Abstract
Objective
The aim of this retrospective university-based study has been to evaluate the longevity and factors associated with failures of adhesive restorations performed in deep carious lesions of permanent molars after complete (CCR) and selective caries removal (SCR).
Materials and methods
The sample was composed of composite resin and resin-modified glass ionomer cement (RMGIC) restorations placed in permanent molars of children attending a university dental service who were followed up for up to 36 months. Information collected retrospectively from clinical records was used for analyzing data. The following factors were investigated: gender, caries experience, visible plaque and gingival bleeding indexes, operator’s experiences, number of restored surfaces, and type of capping and restorative materials. The Kaplan-Meier survival test was used to analyze the longevity of the restorations. Multivariate Cox regression analysis with shared frailty was used to assess the factors associated with failures (p < 0.05).
Results
Four hundred seventy-seven restorations carried out in 297 children (9.1 ± 1.7 years) were included in the analysis. The survival of the restorations reached 57.9 % up to 36 months follow-up with an overall annual failure rate of 16.7 %. There was no difference in restoration longevity when CCR or SCR was performed (p = 0.163); however, CCR presented more pulp exposure (p < 0.001). Multi-surface restorations showed more failures than single-surface (HR 3.22, 95 % CI 1.49; 6.97), and teeth restored with RMGIC had a lower survival rate than those restored with composite resin (HR 4.11, 95 % CI 1.91; 8.81). Patients with evidence of gingivitis had more risk of failure in their restorations (HR 2.88, 95 % CI 1.33; 6.24).
Conclusion
Overall, adhesive restorations performed in young permanent molars of high caries risk children presented limited survival, regardless of the caries removal technique. Risk factors for failure were identified as multi-surface fillings, RMGIC restorative material, and poor oral hygiene, reflected by gingival bleeding.
Clinical relevance
Composite fillings associated with a strict caries preventive regimen may play an important role in the survival of restorations placed in high caries risk children.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although the prevalence of caries has decreased worldwide [1], it still remains the main oral health problem for children and adolescents [2]. The severity of caries is also high in this young population, and the occurrence of deep lesions in permanent teeth is a common feature in daily clinical practice [2]. The treatment based on complete caries removal (CCR) in proximity to the pulp is often associated with immediate or long-term complications [3]. Recent research has demonstrated that complete caries removal in active deep lesions results in increased pulp exposure and post-operative symptoms in comparison with the risk after selective (partial) caries removal (SCR) [4–6].
Therefore, non-invasive and minimally invasive techniques have a great impact on contemporary practice for managing carious lesions, reducing the potentially adverse effects of more invasive treatment in patients [7]. The goal of SCR is based on modification of the microenvironment of the contaminated dentin, intentionally left under the restoration, thereby arresting the cariogenic process while preserving the tooth structure and pulp vitality [8].
Although there is sound scientific evidence that demonstrates the good results of such a technique [4, 5, 9], a high proportion of dentists still prefer to remove all the carious dentin even under the imminent risk of pulp exposure. One of the reasons for clinicians avoiding SCR is the fear of caries progression under the restoration and, consequently, damage to the dental pulp. Dentists also reported preferring more invasive treatment with the aim of improving the longevity of the restoration, even at the risk of compromising pulp vitality [10]. Indeed, there is some question in relation to the potential detrimental effect of affected dentin on the long-term survival of restorations. While some affirm that the demineralized dentine does not significantly decrease the in vitro fracture resistance of restored teeth [11], others hypothesize that caries dentin left in the bottom of the cavity may act as a “soft” layer which, under constant masticatory efforts, could lead to restoration fracture [12]. However, this assumption remains to be clinically evaluated as in vitro studies lack the biological activity of dental pulp cells in the remineralization of the affected dentin via mineral deposits.
The data available on longevity of restorations performed in young permanent teeth after SCR is still limited [6, 13] because the “pulp vitality” has been the main outcome. Moreover, the influence of individual and tooth-related factors associated with restorative failures has not been investigated.
Thus, the aim of this retrospective university-based study has been to evaluate the survival and factors associated with failure of adhesive restorations placed in young permanent molars of a high caries risk population following CCR and SCR. The hypothesis raised here is that the caries removal techniques do not affect the survival of the adhesive restorations performed in young permanent teeth.
Materials and methods
Study characteristics, participants, and study design
For this study, the research protocol gained approval from the Research Committee (n. 26760) and the local University Ethics Committee (n. 35380414.2.0000.5347). For the collection of data, written informed consent was signed by the parents or guardians. The personal information of the patients was kept confidential.
This retrospective university practice-based study was conducted at the Children and Youth Dental Clinic, School of Dentistry, the Federal University of Rio Grande do Sul (UFRGS), Porto Alegre, Brazil. This public pediatric dental clinic attends children and adolescent patients at a low charge, who are mainly from low socioeconomic backgrounds. The target population was children and adolescents treated during the period between 2009 and 2013, when they were attended by undergraduate and graduate dental students, supervised by clinical instructors, who are specialists in pediatric dentistry. All the information employed in this study was gathered from clinical records. To be eligible for the study, children should have received at least one restoration (one, two, or more surfaces), performed with composite resin (CR) or resin-modified glass ionomer cement (RMGIC), placed in vital posterior permanent teeth after complete or selective caries removal. The restorations should have been clinically and/or radiographically followed up for at least 6 months, and individuals should attend the dental clinic at least twice a year. Children with compromised systemic health were excluded from the study.
Caries removal and restorative procedures
The CCR or SCR restorations were performed in one appointment in deep carious lesions (located on the inner half of the dentin) of young permanent teeth. The treatment decision of CCR or SCR was made by the instructors. After administration of local anesthesia and rubber dam isolation, dentinal carious tissue was completely removed from the lateral walls of the cavities using round burs operated at low speed. The same procedure from the lateral walls was performed in the pulp wall for CCR. The absence of carious tissue was confirmed using a blunt-tipped probe. Visual and tactile criteria were used for SCR at the site of “risk for pulp exposure.” The selective caries excavation was performed with a dentin excavator, and caries removal was stopped when dentin with a leathery consistency was achieved. In some cases, a calcium hydroxide liner (Dycal, Dentsply, Brazil) was placed prior to CR or RMGIC restoration. For composite resin restoration, the cavity was conditioned by 37 % phosphoric acid gel for 15 s in dentin and 30 s in enamel. The acid was removed by rinsing with water for 30 s, and the cavity was gently dried with air and cotton pellets. A two-step etch-and-rinse adhesive system (Adper Single Bond, 3M ESPE, St. Paul, MN, USA) was used prior to the insertion of the composite resin (Filtek Z350, 3M ESPE, St. Paul, MN, USA) using the incremental technique. The cavities were filled with RMGIC (Vitremer, 3M ESPE, St. Paul, MN, USA) following the manufacturer’s protocol by applying the primer for 30 s in the entire cavity and then light curing for 20 s. The material was mixed in a 1:1 ratio, placed into the cavity using a syringe system, and then light cured for 40 s. For the proximal cavities, a metal matrix was adapted to the cervical margin with an interproximal wedge. The rubber dam was then removed and the occlusion was checked. Finally, a “finishing” gloss layer (Vitremer, 3M ESPE, St. Paul, MN, USA) was applied on the restorations with RMGIC and they were light cured for 20 s.
After restorative management and caries activity treatment, each patient was registered in an individual preventive program. The recalls consisted of visible plaque (visible plaque index (VPI)) and gingival bleeding (gingival bleeding index (GBI)) exams and dental hygiene orientation.
Data collection
One dentist retrieved all the information from dental records. The factors potentially associated with treatment failure were investigated, including individual and restoration characteristics: gender; patient’s age (years); VPI and GBI in the first appointment and at the end of the follow-up period; decayed, missing, and filled teeth (DMF-T, moderate and high); type of arch (superior and inferior); type of caries removal (complete or selective); number of restored surfaces (one, two, or more); base or liner material used (calcium hydroxide, glass ionomer cement, or adhesive system); restorative material (CR or RMGIC); and pulp complications (irreversible pulpitis or necrosis).
The visible plaque index and gingival bleeding index (Ainamo and Bay) were used to evaluate the routine of plaque control by the patients [14]. For the calculation of these indexes, the number of dental surfaces was divided by the surfaces with visible plaque or gingival bleeding. For the analysis, the values of these two indexes were dichotomized. A satisfactory biofilm control was considered when the VP and GB were less than 20 % [15]. Caries experience was categorized into moderate and high, using the median of DMF-T index as the cut-point.
The main outcome of the study was the failure of restorations placed in permanent molars. Failures were assessed by checking the patient’s records and were considered by the presence of loss of restoration or fracture, requiring re-intervention (restoration repair or replacement). In addition, teeth which underwent pulp intervention (endodontic treatment) or extraction were categorized as treatment failure. The radiographic outcome was performed by assessing the interproximal and periapical radiograph, according to the following criteria: presence of radiolucency in the furcation or periapex and increase in the periodontal space. The examiner was trained for diagnostic reproducibility, and this was determined by assessing 10 % of the radiographs at two different moments (2-week interval). Radiographic evaluation was carried out blind by the examiner. The intra kappa coefficient in the radiographic reproducibility evaluation was 0.86.
Data analysis
The descriptive analysis provides the distribution summary according to the independent variables. Data collected from patient records was included in a database and analyzed using Stata 11.2 software (College Station, TX, USA). The annual failure rate (AFR) of the restorations was calculated according to the formula: (1 − y)z = (1 − x), in which “y” expresses the mean AFR and “x” the total failure rate at “z” years. Restorations placed in teeth with pulp exposure during the dentin excavation (trans-operatory) were excluded from the longevity analysis.
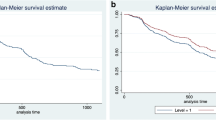
Survival analysis was performed to assess factors associated with the longevity of the restorations, and data was censored at 36 months of follow-up. Survival curves of the restorations were assessed through the Kaplan-Meier method. Curves were also adjusted by individuals to take into account clustering of data (more than one restoration per subject).
Multivariate Cox regression models with shared frailty were performed to identify factors associated with failure of restorations. These models consider that observations within the same group (the patient) are correlated, sharing the same frailty, being analogous to multilevel regression models with random effects. Hazard ratios and their respective 95 % confidence intervals (HR; 95 % CI) were obtained. A backward stepwise procedure was used to select covariates in the fitting of the model. Only those variables presenting p values <0.20 were selected to be included in the final model. A significance level of 5 % was considered.
Results
In this retrospective study, the information was retrieved from 372 dental records. Four hundred and seventy-seven restorations placed in 297 subjects were included in the analysis (Fig. 1, flow diagram). Boys comprised 46.7 % of the sample. The mean age of the children was 9.1 years (±1.7), presenting a DMF-T mean of 6.3 (±3.2). The mean of initial visible plaque index at the first visit was 35.3 % (±27.7), and gingival bleeding index was 27.0 % (±26.2). The mean of VPI and GBI at the last appointment was 26.0 % (±22.6) and 16.7 % (±18.0), respectively. The follow-up period ranged from 6 to 36 months.
The distribution of restorations placed in posterior permanent teeth, according to individual and tooth-level variables, is shown in Table 1.
Overall, the survival rate of restorations up to 36 months reached 57.9 %. The clinical and radiographic success was 82.8 % (395/477). Considering all outcomes (failures = 82), pulp complications (22/82—26.8 %) were less prevalent than restorative failures (60/82—73.2 %). According to the caries removal technique, CCR presented more pulp exposition than SCR during dentin caries excavation (p < 0.001). Pulp necrosis after restoration in unexposed pulp teeth was observed in 4.9 and 4.5 % for CCR or SCR, respectively.
The overall AFR after the 3-year follow-up was 16.7 %. Concerning the restorative material placed in deep caries cavities of posterior permanent teeth, the AFRs were 14.6 and 26.7 % for composite resin and RMGIC, respectively. Regarding caries removal, AFR in restorations where SCR was performed was 17.3 %, while for CCR, it was 13.1 %. No tooth was extracted due to restorative failure.
No difference was found in terms of the longevity of the restorative procedures executed by students at different levels of their education (p = 0.688).
Table 2 shows the results for Cox regression analysis, with crude and adjusted hazard ratios. The adjusted model showed that multi-surface restorations (three or more surfaces) placed in posterior permanent teeth had a risk of failure 3.22 times more than single-surface restorations (p = 0.003). Regarding the restorative material, RMGIC in comparison with composite resin had a risk of failure 4.11 times greater after 3 years of follow-up (p < 0.001). Patients presenting gingivitis (GB >20 %) had 2.88 times more risk of failure in their restorations (p = 0.007). In crude analysis, the use of a base/liner material under the restorations showed a lower survival rate (p = 0.001), but the association lost significance in the adjusted analyses.
Figure 2 shows the Kaplan-Meier curves of the restorations up to 36 months follow-up. Patients with GB index greater than 20 % experienced more failures in the restorations. The number of restored surfaces had a detrimental effect over the longevity of the fillings. Teeth presenting three or more restored surfaces presented more failures when compared to one and two surface restorations. Teeth restored with CR presented more longevity than those restored with RMGIC. Similar performance was observed in terms of longevity of restorations when complete or selective caries removal was performed.
Adjusted Kaplan-Meier survival curves. a Selective (SCR) and complete caries removal (CCR) technique presented similar survival rates. b Teeth presenting multi-restored surfaces showed more failures. c Resin-modified glass ionomer cement (RMGIC) presented more failures than composite resin (CR). d Patients with gingivitis (GBI >20 %) experienced more restorative failures. Curves were adjusted by all variables included in the final Cox regression model
Discussion
This retrospective university-based study provides valuable information regarding the longevity of restorations performed in deep carious lesions of young permanent molars and the associated risk factors for failure in a high caries risk pediatric population. The survival rate of the restorations reached 57.9 % after 3 years follow-up. The presence of gingivitis and the treatment-related variables, such as the number of restored surfaces and the type of restorative material, were associated with restoration failures. The SCR did not produce a detrimental effect on restoration survival, accepting the null hypothesis of this study.
For survival analyses, the Kaplan-Meier estimator was used in this study. Although the survival rate at 36 months appears to be low, it is important to note that the estimator takes into account the censored data, i.e., those restorations that have not yet reached the 36-month evaluation in this retrospective analysis. This explains the low estimated survival rate (57.9 %) of restorations when compared exclusively to clinical and radiographic success (82.8 %), when just the failures were counted (82/477), independently of the time in function.
The SCR constitutes the first option to treat deep carious lesions of deciduous and permanent teeth at the Children and Youth Dental Clinic (UFRGS), and undergraduate and graduate students have practiced it since the mid-1990s. In the present research, the majority of the restorative procedures involved SCR in deep caries lesions (78.82 %), which was performed in one appointment. Two CCR alternatives, in one and two steps, are commonly described for deep carious lesion management. In the two-step (stepwise) CCR, the carious dentin is incompletely removed in the proximity of the pulp wall and a temporary filling is placed to allow tertiary dentinogenesis. A second visit is then required for lesion re-entry and final complete excavation of the remaining carious dentin [16]. In SCR, carious dentin is partially removed nearest to the pulp, and a definitive restoration is placed in a single visit [6, 13]. Data from a randomized clinical trial has already shown the advantage of SCR compared with CCR in two steps (stepwise treatment) when pulp vitality was defined as the outcome [6].
Recently, a systematic review with meta-analysis demonstrated that SCR had a significant overall risk reduction of pulp exposure (OR [95 % CI] 0.31 [0.19–0.49]) compared with complete caries excavation [5]. Corroborating with the current literature, results from this retrospective study revealed that CCR was more harmful for the pulp as it induced more pulp exposure than SCR (p < 0.001). Pulp exposure occurring during caries removal and treated with conservative pulp therapies produces very low clinical success rate after long periods of time [17]. The pulp necrosis (4.6 %) that was observed during the follow-up period, for both CCR and SCR, could be associated with the limitation of establishing a correct diagnosis of pulp inflammation at the time of the restorative procedure. This difficulty is expected in teeth with incomplete root formation, wherein the responses of vitality tests are not accurate.
While research has strongly supported that SCR prevents pulp exposure and pulp sensitivity compared to CCR, the effectiveness in terms of longevity of the restorations is still lacking in evidence [5]. It is suggested that the softer and demineralized dentin may not sufficiently support the load from masticatory function and could reduce the bond resistance between the adhesive restoration and the tooth substrate [12]. The SCR showed higher frequency of restorative failures (15.4 %) compared to CCR (2.0 %). However, in the adjusted Cox regression analysis, the type of caries removal (complete or selective) was not found to be a significant factor affecting the restoration survival. This is an important finding from the present study because the potential detrimental effect on the restoration longevity has been considered a shortcoming for the SCR technique and this is one of the first clinical studies investigating this hypothesis.
It is also important to highlight that, clinically, the presence of affected dentin under the restorations may not be a problem as such lesions are normally surrounded by sound dentin or enamel [18, 19]. Moreover, all this information must be seen under the light of a biological balance perspective. Life expectation is increasing worldwide; thereby, if more invasive procedures are avoided, especially at younger ages, the occurrence of pulp intervention and its detrimental consequences can be prevented or, at least, postponed. Likewise, a cost effectiveness study comparing SCR and CCR (one and two steps) for deep carious lesions showed that CCR raises the risk of pulp damage and often initiates a cascade of re-intervention, which ultimately leads to tooth extraction. The study used a model that simulates the treatment of a molar tooth with a deep carious lesion in a 15-year-old patient. Results revealed that one-step SCR reduces patient pain and is a less time-consuming technique, besides reducing costs and keeping teeth vital for longer [3].
The presence of a lining material under the restorations could represent a significant effect on longevity of the restorations [20]. A practice-based study showed that the use of a calcium hydroxide liner under the composites placed in permanent teeth of children and adolescents presented a lower survival rate [21]. Also, the failures observed over time in restorations with a GIC base or liner material have been credited to fatigue, related to the weaker cement layer [22]. In crude analysis of the present research, the use of a capping or base material (calcium hydroxide or GIC) resulted in restorations with a lower survival rate (p < 0.001), but it lost significance after the adjustments (0.193). A possible explanation for this occurrence is based on the size of the cavities receiving the capping material. Commonly, larger cavities received the capping or base materials; thus, the size of the restored cavity had a greater influence on the failures of the restorations than the capping material, after the adjustment of the data. Corroborating with our results, a recent long-term clinical study showed no difference in posterior composite restoration survival when using a “soft” intermediate material compared to those without intermediate material [23].
In Brazil, there is a preference for tooth-colored direct materials, such as GIC and composite materials, to restore primary and permanent teeth of children and adolescents [24]. The GIC-based materials have several advantageous characteristics that qualify them for use in children’s clinics. They are used as restorers and base materials because they reduce marginal leakage and compensate for the polymerization shrinkage of composite restorations [25]. Moreover, they adhere chemically to the dentin and release fluoride ions, which can prevent the formation of adjacent lesions [26]. However, the major reason for their widespread use in pediatric dentistry is related to the facility of the technique, which is extremely important in the management of difficult behavior patients [27]. Concerning the restorative material placed in deep caries lesions of posterior permanent teeth, the survival rates after 3 years were 62.2 % for composite fillings and 39.3 % for light-cured modified glass ionomer restorations (p < 0.001). The superior behavior of composite restorations compared to GIC, which is credited to their mechanical properties, is well documented in the literature. Composite resin presents higher resistance to wear, higher micro-hardness, and a smoother surface when compared with GIC [28], and these characteristics over time should play a significant influence on the longevity of restorations. A recent study, evaluating posterior restorations placed in primary teeth from patients of low socioeconomic income in a pediatric clinic, showed a significantly higher risk of failure for GIC than for composite restorations after up to 4 years of follow-up [29].
The number of restored surfaces also had a detrimental effect over the longevity of the fillings. Teeth presenting three restored surfaces presented more failures when compared to one and two restored surfaces (p < 0.001). One study demonstrated that restorations with three or more involved surfaces have a relative risk of failure of 3.3 compared to class I restorations [30]. A systematic review and a prospective practice-based study on permanent teeth have already demonstrated a higher failure rate of multi-surface restorations [21, 31]. Several studies have shown that cavity size, cavity type, and the number of restores surfaces are associated with the failure risk [30–32].
It is well documented in the literature that dental biofilm is a marker for oral health patterns. While evaluating the trajectory of dental plaque from childhood until adult life in a birth cohort, investigators observed that a lifetime exposure to dental biofilm may be a key risk factor in cumulative dental diseases, such as caries, failure in restorative procedures, and tooth loss [33]. The results showed that patients presenting more sites with gingival bleeding (GBI >20 %) have 2.88 times more risk of failure in their restorations (p = 0.007). This clinical parameter (GB) is a more “faithful” reference from oral hygiene routine performed by patients than plaque index because patients usually brush their teeth before the dental appointment. Thus, gingival bleeding reveals that dental cleaning is not performed continuously. The population evaluated in the present study comprises high caries risk patients, which represents a challenging situation for restoration survival. Individuals at high caries risk were more likely to display failed composite restorations compared to those at lower risk [34].
All 477 restorative procedures were performed by undergraduate (fourth clinical year) and graduate students (specialization program in pediatric dentistry) under the supervision of clinical instructors. Although the operator could be an influential factor in restoration longevity [20], a recent study showed that undergraduate students at the fourth year from public Brazilian dental schools are able to produce high-quality anterior and posterior composite restorations [35].
Given the RCT as the gold standard design for longitudinal restoration analysis, the results of the present study should be viewed considering their possible methodological limitations. Some specific details could not be given, such as the presence of bruxism and children’s behavior during the treatment, as well as the reasons for restoration failure, which were not available in the patient’s records. Another restriction is in regard to the limited traceability of the real volume and depth of the cavities where the liner material was used, as well as the distribution among the used materials. In this study, the treatment decision was made by clinical instructors at the moment of the procedure. Usually, the deepest cavities are treated by SCR to avoid pulp exposure. The use of RMGIC is generally preferred in cases where there was no clinical time for restoration with composite resin and in non-cooperative children. If, on the one hand, the retrospective design lacks standardization of indication and treatment protocols, on the other hand, the results of RCTs have limitations for extrapolation to clinical practice because of the controlled conditions that are imposed [20, 36].
The relatively short follow-up period may also be considered as a limitation of the study as most of the failures in adhesive restorations occurred after 5 or 10 years in a low caries risk population [20]. Nevertheless, the young age associated with the high caries risk profile of children attended in the present study could have accelerated the failure process, which is a significant consideration for clinicians and researches dealing with individuals with this clinical profile.
Overall, this retrospective study demonstrates that the adhesive restorations offered restricted survival when placed in permanent molars of high risk caries children, with composite resin presenting better longevity than RMGIC, regardless of the caries removal technique. Multi-surface fillings and poor oral hygiene, reflected by gingival inflammation, reduced the longevity of the restorations.
References
Petersen PE (2003) The World Oral Health Report 2003: continuous improvement of oral health in the 21st century—the approach of the WHO Global Oral Health Programme. Community Dent Oral Epidemiol 31:3–24
SB BRAZIL (2010) National research on oral health 2010: main results
Schwendicke F, Stolpe M, Meyer-Lueckel H, Paris S, Dörfer CE (2013) Cost-effectiveness of one- and two-step incomplete and complete excavations. J Dent Res 10:880–887
Ricketts D, Lamont T, Innes NP, Kidd E, Clarkson JE (2013) Operative caries management in adults and children. Cochrane Database Syst Rev 3. doi:10.1002/14651858
Schwendicke F, Dörfer CE, Paris S (2013) Incomplete caries removal: a systematic review and meta-analysis. J Dent Res 92:306–314
Maltz M, Garcia R, Jardim JJ, de Paula LM, Yamaguti PM, Moura MS, Garcia F, Nascimento C, Oliveira A, Mestrinho HD (2012) Randomized trial of partial vs. stepwise caries removal: 3-year follow-up. J Dent Res 91:1026–1031
Ericson D (2007) The concept of minimally invasive dentistry. Dent Updat 34:9–10
Thompson V, Craig RG, Curro FA, Green WS, Ship JA (2008) Treatment of deep carious lesions by complete excavation or partial removal: a critical review. J Am Dent Assoc 139:705–712
Hayashi M, Fujitani M, Yamaki C, Momoi Y (2011) Ways of enhancing pulp preservation by stepwise excavation—a systematic review. J Dent 39:95–107
Schwendicke F, Meyer-Lueckel H, Dörfer C, Paris S (2013) Attitudes and behaviour regarding deep dentin caries removal: a survey among German dentists. Caries Res 47:566–573
Schwendicke F, Kern M, Meyer-Lueckel H, Boels A, Doerfer C, Paris S (2014) Fracture resistance and cuspal deflection of incompletely excavated teeth. J Dent 42(2):107–113
Hevinga MA, Opdam NJ, Frencken JE, Truin GJ, Huymans MC (2010) Does incomplete caries removal reduce strength of restored teeth? J Dent Res 89:1270–1275
Maltz M, Jardin JJ, Mestrinho HD, Yamaguti PM, Podestá K, Moura MS, de Paula LM (2013) Partial removal of carious dentine: a multicenter randomized controlled trial and 18-month follow-up results. Caries Res 47:103–109
Ainamo J, Bay I (1975) Problems and proposals for recording gingivitis and plaque. Int Dent J 25:229–235
Lang NP, Tonetti MS (2003) Periodontal risk assessment (PRA) for patients in supportive periodontal therapy (SPT). Oral Health Prev Dent 1:7–16
Bjorndal L, Larsen T, Thylstrup A (1997) A clinical and microbiological study of deep carious lesion during stepwise excavation using long treatment intervals. Caries Res 31:411–417
Barthel CR, Rosenkranz B, Leuenberg A, Roulet JF (2000) Pulp capping of carious exposures: treatment outcome after 5 and 10 years: a retrospective study. J Endod 26:525–528
Schwendicke F, Kern M, Blunck U, Dörfer C, Drenck J, Paris S (2014) Marginal integrity and secondary caries of selectively excavated teeth in vitro. J Dent 10:1261–1268
Yoshiyama M, Tay FR, Doi J, Nishitani Y, Yamada T, Itou K, Carvalho RM, Nakajima M, Pashley DH (2002) Bonding of self-etch and total-etch adhesives to carious dentin. J Dent Res 8:556–560
Demarco FF, Corrêa MB, Cenci MS, Moraes RR, Opdam NJ (2012) Longevity of posterior composite restorations: not only a matter of materials. Dent Mater 28:87–101
Pallesen U, van Dijken JW, Halken J, Hallonsten AL, Höigaard R (2013) Longevity of posterior resin composite restorations in permanent teeth in public dental health service: a prospective 8 years follow up. J Dent 4:297–306
De Munck J, Van Landuyt KL, Coutinho E, Poitevin A, Peumans M, Lambrechts P et al (2005) Fatigue resistance of dentin/composite interfaces with an additional intermediate elastic layer. Eur J Oral Sci 113:77–82
van de Sande FH, Da Rosa Rodolpho PA, Basso GR, Patias R, da Rosa QF, Demarco FF et al (2015) 18-year survival of posterior composite resin restorations with and without glass ionomer cement as base. Dent Mater 31:669–675
Azevedo MS, Vilas Boas D, Demarco FF, Romano AR (2010) Where and how are Brazilian dental students using glass ionomer cement? Braz Oral Res 24:482–487
Taha NA, Palamara JE, Messer HH (2009) Cuspal deflection, strain and microleakage of endodontically treated premolar teeth restored with direct resin composites. J Dent 37:724–730
Basso GR, Della Bona A, Gobbi D, Cecchetti D (2011) Fluoride release from restorative materials. Braz Dent J 22:355–358
Casagrande L, Dalpian DM, Ardenghi TM, Zanatta FB, Balbinot CE, García-Godoy F, De Araujo FB (2013) Randomized clinical trial of adhesive restorations in primary molars. 18-month results. Am J Dent 6:351–355
Barbosa RP, Pereira-Cenci T, Silva WM, Coelho-de-Souza FH, Demarco FF, Cenci MS (2012) Effect of cariogenic biofilm challenge on the surface hardness of direct restorative materials in situ. J Dent 40:359–363
Pinto Gdos S, Oliveira LJ, Romano AR, Schardosim LR, Bonow ML, Pacce M et al (2014) Longevity of posterior restorations in primary teeth: results from a paediatric dental clinic. J Dent 42:1248–1254
Da Rosa Rodolpho PA, Donassollo TA, Cenci MS, Loguercio AD, Moraes RR, Bronkhorst EM, Opdan NJ, Demarco FF (2011) 22-year clinical evaluation of the performance of two posterior composites with different filler characteristics. Dental Mater 27:955–963
Opdam NJ, Bronkhorst EM, Roeters JM, Loomans BA (2007) Longevity and reasons for failure of sandwich and total-etch posterior composite resin restorations. J Adhes Dent 9:469–475
Van Nieuwenhuysen JP, D’Hoore W, Carvalho J, Qvist V (2003) Long-term evaluation of extensive restorations in permanent teeth. J Dent 31:395–405
Broadbent JM, Thomson WM, Boyens JV (2011) Dental plaque and oral health during the first 32 years of life. Am J Dent 142:415–426
van de Sande FH, Opdam NJ, Rodolpho PA, Correa MB, Demarco FF, Cenci MS (2013) Patient risk factors’ influence on survival of posterior composites. J Dent Res 92:78–83
Moura FR, Romano AR, Lund RG, Piva E, Rodrigues Júnior SA, Demarco FF (2011) Three-year clinical performance of composite restorations placed by undergraduate dental students. Braz Dent J 22:111–116
Opdam NJM, Bronkhorst E, Cenci M, Huysmans MC, Wilson NHF (2011) Age of failed restorations: a deceptive longevity parameter. J Dent 39:225–230
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Author Alejandra Tejeda Seminario declares that she has no conflict of interest; author Marcos Britto Correa declares that he has no conflict of interest; author Stefanie Bressan Werle declares that she has no conflict of interest; author Marisa Maltz declares that she has no conflict of interest; author Flávio Fernando Demarco declares that he has no conflict of interest; author Fernando Borba de Araujo declares that he has no conflict of interest; and author Luciano Casagrande declares that he has no conflict of interest.
Funding
The costs of this retrospective study were funded by the researchers.
Ethical approval
All procedures performed in the present research were in accordance with the ethical standards of the Resolution of the National Council on Ethics in Research (n. 466,/2012) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from the parents or guardians of all children included in the study. The protocol of this research was submitted and approved by the Research Committee (n. 26760) and the Ethic Committee (n. 35380414.2.0000.5347) of the Federal University of Rio Grande do Sul, Porto Alegre, RS - Brazil.
Rights and permissions
About this article
Cite this article
Casagrande, L., Seminario, A.T., Correa, M.B. et al. Longevity and associated risk factors in adhesive restorations of young permanent teeth after complete and selective caries removal: a retrospective study. Clin Oral Invest 21, 847–855 (2017). https://doi.org/10.1007/s00784-016-1832-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-016-1832-1