Abstract
Objectives
Tori are frequent paucisymptomatic bony outgrowths of the oral cavity in three locations: torus palatinus (TP), mandibularis (TM), and maxillaris (TMax). Their usually described histological characteristics are unspecific: normal cortical bone with more or less trabecular bone. The aim of this study was to describe tori’s specific morphological and histomorphometric characteristics.
Materials and methods
Histological characteristics in a series of 18 tori collected after surgical removal were analyzed. Microcomputed tomography provided a 3D analysis. Mineral apposition rate (MAR) was measured after double tetracycline labeling. Osteoid tissue was identified by Goldner’s trichrome and osteoclasts by the tartrate resistant acid phosphatase identification in undecalcified sections. Iron and aluminum were detected by histochemical staining methods. Osteoid thickness and MAR were determined at the outer surface of the torus and in the Haversian canals.
Results
Tori appeared made of lamellar Haversian bone in 16/18 cases. Osteoid thickness did not differ between the outer surface and within the canals. An asymmetric bone remodeling was observed in the Haversian canals of 15 tori: osteoid seams were deposited on the side close to the free torus surface, and Howship’s lacunae with numerous osteoclasts were observed on the opposite side. A high MAR was found at the surface of the tori and within the canals. There was no iron or aluminum deposit.
Conclusions
Tori may be characterized by a specific asymmetric bone remodeling which seems to determine their shape.
Clinical relevance
This finding could constitute a specific histological feature allowing to differentiate tori from exostoses.

Graphical abstract
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tori are frequent and benign bony outgrowths of the oral cavity. They are named after the Latin torus that means “lump”. They are covered with a thin and poorly vascularized mucosa [1, 2]. They present a slow and progressive growth that may stop spontaneously [1]. A torus palatinus (TP) is usually located at the palate, along the longitudinal ridge of the hard palate on either side of the median raphe of the palatine bone. A torus mandibularis (TM) is usually located at the mandible (on the lingual side of the horizontal branch above the mylohyoid line at the level of the premolar and/or canine area) [1]. A less common form is torus maxillaris (TMax) which is located at the maxilla (on the palatal or vestibular side of the alveolar process of the maxilla) [2]. According to the anatomical location (TP, TM, or TMax), the clinical and epidemiological characteristics are not strictly alike [2]. They are often bilateral but may be unilateral [3]. The general prevalence is about 10 to 30% and varies according to ethnic groups, age, and gender [1, 4, 5]. Tori are more frequent in some ethnic groups (Japanese, Caucasian, Norwegian, Eskimos) [1, 3, 6]. The etiology remains unknown and could be multifactorial. A genetic origin is the most widely accepted theory today, but an autosomal dominant inheritance explains only 30% of the cases [1, 2]. Environmental factors seem to play a role in the incidence of tori. A mechanical origin due to occlusal stress is advocated to explain the occurrence of TM [1, 3, 6]. An interplay between genetic and environmental factors cannot be excluded [7]. Tori are frequently asymptomatic, and their surgical removal is indicated in some cases, mainly, before dental prosthetic rehabilitation, as a source of autogenous bone graft in implant surgery or for patients’ desire (esthetic reasons or cancerophobia) [1]. The usually described histological characteristic is not specific: tori are composed of normal cortical bone with more or less trabecular bone according to their size [1, 7, 8]. The aim of the present study was to find tori’s specific characteristics by describing morphological and histological bone characteristics in a series of human tori. Microcomputed tomography (microCT), histology, and histochemical were used to characterize the morphological aspect of the tori.
Participants and methods
Participants
Tori were collected in three maxillo-facial surgery departments in Angers, Paris, and Tours (France). All patients undergoing surgical removal of a torus between 2011 and 2015 were included. All participants had given their informed consent before participating to the study. Clinical characteristics are summarized in Table 1. Ten participants, 2 males, and 8 females were included. All participants were Caucasians. The average age was 51.8 ± 5.11 years. Tumors were removed in one piece and fixed in formalin until use. They were then sent to the bone histopathology unit of Angers University Hospital.
A double tetracycline labeling technique was used to measure mineral apposition rate (MAR) by osteoblasts [9]. Demethyl chlortetracycline (Alkonatrem®, Laboratoires Genopharm, Saint-Thibault-des-Vignes, France) was given at the dose of 600 mg, twice a day according to a strict schedule: 2 days on, 10 days off, 4 days on. Surgical removal of the torus was performed between 2 and 7 days after the end of the second label (in order to avoid unspecific label on the eroded surfaces). Samples were fixed immediately in formalin and stored in a fridge until analysis.
This experimental protocol was approved by the local ethical committee of Angers University Hospital and was done in accordance with the institutional guidelines of the French Ethical Committee (protocol number 2016-31) and with the 1964 Helsinki declaration and its later amendments.
Microcomputed tomography
Samples were analyzed by microCT prior to histological embedding. MicroCT allowing a 3D evaluation of these tumors was performed using a Skyscan 1172 X-ray computerized microtomograph (Bruker microCT, Kontich, Belgium) equipped with an X-ray tube working at 70 kV/100 μA. Bone samples were placed in plastic tubes filled with water to prevent desiccation. The tube was fixed on a brass stub with plasticine. Analysis was done with a pixel size corresponding to 8.29 μm; the rotation step was fixed at 0.25° with a 0.5-mm aluminum filter. For each sample, a stack of 2D sections was obtained and reconstructed using NRecon software (Bruker microCT, Kontich, Belgium) and analyzed with CTAn software release 1.13.11.0 (Bruker microCT, Kontich, Belgium). The 3D reconstruction of the specimens was obtained with the ANT and CTVol softwares (Bruker microCT, Kontich, Belgium). The programs allowed reconstruction from the stacks of 2D sections by either surface or volume rendering.
Histology
The size of the tori was determined according to Woo’s classification [8, 10]. Bone samples were embedded undecalcified in poly(methyl methacrylate). Sections (7 μm in thickness) were cut dry on a heavy-duty microtome equipped with 50° tungsten carbide knives (Leica Polycut S, Rueil-Malmaison, France). Sections were stained by Goldner’s trichrome for the identification of osteoid. Histochemical identification of osteoclasts (bone resorbing cells) was done by the tartrate resistant acid phosphatase (TRAcP) method [11]. The presence of iron (Fe) and aluminum (Al) in tori was searched by histochemical methods. The Perls’ Prussian blue and solochrome azurine staining methods were used for the identification of Fe3+ and Al3+, respectively [12]. These histochemical reactions were done in cleaned glass vials, and the technicians never used metallic forceps during the staining to avoid contamination. Observations were performed at the cortical (outer) surface of each torus (Ct.) and at the surface of the Haversian canal (Ca.). The osteoid seam thickness was determined at the outer surface of the torus (Ct.O.Th) and at the surface of the Haversian canal (Ca.O.Th). The MARs were determined on unstained 10 μm thick sections, at the outer surface of the torus (Ct.MAR), and at the surface of the Haversian canal (Ca.MAR). It was determined as the average value of the distance between all double labels (four measurements at equidistant locations per label) divided by the number of days between the given doses of tetracycline. All histomorphometric measurements and the nomenclature used follow the ASBMR (American Society for Bone and Mineral Research) recommendations [13].
Statistical analysis
Statistical analysis was performed using the Systat statistical software release 13.1 (Systat Software Inc., San José, CA). All data were expressed as mean ± standard error of the mean (SEM). Differences among groups were analyzed by a non-parametric ANOVA (Kruskall–Wallis) and between groups by the Mann and Whitney’s U test. Means were compared using a paired t test. Differences were considered significant when p < 0.05.
Results
Clinical characteristics
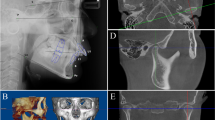
All participants underwent surgical removal of the tori before prosthetic rehabilitation or for esthetical reasons (Table 1). Eighteen tori from 10 participants were analyzed. They were all localized on the internal (lingual) side of the horizontal branch of the mandible, above the mylohyoid line, and at the level of the canine and/or the first premolar except two that were localized at vestibular side of the maxilla in one participant. They all presented a convex shape in the oral cavity (Fig. 1). Five tori presented an elongated shape, and 13 tori presented a round shape. Tori were bilateral in five participants and were situated on the same side in three participants. Tori were unique and unilateral in two participants. No TP were enrolled in the present study.
Microcomputed tomography
The general globular shape of the tori was clearly identified with a smooth free surface, and the implantation surface was well differentiated (Fig. 2a). The software possibility to threshold the internal porosity inside the torus revealed the presence of numerous Haversian canals. The 3D orientation of the canals was often in random directions in contrast to the canalar orientation in the normal mandibular cortice which runs in parallel (Fig. 2b). This aspect can be well identified in the supplementary video.
Histological analysis
According to Woo’s classification, there were 13 small and 5 medium tori. The average length of the tori was 9.8 ± 1.54 mm, and the average elevation was 3.66 ± 0.5 mm. Under polarization microscopy, tori appeared made of lamellar bone in 16/18 cases and the structure units were true osteons with a central Haversian canal (Fig. 3a). In 2/18 tori, the bone texture was a mix of woven bone packed with a small amount of lamellar bone. Histological analysis revealed the presence of osteoid seams in two different locations: at the external free surface of the torus and inside the Haversian canals in 17/18 cases. Osteoid thickness was similar at the surface of the tori and inside the canals (Ct.O.Th: 12.0 ± 1.3 μm; Ca.O.Th: 13.6 ± 0.7 μm; p = 0.093) (Table 2). The most intriguing aspect was the asymmetric disposition of the osteoid seams which were laid on the canal surface closest to the free torus surface in 15/18 tori of the study (Fig. 3b). The opposite surface of the canal was frequently occupied by Howship’s lacunae (Fig. 3b). TRAcP-stained sections evidenced numerous true osteoclasts in this location in 11/18 tori (Fig. 3c). This corresponds to an active and asymmetric bone remodeling observed in almost every tori of the study.
Histological analysis. a Torus section seen in polarized microscopy showing normal cortical bone made of lamellar bone with true osteons and a central Haversian canal. b Torus section stained by Goldner’s trichrome showing the presence of osteoid seams in two different locations: at the external free surface of the torus (green arrow) and inside the Haversian canals (black arrows). Note the asymmetric disposition of the osteoid seams which are laid on the canal surface closest to the free torus surface. The opposite surface of the canal is occupied by Howship’s lacunae. c TRAcP-stained section showing asymmetric disposition of osteoclasts (arrow) which are laid on the canal surface furthest to the free torus surface. d Torus section showing double tetracycline labeling in the same locations as osteoid seams: at the external free surface of the torus (white arrow) and on the Haversian canals surface closest to the free torus surface (green arrow)
In the six participants having received a double tetracycline labeling, the mineralization rate was not statistically different at the surface of the tori and inside the canals (Ct.MAR: 0.66 ± 0.12 μm/day; Ca.MAR: 0.92 ± 0.09 μm/day; p = 0.121) (Fig. 3d). The Ca.MAR determined here was higher (p = 0.0001) than the normal MAR (0.72 ± 0.12 μm/day) [14]. There was no difference between Ct.MAR and normal MAR (p = 0.2289) (Table 2). It attests high mineralization rates in tori of the present study.
Fe3+ and Al3+ were not identified in the bone matrix of any torus of the present study.
Discussion
In the literature, the most frequent indication for torus removal is a prosthetic treatment or an interference with dental prosthesis; it was the same in the present study [1, 15]. Tori are also frequently removed as a source of autogenous bone graft in implant surgery [1, 15–19]. Other causes of excision are disturbances of phonation, limitation of masticatory mechanics, sensitivity due to a thin mucosa layer, inflammation, ulcer of traumatic origin, retention of food remains, and patients’ desire (esthetic reasons or cancerophobia) [1]. Other possible complications due to the presence of tori are submandibular calculi, bisphosphonate-related osteonecrosis, osteitis, osteomyelitis, and intubation difficulties [3, 20–26]. However, tori remain frequently asymptomatic, and their removal is rarely indicated [1, 27]. The indication for a surgical removal of tori must be carefully established, since complications may occur: infections, fractures, or hemorrhages. Specific complications may also occur: neighboring teeth devitalization, palatine or lingual nerves injuries, and salivary ducts injuries [1, 28]. Surgery is usually performed under local anesthesia, and a general anesthesia is frequently required for TP excision [2]. The sub-periosteal detachment must provide a large operating field. The lesion can be removed in one piece or not, using osteotomes, burrs, and/or high speed turbines [1].
The overall prevalence of tori is variable and can reach 10 to 30% in some papers; it varies according to ethnic groups and gender [1, 2, 4–6, 29–41]. Tori are more frequent in some ethnic groups (Japanese, Caucasian, Norwegian, Indian, and Eskimo) [1–3, 6]. The prevalence also increases with age [2, 6]. TP seem to be more often present in females and TM in males [1, 4]. According to the anatomic location, the overall prevalence is about 20% for TP, 17% for TM, and 6% for TMax in the general population [2]. They are frequently bilateral in 80% of the cases [2]. TMax localized on the palatal side are sometimes classified as TP by some authors [2].
The etiology remains unknown and could be multifactorial. An embryological theory has been proposed to explain the origin of TM with the existence of an alteration at the protruding medial lamina and the bending Meckel’s cartilage formed during the development of the mandible [42]. A genetic origin, with autosomal dominant inheritance, is the most widely accepted theory today for TM, TP, and TMax [1–3]. However, a strictly genetic inheritance is found only in 30% of the cases [1]. Furthermore, a link between the occurrence of tori and genetic bone diseases has been shown [43]. Mutations in the low-density lipoprotein receptor-related protein 5 (LRP5) gene can result in osteosclerosis and may lead to a thickened or an elongated mandible with the occurrence of tori [44, 45]. Tori are also a characteristic of the Gardner’s syndrome, an autosomal dominant disease characterized by the development of gastrointestinal polyps and malignant transformation [46, 47].
On the other hand, mechanical factors related to the occlusal stress during mastication are advocated by many authors for TM [1–3, 6]. The occlusal force was found significantly higher in patients with TM by using a pressure sensitive sheet [6]. A significant correlation between the incidence of tori and the presence of abraded teeth due to bruxism has also been shown [7, 40]. In an animal model with paralysis of the masticatory muscles (M. masseter and M. temporalis) by the Botulinum toxin, the occurrence of a hypertrophic bone metaplasia at the enthesis of M. Digastricus was found [48]. It is well-known that an increased muscle activity can stimulate bone remodeling and increases bone apposition [49]. This fact supports the etiological hypothesis of mechanical causes related to a disequilibrium of occlusal forces due to an increased muscle activity. However, since tori have no topographical relation with muscle attachments, this pathological sequence cannot be extrapolated to human tori. So, an interplay between genetic and environmental factors cannot be excluded [7]. The cause of tori can therefore be explained by the conjunction of different factors: a torus is primarily a genetic trait, and environmental factors such as mechanical stress could be necessary for its development [4].
Few articles in the literature describe the histology of tori, and they often report histological organization similar to normal bone [1]. Tori are usually described made of lamellar cortical bone with the central presence of a cancellous network, sometimes made of woven bone, only when a large size is attained [1, 7, 8]. The presence of “lacunae” (Haversian canals), normal osteocytes, and scattered areas of connective tissue containing dilated blood vessels is also reported [2, 7]. The nature, texture, and structure of the bone constituting the tori correspond to a bone quality encountered in normal bone cell activity [50]. This explains that good clinical results are observed when tori are used for bone grafting [1, 15–19]. In the present study, an asymmetric active bone remodeling is reported for the first time. It leads to a unidirectional bone growth toward the oral cavity that explains the usual convex shape of tori and an escape to the mechanical stimuli related to occlusal forces. The use of undecalcified bone sections allowed the identification of osteoid tissue together with a histodynamic analysis after tetracycline labeling. These findings cannot be obtained using conventional histopathologic methods after decalcification and paraffin embedding. It is also the first time that microCT is used to characterize the external and internal microarchitecture of these tumors. This technique offers a unique possibility to evidence the 3D network of Haversian canals distribution in cortical bone [51]. This facility was used here to evidence the complex 3D distribution of Haversian canals in the tori.
The osteoid seam thicknesses determined in the present study were found normal (<15 μm) indicating the absence of osteomalacia. The Ca.MAR determined here was higher than normal MAR. This attests a high osteoblastic activity at the outer surface of the Haversian canals. The presence of woven bone reflects an active remodeling in 2/18 tori of the study. This might concern tori at an early stage before being completely remodeled in lamellar bone. Unfortunately, these two participants did not receive the double tetracycline labeling.
Tori are not similar to bone exostosis developing at the metaphysis of long bones in children and teenagers. Exostosis is a frequent benign cartilage-capped bony tumor. They may occur as solitary tumors (due to a possible dysregulation of osteoprogenitor cells) or as multiple tumors in the case of an autosomal genetic disorder (the multiple hereditary exostoses-MHE). A study found the pathologic presence of Al in exostosis in two thirds of the patients and the presence of Fe in half of the patients [12, 52]. In the present study, Fe and Al were never observed in the tori. This may seem surprising since tori develop inside the oral cavity, and ingesta are known to be a major source for Al to enter in the body [12].
Conclusion
Tori are a specific entity that develops on bones built by intramembranous ossification, and their shape seems to be determined by a specific asymmetric bone remodeling. This finding constitutes a specific histological feature allowing pathologists to differentiate tori from exostoses.
References
Garcia-Garcia AS, Martinez-Gonzalez JM, Gomez-Font R, Soto-Rivadeneira A, Oviedo-Roldan L (2010) Current status of the torus palatinus and torus mandibularis. Med Oral Patol Oral Cir Bucal 15:e353–e360
Loukas M, Hulsberg P, Tubbs RS, Kapos T, Wartmann CT, Shaffer K, Moxham BJ (2013) The tori of the mouth and ear: a review. Clin Anat 26:953–960
Chossegros C, Foletti JM, Graillon N, Guyot L (2016) Oral torus or tori, why? Rev Stomatol Chir Maxillofac Chir Oral 117:59–61
Ihunwo AO, Phukubye P (2006) The frequency and anatomical features of torus mandibularis in a Black South African population. Homo 57:253–262
Yoshinaka M, Ikebe K, Furuya-Yoshinaka M, Hazeyama T, Maeda Y (2010) Prevalence of torus palatinus among a group of Japanese elderly. J Oral Rehabil 37:848–853
Yoshinaka M, Ikebe K, Furuya-Yoshinaka M, Maeda Y (2014) Prevalence of torus mandibularis among a group of elderly Japanese and its relationship with occlusal force. Gerodontology 31:117–122
Antoniades DZ, Belazi M, Papanayiotou P (1998) Concurrence of torus palatinus with palatal and buccal exostoses: case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 85:552–557
Seah YH (1995) Torus palatinus and torus mandibularis: a review of the literature. Aust Dent J 40:318–321
Melsen F, Mosekilde L (1978) Tetracycline double-labeling of iliac trabecular bone in 41 normal adults. Calcif Tissue Res 26:99–102
Woo JK (1950) Torus palatinus. Am J Phys Anthropol 8:81–111
Chappard D (2014) Technical aspects: how do we best prepare bone samples for proper histological analysis? In Heymann D (ed) bone cancer: progression and therapeutic approaches, 2nd edn. Acad. Press; Elsevier Inc., London, pp 111–120
Chappard D, Bizot P, Mabilleau G, Hubert L (2016) Aluminum and bone: review of new clinical circumstances associated with Al(3+) deposition in the calcified matrix of bone. Morphologie 100:95–105
Dempster DW, Compston JE, Drezner MK, Glorieux FH, Kanis JA, Malluche H, Meunier PJ, Ott SM, Recker RR, Parfitt AM (2013) Standardized nomenclature, symbols, and units for bone histomorphometry: a 2012 update of the report of the ASBMR Histomorphometry Nomenclature Committee. J Bone Miner Res 28:2–17
Meunier PJ, Chavassieux P (1985) L'histomorphométrie moyen d'évaluation de la masse osseuse. Rev Rhum Malad Osteo-Art 52:669–673
Ephros H, Klein R, Sallustio A (2015) Preprosthetic surgery. Oral Maxillofac Surg Clin North Am 27:459–472
Wang CJ, Huang CB, Grossman SH, Pourati J (2016) Vertical ridge augmentation with mandibular lingual torus block graft : a case letter. J Oral Implantol 42:369–372
Moraes EF Jr, Damante CA, Araujo SR (2010) Torus palatinus: a graft option for alveolar ridge reconstruction. Int J Periodont Rest Dent 30:283–289
Hassan KS, Al-Agal A, Abdel-Hady AI, Swelam WM, Elgazzar RF (2015) Mandibular tori as bone grafts: an alternative treatment for periodontal osseous defects-clinical, radiographic and histologic morphology evaluation. J Contemp Dent Pract 16:192–200
Santhanakrishnan M, Rangarao S (2014) Mandibular Tori: a source of autogenous bone graft. J Ind Soc Periodontol 18:767–771
Kaneko K, Takahashi H (2014) Bisphosphonate-related osteonecrosis of the palatal torus. ORL J Otorhinolaryngol Relat Spec 76:353–356
Godinho M, Barbosa F, Andrade F, Cuzzi T, Ramos ESM (2013) Torus palatinus osteonecrosis related to bisphosphonate: a case report. Case Rep Dermatol 5:120–125
Durrani MA, Barwise JA (2000) Difficult endotracheal intubation associated with torus mandibularis. Anesth Analg 90:757–759
Manganaro AM, Faulk-Eggleston J, Schanzer RB, Dagostino M (1997) Osteitis in a torus mandibularis secondary to trauma. Gen Dent 45:74–77
Pasqual HN, Pasqual RJ (1968) Osteomyelitis of torus palatinus: report of a case. Oral Surg Oral Med Oral Pathol 25:532–533
Smith HW (1963) Osteitis of the torus palatinus with sequestration. Review of the literature and report of two cases. Arch Otolaryngol 78:811–815
Best SR, Kobler JB, Friedman AD, Barbu AM, Zeitels SM, Burns JA (2014) Effect of mandibular tori on glottic exposure during simulated suspension microlaryngoscopy. Ann Otol Rhinol Laryngol 123:188–194
MacInnis EL, Hardie J, Baig M, al-Sanea RA (1998) Gigantiform torus palatinus: review of the literature and report of a case. Int Dent J 48:40–43
Kun-Darbois JD, Pare A, Chemli H, Daher G, Breheret R (2014) Cervical crepitus after dental extraction. Rev Stomatol Chir Maxillofac Chir Orale 115:e17–e18
Romanos GE, Sarmiento HL, Yunker M, Malmstrom H (2013) Prevalence of torus mandibularis in Rochester, New York, region. N Y State Dent J 79:25–27
Sathya K, Kanneppady SK, Arishiya T (2012) Prevalence and clinical characteristics of oral tori among outpatients in Northern Malaysia. J Oral Biol Craniofac Res 2:15–19
Choi Y, Park H, Lee JS, Park JC, Kim CS, Choi SH, Cho KS, Chai JK, Jung UW (2012) Prevalence and anatomic topography of mandibular tori: computed tomographic analysis. J Oral Maxillofac Surg 70:1286–1291
Hiremath VK, Husein A, Mishra N (2011) Prevalence of torus palatinus and torus mandibularis among Malay population. J Int Soc Prev Community Dent 1:60–64
Sisman Y, Ertas ET, Gokce C, Akgunlu F (2008) Prevalence of torus palatinus in cappadocia region population of Turkey. Eur J Dent 2:269–275
Jainkittivong A, Apinhasmit W, Swasdison S (2007) Prevalence and clinical characteristics of oral tori in 1,520 Chulalongkorn University Dental School patients. Surg Radiol Anat 29:125–131
Yildiz E, Deniz M, Ceyhan O (2005) Prevalence of torus palatinus in Turkish schoolchildren. Surg Radiol Anat 27:368–371
Bruce I, Ndanu TA, Addo ME (2004) Epidemiological aspects of oral tori in a Ghanaian community. Int Dent J 54:78–82
Al-Bayaty HF, Murti PR, Matthews R, Gupta PC (2001) An epidemiological study of tori among 667 dental outpatients in Trinidad & Tobago, West Indies. Int Dent J 51:300–304
Gorsky M, Raviv M, Kfir E, Moskona D (1996) Prevalence of torus palatinus in a population of young and adult Israelis. Arch Oral Biol 41:623–625
Shah DS, Sanghavi SJ, Chawda JD, Shah RM (1992) Prevalence of torus palatinus and torus mandibularis in 1000 patients. Ind J Dent Res 3:107–110
Reichart PA, Neuhaus F, Sookasem M (1988) Prevalence of torus palatinus and torus mandibularis in Germans and Thai. Community Dent Oral Epidemiol 16:61–64
Ohno N, Sakai T, Mizutani T (1988) Prevalence of torus palatinus and torus mandibularis in five Asian populations. Aichi Gakuin Dent Sci 1:1–8
Rodriguez-Vazquez JF, Sakiyama K, Verdugo-Lopez S, Amano O, Murakami G, Abe S (2013) Origin of the torus mandibularis: an embryological hypothesis. Clin Anat 26:944–952
Hosoi T, Yoda T, Yamaguchi M, Amano H, Orimo H (2003) Elderly women with oral exostoses had higher bone mineral density. J Bone Miner Metab 21:120–122
Wang C, Zhang BH, Zhang H et al (2013) The A242T mutation in the low-density lipoprotein receptor-related protein 5 gene in one Chinese family with osteosclerosis. Intern Med 52:187–192
Boyden LM, Mao J, Belsky J, Mitzner L, Farhi A, Mitnick MA, Wu D, Insogna K, Lifton RP (2002) High bone density due to a mutation in LDL-receptor-related protein 5. N Engl J Med 346:1513–1521
Agrawal D, Newaskar V, Shrivastava S, Nayak PA (2014) External manifestations of Gardner’s syndrome as the presenting clinical entity. BMJ Case Rep DOI. doi:10.1136/bcr-2013-200293
Bilkay U, Erdem O, Ozek C, Helvaci E, Kilic K, Ertan Y, Gurler T (2004) Benign osteoma with Gardner syndrome: review of the literature and report of a case. J Craniofac Surg 15:506–509
Kun-Darbois JD, Libouban H, Chappard D (2015) Botulinum toxin in masticatory muscles of the adult rat induces bone loss at the condyle and alveolar regions of the mandible associated with a bone proliferation at a muscle enthesis. Bone 77:75–82
Sugiyama T, Meakin LB, Browne WJ, Galea GL, Price JS, Lanyon LE (2012) Bones’ adaptive response to mechanical loading is essentially linear between the low strains associated with disuse and the high strains associated with the lamellar/woven bone transition. J Bone Miner Res 27:1784–1793
Chappard D, Baslé MF, Legrand E, Audran M (2011) New laboratory tools in the assessment of bone quality. Osteoporos Int 22:2225–2240
Cooper D, Turinsky A, Sensen C, Hallgrimsson B (2003) Quantitative 3D analysis of the canal network in cortical bone by micro-computed tomography. Anat Rec B 274:169–179
Chappard D, Mabilleau G, Moukoko D, Henric N, Steiger V, Le Nay P, Frin JM, De Bodman C (2015) Aluminum and iron can be deposited in the calcified matrix of bone exostoses. J Inorg Biochem 152:174–179
Acknowledgments
Authors are greatly indebted to all surgeons who addressed bone samples to the laboratory and especially Pr. D. Goga and Dr. S. Badja. Authors also thank Mrs. Nadine Gaborit for her skillful assistance with microCT and histotechnology.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
No financial disclosure.
Ethical approval
All procedures performed in the present study were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments. This experimental protocol was approved by the local ethical committee of Angers University Hospital (France) and was done in accordance with the institutional guidelines of the French Ethical Committee (protocol number 2016-31).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Financial disclosure
None.
Electronic supplementary material
Supplementary material
Video of a TM imaged by MicroCT. External view and internal porosity due to Haversian canals (in green) (MP4 5702 kb)
Rights and permissions
About this article
Cite this article
Kün-Darbois, JD., Guillaume, B. & Chappard, D. Asymmetric bone remodeling in mandibular and maxillary tori. Clin Oral Invest 21, 2781–2788 (2017). https://doi.org/10.1007/s00784-017-2080-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-017-2080-8