Abstract
Objectives
The use of platelet concentrates has gained increasing awareness in recent years for regenerative procedures in modern dentistry. The aim of the present study was to compare growth factor release over time from platelet-rich plasma (PRP), platelet-rich fibrin (PRF), and a modernized protocol for PRF, advanced-PRF (A-PRF).
Materials and methods
Eighteen blood samples were collected from six donors (3 samples each for PRP, PRF, and A-PRF). Following preparation, samples were incubated in a plate shaker and assessed for growth factor release at 15 min, 60 min, 8 h, 1 day, 3 days, and 10 days. Thereafter, growth factor release of PDGF-AA, PDGF-AB, PDGF-BB, TGFB1, VEGF, EGF, and IGF was quantified using ELISA.
Results
The highest reported growth factor released from platelet concentrates was PDGF-AA followed by PDGF-BB, TGFB1, VEGF, and PDGF-AB. In general, following 15–60 min incubation, PRP released significantly higher growth factors when compared to PRF and A-PRF. At later time points up to 10 days, it was routinely found that A-PRF released the highest total growth factors. Furthermore, A-PRF released significantly higher total protein accumulated over a 10-day period when compared to PRP or PRF.
Conclusion
The results from the present study indicate that the various platelet concentrates have quite different release kinetics. The advantage of PRP is the release of significantly higher proteins at earlier time points whereas PRF displayed a continual and steady release of growth factors over a 10-day period. Furthermore, in general, it was observed that the new formulation of PRF (A-PRF) released significantly higher total quantities of growth factors when compared to traditional PRF.
Clinical relevance
Based on these findings, PRP can be recommended for fast delivery of growth factors whereas A-PRF is better-suited for long-term release.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A number of techniques have been utilized in modern dentistry to speed the regeneration of either hard or soft tissues [1–4]. While a great deal of effort in recent years has been focused on the use of biologics as key mediators of tissue regeneration, some of the disadvantages of utilizing recombinant growth factors include high supra-physiological doses as well as high costs associated with their use [5–7]. Nevertheless, the use of growth factors such as recombinant platelet-derived growth factor (PDGF) has been shown to positively increase tissue formation across a wide variety of clinical procedures in both dentistry and medicine [8].
While the use of recombinant growth factors have demonstrated significant advantages, the use of autologous platelet concentrates has also been shown to support tissue regeneration [9, 10]. Platelet-rich plasma (PRP) is an autologous concentration of growth factors derived from patient whole blood centrifuged to reach super-natural concentrations [9, 10]. In the 1970s, it was introduced as “fibrin glue” and has gained popularity in the medical and dental fields for the regeneration of both hard and soft tissues [11–16]. Early experiments revealed the ability for several key growth factors found in the blood (including PDGF) to significantly modulate tissue repair and wound healing events [11–16].
The use of PRP has since been utilized by both oral surgeons and periodontists alike demonstrating advantages associated with its use for a variety of extensive dental regenerative procedures [16–21]. Furthermore, reports have demonstrated that PRP may also successfully be combined with various biomaterials including collagen membranes and bone grafting materials [22–27]. One of the reported drawbacks of PRP is that it contains anticoagulants, an event that interferes with the natural healing process despite containing a number of growth factors implicated in tissue repair [9, 10].
Following numerous research utilizing PRP, further investigation found that a platelet concentrate made from whole blood without the use of coagulants could also be further utilized to improve wound healing [28–32]. This protocol has been termed platelet-rich fibrin (PRF, also more recently referred to as leukocyte-PRF or L-PRF) and involves the use of a fibrin clot which may be utilized as a membrane containing autologous growth factors hypothesized to slowly release growth factors to the surrounding environment during wound healing [21, 33–36].
Recently, these investigators have formulated a new protocol for PRF where centrifugation procedures have been altered to further improve tissue regeneration [37]. While standard PRF is centrifuged at 2700 rpm for 12 min, the advanced platelet-rich fibrin (A-PRF) is centrifuged at slower speeds (1500 rpm, 14 min). This modification to centrifugation protocol has previously been shown to increase platelet cell numbers and monocytes/macrophages behavior [37]. Despite these findings, little is known about the release of growth factors from the various platelet concentrates over time with no data available to date on A-PRF. Therefore, the aim of the present study was to compare growth factor release from PRP, PRF, and A-PRF over time and investigate the in vitro release of seven growth factors at 15 min, 60 min, 8 h, 1 day, 3 days, and 10 days post incubation. The growth factors investigated include PDGF-AA, PDGF-AB, PDGF-BB, transforming growth factor beta 1 (TGFB1), vascular endothelial growth factor (VEGF), epidermal growth factor (EGF), and insulin-like growth factor (IGF).
Materials and methods
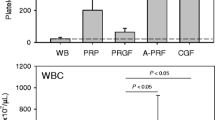
Platelet concentrations
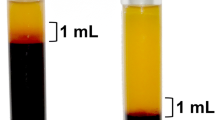
Three samples of blood were collected with the informed consent of six volunteer donors (18 total samples) and the blood was then processed for PRP, PRF, or A-PRF centrifugation. All blood samples were obtained from members of our laboratory between the ages of 30 and 60. PRP platelet concentration was prepared via a protocol as previously described [38]. Briefly, 10 mL of whole blood was centrifuged for 7 min at 1000 rpm (45 g) at room temperature without brake (centrifuge 5702; Eppendorf, Darmstadt, Germany). The plasma rum was decanted up to the erythrocyte sediment and then centrifuged again for 10 min at 3,000 rpm (400g) at room temperature. Finally, the PRP was decanted and the final PRP sediment was suspended in 6-well in vitro plastic culture dishes with 5 mL of culture media and processed as further described.
The PRF and A-PRF were also isolated as previously described [37]. Ten milliliters of whole blood without anticoagulant was centrifuged at 2,700 rpm (325g) for 12 min whereas A-PRF was centrifuged at 1,500 (100g) for 14 min. The lack of anticoagulants in these samples allows for a fibrin clot formation to form which can then be collected in the middle of the tube between the red corpuscles at the bottom and acellular plasma at the top. Thereafter, PRP, PRF, and A-PRF clots were then transferred to 6-well in vitro plastic culture dishes with 5 mL and processed for further investigation.
Protein quantification with ELISA
In order to determine the amount of released growth factors at 15 min, 60 min, 8 h, 1 day, 3 days, and 10 days, samples were placed into a shaking incubator at 37 °C to allow for growth factor release into the culture media. At each time point, the 5 mL of culture media was collected, frozen, and replaced with 5 mL of additional culture media. Protein quantification was carried out using ELISA. At desired time points, PDGF-AA (DY221, range = 15.60–1000 pg/mL), PDGF-AB (DY222, range = 15.60–1,000 pg/mL), PDGF-BB (DY220, 31.20–2,000 pg/mL_, TGFβ1 (DY240, range = 31.20–2,000 pg/mL), VEGF (DY293B, range = 31.20–2,000 pg/mL), IGF (DY291, range = 31.20–2,000 pg/mL) and EGF (DY236), range = 3.91–250 pg/mL) were quantified using an ELISA assays (RND Systems, Minneapolis, MN, USA) according to manufacturer’s protocol as previously described [39]. Briefly, 100 μL of assay diluents and 100 μL of sample were incubated for 2 h at room temperature in antibody-precoated 96-well plates. Wells were washed four times with washing buffer, incubated for 2 h with peroxidase-conjugated antibody solution, washed again, followed by addition of 100 μL of substrate solution for 20 min and 50 μl of stopping solution for 20 min. Absorbance was measured at 450 and 570 nm on an Infinite 200 microplate reader (Tecan Group LTD, Männedorf, Switzerland) and subtracted at 570 nm from the readings at 450 nm. All samples were measured in triplicate and three independent experiments were performed for each platelet concentrate. Statistical analysis was performed by two-way ANOVA with Bonferroni test.
Results
Total protein released from PRP, PRF, and A-PRF after 10 days
All proteins were quantified for both growth factor release at desired time points as well as the total accumulated protein quantities (Figs. 1–3, Table 1). It was found that A-PRF released the highest total amount of growth factors when compared to either PRF or PRP (Table 1). Subsequently, release of PDGF-AA was found highest for all platelet concentrates followed by TGF-beta1, PDGF-BB, PDGF-AB, VEGF, EGF, and IGF with slight differences observed between groups (Table 1). It was found that A-PRF released 11048.19 ng/mL of total protein after 10 days, significantly more than PRF 9261.89 ng/mL and PRP 6176.15 ng/mL. Interestingly, PDGF-AA was found released from all platelet concentrations at 6–10-fold higher concentrations when compared to PDGF-AB and PDGF-BB. Furthermore, significantly lower levels of EGF and IGF were found when compared to PDGF, TGF-beta1, and VEGF concentrations (Table 1).
ELISA protein quantification at each time point of a PDGF-AA, c PDGF-AB, and e PDGF-BB over a 10-day period. Total accumulated growth factor released over a 10-day period for b PDGF-AA, d PDGF-AB, and f PDGF-BB. (*p < 0.05 signifies significant difference between groups, **p < 0.05 signifies significantly higher than all other groups, # p < 0.05 signifies significantly lower than all groups.) Assay performed in triplicate from six different blood samples
PDGF-AA, PDGF-AB, and PDGF-BB growth factor release from PRP, PRF, and A-PRF over time
Analysis of growth factor release of PDGF-AA, PDGF-AB, and PDGF-BB at each time point as well as accumulated over time is displayed in Fig. 1. It was found that after 15 min, significantly higher levels of PDGF-AA was released from PRP when compared to PRF or A-PRF. Interestingly, significantly lower levels were observed at 60 min demonstrating that PRP rapidly releases PDGF-AA between 0 and 15 min and thereafter significantly less release is observed comparatively up to 10 days (Fig. 1a). No significant differences between A-PRF and PRF at times points ranging from 15 min to 1 day; however, at 3 days, A-PRF showed significantly higher growth factor release of PDGF-AA when compared to either PRP or PRF (Fig. 1a). The total PDGF-AA accumulated proteins over time (Fig. 1b) demonstrated that while PRP showed significantly higher levels at an early time point of 15 min, thereafter significantly lower levels could be observed from 8 h till 10 days. In contrast, significantly higher levels were found for A-PRF from 1 to 10 days when compared to PRP or PRF (Fig. 1b). Similar trends were also observed for PDGF-AB and PDGF-BB (Fig. 1c–f). Interestingly, however, the total protein content for growth factor PDGF-BB was significantly higher in PRP samples when compared to PRF and A-PRF at all time points (Fig. 1f).
TGFB1 and VEGF growth factor release from PRP, PRF, and A-PRF over time
Thereafter, the release of TGFB1 and VEGF were quantified over time (Fig. 2). Once again, it was observed that PRP demonstrated significantly higher levels at early time points of 15 min and 8 h when compared to PRF and A-PRF (Fig. 2a, c). Thereafter, PRP levels dropped to significantly lower levels when compared to PRF or A-PRF with A-PRF demonstrating the significantly highest levels at 1, 3, and 5 days for both TGFB1 and VEGF concentrations (Fig. 2a, c). Parallel to the results obtained with PDGF, total protein accumulation was significantly highest at early time points for PRP and significantly dropped to lower levels by 10 days when compared to PRF and A-PRF (Fig. 2b, d). Total protein release was significantly highest for A-PRF at 3 and 10 days for TGFB1 and 1, 3, and 10 days for VEGF when compared to PRP and PRF (Fig. 2b, d).
ELISA protein quantification at each time point of a TGFB1 and c VEGF over a 10-day period. Total accumulated growth factor released over a 10-day period for b TGFB1 and d VEGF. (*p < 0.05 signifies significant difference between groups, **p < 0.05 signifies significantly higher than all other groups, # p < 0.05 signifies significantly lower than all groups.) Assay performed in triplicate from six different blood samples
EGF and IGF growth factor release from PRP, PRF, and A-PRF over time
Different trends were observed for the release of EGF and IGF (Fig. 3). Significantly highest levels for PRP were found only at 15 days for PRP (Fig. 3a). Thereafter, significantly highest protein release was found on A-PRF for EGF at 60 min, 8 h, 1 day, and 3 days (Fig. 3a). While no differences in PRF and A-PRF could be observed for protein release of IGF at almost all time points, significantly lower levels were observed for PRP at 15 min, 60 min, 8 h, and 1 day comparatively (Fig. 3c). Total protein accumulation demonstrated the highest total growth factor of EGF for A-PRF with the lowest being PRP whereas slightly higher PRF results were observed for IGF when compared to A-PRF (Fig. 3d).
ELISA protein quantification at each time point of a EGF and c IGF over a 10-day period. Total accumulated growth factor released over a 10-day period for b EGF and d IGF. (*p < 0.05 signifies significant difference between groups, **p < 0.05 signifies significantly higher than all other groups, # p < 0.05 signifies significantly lower than all groups.) Assay performed in triplicate from six different blood samples
Discussion
The aim of the present study was to compare growth factor release from three different platelet concentrates including PRP, PRF, and a new protocol established termed advanced-PRF. While the advancements made in terms of platelet concentrates have been hypothesized to improve tissue regeneration [37], no information is available to date regarding the growth factors released from these three platelet concentrates over time. Therefore, the aim of the present study was to investigate in detail five different growth factors including three isomers of PDGF (AA, AB, and BB) on protein release over time from PRP, PRF, and A-PRF.
Three things stand out from the results in the current investigation. First, it was found that PRP released the highest amount of growth factors at early time points when compared to either PRF or A-PRF. The fast action of released proteins found in PRP concentrates may be hypothesized to speed the recruitment of incoming progenitor cells in defect locations and could prove a valuable means in medical and dental procedures requiring rapid incoming recruitment of regenerative cells. Secondly, while the release of PRP had rapid release of growth factors, it was interesting to note that over time, PRF not only had more growth factor released at later time points but also contained more growth factors as a whole from within their fibrin matrix. One of the hypothesized reasons for this is the fact that PRF and A-PRF have been shown to contain more living cells [37]. Therefore, these cells are likely the contributing difference between the results observed between PRF, A-PRF, and PRP. Lastly, one of the surprising findings from the present study was the significant increase in total protein released between PRF and A-PRF. While it has been shown that A-PRF contains more living progenitor cells and platelets when compared to PRF [37], the subsequent significant increase in total protein release may therefore present additional advantages for clinical use.
Although this is the first report to investigate release of growth factors from A-PRF, previous authors have investigated protein release from either PRP or PRF and further investigated its subsequent effect on cell activity. In a first study, El-Sharkawy et al. demonstrated that PRP was able to promote increases in PDGF-AB, PDGF-BB, TGF-B1, VEGF, and EGF when compared to whole blood [40]. Furthermore, in another previous study it has been shown that PRF could release various growth factors including PDGF-AB, TGF-B1, VEGF, EGF, and IGF-1 [41]. The results from that study demonstrate an increase in growth factor over time from 5 to 300 min but did not look at later time points. Furthermore, the release of growth factors was not compared to a second platelet concentrate making it difficult to investigate the potency of PRF in comparison to either PRP or A-PRF [41].
It has also previously been shown that PRP has high levels of secreted PDGF and TGFB [42] which subsequently stimulates collagen synthesis in PDL cells and gingival fibroblasts [43, 44], induces cell proliferation [45] and mineralization potential in osteoblasts [46], and increases endothelial cell activity [47] in vitro. Gassling et al. showed that osteoblasts and fibroblasts that were cultured with PRP or PRF demonstrated varying expression of various growth factors with those cultured with PRP favoring significantly higher levels of PDGF-AB and TGFB1 expression [38]. Furthermore, a second report by this group compared PRF (as a membrane) to bovine-derived collagen membranes (BioGide) and tested osteoblast response to the two biomaterials [48]. It was found that cell growth was significantly higher on PRF when compared to the bovine collagen membrane [48].
Another aspect that needs to be considered when comparing in vivo work with in vitro studies is the variability in growth factor concentrations between donors. In the present study, the patient age range was between 30 and 60. We found reported differences between minimum and maximum growth factor accumulation between donors as reported in Table 1. Furthermore, with an increasingly aging population continuously requiring regenerative procedures, one can only expect that with advanced age (and the likelihood of increased systemic diseases and medications), a much larger variability may also be expected. Therefore, ongoing research investigating the optimal concentrations may be required to further optimize this avenue of research. It was also found in the present study that the slower spinning protocols of A-PRF released more growth factor than the prototype PRF. As one previous report demonstrated that A-PRF contains more platelets and neutrophilic granulocytes [37], it may be hypothesized that these cells contributed to the slight increase in total growth factor accumulation after a 10-day period. This hypothesis however requires further investigation.
There remain several aspects of research necessary to further compare the various platelet formulations investigated in this study. First, it is unclear how the release of the various platelet concentrates including PRP, PRF, and A-PRF will affect cell behavior over time. Therefore, a comparative in vitro cell study further investigating the use of PRP, PRF, and A-PRF on cell behavior of various cell types including osteoblasts, gingival fibroblasts, and periodontal ligament cells could further provide rationale for which treatment modalities stimulates a higher cell response. Furthermore, it is known that platelet concentrates are often combined with various biomaterials such as collagen membranes and bone grafting materials. Therefore, it would also be worthwhile to compare growth factor release from a variety of biomaterials following coating with either PRP, PRF, or A-PRF. Future research comparing the various platelet formulations in a clinical setting would also be valuable to compare which indications may serve better for various clinical scenarios.
Conclusion
The results from the present study demonstrated that PRP, PRF, and A-PRF were able to release growth factors over time from their respective platelet formulations. Interestingly, PRP demonstrated the ability to release significantly higher levels of growth factors at very early time points whereas PRF and A-PRF had a more gradual release of growth factors up to a 10-day period. The new formulation of PRF (called advanced-PRF) stimulated significantly higher growth factor release over time when compared to standard PRF and may prove clinically beneficial for future regenerative procedures. Future investigations studying the effects of each platelet formulation on cell behavior as well as in vivo study would further enhance our understanding for how A-PRF compares to previously utilized PRP and A-PRF.
References
Dohan Ehrenfest DM, Wang HL, Galindo-Moreno P, Bowler D, Dym H (2015) Bone morphogenic protein: application in implant dentistry. BioMed Res Int 59:493–503. doi:10.1155/2015/34132710.1016/j.cden.2014.10.006
Padial-Molina M, O’Valle F, Lanis A and Mesa F (2015) Clinical application of mesenchymal stem cells and novel supportive therapies for oral bone regeneration. Biomed Res Int 2015:341327. doi:10.1155/2015/341327
Sanz-Sanchez I, Ortiz-Vigon A, Sanz-Martin I, Figuero E, Sanz M (2015) Effectiveness of lateral bone augmentation on the alveolar crest dimension: a systematic review and meta-analysis. J Dent Res 94:128s–142s. doi:10.1177/0022034515594780
Miron RJ, Zhang YF (2012) Osteoinduction: a review of old concepts with new standards. J Dent Res 91:736–744. doi:10.1177/0022034511435260
Anusaksathien O, Giannobile WV (2002) Growth factor delivery to re-engineer periodontal tissues. Curr Pharm Biotechnol 3:129–139
Carreira AC, Lojudice FH, Halcsik E, Navarro RD, Sogayar MC, Granjeiro JM (2014) Bone morphogenetic proteins: facts, challenges, and future perspectives. J Dent Res 93:335–345. doi:10.1177/0022034513518561
Rocque BG, Kelly MP, Miller JH, Li Y, Anderson PA (2014) Bone morphogenetic protein-associated complications in pediatric spinal fusion in the early postoperative period: an analysis of 4658 patients and review of the literature. J Neurosurg Pediatr 14:635–643. doi:10.3171/2014.8.peds13665
Kaigler D, Avila G, Wisner-Lynch L, Nevins ML, Nevins M, Rasperini G, Lynch SE, Giannobile WV (2011) Platelet-derived growth factor applications in periodontal and peri-implant bone regeneration. Expert Opin Biol Ther 11:375–385. doi:10.1517/14712598.2011.554814
Del Corso M, Vervelle A, Simonpieri A, Jimbo R, Inchingolo F, Sammartino G, Dohan Ehrenfest DM (2012) Current knowledge and perspectives for the use of platelet-rich plasma (PRP) and platelet-rich fibrin (PRF) in oral and maxillofacial surgery part 1: periodontal and dentoalveolar surgery. Curr Pharm Biotechnol 13:1207–1230
Simonpieri A, Del Corso M, Vervelle A, Jimbo R, Inchingolo F, Sammartino G, Dohan Ehrenfest DM (2012) Current knowledge and perspectives for the use of platelet-rich plasma (PRP) and platelet-rich fibrin (PRF) in oral and maxillofacial surgery part 2: bone graft, implant and reconstructive surgery. Curr Pharm Biotechnol 13:1231–1256
Medina-Porqueres I, Alvarez-Juarez P (2015) The efficacy of platelet-rich plasma injection in the management of hip osteoarthritis: a systematic review protocol. Musculoskeletal Care. doi:10.1002/msc.1115
Salamanna F, Veronesi F, Maglio M and Della Bella E (2015) New and emerging strategies in platelet-rich plasma application in musculoskeletal regenerative procedures: general overview on still open questions and outlook. 2015:846045. doi: 10.1155/2015/846045
Albanese A, Licata ME, Polizzi B, Campisi G (2013) Platelet-rich plasma (PRP) in dental and oral surgery: from the wound healing to bone regeneration. Immun Ageing 10:23. doi:10.1186/1742-4933-10-23
Dohan Ehrenfest DM, Andia I, Zumstein MA, Zhang CQ, Pinto NR, Bielecki T (2014) Classification of platelet concentrates (platelet-rich plasma-PRP, platelet-rich fibrin-PRF) for topical and infiltrative use in orthopedic and sports medicine: current consensus, clinical implications and perspectives. Muscles, Ligament Tendons J 4:3–9
Maney P, Amornporncharoen M, Palaiologou A (2013) Applications of plasma rich in growth factors (PRGF) in dental surgery: a review. J West Soc of Periodontol Periodontal Abstr 61:99–104
Panda S, Doraiswamy J, Malaiappan S, Varghese SS and Del Fabbro M (2014) Additive effect of autologous platelet concentrates in treatment of intrabony defects: a systematic review and meta-analysis. J Investig Clin Dent. doi: 10.1111/jicd.12117
Marx RE (2001) Platelet-rich plasma (PRP): what is PRP and what is not PRP? Implant Dent 10:225–228
Marx RE (2004) Platelet-rich plasma: evidence to support its use. J Oral Maxillofac Surg Off J Am Assoc Oral Maxillofac Surg 62:489–496
Marx RE, Carlson ER, Eichstaedt RM, Schimmele SR, Strauss JE, Georgeff KR (1998) Platelet-rich plasma: growth factor enhancement for bone grafts. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 85:638–646
Kukreja BJ, Dodwad V, Kukreja P, Ahuja S, Mehra P (2014) A comparative evaluation of platelet-rich plasma in combination with demineralized freeze-dried bone allograft and DFDBA alone in the treatment of periodontal intrabony defects: a clinicoradiographic study. J Indian Soc of Periodontol 18:618–623. doi:10.4103/0972-124x.142457
Pradeep AR, Rao NS, Agarwal E, Bajaj P, Kumari M, Naik SB (2012) Comparative evaluation of autologous platelet-rich fibrin and platelet-rich plasma in the treatment of 3-wall intrabony defects in chronic periodontitis: a randomized controlled clinical trial. J Periodontol 83:1499–1507. doi:10.1902/jop.2012.110705
Dori F, Arweiler N, Huszar T, Gera I, Miron RJ, Sculean A (2013) Five-year results evaluating the effects of platelet-rich plasma on the healing of intrabony defects treated with enamel matrix derivative and natural bone mineral. J Periodontol 84:1546–1555. doi:10.1902/jop.2013.120501
Ozdemir B, Okte E (2012) Treatment of intrabony defects with beta-tricalciumphosphate alone and in combination with platelet-rich plasma. J Biomed Mater Res B, Appl Biomater 100:976–983. doi:10.1002/jbm.b.32660
Yilmaz S, Kabadayi C, Ipci SD, Cakar G, Kuru B (2011) Treatment of intrabony periodontal defects with platelet-rich plasma versus platelet-poor plasma combined with a bovine-derived xenograft: a controlled clinical trial. J Periodontol 82:837–844. doi:10.1902/jop.2010.100503
Camargo PM, Lekovic V, Weinlaender M, Divnic-Resnik T, Pavlovic M, Kenney EB (2009) A surgical reentry study on the influence of platelet-rich plasma in enhancing the regenerative effects of bovine porous bone mineral and guided tissue regeneration in the treatment of intrabony defects in humans. J Periodontol 80:915–923. doi:10.1902/jop.2009.080600
Camargo PM, Lekovic V, Weinlaender M, Vasilic N, Madzarevic M, Kenney EB (2005) A reentry study on the use of bovine porous bone mineral, GTR, and platelet-rich plasma in the regenerative treatment of intrabony defects in humans. Int J Periodontics Restorative Dent 25:49–59
Yassibag-Berkman Z, Tuncer O, Subasioglu T, Kantarci A (2007) Combined use of platelet-rich plasma and bone grafting with or without guided tissue regeneration in the treatment of anterior interproximal defects. J Periodontol 78:801–809. doi:10.1902/jop.2007.060318
Choukroun J, Diss A, Simonpieri A, Girard MO, Schoeffler C, Dohan SL, Dohan AJ, Mouhyi J, Dohan DM (2006) Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part V: histologic evaluations of PRF effects on bone allograft maturation in sinus lift. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 101:299–303. doi:10.1016/j.tripleo.2005.07.012
Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, Gogly B (2006) Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part II: platelet-related biologic features. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 101:e45–e50. doi:10.1016/j.tripleo.2005.07.009
Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, Gogly B (2006) Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part I: technological concepts and evolution. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 101:e37–e44. doi:10.1016/j.tripleo.2005.07.008
Sunitha Raja V, Munirathnam Naidu E (2008) Platelet-rich fibrin: evolution of a second-generation platelet concentrate. Indian J Dent Res Off Publ Indian Soc Dental Res 19:42–46
Man D, Plosker H, Winland-Brown JE (2001) The use of autologous platelet-rich plasma (platelet gel) and autologous platelet-poor plasma (fibrin glue) in cosmetic surgery. Plast Reconstr Surg 107:229–237 discussion 238-9
Lekovic V, Milinkovic I, Aleksic Z, Jankovic S, Stankovic P, Kenney EB, Camargo PM (2012) Platelet-rich fibrin and bovine porous bone mineral vs. platelet-rich fibrin in the treatment of intrabony periodontal defects. J Periodontal Res 47:409–417. doi:10.1111/j.1600-0765.2011.01446.x
Panda S, Jayakumar ND, Sankari M, Varghese SS, Kumar DS (2014) Platelet rich fibrin and xenograft in treatment of intrabony defect. Contemporary Clinical Dentistry 5:550–554. doi:10.4103/0976-237x.142830
Sharma A, Pradeep AR (2011) Treatment of 3-wall intrabony defects in patients with chronic periodontitis with autologous platelet-rich fibrin: a randomized controlled clinical trial. J Periodontol 82:1705–1712. doi:10.1902/jop.2011.110075
Kumar RV, Shubhashini N (2013) Platelet rich fibrin: a new paradigm in periodontal regeneration. Cell Tissue Bank 14:453–463. doi:10.1007/s10561-012-9349-6
Ghanaati S, Booms P, Orlowska A, Kubesch A, Lorenz J, Rutkowski J, Landes C, Sader R, Kirkpatrick C, Choukroun J (2014) Advanced platelet-rich fibrin: a new concept for cell-based tissue engineering by means of inflammatory cells. J Oral Implantol 40:679–689. doi:10.1563/aaid-joi-D-14-00138
Gassling VL, Acil Y, Springer IN, Hubert N, Wiltfang J (2009) Platelet-rich plasma and platelet-rich fibrin in human cell culture. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 108:48–55. doi:10.1016/j.tripleo.2009.02.007
Miron RJ, Gruber R, Hedbom E, Saulacic N, Zhang Y, Sculean A, Bosshardt DD, Buser D (2013) Impact of bone harvesting techniques on cell viability and the release of growth factors of autografts. Clin Implant Dent Relat Res 15:481–489. doi:10.1111/j.1708-8208.2012.00440.x
El-Sharkawy H, Kantarci A, Deady J, Hasturk H, Liu H, Alshahat M, Van Dyke TE (2007) Platelet-rich plasma: growth factors and pro- and anti-inflammatory properties. J Periodontol 78:661–669. doi:10.1902/jop.2007.060302
Su CY, Kuo YP, Tseng YH, Su CH, Burnouf T (2009) In vitro release of growth factors from platelet-rich fibrin (PRF): a proposal to optimize the clinical applications of PRF. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 108:56–61. doi:10.1016/j.tripleo.2009.02.004
Okuda K, Kawase T, Momose M, Murata M, Saito Y, Suzuki H, Wolff LF, Yoshie H (2003) Platelet-rich plasma contains high levels of platelet-derived growth factor and transforming growth factor-beta and modulates the proliferation of periodontally related cells in vitro. J Periodontol 74:849–857. doi:10.1902/jop.2003.74.6.849
Kawase T, Okuda K, Wolff LF, Yoshie H (2003) Platelet-rich plasma-derived fibrin clot formation stimulates collagen synthesis in periodontal ligament and osteoblastic cells in vitro. J Periodontol 74:858–864. doi:10.1902/jop.2003.74.6.858
Fan WJ, Yang M, Zhang C, Xue R, Zhang W, Qin HX (2013) Effects of Choukroun’s platelet-rich fibrin on human gingival fibroblasts proliferation, migration and type I collagen secretion. Zhonghua kou qiang yi xue za zhi = Zhonghua kouqiang yixue zazhi =. Chin J Stomatol 48:72–76
Dohan Ehrenfest DM, Doglioli P, de Peppo GM, Del Corso M, Charrier JB (2010) Choukroun’s platelet-rich fibrin (PRF) stimulates in vitro proliferation and differentiation of human oral bone mesenchymal stem cell in a dose-dependent way. Arch Oral Biol 55:185–194. doi:10.1016/j.archoralbio.2010.01.004
Kawase T, Okuda K, Saito Y, Amizuka N, Suzuki H, Yoshie H (2005) Platelet-rich plasma provides nucleus for mineralization in cultures of partially differentiated periodontal ligament cells. In Vitro Cell Dev Biol Anim 41:171–176. doi:10.1290/0502013.1
Kawase T, Tanaka T, Okuda K, Tsuchimochi M, Oda M, Hara T (2015) Quantitative single-cell motility analysis of platelet-rich plasma-treated endothelial cells in vitro. Cytoskeleton (Hoboken, NJ) 72:246–255. doi:10.1002/cm.21221
Gassling V, Hedderich J, Acil Y, Purcz N, Wiltfang J, Douglas T (2013) Comparison of platelet rich fibrin and collagen as osteoblast-seeded scaffolds for bone tissue engineering applications. Clin Oral Implants Res 24:320–328. doi:10.1111/j.1600-0501.2011.02333.x
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Funding
The project was funded by the Department of Cranio-Maxillofacial Surgery at the University of Bern.
Ethical approval
Blood was drawn from patients (lab members) with informed signed consent. An ethical approval was not required for this purpose. No animals were used in this study.
Informed consent
All blood was drawn from patients (lab members) with informed signed consent.
Rights and permissions
About this article
Cite this article
Kobayashi, E., Flückiger, L., Fujioka-Kobayashi, M. et al. Comparative release of growth factors from PRP, PRF, and advanced-PRF. Clin Oral Invest 20, 2353–2360 (2016). https://doi.org/10.1007/s00784-016-1719-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-016-1719-1