Abstract
Objectives
The aim of this study is to evaluate the effect of operators experience and skill on treatment results of initial non-surgical periodontal therapy.
Materials and methods
Initial periodontal treatment was carried out by either second-year periodontal residents (PR) or last year dental students (DS). From the treatment records of patients in each group, plaque and bleeding indices, and pocket depth (PD) at baseline and at re-evaluation were collected retrospectively on each tooth at six locations. Data were separated according to tooth type, area, and probing depth categories, sub-grouped to 1–3, 4–5, and ≥ 6 mm.
Results
Fifty and 49 records of DS and PR patients, accordingly, were analyzed. Initial periodontal treatment improved patient compliance in both groups and reduced signs of inflammation with significantly superior results in the PR group. Significant change in percentage of pockets was recorded in each category. The increase in percentage of sites with PD 1–3 mm and decrease in percentage of PD ≥ 6 mm pockets was significantly (p ≤ 0.001) superior in patients treated by PR. Percentage of 4–5 mm pockets was significantly reduced in both groups (p ≤ 0.01), with a significantly greater reduction in the mandibular molar and anterior teeth in the PR group.
Conclusions
Experience and skill significantly affect the outcome of non-surgical periodontal therapy, with more positive improvement in patient compliance and clinical parameters when performed by a more qualified operator.
Clinical relevance
Improvement of operator skills may decrease the number of residual pockets and increase patient compliance following non-surgical periodontal treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The first step of periodontal therapy consists of non-surgical mechanical therapy, i.e., efficient personal plaque control and supra- and sub-gingival scaling and root planing [1, 2]. It is followed by the diagnostic re-evaluation phase during which the need for further treatment, usually surgical, is established [3]. The well-validated beneficial effects of this treatment on the periodontal tissues are reduced inflammation and decreased probing depth [4,5,6,7]. These changes are due to a reduction in the quantity of living bacteria in the microbial biofilm, and that of calcified biofilm microorganisms of the dental calculus [8] and a microbial shift to a less pathogenic flora [6, 9,10,11,12]. The magnitude of the changes is related to the initial pocket depth [13, 14], quality of oral hygiene [4, 10, 15, 16], and systemic factors [17].
The amount of residual plaque and calculus is severely impacted by restricted access and thus directly related to the probing depth present at the time of initial instrumentation [18]. Complete plaque and calculus removal is more difficult in deep than in shallow pockets, i.e., probing depth ≤ 3 mm (success fairly good), 3–5 mm (failure becomes greater), and > 5 mm (more likely to fail) [8, 18,19,20,21,22].
An important factor in the final result of sub-gingival debridement is operator experience [23, 24]. The more experienced operators produce a significantly greater number of calculus-free root surfaces in moderate and deep pockets [25, 26]. Results suggest that in molars with furcation involvement, although both surgical access and a more experienced operator significantly enhance calculus removal, total calculus removal may be limited [27]. Many clinical studies assess the efficacy of various periodontal treatment modalities, but limited numbers of studies take the differences in operator experience and skill into consideration. Badersten et al. [28] reported that the effect of operator variability on results of non-surgical periodontal therapy is minimal. However, since the above study design did not include molar teeth and oral hygiene instructions were not given to the patient by the operator who performed the scaling and root planing procedures, these results could be problematical.
Therefore, the aim of the present retrospective study was to assess whether the experience and skill of the operator performing the initial non-surgical periodontal treatment affect the clinical outcome as measured during the re-evaluation phase.
Material and methods
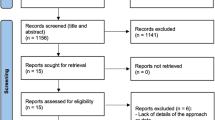
The study was approved by the Tel Aviv University Ethics Committee. Data were collected from periodontal records of two groups of patients treated for periodontal disease by either second-year periodontal residents (PR) or last year (second clinical year) dental students (DS). The background of the operators was as follows:
Dental students have been trained in SRP on manikin according to systematic guidelines for the use of hand instruments during 14 h of tuition by experienced periodontists, Periodontal Department members. The students are assessed by a final examination, after which, they are eligible to treat patients under supervision. The students are trained to use an ultrasonic scaler while they treat patients under supervision of experienced periodontists.
Periodontal residents are licensed dentists working as general practitioners during 2–5 years since their graduation. The periodontal residents are given 3 h refreshment/calibration tuition on the subject of SRP by the Periodontal Department experienced periodontists.
Criteria for patients’ data inclusion, in this retrospective study, were moderate-to-advanced periodontitis with no previous periodontal treatment within 12 months prior to treatment. Patients in need of prophylactic antibiotics, smokers, diabetes, and those diagnosed as suffering from aggressive periodontal disease were excluded. From the baseline examination, the following parameters were traced on each tooth with the exception of the wisdom tooth: Plaque Index (PI) [29], Bleeding Index (BI) [30], and pocket depth (PD) at six locations (facial, lingual, and proximal).
As recorded in the medical files, patients were instructed by their personal operator (PR or DS) in oral hygiene techniques based on intrasulcular brushing and interdental cleaning with dental floss and/or interproximal brushes according to guidelines recommended by the Department of Periodontology. Reinstruction and reinforcement of oral hygiene protocols were provided during the appointments. Supra- and sub-gingival instrumentation was carried out under local anesthesia. Both, ultrasonic and hand instruments (Gracey curettes 1/2, 7/8, 11/12, and 13/14, and Universal curettes 13/14) were used for scaling and root planing (SRP) by the operators in DS and PR groups.
According to the files, re-evaluation of the periodontal condition was carried out by the same treating operator 6 to 8 weeks after completion of the non-surgical initial therapy [31], and PI, BI, and PD were re-recorded.
All the relevant data were collected from the medical files and divided according to oral site (maxilla, mandibula, buccal, lingual/palatal, interproximal) and tooth type. The pocket depth measurements were categorized in three subgroups: shallow (1–3 mm), moderate (4–5 mm), and deep (≥ 6 mm). The data were analyzed using Student’s t test and ANOVA with repeated measures, with significance level of p ≤ 0.05.
Results
Records of 99 patients, in age range from 19 to 72 years (mean 42 ± 10.6 years), were included in the study, 50 were treated by 26 dental students (DS group), and 49 were treated by 10 periodontal residents (PR group). All treatments of an individual patient were performed by the same operator.
Dental plaque
Initially, plaque was shown on 59% (DS) and 72% (PR) of the treated tooth surfaces. At re-evaluation, plaque levels dropped significantly (p ≤ 0.001) to 42% (DS) and 28% (PR). Reduction was significantly (p ≤ 0.001) more pronounced in patients treated by PR (44%) than patients treated by DS (16.5%).
All area-specific plaque scores were significantly (p ≤ 0.001) lower in the PR group (Table 1).
Bleeding on probing
At initial examination, 29.5% (DS) and 49% (PR) of the sites showed bleeding on probing, which were markedly (p ≤ 0.001) reduced to 15% (DS) and 17% (PR) at re-evaluation. All sites improved, but significantly greater improvement (p ≤ 0.001) was recorded in the PR group (Table 1).
Probing depth
Initial probing was as follows: 60% of the sites in PR group and 78% in DS group were in the range of 1–3 mm depth, 24.5% (PR) and 18% (DS) were in the range of 4–5 mm depth, and 14.5% (PR) and 4% (DS) were ≥ 6 mm (Table 1). After mechanical therapy, both groups showed significant change in percentage of sites in each pocket category when re-evaluated.
Percentage of sites with 1–3 mm depth increased significantly (p ≤ 0.001) to 74 (PR) and 85.5% (DS) with significantly superior improvement (p ≤ 0.01) in the PR group (14%) compared to the DS group (7.75%).
Percentage of sites with 4–5 mm depth decreased significantly (p ≤ 0.01) in both groups to 18% (PR) and 12% (DS) with non-significant Δ difference (p = 0.893) between groups (6.6 vs. 6.4%). However, the shift was tooth type and tooth area specific, i.e., treatment in the PR group resulted in a significant reduction (p ≤ 0.008) compared to the DS group in the B/L maxilla anterior teeth and M/D area of mandibular molars.
Percentage of sites with ≥ 6 mm depth decreased significantly (p ≤ 0.001) in both groups to 6.7 (PR) and 2.24% (DS) with a significantly greater change (p ≤ 0.001) in the PR (8%) group compared to the DS (1.5%) group. The PR operators’ better performance was statistically significant in the maxilla at the B/P and M/D surfaces of anterior teeth and M/D surfaces of premolars, and in the mandible at the M/D surfaces of premolars and molars.
Discussion
In the present retrospective study, patients were subjected to a non-surgical treatment based on plaque control instruction, scaling, and root planing. The objectives of this treatment regime were to resolve inflammation and arrest the progression of periodontal disease. The treatment outcome was reflected in the patient’s compliance with the suggested oral hygiene regime (plaque scores) and in the periodontal condition (bleeding scores and pocket depth measurements).
A significant positive treatment outcome was shown regardless of the operator’s experience, i.e., patients’ periodontal status improved by both experienced and less experienced operators. Nevertheless, the more experienced operators achieved significantly superior results with concern to patient compliance and periodontal parameters (Plaque Index, Bleeding Index, and pocket depth).
Non-surgical periodontal therapy consists of instructions in self-administered oral health care measures directed towards reducing the bacterial load in the supra-gingival area. Satisfactory oral hygiene combined with sub-gingival debridement initiates and improves healing response. In the absence of adequate oral hygiene measures, the healing response is reduced [10, 32]. In the present study, the mean plaque control record of 42% among the DS group at re-evaluation can be categorized as moderate-to-poor compliance [33], which probably reduced the healing response and influenced the clinical outcome of the given non-surgical treatment. Furthermore, in the DS group, the significantly lower patient compliance in oral hygiene exposes these individuals to a higher risk regarding short-term beneficial results of the initial therapy and to disease recurrence [16, 34,35,36,37]. The average patient has difficulty in changing oral hygiene habits. It is not known why some individuals are more easily motivated than others with no association between various patient characteristics and outcome of oral hygiene instruction [38, 39]. The level of oral hygiene before therapy may be an indicator to future efficacy in plaque removal, i.e., patients with greater than 50% plaque (on the O’Leary Index) do not improve oral hygiene over time, but patients with less than 50% show marked improvement with oral hygiene instruction [40]. In the present study, plaque scores were greater than 50% at baseline in both groups. At the re-evaluation appointment, patients treated by PR operators presented low level of supragingival plaque (28% on the O’Leary Index), significantly lower as compared to patients treated by DS. Those results certainly reflect the superiority of the PR operator in patient motivation/instruction. It can be speculated that the PR group, favored by their professional confidence, succeeded to create an atmosphere of utmost importance with respect to plaque control. Their skill and experience contributed to successful communication and provided constructive guidance, together with reinforcement and positive feedback, which raised the patient’s performance level.
Bleeding on probing indicates gingival inflammation and is considered as a more sensitive sign of gingival inflammation/healing response than visual alteration [41,42,43]. Furthermore, bleeding shows some relationship to the presence of residual calculus as clinically determined [44]. There is a linear correlation between probing force and bleeding on probing percentage. Thus, the use of uncontrolled forces may result in a proportion of false-positive Bleeding Index readings [45]. Therefore, the dental students and the periodontal residents are instructed, trained, and supervised to perform careful probing by the experienced periodontists members of the Periodontal Department. The present study showed that in both groups, the mechanical non-surgical debridement improved the gingival health, as measured by percentage of non-bleeding sites, with a greater improvement in patients treated by more experienced operators.
Probing depth at re-evaluation is one of the criteria used to measure the results of the initial treatment and to decide whether supplementary surgical treatment is required. [46]. According to the results, an identical reduction in percentage of moderate pockets (6%) is achieved in both—the PR and DS groups. It can be speculated that there is an explanation for this outcome. It is well established that instrumentation of pockets below a “critical probing depth” of approximately 2.9 mm can cause immediate attachment loss [47, 48]. That loss does not always recover [7, 49] and may account for the increase in percentage of moderate pockets (4–5 mm). In deep pockets (≥ 6 mm), a 1.5–2.3 mm pocket reduction can be expected following non-surgical treatment [14]. Therefore, the observed change in percentage of moderate pockets following treatment is due to either the repair of deep pockets, or irreversible iatrogenic insult to shallow pockets, both resulting in an increase in moderate pocket percentage.
Clinically, residual periodontal pockets are important as potential habitants of pathogenic microbiota. Within 6–10 weeks after professional sub-gingival debridement, sub-gingival microbial repopulation with periodontitis associated microflora occurs with return to baseline value [9, 32, 50, 51]. Therefore, the re-evaluation examination was performed at 6–8 weeks following treatment, before repopulation occurs as proposed accordingly by Segelnick and Weinberg [31]. An interval of 6 to 8 weeks after non-surgical debridement is considered as adequate time for tissues to be assessed for signs of inflammation and for changes in probing depth and clinical attachment [31].
Data from multiple longitudinal studies indicate that sites with probing depths of ≥ 6 mm at the re-evaluation phase are at a significantly higher risk to develop additional attachment loss in future, if left untreated [46]. In these sites even when kept free from supragingival deposits, a subgingival microbiota with a large proportion of motile bacteria soon recurred [32]. In shallow and moderate pockets, supra-gingival flora influences the sub-gingival flora [52,53,54]. The sub-optimal plaque control practiced by patients, who were instructed by less experienced operators (DS), may cause later earlier re-establishment of more pathogenic sub-gingival flora. This may have a negative effect on long-term stability of treatment results [15, 55, 56].
Total sub-gingival debridement based on plaque and calculus removal is more difficult in deep than in shallow pockets, i.e., fairly good at probing depths of ≥ 3 mm, failure greater than success at 3–5 mm, and failure significantly dominant at > 5 mm [20, 22, 57]. Since the present study evaluated the operator’s performance, pocket depth data were sub-grouped accordingly: shallow (≥ 3 mm), moderate (4–5 mm), and deep (> 6 mm). Complete calculus removal from a periodontally diseased root surface is rare [58]. According to Buchanan and Robertson [59], following scaling and root planing, 11% of treated pocket area was occupied by residual calculus and 62% of the treated teeth were calculus positive [59]. Also, 3.1% residual calculus per surface area and 57% of all teeth with residual microscopic calculus were detected by Shermann et al. [60]. Residual calculus has been observed more often in deeper than in shallower pockets and molar sites more frequently than nonmolar sites, with little variation between probing depths when calculated as a percentage of sub-gingival area with residual calculus [60]. Less experienced operators are expected to render a less effective debridement [26] than more trained and skilled ones. We can assume that the PR operator in the present study, as a more trained and skilled operator, is more efficient in subgingival scaling and root planing. The significantly greater reduction in total percentage of deep pockets (≥ 6 mm) in the PR group (8%), compared to the DS group (1.5%), reflects advantage of experienced and skilled treatment. The experienced operator can be more effective in using hand instruments, which are more difficult in handling in comparison to the use of ultrasonic scaler and may better combine both instruments during the treatment. As well, experience can account for superiority in overcoming the difficulties in clinically determining the thoroughness of subgingival instrumentation [60]. However, in both treatment groups, improvement in pocket depth was recorded, i.e., increase in percentage of shallow pockets and a decrease in percentage of moderate and deep pockets. This shift is a clinical reflection of the healing process of the dento-gingival area, based on a combination of changes in location of gingival margin, base of gingival pocket, and improved gingival tonus [61]. Therefore, the present study showed that significant gingival healing and clinical improvement can be accomplished in spite of the inferior effectiveness of root planing by the less experienced operator, who would most likely leave more residual calculus spots. This is in accordance to the conclusion of Sherman et al. [44] that in most situations, small amounts of residual calculus may be compatible with clinical improvement of gingival tissue, at least on a short-term basis (3 months observation period). However, since the treatment objectives are to arrest the progression of the disease by non-surgical methods and to minimize the number of sites which demand further intervention (mostly surgical), the improvement per se is not a satisfactory result. Since the more skilled operators improved the periodontal condition of their patients with a two-fold increase in the percentage of shallow pockets and a five-fold decrease in the percentage of deep pockets, as compared to the less experienced operator, the former operator is definitively the one preferred.
In conclusion, while applying mechanical non-surgical therapy, both the experienced and less experienced operators improved the periodontal health of their patients. However, the less experienced operator can predispose the patients to an unstable outcome and to surgical interventions aimed to treat the residual pockets.
References
Ishikawa I, Baehni P (2004) Nonsurgical periodontal therapy-where do we stand now? Periodontology 2000 36:4–14
Wennstrom JL, Tomasi C (2015) Non-surgical therapy Clinical Periodontology and Implant Dentistry, Sixth Edition. Edited by Niklaus P. Lang and Jan Lindhe:. Published 2015 by John Wiley & Sons, Ltd 38 :749–764
Claffey N, Polyzois I, Ziaka P (2004) An overview of nonsurgical and surgical therapy. Periodontology 2000 36:35–44
Cercek JK, Kiger RD, Garrett S, Egelberg J (1983) Relative effects of plaque control and instrumentation on the clinical parameters of human periodontal disease. J Clin Periodontol 10:46–56
Cobb CM (1996) Non-surgical pocket therapy. Ann Periodontol 1:443–490
Haffajee AD, Cugini MA, Dibart S, Smith C, Kent RL Jr, Socransky SS (1997) The effect of SRP on the clinical and microbiological parameters of periodontal diseases. J Clin Periodontol 24:324–334
Suvan JE (2005) Effectiveness of mechanical nonsurgical pocket therapy. Periodontology 2000 37:48–71
Adriaens PA, Adriaens LM (2004) Effects of nonsurgical periodontal therapy on hard and soft tissues. Periodontology 2000 36:121–145
Mousques T, Listgarten MA, Philips RW (1980) Effect of scaling and root planing on the composition of the human subgingival microbial flora. J Periodontal Res 15:144–151
Loos B, Claffey N, Crigger M (1988) Effects of oral hygiene measurers on clinical and microbiological parameters of periodontal disease. J Clin Periodontol 18:211–216
Umeda M, TakeuchiY NK, Huang Y, Koshy G, Ishikawa I (2004) Effect of nonsurgical periodontal therapy on the microbiota. Periodontology 2000 36:98–120
Haffajee AD, Teles RP, Socransky SS (2006) The effect of periodontal therapy on the composition of the subgingival microbiota. Periodontology 2000 42:219–258
Cobb CM (2002) Clinical significance of non-surgical periodontal therapy: an evidence-based perspective of scaling and root planing. J Clin Periodontol 29(suppl 2):6–16
van der Weijden GA, Timmerman MF (2002) A systematic review on the clinical efficacy of subgingival debridement in the treatment of chronic periodontitis. J Clin Periodontol 29(suppl 3):55–71
Lindhe J, Nyman S (1984) Long-term maintenance of patients treated for advanced periodontal disease. J Clin Periodontol 11:504–511
Kornman KS (1986) The role of supragingival plaque in the prevention and treatment of periodontal disease. A review of current concepts. J Periodontal Res 21:5–22
Jin L, Wong KY, Leung WK, Corbet EF (2000) Comparison of treatment response patterns following scaling and root planing in smokers and non-smokers with untreated adult periodontitis. Journal of Clin Dent 11:35–41
Rabbani GM, Ash MM, Caffesse RG (1981) The effectiveness of subgingival scaling and root planing in calculus removal. J Periodontol 52:119–123
Waerhaug J (1978a) Healing of dentoepithelial junction following subgingival plaque control. I. As observed in human biopsy material. J Periodontol 49:1–8
Waerhaug J (1978b) Healing of dentoepithelial junction following subgingival plaque control. II. As observed on extracted teeth. J Periodontol 49:119–134
Stambaugh RV, Dragoo M, Smith DM, Carasali L (1981) The limits of subgingival scaling. Int J Periodontics and Restorative Dent 1:30–41
Oda S, Nitta H, Setoguchi T, Izumi Y, Ishikawa I (2004) Current concepts and advances in manual and power-driven instrumentation. Periodontology 2000 36:45–58
Kocher T, Ruehling A, Momsen H, Plagmann HC (1997) Effectiveness of subgingival instrumentation with power-driven instruments in the hands of experienced and inexperienced operators. A study on manikins. J Clin Periodontol 24:498–504
Graetz C, Schwendicke F, Plaumann A, Rauschenbach S, Springer C, Kahl M, Sȁlzer S, Dörfer CE (2017) Subgingival instrumentation to remove simulated plaque in vitro: influence of operators’ experience and type of instrument. Clin Oral Invest 19:987–995
Eaton KA, Kieser JB, Davis RM (1985) The removal of root surface deposits. J Clin Periodontol 12:141–152
Brayer WK, Mellonig JT, Dunlap RM, Marinak KW, Carson RE (1989) Scaling and root planing effectiveness: the effect of root surface access and operator experience. J Periodontol 60:67–72
Fleischer HC, Mellonig JT, Brayer WK, Gray JL, Barnett JD (1989) Scaling and root planing efficacy in multirooted teeth. J Periodontol 60:402–409
Badersten A, Nilvéus R, Egelberg J (1985) Effect of non-surgical periodontal therapy (IV). Operator variability. J Clin Periodontol 12:190–200
O'Leary TJ (1972) The plaque control record. J Periodontol 43:38–40
Mühlemann HR, Son S (1971) Gingival sulcus bleeding—a leading symptom in initial gingivitis. Helvetica Odontologica Acta 15:107–113
Segelnick SL, Weinberg MA (2006) Reevaluation of initial therapy: when is the appropriate time? J Periodontol 77:1598–1601
Magnusson I, Lindhe J, Yoneyama T, Liljenberg B (1984) Recolonization of a subgingival microbiota following scaling in deep pockets. J Clin Periodontol 11:193–207
Axelsson P, Nystrom B, Lindhe J (2004) The long-term effect of a plaque control program on tooth mortality, caries and periodontal disease in adults. Results after 30 years of maintenance. J Clin Periodontol 31:749–757
Axelsson P, Lindhe J (1981a) Effect of controlled oral hygiene procedures on caries and periodontal disease in adults. J Clin Periodontol 8:239–248
Axelsson P, Lindhe J (1981b) The significance of maintenance care in the treatment of periodontal disease. J Clin Periodontol 8:281–294
Bakdash B (1994) Oral hygiene compliance as risk factor in periodontitis. J Periodontol 65(suppl 5):539–544
König J, Plagmann HC, Langenfeld N, Kocher T (2001) Retrospective comparison of clinical variables between compliant and non-compliant patients. J Clin Periodontol 28:227–232
Wilson TG (1996) Compliance and its role in periodontal therapy. Periodontol 12:16–2338
Wilson TG (1998) How patient compliance to suggested oral hygiene and maintenance affect periodontal therapy. Dent Clin N Am 42:389–403
Heasman P, Jacobs DJ, Chapple I (1989) An evaluation of the effectiveness and patient compliance with plaque control methods in the prevention of periodontal disease. Clin Prev Dent 11:24–28
Meitner SW, Zander HA, Iked HP, Polson AP (1979) Identification of inflamed gingival surfaces. J Clin Periodontol 6:93–97
Polson AP, Caton JG (1985) Current diagnosis of bleeding in the diagnosis of periodontal diseases. J Periodontol 56(11 Suppl):1–3
Lang NP, Adler R, Joss A, Nyman S (1990) Absence of bleeding on probing. An indicator of periodontal stability. J Clin Periodontol 17:714–721
Sherman PR, Hutchens LH, Jewson LG (1990b) The effectiveness of subgingival scaling and root planing. II. Clinical responses related to residual calculus. J Periodontol 61(1):9–15
Lang NP, Joss A, Tonetti MS (1996) Monitoring disease during supportive periodontal treatment by bleeding on probing. Periodontology 2000 12:44–55
Armitage GC (1996) Manual periodontal probing in supportive periodontal treatment. Periodontology 2000 12:33–39
Lindhe J, Nyman S, Karring T (1982a) Scaling and root planing in shallow pockets. J Clin Periodontol 9:415–418
Lindhe J, Socransky SS, Nymann S, Haffajee A, Westfelt E (1982b) “Critical probing depths” in periodontal therapy. J Clin Periodontol 9:115–128
Hallmon WW, Rees TD (2003) Local anti-infective therapy: mechanical and physical approaches. A systematic review. Ann Periodontol 8:99–114
Lavanchy D, Bickel M, Baehni P (1987) The effect of plaque control after scaling and root planing on the subgingival microflora in human periodontitis. J Clin Periodontol 14:295–299
Sbordone L, Ramaglia L, Guletta E, Iacono V (1990) Recolonization of the subgingival microflora after scaling and root planing in human periodontitis. J Periodontol 61:579–584
Dahlén G, Lindhe J, Sato K, Hanamura H, Okamoto H (1992) The effect of supragingival plaque control on the subgingival microbiota in subjects with periodontal disease. J Clin Periodontol 19:802–809
McNabb H, Mombelli A, Lang NP (1992) Supragingival cleaning three times a week: the microbiological effects in moderately deep pockets. J Clin Periodontol 19:348–356
Hellström MK, Ramberg P, Krok L, Lindhe J (1996) The effect of supragingival plaque control on the subgingival microflora in human periodontitis. J Clin Periodontol 23:934–940
Ramfjord SP, Morrison EC, Burgett FG, Nissle RR, Shick RA, Zann GJ, Knowles JW (1982) Oral hygiene and maintenance of periodontal support. J Periodontol 53:26–30
Ramfjord SP (1987) Maintenance care for treated periodontitis patients. J Clin Periodontol 13:433–437
Caffesse RG, Sweeney PL, Smith BA (1986) Scaling and root planing with and without periodontal flap surgery. J Clin Periodontol 13:205–210
Kepic TJ, O’Leary TJ, Kafrawy AH (1990) Total calculus removal: an attainable objective. J Periodontol 61:16–20
Buchanan SA, Robertson PA (1987) Calculus removal by scaling/root planing with and without surgical access. J Periodontol 58:159–163
Sherman PR, Hutchens LH, Jewson LG, Moriarty JM, Greco GW, McFall WT (1990a) The effectiveness of subgingival scaling and root planing. I. Clinical detection of residual calculus. J Periodontol 61:3–8
Greenstein G (1992) Periodontal response to mechanical non-surgical therapy: a review. J Periodontol 63:118–130
Acknowledgements
The authors are grateful to Dr. Ronit Bar-Ness Greenstein (The Maurice and Gabriela Goldschleger School of Dental Medicine, Tel Aviv University, Tel Aviv, Israel) for helpful discussion and significant help in writing the manuscript.
Funding
The work was supported by the Department of Periodontology and Implant Dentistry, The Maurice and Gabriela Goldschleger School of Dental Medicine, Tel Aviv University, Tel Aviv, Israel.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
Author A: Avital Kozlovsky declares that she has no conflict of interests.
Author B: Alex Rapaport declares that he has no conflict of interests.
Author C: Zvi Artzi declares that he has no conflict of interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional ethical committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study, informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Kozlovsky, A., Rapaport, A. & Artzi, Z. Influence of operator skill level on the clinical outcome of non-surgical periodontal treatment: a retrospective study. Clin Oral Invest 22, 2927–2932 (2018). https://doi.org/10.1007/s00784-018-2380-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-018-2380-7