggesting that these gaps represent the primary source of scatter radiation reaching the lens [54]. Research shows poor compliance with leaded eyeglasses despite their known benefits [15, 58], possibly due to eyeglass discomfort [16]. As such, another important component of eyeglass development is the creation of more ergonomic eyeglass models that provide more efficient lens protection.
Leaded shields represent another fundamental technique for lens protection. Usage of the ceiling-suspended shield in the in vivo arm of the van Rooijen study reduced radiation to the left and right eye by a factor of 5.7 and 4.8, respectively [52]. The Koukorova phantom study found that shielding reduced lens dose by 98 % [33]. Analyzing cardiologists performing coronary angiography, Maeder showed that shielding reduced DAP-normalized lens dose by a factor of 19 [59]. In the ORAMED study, ceiling-suspended shields reduced lens dose in embolization and ERCP but not lower limb angiography [14]. The authors state that ineffective shielding likely occurred when the shield was improperly placed. A phantom study simulating cardiac interventions offered some insight into shield positioning by showing that dose reduction ranged from ~20 to 80 % based on shield position [60]. Optimal protection was seen with the shield abutting the patient and adjacent to the access point, whereas inferior protection was seen when the shield was lifted above the patient or moved away from the access point towards the source.
Multiple studies support the efficacy of ceiling-suspended shields. In general, shielding offers protection that is superior to that of leaded eyeglasses [50, 52, 61]. Shielding avoids the gaps in the protective barrier that plague leaded eyeglasses and provides excellent protection for both eyes. A primary weakness of the shielding approach, however, is that shielding cannot be utilized in all procedures due to space constraints. There also seems to be variability in shield efficacy related to the specifics of shield positioning [14, 60], and further research is needed to clarify optimal shield position for various access points. In addition, research should further explore specialized systems that combine multiple shielding materials for comprehensive protection [62, 63]. These systems show potential in current literature and may eventually obviate the need for leaded gowns or eyeglasses.
Radiation-absorbing surgical drapes also have utility in lens protection. Research has explored disposable, lead-free drapes containing bismuth and barium that block scatter radiation from the patient [64]. Studies across a variety of interventional procedures have demonstrated that drapes reduce operator lens dose in a statistically significant manner [60, 64–67] (Table 3). In one study, the drapes provided significant protection despite the use of a ceiling-suspended shield, suggesting the attenuation of radiation not blocked by shielding [67]. These drapes have a number of benefits, including lens protection, ease of use, and operator comfort. Furthermore, studies analyzing both phantoms [68, 69] and in vivo cardiology procedures [70–72] suggest the drapes protect regions other than the lens. A potential disadvantage of the drapes is additional per-procedure cost, although this expense is relatively trivial at $39 US/drape [69]. In addition, there is theoretical concern that in some positions the drapes may obstruct the primary beam and cause increased lens dose via automatic brightness control feedback [66].
Two additional strategies are believed to have utility in minimizing lens exposure. First, a growing body of data shows that formal training in radiation safety reduces operator dose [17, 18], and a joint guideline statement by the SIR and CIRSE emphasized the importance of radiation safety training. Second, appropriate dosimeter use is critical to a clear understanding of lens dose. The ICRP recommends wearing a minimum of two dosimeters, one at the collar above the apron and one below the apron, with the collar dosimeter allowing for lens dose estimation [19]. The SIR and CIRSE support this recommendation [19].
A variety of approaches offer substantial lens protection. A summary of the various protection techniques is provided in Table 3. Further research is needed to determine the optimal means of lens protection, both minimizing lens dose and maximizing operator comfort and function.
Conclusions
In this text, we review radiation-induced cataractogenesis and techniques for lens protection. A review of the literature allows us to establish a number of general conclusions. First, radiation-induced cataractogenesis may be stochastic rather than deterministic, and any lens exposure may have associated cataract risk. Second, a wealth of evidence suggests that IR work increases the probability of cataract development. Further research is needed to clarify the details of this response, including dose thresholds and the likelihood of progression to symptomatic cataract requiring treatment. Data also suggests that standard IR workloads have the potential to deliver lens doses exceeding the ICRP occupational dose limit if radiation protection tools are not properly used. Furthermore, the available dose data may actually underestimate clinical reality if studied interventionists modify their behavior to reduce dose. Given the immense variability in per procedure lens dose, IR physicians should monitor their own exposure using an above-apron dosimeter. Finally, protective measures should be used routinely, including leaded eyeglasses in all cases and protective screens when practically feasible. Radiation-absorbing drapes may also reduce lens exposure. Given data suggesting that radiation safety compliance is poor due to an insufficient understanding of risk, we hope that the current review increases awareness and results in heightened efforts for lens protection.
References
Shore RE, Neriishi K, Nakashima E. Epidemiological studies of cataract risk at low to moderate radiation doses: (not) seeing is believing. Radiat Res. 2010;174:889–94.
Hammer GP, Scheidemann-Wesp U, Samkange-Zeeb F, Wicke H, Neriishi K, Blettner M. Occupational exposure to low doses of ionizing radiation and cataract development: a systematic literature review and perspectives on future studies. Radiat Environ Biophys. 2013;52:303–19.
Robman L, Taylor H. External factors in the development of cataract. Eye. 2005;19:1074–82.
Ainsbury EA, Bouffler SD, Dörr W, et al. Radiation cataractogenesis: a review of recent studies. Radiat Res. 2009;172:1–9.
Jacob S, Michael M, Brezlin A, Laurier D, Bernier M-O. Ionizing radiation as a risk factor for cataract: what about low-dose effects?. Clin Exp Ophthalmol. 2011.
Nakashima E, Neriishi K, Minamoto A. A reanalysis of atomic-bomb cataract data, 2000–2002: a threshold analysis. Health Phys. 2006;90:154–60.
Neriishi K, Nakashima E, Minamoto A, et al. Postoperative cataract cases among atomic bomb survivors: radiation dose response and threshold. Radiat Res. 2007;168:404–8.
Worgul BV, Kundiyev YI, Sergiyenko NM, et al. Cataracts among Chernobyl clean-up workers: implications regarding permissible eye exposures. Radiat Res. 2007;167:233–43.
Miller DL, Balter S, Schueler BA, Wagner LK, Strauss KJ, Vañó E. Clinical radiation management for fluoroscopically guided interventional procedures. Radiology. 2010;257:321–32.
Brown KR, Rzucidlo E. Acute and chronic radiation injury. J Vasc Surg. 2011;53:15S–21S.
Worgul BV, Smilenov L, Brenner DJ, Junk A, Zhou W, Hall EJ. Atm heterozygous mice are more sensitive to radiation-induced cataracts than are their wild-type counterparts. Proc Natl Acad Sci USA. 2002;99:9836–9.
Vano E, Gonzalez L, Fernandez JM, Prieto C, Guibelalde E. Influence of patient thickness and operation modes on occupational and patient radiation doses in interventional cardiology. Radiat Prot Dosim. 2006;118:325–30.
Ainsbury EA, Bouffler S, Cocker M, et al. Public health England survey of eye lens doses in the UK medical sector. J Radiol Prot. 2014;34:15–29.
Vanhavere F, Carinou E, Domienik J, et al. Measurements of eye lens doses in interventional radiology and cardiology: final results of the ORAMED project. Radiat Meas. 2011;46:1243–7.
Niklason LT, Marx MV, Chan HP. Interventional radiologists: occupational radiation doses and risks. Radiology. 1993;187:729–33.
Jacob S, Boveda S, Bar O, et al. Interventional cardiologists and risk of radiation-induced cataract: results of a French multicenter observational study. Int J Cardiol. 2013;167:1843–7.
Abatzoglou I, Koukourakis M, Konstantinides S. Reduction of the radiation dose received by interventional cardiologists following training in radiation protection. Radiat Prot Dosim. 2013;155:119–21.
Sheyn DD, Racadio JM, Ying J, Patel MN, Johnson ND. Efficacy of a radiation safety education initiative in reducing radiation exposure in the pediatric IR suite. Pediatr Radiol. 2008;38:669–74.
Miller DL, Vañó E, Bartal G, et al. Occupational radiation protection in interventional radiology: a joint guideline of the Cardiovascular and Interventional Radiology Society of Europe and the Society of Interventional Radiology. J Vasc Interv Radiol. 2010;21:607–15.
Stewart FA, Akleyev AV, Hauer-Jensen M, et al. ICRP publication 118: ICRP statement on tissue reactions and early and late effects of radiation in normal tissues and organs–threshold doses for tissue reactions in a radiation protection context. Ann ICRP. 2012;41:1–322.
Ciraj-Bjelac O, Rehani M, Minamoto A, Sim KH, Liew HB, Vano E. Radiation-induced eye lens changes and risk for cataract in interventional cardiology. Cardiology. 2012;123:168–71.
Cucinotta FA, Manuel FK, Jones J, et al. Space radiation and cataracts in astronauts. Radiat Res. 2001;156:460–6.
Chodick G, Bekiroglu N, Hauptmann M, et al. Risk of cataract after exposure to low doses of ionizing radiation: a 20-year prospective cohort study among US radiologic technologists. Am J Epidemiol. 2008;168:620–31.
Hall P, Granath F, Lundell M, Olsson K, Holm LE. Lenticular opacities in individuals exposed to ionizing radiation in infancy. Radiat Res. 1999;152:190–5.
Piccone J. New International Commission on Radiological Protection: recommendations on the Annual Dose Limit to the Lens of the Eye. Federal Register. 2011. Web. 2014.
Shore RE. Radiation impacts on human health: certain, fuzzy, and unknown. Health Phys. 2014;106:196–205.
Efstathopoulos EP, Pantos I, Andreou M, et al. Occupational radiation doses to the extremities and the eyes in interventional radiology and cardiology procedures. Br J Radiol. 2011;84:70–7.
Vañó E, González L, Beneytez F, Moreno F. Lens injuries induced by occupational exposure in non-optimized interventional radiology laboratories. Br J Radiol. 1998;71:728–33.
Junk A, Haskal Z, Worgul B. Cataract in interventional radiology—an occupational hazard? Invest Ophthalmol Vis Sci. 2004;45:388.
Vano E, Kleiman NJ, Duran A, Rehani MM, Echeverri D, Cabrera M. Radiation cataract risk in interventional cardiology personnel. Radiat Res. 2010;174:490–5.
Vano E, Kleiman NJ, Duran A, Romano-Miller M, Rehani MM. Radiation-associated lens opacities in catheterization personnel: results of a survey and direct assessments. J Vasc Interv Radiol. 2013;24:197–204.
Ciraj-Bjelac O, Rehani MM, Sim KH, Liew HB, Vano E, Kleiman NJ. Risk for radiation-induced cataract for staff in interventional cardiology: is there reason for concern? Catheter Cardiovasc Interv. 2010;76:826–34.
Koukorava C, Carinou E, Simantirakis G, et al. Doses to operators during interventional radiology procedures: focus on eye lens and extremity dosimetry. Radiat Prot Dosim. 2011;144:482–6.
Lie Ø, Paulsen GU, Wøhni T. Assessment of effective dose and dose to the lens of the eye for the interventional cardiologist. Radiat Prot Dosim. 2008;132:313–8.
Sadick V, Reed W, Collins L, Sadick N, Heard R, Robinson J. Impact of biplane versus single-plane imaging on radiation dose, contrast load and procedural time in coronary angioplasty. Br J Radiol. 2010;83:379–94.
Hidajat N, Wust P, Kreuschner M, Felix R, Schröder RJ. Radiation risks for the radiologist performing transjugular intrahepatic portosystemic shunt (TIPS). Br J Radiol. 2006;79:483–6.
McParland BJ. A study of patient radiation doses in interventional radiological procedures. Br J Radiol. 1998;71:175–85.
Vano E, Gonzalez L, Fernández JM, Haskal ZJ. Eye lens exposure to radiation in interventional suites: caution is warranted. Radiology. 2008;248:945–53.
Miller DL, Balter S, Cole PE, et al. Radiation doses in interventional radiology procedures: the RAD-IR study: part I: overall measures of dose. J Vasc Interv Radiol. 2003;14:711–27.
Anastasian ZH, Strozyk D, Meyers PM, Wang S, Berman MF. Radiation exposure of the anesthesiologist in the neurointerventional suite. Anesthesiology. 2011;114:512–20.
Harstall R, Heini PF, Mini RL, Orler R. Radiation exposure to the surgeon during fluoroscopically assisted percutaneous vertebroplasty: a prospective study. Spine. 2005;30:1893–8.
Heusch P, Kröpil P, Buchbender C, et al. Radiation exposure of the radiologist’s eye lens during CT-guided interventions. Acta Radiol. 2014;55:86–90.
Kloeckner R, dos Santos DP, Schneider J, Kara L, Dueber C, Pitton MB. Radiation exposure in CT-guided interventions. Eur J Radiol. 2013;82:2253–7.
Buls N, Pagés J, de Mey J, Osteaux M. Evaluation of patient and staff doses during various CT fluoroscopy guided interventions. Health Phys. 2003;85:165–73.
Paulson EK, Sheafor DH, Enterline DS, McAdams HP, Yoshizumi TT. CT fluoroscopy–guided interventional procedures: techniques and radiation dose to radiologists. Radiology. 2001;220:161–7.
Dekker LR, van der Voort PH, Simmers TA, et al. New image processing and noise reduction technology allows reduction of radiation exposure in complex electrophysiologic interventions while maintaining optimal image quality: a randomized clinical trial. Heart Rhythm. 2013;10:1678–82.
Racadio J, Strauss K, Abruzzo T, et al. Significant dose reduction for pediatric digital subtraction angiography without impairing image quality: preclinical study in a piglet model. Am J Roentgenol. 2014;203:904–8.
Söderman M, Holmin S, Andersson T, Palmgren C, Babic D, Hoornaert B. Image noise reduction algorithm for digital subtraction angiography: clinical results. Radiology. 2013;269:553–60.
Söderman M, Mauti M, Boon S, et al. Radiation dose in neuroangiography using image noise reduction technology: a population study based on 614 patients. Neuroradiology. 2013;55:1365–72.
Kim KP, Miller DL. Minimising radiation exposure to physicians performing fluoroscopically guided cardiac catheterisation procedures: a review. Radiat Prot Dosim. 2009;133:227–33.
Sturchio GM, Newcomb RD, Molella R, Varkey P, Hagen PT, Schueler BA. Protective eyewear selection for interventional fluoroscopy. Health Phys. 2013;104:S11–6.
van Rooijen BD, de Haan MW, Das M, et al. Efficacy of radiation safety glasses in interventional radiology. Cardiovasc Intervent Radiol. 2014;37:1149–55.
Geber T, Gunnarrson M, Mattsson S. Eye lens dosimetry for interventional procedures e Relation between the absorbed dose to the lens and dose at measurement positions In. Radiat Meas. 2011;46:1238–51.
Koukorava C, Farah J, Struelens L, et al. Efficiency of radiation protection equipment in interventional radiology: a systematic Monte Carlo study of eye lens and whole body doses. J Radiol Prot. 2014;34:509–28.
Moore WE, Ferguson G, Rohrmann C. Physical factors determining the utility of radiation safety glasses. Med Phys. 1980;7:8–12.
Challa K, Warren SG, Danak S, Bates MC. Redundant protective barriers: minimizing operator occupational risk. J Interv Cardiol. 2009;22:299–307.
Dash H, Leaman DM. Operator radiation exposure during percutaneous transluminal coronary angioplasty. J Am Coll Cardiol. 1984;4:725–8.
Donadille L, Carinou E, Brodecki M, et al. Staff eye lens and extremity exposure in interventional cardiology: Results of the ORAMED project. Radiat Meas. 2011;46:1203–9.
Maeder M, Brunner-La Rocca HP, Wolber T, et al. Impact of a lead glass screen on scatter radiation to eyes and hands in interventional cardiologists. Catheter Cardiovasc Interv. 2006;67:18–23.
Fetterly KA, Magnuson DJ, Tannahill GM, Hindal MD, Mathew V. Effective use of radiation shields to minimize operator dose during invasive cardiology procedures. JACC Cardiovasc Interv. 2011;4:1133–9.
Thornton RH, Dauer LT, Altamirano JP, Alvarado KJ. St Germain J, Solomon SB. Comparing strategies for operator eye protection in the interventional radiology suite. J Vasc Interv Radiol. 2010;21:1703–7.
Marichal DA, Anwar T, Kirsch D, et al. Comparison of a suspended radiation protection system versus standard lead apron for radiation exposure of a simulated interventionalist. J Vasc Interv Radiol. 2011;22:437–42.
Fattal P, Goldstein JA. A novel complete radiation protection system eliminates physician radiation exposure and leaded aprons. Catheter Cardiovasc Interv. 2013;82:11–6.
Kloeze C, Klompenhouwer EG, Brands PJ, van Sambeek MR, Cuypers PW, Teijink JA. Editor’s choice–Use of disposable radiation-absorbing surgical drapes results in significant dose reduction during EVAR procedures. Eur J Vasc Endovasc Surg. 2014;47:268–72.
King JN, Champlin AM, Kelsey CA, Tripp DA. Using a sterile disposable protective surgical drape for reduction of radiation exposure to interventionalists. Am J Roentgenol. 2002;178:153–7.
Simons GR, Orrison WW. Use of a sterile, disposable, radiation-absorbing shield reduces occupational exposure to scatter radiation during pectoral device implantation. Pacing Clin Electrophysiol. 2004;27:726–9.
Politi L, Biondi-Zoccai G, Nocetti L, et al. Reduction of scatter radiation during transradial percutaneous coronary angiography: a randomized trial using a lead-free radiation shield. Catheter Cardiovasc Interv. 2012;79:97–102.
Sawdy JM, Gocha MD, Olshove V, et al. Radiation protection during hybrid procedures: innovation creates new challenges. J Invasive Cardiol. 2009;21:437–40.
Dromi S, Wood BJ, Oberoi J, Neeman Z. Heavy metal pad shielding during fluoroscopic interventions. J Vasc Interv Radiol. 2006;17:1201–6.
Germano JJ, Day G, Gregorious D, Natarajan V, Cohen T. A novel radiation protection drape reduces radiation exposure during fluoroscopy guided electrophysiology procedures. J Invasive Cardiol. 2005;17:469–72.
Murphy JC, Darragh K, Walsh SJ, Hanratty CG. Efficacy of the RADPAD protective drape during real world complex percutaneous coronary intervention procedures. Am J Cardiol. 2011;108:1408–10.
Brambilla M, Occhetta E, Ronconi M, Plebani L, Carriero A, Marino P. Reducing operator radiation exposure during cardiac resynchronization therapy. Europace. 2010;12:1769–73.
Funding
All authors report no financial support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
All authors declare that they have no conflict of interest.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors. IRB approval was not required for this literature review.
Informed Consent
None.
Rights and permissions
About this article
Cite this article
Seals, K.F., Lee, E.W., Cagnon, C.H. et al. Radiation-Induced Cataractogenesis: A Critical Literature Review for the Interventional Radiologist. Cardiovasc Intervent Radiol 39, 151–160 (2016). https://doi.org/10.1007/s00270-015-1207-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-015-1207-z